ABSTRACT
Endoscopic placement of the plastic stent has been adopted as an initial treatment for chronic pancreatitis with pancreatic duct stricture. Stent fracture while attempting removal is one of the complications of stent exchange. The use of the unilateral-flange stent in these patients has never been reported. We investigated the outcomes associated with the use of this stent with regard to stent exchange and stent-related adverse events. From 2011 to 2015, 9 patients with chronic pancreatitis and main pancreatic duct (MPD) stricture treated with the unilateral-flange stent were included. Eleven endoscopic treatment sessions, 53 endoscopic stent deployments or exchange procedures were analyzed. Technical success rate was 100%. Forty-eight stents were exchanged on a regular basis in 1 to 6-month intervals. Another 5 stent exchange procedures were urgently performed due to stent obstruction and caused pancreatitis (n=2), symptomatic external stent migration (n=2), and concurrent cholangitis (n=1). The rate of symptomatic migration was 3.7%. The mean duration for stent exchange was 29 minutes and no stent fracture occurred during the procedure. Of 11 endoscopic treatment sessions, 7 were successful, 3 were changed to the metallic stents, and 1 was lost to follow-up. According to this study, unilateral-flange stent placement for benign MPD stricture is technically feasible and effective. Stent removal during the exchange period is unchallenging and without stent fracture.
Key Words: stents, pancreatic ducts, chronic pancreatitis, stricture, endoscopic retrograde cholangiopancreatography
INTRODUCTION
The management of benign main pancreatic duct (MPD) stricture due to chronic pancreatitis is mostly performed initially with endoscopy due to the lower invasiveness and short hospital stay associated with the modality. A treatment session usually comprises multiple procedures such as stent placement and subsequent replacement with a new stent. Generally, the bilateral-flange plastic stent has been used to prevent both internal and external migration1).
In patients with chronic pancreatitis, attempts to remove the old stent during the exchange procedure is occasionally challenging. Chronic inflammation which leads to stent clogging and impaction in the MPD has been implicated for this difficulty. Occasionally, stent fracture occurs, with a rate of about 1% as noted in a recently published study2). Despite its rareness, stent fracture is particularly challenging for the endoscopist owing to the difficulty of removing the distal fractured part through the stricture. Successful removal via endoscopy is reported only in approximately 50% of cases, with some patients requiring surgery.
The unilateral-flange stent, which has only one external flange, has been commonly used for the prevention of post-endoscopic retrograde cholangiopancreatograophy (post-ERCP) pancreatitis. The stent can spontaneously migrate into the intestine due to its small caliber and lack of an internal flange, making repeated endoscopy to remove the stent unnecessary. To our knowledge, no study has reported the use of this stent for treating patients with pancreatic duct stricture. We postulated that the unilateral-flange stent would reduce difficulty during stent exchange and stent fracture rates. The aim of this study was to evaluate the feasibility of the unilateral-flange stent, in terms of technical success and stent-related adverse events.
MATERIALS AND METHODS
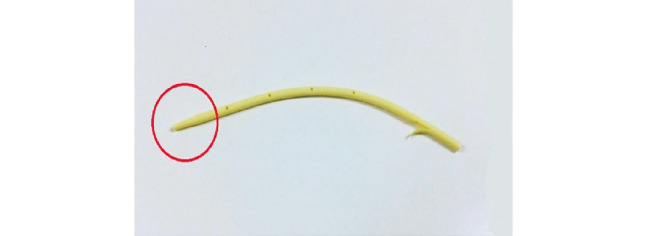
We developed a plastic stent, with a unilateral flange (CX-T™ stent, Gadelius Medical, Tokyo, Japan) and with a size of 7-10 Fr, for stricture treatment. In addition, the upstream tip of the stent which is advanced into the MPD has a tapered end facilitating easier removal (Figure 1).
Fig. 1.
Unilateral-flange stent. Note the internal tapered end without a flange (red circle).
Patients were initially sedated using 5 mg of diazepam and 50 mg of meperidine. Additional doses were administered according to patient’s level of sedation. A side-viewing endoscope (JF240, JF260V or TJF260V, Olympus, Japan) was used. Cannulation into the MPD was achieved using a taper-tipped catheter (TandemTM, Boston scientific, US), and a 0.025-inch wire (Visiglide®, Olympus, Japan). Examination of the ductal stricture was accomplished by injecting contrast media. One unilateral-flange stent (CX-T ™ stent, Gadelius Medical, Tokyo, Japan) was placed during each individual endoscopic procedure. Stent size and length were decided depending on the tightness and length of the MPD stricture, and a 7-10 Fr unilateral-flange stent was placed. We scheduled the patients for stent exchange on a regular basis, ranging from 1-6 months. Changing management from the unilateral-flange stent to the self-expandable metallic stent (SEMS) was at the discretion of the endoscopist. Generally, we changed the management to SEMS when the management of stenosis exceeded 12 months or 5 procedures, especially if the stenosis was considered by the endoscopist to have a hard consistency, which could make inserting the plastic stent difficult.
We conducted this retrospective study in Aichi Cancer Center, Japan, after implementing this stent over a period. Data of patients with chronic pancreatitis who had benign MPD stricture and had been treated with endoscopic plastic stent placement were identified. Patient characteristics, number of stents used, previous treatment before unilateral-flange stent placement, outcome, and adverse events were collected. Adverse events were reported based on a previous report3). We described average as mean and median and described proportion as percentage. The outcome of treatment was considered successful if there was an improvement in the stricture and symptom or lesionleading to the procedure was successfully managed. This study was conducted with the formal approval of the hospital institutional review board.
RESULTS
Patient and disease characteristics (Table 1)
Table 1.
Patient characteristics.
| Patient characteristics | N |
|---|---|
| Gender; M;F | 7:2 |
| Etiology of chronic pancreatitis | |
| Alcoholic | 7 |
| Idiopathic | 2 |
| Mean age; year (range) | 57.5 (39-69) |
| Coexisting pancreatic ductal stone | 4 |
| Site of stricture | |
| Pancreatic head | 8 |
| Pancreatic body | 1 |
| Length of stricture | |
| Less than 10 mm | 7 |
| 10-20 mm | 1 |
| More than 20 mm | 1 |
| Indication for therapy | |
| Abdominal pain due to chronic pancreatitis | 2 |
| Acute exacerbation of pancreatitis | 3 |
| Pancreatic pseudocyst | 2 |
| Increased upstream main pancreatic duct dilatation | 1 |
| Pancreatic duct stone | 1 |
Nine patients (7 male and 2 female) aged between 39-69 years were identified. The etiology of the chronic pancreatitis was alcoholic (n=7) and idiopathic (n=2). Coexisting MPD stones occurred in 4 patients. Previous treatments of ductal stricture before the use of the unilateral-flange stent were endoscopic pancreatic sphincterotomy (n=4) and bilateral-flange plastic stent placement (n=7). Five patients underwent endoscopic treatment due to symptoms related to MPD stricture; another 4 patients were asymptomatic but had lesions related to the treatment. All except 1 patient had MPD stricture at the pancreatic head.
Procedure characteristics
Among 9 patients, 2 experienced recurrence of index diseases. Therefore, a total of 11 treatment sessions and 53 endoscopic procedures composed of at least one unilateral-flange stent placement or removal were included in this study. The median (range) duration of stent insertion was 324 days (166-1231 days). The median number of stents used per session was 4 (range 1-20).
Outcome and adverse events
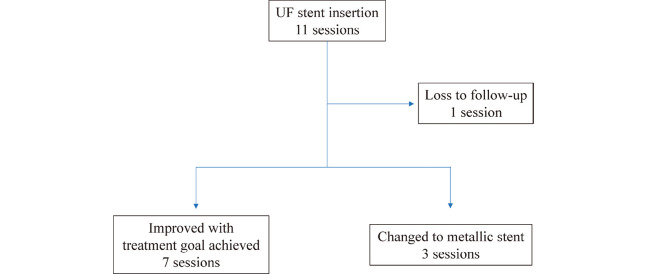
Technical success rate of stent placement was 100%. Among 11 endoscopic treatment sessions, 7 were successful. In 3, the stents were changed from the unilateral-flange stent to SEMS. One patient was lost to follow-up (Figure 2).
Fig. 2.
Outcome of main pancreatic duct stricture treated with the unilateral-flange stent in 11 endoscopic sessions.
Of 53 unilateral-flange stent placement procedures, stent exchange was performed for 48 (90.5%) as scheduled. Five new unilateral-flange stent insertion procedures were urgently performed due to the external migration of the stent resulting in symptom recurrence (n=2, 3.8%), stent obstruction and pancreatitis (n=2, 3.8%), and concurrent cholangitis (n=1, 1.9%). These migrations occurred at 20 and 58 days, respectively, after the previous procedure, and obstruction occurred at 59 and 147 days, respectively. Other mild adverse events were mild post-procedure pancreatitis (n=3, 5.7%), low-grade fever lasting less than 2 days (n=1, 1.9%), and Mallory-Weiss syndrome without clinically significant bleeding (n=1, 1.9%) (Table 2). Another two stents (3.8%) were externally migrated without symptom recurrence and change in the patient care. The characteristics of patients with stent migration are shown in Table 3. The mean stent exchange duration was 29 minutes and no stent fracture was observed.
Table 2.
Adverse events in the unilateral-flange stent placement procedure.
| Adverse events | n (%) |
|---|---|
| Stent-related adverse events | |
| Stent external migration resulting in symptom recurrence | 2 (3.8%) |
| Pancreatitis due to stent obstruction | 2 (3.8%) |
| Procedure-related adverse events | |
| Mild post-procedure pancreatitis | 3 (5.7%) |
| Low-grade fever | 1 (1.9%) |
| Mallory-Weiss syndrome | 1 (1.9%) |
| Cholangitis | 1 (1.9%) |
Table 3.
Characteristics of patients with unilateral-flange stent migration.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
|---|---|---|---|---|
| Gender | Female | Female | Male | Male |
| Age | 57 | 58 | 65 | 59 |
| Etiology of pancreatitis | Idiopathic | Idiopathic | Alcoholic | Alcoholic |
| Stricture location | Body | Body | Head | Head |
| Stricture length | <10 mm | <10 mm | <10 mm | <10 mm |
| Duration of PS before migration (days) | 706 | 769 | 926 | 539 |
| Symptomatic migration | Yes | No | Yes | No |
| Persistence of stricture | Yes | Yes | Yes | No |
| Management after migration | Reinserted UF stent | Changed to metallic stent | Reinserted UF stent | Stent-free |
| Final outcome | Successful | Successful | Successful | Successful |
PS, plastic stent; UF, unilateral-flange.
DISCUSSION
To our knowledge, this is the first study reporting the feasibility of the unilateral-flange stent for the treatment of benign MPD stricture due to chronic pancreatitis. To avoid migration in both internal and external directions, the bilateral-flange plastic stent has been routinely used for this indication. However, our study shows that despite the absence of an inner flange, the rate of external migration (7.6%) was not significantly higher than that of the bilateral-flange stent, which was reported to be between 3.8 and 7.5%2,4). Moreover, half of the migration in our study was due to the improvement of the stricture and needed no further management.
Unlike the unilateral-flange stent used to prevent post-ERCP pancreatitis and which has a 30-day migration rate of 80-90%5,6), more than 90% of the unilateral-flange stents in our study were still in place until the scheduled day of exchange. Larger caliber stents and the narrowness of the pancreatic ductal stricture may have helped to hold the stent, and explain the result of our study.
In addition, our study showed that the efficacy of the unilateral-flange stent for treating MPD stricture was approximately equal to that of bilateral-flange stent7). Successful treatment with the unilateral-flange stent was achieved in nearly 64% of patients. The rate of serious adverse events was also acceptable.
The precipitation of albumin and lithostatin, especially in the side hole and inner flange of the pancreatic plastic stent8), was expected to cause stent impaction within the MPD, which also causes difficulty during removal and occasional stent fracture. Our study showed that the unilateral-flange stent can easily be exchanged; we reported a short mean duration of the stent exchange procedure. Moreover, no stent fracture was observed in our study; the lag of the internal flange and the tapered distal end of the stent may be the main reasons for our findings.
Our study limitations are its retrospective in nature and the small number of patients. One patient was lost to follow-up during the endoscopic treatment session; thus, it is unknown whether any adverse event occurred in this patient. The small number of patients may have precluded our study from identifying rare adverse events, such as intestinal perforation caused by an externally migrated stent, which has been reported recently9).
CONCLUSION
The unilateral-flange stent can be used to treat benign MPD stricture due to chronic pancreatitis. Compared to the routinely used bilateral-flange plastic stent, the unilateral-flange stent seems to have similar outcomes, is easily exchanged, and has a lower rate of stent fracture. A larger prospective study seems necessary to verify our findings.
ACKNOWLEDGEMENTS
We would like to thank Dr. Shibuya Hitoshi, Dr. Hirayama Takashi, Dr. Suzuki Hirotaka, Dr. Kondo Hisashi, Dr. Fujita Akashi, Dr. Matsumoto Shinpei, Dr. Iwaya Hiroshi, Dr. Kuraoka Naosuke, and Dr. Itou Ayako, for their support regarding the medical chart review and language translation.
REFERENCES
- 1).Artifon EL, Vila JJ, Otoch JP. Pancreaticobiliary Stent Removal: Migrated and Nonmigrated. In: Baron TH, Kozarek RA, Carr-Locke DL. ERCP. Philadelphia, Pa: Elsevier Health Sciences; 2012: 212-221.
- 2).Kawaguchi Y, Lin JC, Kawashima Y, Maruno A, Ito H, Ogawa M, et al. Risk factors for migration, fracture, and dislocation of pancreatic stents. Gastroenterol Res Pract, 2015; 2015: 365457. [DOI] [PMC free article] [PubMed]
- 3).Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc, 2010; 71: 446-454. [DOI] [PubMed]
- 4).Johanson JF, Schmalz MJ, Geenan JE: Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest Endosc, 1992; 38: 41-346. [DOI] [PubMed]
- 5).Lawrence C, Cotton PB, Romagnuolo J, Payne KM, Rawls E, Hawes RH. Small prophylactic pancreatic duct stents: an assessment of spontaneous passage and stent-induced ductal abnormalities. Endoscopy, 2007; 39: 1082-1085. [DOI] [PubMed]
- 6).Moffatt DC, Coté GA, Fogel EL, Watkins JL, McHenry L, Lehman GA, et al. Acute pancreatitis after removal of retained prophylactic pancreatic stents. Gastrointest Endosc, 2011; 73: 980-986. [DOI] [PubMed]
- 7).ASGE Standards of Practice Committee, Chandrasekhara V, Chathadi KV, Acosta RD, Decker GA, Early DS, Eloubeidi MA, et al. The role of endoscopy in benign pancreatic disease. Gastrointest Endosc, 2015; 82: 203-214. [DOI] [PubMed]
- 8).Farnbacher MJ, Voll RE, Faissner R, Wehler M, Hahn EG, Löhr M, et al. Composition of clogging material in pancreatic endoprostheses. Gastrointest Endosc, 2005; 61: 862-866. [DOI] [PubMed]
- 9).Ortega PM, Zozaya-Larequi G, Arredondo J, Martí-Cruchaga P, Bellver M, Sánchez-Justicia C, et al. Distal migration of a transanastomotic pancreatic stent resulting in bowel perforation 19 years after pancreatoduodenectomy: report of a case. Surg Today, 2015; 45: 374-377. [DOI] [PubMed]