ABSTRACT
Patellofemoral cartilage degeneration is a potential complication of anterior cruciate ligament reconstruction (ACLR) surgery. Hypomobility of the patella in the coronal plane is often observed after ACLR. Few studies, however, have examined the relationship between cartilage degeneration in the patellofemoral joint and mobility after ACLR. The present study investigated 1) the coronal mobility of the patella after ACLR, 2) the relationship between patellar mobility and cartilage degeneration of the patellofemoral joint, and 3) the relationship between patellar mobility and knee joint function after ACLR. Forty patients who underwent medial hamstring-based ACLR participated in the study. Lateral and medial patellar displacements were assessed with a modified patellofemoral arthrometer, and the absolute values of the displacements were normalized to patient height. The International Cartilage Repair Society (ICRS) cartilage injury classification of the patellar and femoral (trochlear) surfaces, and the Lysholm Knee Scoring Scale were used to evaluate knee function. Lateral and medial patellar displacements were reduced compared with the non-operated knee at the second-look arthroscopy and bone staple extraction operation (second operation; 24.4 ± 7.9 months after ACLR, P<0.01). The ICRS grades of the patellofemoral joint (patella and trochlea) were significantly worse than those pre-ACLR. Neither lateral nor medial patellar mobility, however, were significantly correlated with the ICRS grade or the Lysholm score. Although patellar mobility at approximately 2 years after ACLR was decreased compared to the non-operated knee, small displacement of the patella was not related to cartilage degeneration or knee joint function at the time of the second operation.
Key Words: patellofemoral joint, cartilage, patellar mobility, anterior cruciate ligament reconstruction
INTRODUCTION
Cartilage degeneration and/or osteoarthritis of the patellofemoral (PF) joint is a potential complication following anterior cruciate ligament reconstruction (ACLR),1-3) and occurs in as many as around 30% of patients after ACLR.4) Cartilage degeneration leads to the deterioration of knee joint function, resulting in PF joint pain, especially during sport activities.5,6) A previous report described an association between PF joint pain and abnormal patellar mobility, such as hypomobility or hypermobility, in the coronal plane.7) Hypomobility of the patella is often seen after ACLR due to the invasiveness of knee joint surgery, and limited patellar mobility is reported to worsen patellar cartilage degeneration due to excessive patellofemoral contact force8). Therefore, therapy to improve patellar mobility is implemented as postoperative rehabilitation.9,10) Restricted patellar mobility after ACLR has been described,11) but the assessments were subjective. Due to the limited data available regarding the relationship between patellar mobility and chondropathy of the PF joint after ACLR, the effects of therapeutic improvement of patellar mobility after surgery to prevent patellar cartilage degeneration and maintain physical function should be investigated.
The purpose of the present study was to investigate 1) coronal mobility of the patella after ACLR, 2) the relationship between patellar mobility and cartilage degeneration in the PF joint, and 3) the relationship between patellar mobility and knee joint function after ACLR.
METHODS
Subjects
Forty patients (men: 26, women: 14, mean age: 30.9 years, range 18 – 49 years) underwent ACLR surgery from April 2011 through January 2012, and secondary surgery, i.e., second-look arthroscopy and bone staple extraction at Nagoya Mitsubishi Hospital. All patients underwent medial hamstring-based ACLR, and the same surgeon (K.K.) performed the ACLR surgery and second operation. The non-operated knee joint in all patients had no history of knee joint surgery and no knee joint problems at the second operation; all patients underwent medial hamstring-based ACLR. The mean postoperative follow-up period after ACLR was 24.4 ± 7.9 months. The present study was approved by the Ethics committee of Nagoya Mitsubishi Hospital.
Assessment of patellar mobility
Passive coronal mobility of the patella was assessed with a modified patellofemoral arthrometer (PFA, Brace-Fit, LLC, Aichi, Japan, Fig. 1) using the same measurement procedures with acceptable reliability (intraclass correlation coefficient [ICC] = 0.89-0.97 between testers)7) and validity (ICC = 0.86 compared to magnetic resonance imaging measurement)12). The patients were positioned supine with the leg in a neutral position (0° hip rotation). The PFA was fixed on the femoral condyles, and the PFA was clamped to the femoral condyles aligned parallel with the table (Fig. 1A). A digital caliper was adjusted perpendicular to the line between the center of the patella and the anterior superior iliac spine to assess the lateral passive patellar displacement (LPD) and medial passive patellar displacement (MPD) (Fig. 1B).
Fig. 1.
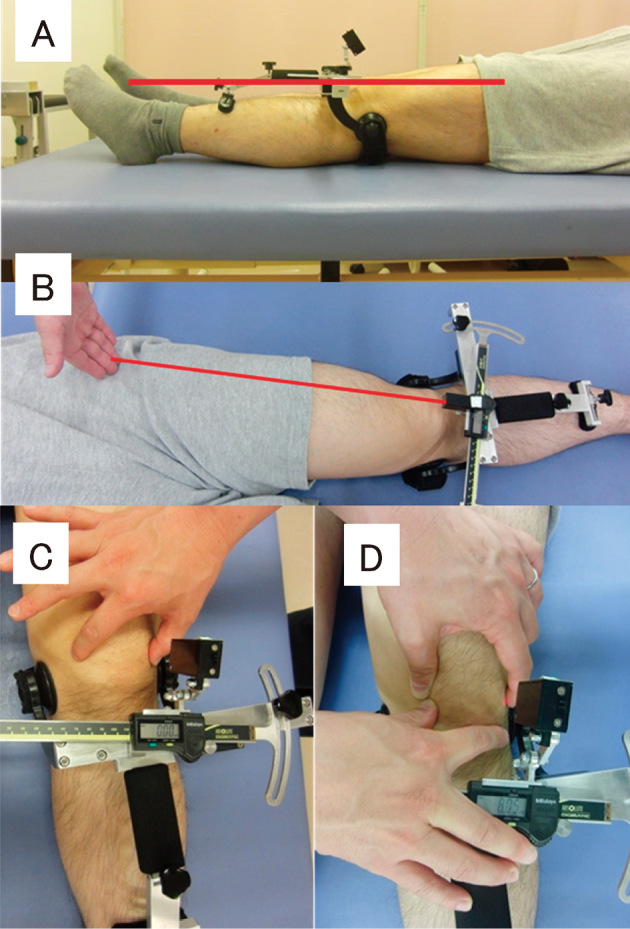
Method of testing lateral patellar displacement using a modified patellofemoral arthrometer (PFA).
The PFA was clamped to the femoral condyles aligned parallel with the table (A). The digital caliper was positioned at a 90° angle to the line between the center of the patella and the anterior superior iliac spine (B). The difference in the patellar border between the initial measurement (C) and at manual displacement was measured (D), and defined as patellar displacement (patellar mobility).
To measure LPD, the lateral side of the patellar border was palpated and located with a laser using an adjustable laser module arm (Fig. 1C), and the digital caliper was set at zero to define this point as the initial position. LPD was then determined by manually pushing the patella laterally, at which point the side of the patella was again located by sliding the laser module arm and the distance read (Fig.1D). Pushing force was subjectively determined by feeling the end motion by one tester (K.K.). The MPD was assessed in the same manner, pushing the patella medially. Patellar mobility was measured under anesthesia just before the second operation.
Evaluation of cartilage degeneration of the PF joint and physical examination
The cartilage of the patellar and femoral (trochlear) surface was evaluated based on the International Cartilage Repair Society (ICRS) cartilage injury classification (grade) by one surgeon (K.K.). Cartilage evaluation was performed at the time of the ACLR surgery (pre-ACLR surgery) and at the second surgery by the same surgeon (K.K.). Physical function was assessed using the Lysholm Knee Scoring Scale, and passive knee extension angles (positive value indicates hyperextension of the knee joint) were measured with the patient in a supine position using a general goniometer at the second operation. The same rehabilitation program was applied to all patients after ACLR by physical therapists in the perioperative period at the Mitsubishi Nagoya Hospital. The orthopedic checkup was performed by one surgeon (K.K.) periodically, and the rehabilitation schedule was the same for all patients.
Data analysis
The absolute values of the LPD and MPD, those values normalized to patient height (LPH/HT and MPD/HT, respectively), and the difference between LPD and MPD (LPD-MPD, LPD-MPD/HT, respectively) as the latero-medial balance,13) were used for the final analysis of patellar mobility. The data were tested for normal distribution using the Shapiro-Wilk test. For normally distributed data, the paired t-test was used to determine differences. For non-normally distributed data, the Wilcoxon signed-rank test (dependent samples) or Mann-Whitney U test (independent samples) was used to determine differences. The correlation of patellar mobility with knee joint function (Lysholm score and knee extension angle) was analyzed using Pearson’s correlation or Spearman’s rank correlation based on the data distribution. A P value less than 0.05 was considered statistically significant. All statistical analyses were performed with SPSS, version 16 for Japanese (IBM Japan, Tokyo, Japan).
RESULTS
The results of the patellar mobility assessment and physical examinations at the second operation are shown in Table 1. The LPD, MPD, LPD/HT, and MPD/HT values of the surgery knee were significantly smaller than those of the non-operated knee (p < 0.01). LPD-MPD and LPD-MPD/HT, however, were not significantly different between operated and non-operated knees. The mean knee extension angle was 1.7±2.1 degrees and mean Lysholm knee score was 97.4±16.2 at the second operation.
Table 1.
Patellar mobility and physical examination results at the second operation.
| Operated knee | Non-operated knee | P value | |
|---|---|---|---|
| LPD (mm) | 7.0±1.9 | 8.6±2.1 | <0.001b |
| MPD (mm) | 7.6±2.0 | 8.8±3.0 | 0.005b |
| LPD/HT (%) | 0.42±0.12 | 0.51±0.12 | <0.001a |
| MPD/HT (%) | 0.45±0.12 | 0.52±0.17 | 0.004b |
| LPD - MPD (mm) | -0.58±1.8 | -0.21±3.2 | 0.126b |
| LPD - MPD/HT (%) | -0.03±0.11 | -0.01±0.19 | 0.133b |
| Knee extension angle (°) | 1.7±2.6 | — | — |
| Lysholm knee score (points) | 97.4±16.2 | — | |
a paired t-test.
b Wilcoxon signed-rank test.
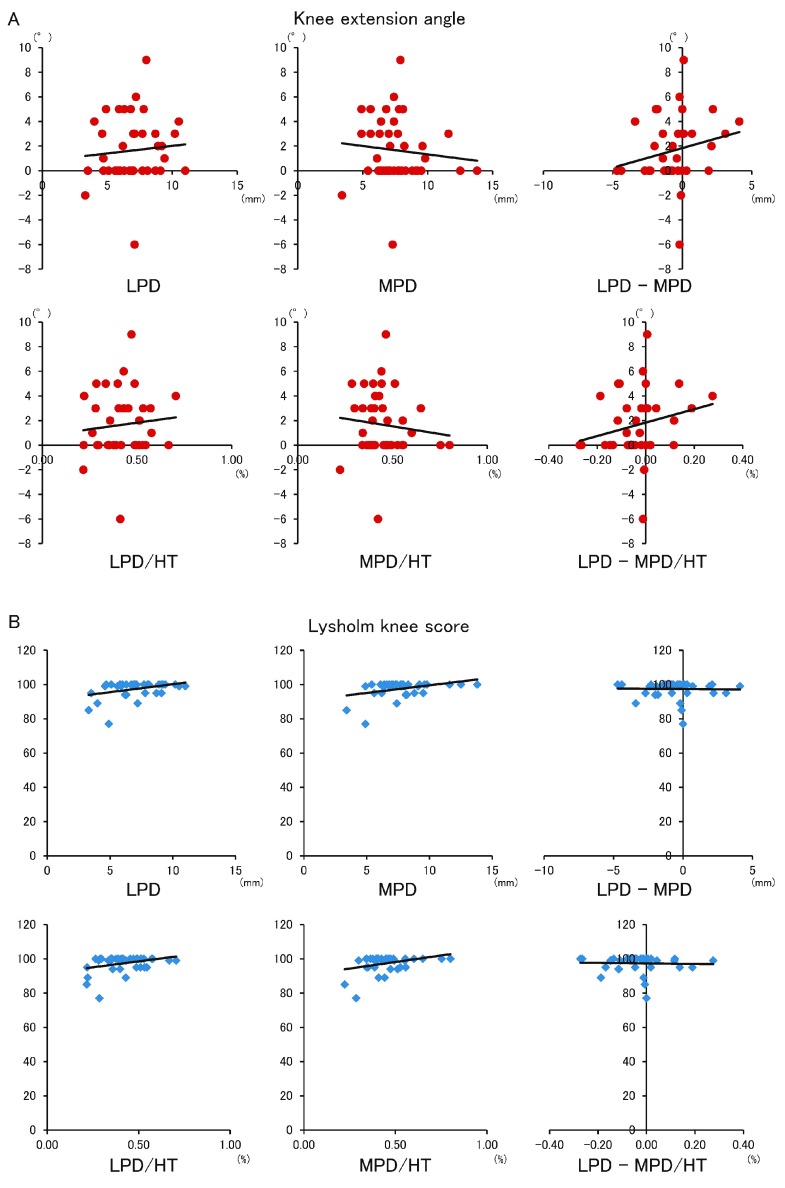
The ICRS grades of the PF joint at the second operation were significantly worse than those pre-ACLR (Table 2). Patellar mobility was not significantly correlated to the ICRS score of the patellar and trochlear surfaces. (Table 3). The LPD, MPD, LPD/HT, and MPD/HT values were not significantly correlated with knee extension angle or the Lysholm score (Tables 4, 5, Fig. 2).
Table 2.
Patellofemoral joint cartilage assessment results at pre-ACLR and at the second operation (Wilcoxon signed-rank test).
| ICRS grade | 0 | 1 | 2 | 3 | Median | P value | |
|---|---|---|---|---|---|---|---|
| Patella | pre-ACLR surgery | 16 | 19 | 2 | 3 | 1 | 0.018 |
| Second operation | 7 | 25 | 5 | 3 | 1 | ||
| Trochlea | pre-ACLR surgery | 24 | 11 | 2 | 3 | 0 | 0.002 |
| Second operation | 14 | 14 | 5 | 7 | 1 |
ICRS, International Cartilage Repair Society
Table 3.
Correlations (r value) between patellar mobility and patellofemoral joint cartilage assessment results (International Cartilage Repair Society grade) at the second operation (Spearman’s correlation coefficient).
| Patella | P value | Trochlea | P value | |
|---|---|---|---|---|
| LPD | 0.14 | 0.38 | 0.04 | 0.81 |
| MPD | 0.21 | 0.20 | 0.11 | 0.51 |
| LPD/HT | 0.14 | 0.45 | 0.03 | 0.88 |
| MPD/HT | 0.20 | 0.22 | 0.10 | 0.54 |
| LPD - MPD | -0.04 | 0.96 | -0.03 | 0.91 |
| LPD - MPD/HT | -0.13 | 0.98 | -0.12 | 0.88 |
LPD, lateral patellar displacement; MPD, medial patellar displacement; HT, height
Table 4.
Correlations (r value) between patellar mobility, and cartilage change, knee extension angle, and Lysholm score.
| Knee ext. angle |
P value | Lysholm knee score |
P value | |
|---|---|---|---|---|
| LPD | 0.09 | 0.59a | 0.23 | 0.15b |
| MPD | -0.10 | 0.53a | 0.26 | 0.11b |
| LPD/HT | 0.09 | 0.57a | 0.19 | 0.24b |
| MPD/HT | -0.11 | 0.50a | 0.23 | 0.15b |
| LPD - MPD | 0.21 | 0.19a | -0.09 | 0.58 b |
| LPD - MPD/HT | 0.22 | 0.17a | -0.09 | 0.57b |
Knee ext. angle, knee extension angle; LPD, lateral patellar displacement; MPD, medial patellar displacement; HT, height.
a Pearson’s correlation coefficient.
b Spearman’s correlation coefficient.
Table 5.
Correlations (r value) between patellar mobility and section scores of the Lysholm Knee Scoring Scale (Spearman’s correlation coefficient).
| Pain | P | In- Stability |
P | Locking | P | Stair climbing |
P | Squatting | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| LPD | 0.13 | 0.44 | 0.11 | 0.50 | 0.11 | 0.51 | 0.19 | 0.25 | 0.30 | 0.06 |
| MPD | -0.06 | 0.70 | 0.14 | 0.37 | 0.11 | 0.48 | 0.25 | 0.12 | 0.25 | 0.12 |
| LPD/HT | 0.13 | 0.43 | 0.11 | 0.50 | 0.15 | 0.35 | 0.20 | 0.21 | 0.27 | 0.09 |
| MPD/HT | -0.01 | 0.94 | 0.16 | 0.33 | 0.15 | 0.36 | 0.26 | 0.11 | 0.24 | 0.14 |
| L-M | 0.19 | 0.25 | 0.00 | 1.00 | -0.05 | 0.77 | -0.11 | 0.50 | -0.08 | 0.62 |
| L-M/HT | 0.19 | 0.25 | 0.00 | 1.00 | -0.04 | 0.79 | -0.11 | 0.50 | -0.08 | 0.62 |
LPD, lateral patellar displacement; MPD, medial patellar displacement; HT, height; L-M, LPD-MPD; P: p value.
Fig. 2.
Correlations between patellar mobility and knee extension angle (A) and the Lysholm score (B) with scatter plots.
Note: There were no significant correlations between any of the parameters. Fig.2B shows the celling effect of the Lysholm score.
DISCUSSION
The LPD, MPD, LPD/HT, and MPD/HT values at the second-look arthroscopy (second operation) around 2 years after ACLR revealed significantly decreased mobility compared with the non-operated knee. Reduced patellar mobility is reportedly associated with PF pain14) and stiff knee after knee joint injuries.15,16) Peri-patellar soft tissue,15-19) patellar height,20,21) and morphology of the patella and trochlea20) are associated with lateral and medial patellar mobility. Reduced elasticity of the medial peri-patellar soft tissues, including the medial patella femoral ligament and retinaculum, are associated with restricted lateral patellar mobility,17-19) and reduced elasticity of the lateral peri-patellar soft tissues, including the iliotibial band and retinaculum, are associated with restricted medial patellar mobility. The restricted lateral and medial patellar mobility in the present study was assumed to be related to soft tissue tightness following knee joint surgery. Although the present study did not investigate the factors involved in the reduced lateral and medial patellar mobility, this is the first report of reduced patellar mobility after ACLR based on quantitative assessment. The present findings also indicate reduced patellar mobility at approximately 2 years after ACLR compared to the non-operated knee.
The ICRS scores of the patellar and trochlea surfaces were significantly different between the first and second operation (Table 2), but patellar mobility was not significantly correlated to cartilage degeneration assessed with ICRS score of the patellar and trochlear surfaces (Table 3). Fulkerson et al.22) and Mercian et al.23) reported that lateral compression force on the PF joint due to a large lateral patellar tilt with tightness of the lateral peri-patellar soft tissues induces degeneration of the PF cartilage. The present study indicated that the difference between LPD and MPD (i.e., LPD-MPD) values were not significantly different between the knee that underwent ACLR and the non-operated knee (Table 1), and therefore excessive partial high pressure on the PF joint might not have occurred in our subjects.
The subjects in the present study exhibited no knee extension angle restriction at the second operation, and the angle was not correlated with patellar mobility (Table 4, Fig. 2A). Patellar stability changed according to the knee joint flexion angle due to complex interactions attributed to individual variability in the trochlear groove anatomy,24) tibia tubercle position,25) patellar height,26) and peri-patellar soft tissues, including mainly the medial patellofemoral ligament.21,27) No passive patellar mobility data are available for multiple knee joint angles. Future studies should investigate the influence of the knee joint angle on passive patellar mobility based on differences in the trochlear groove anatomy.
LPD, MPD, LPD/HT, MPD/HT, LDP-MPD, and LDP-MPD/HT were not correlated with knee joint function, as assessed by the Lysholm score (Table 4, Fig. 2B). Hypomobility of the patella was assumed to induce high compressive force on the patellofemoral joint or mal-tracking of the patella,22,23) but no significant correlation was detected because of the ceiling effect of the Lysholm score with a high number of patients having a high Lysholm score (Fig. 2B). Consequently, each section of the Lysholm Knee Scoring Scale was investigated separately, and patellar mobility was not significantly correlated with any of the subsections of the Lysholm Knee Scoring Scale (Table 5). Although the correlation was not significant, the squatting subscore was borderline significant correlated with both LPD (r = 0.30, P = 0.06) and LPD/HT (r = 0.27 and P = 0.09). Therefore, we should consider the relationship between squatting and lateral patellar mobility, especially during the early stage with decreased knee joint function. If lateral patellar mobility is significantly correlated with squatting, improvement of lateral patellar mobility should be an aim of rehabilitation. Clinically, patellar mobilization9,22,28) improvement therapy was applied in cases of reduced patellar mobility with patellofemoral pain and/or after knee joint surgery. If the relationship between the direction of the reduced patellar mobility and knee function, including knee pain and limitation of knee range of motion, is clear, then therapy could be applied more specifically to increase patellar mobility (patellar mobilization).
The present study has three limitations. First, patellar mobility was assessed at only the second operation and therefore, we could not infer a longitudinal relationship between patellar mobility and knee joint function. Patellar mobility should have been assessed both pre-ACLR and at the second operation. Second, although patellar mobility was assessed according to a previous report, the amount of pushing force in the present study was only subjectively estimated and therefore not exactly the same as in the previous report.7,29) Thus, patellar displacement could not be compared with that in healthy individuals in previous reports. Third, one tester measured patellar displacement as described previously, but the reliability of the patellar mobility testing was not assessed. Additionally, the reliability of the ICRS grade was not determined in the present study.
In conclusion, lateral and medial patellar mobility were reduced after ACLR compared with that on the non-operated knee, and the reduced patellar mobility 2 years after ACLR was not related to decreased knee joint function after ACLR.
CONFLICT OF INTEREST
S. Ota has a national patent in Japan for a patellofemoral arthrometer (patent number 4800016). Brace•Fit LLC has the exclusive license. Brace•Fit LLC had no control over the design, analysis, interpretation, writing, or publication of this study.
REFERENCES
- 1).Asano H, Muneta T, Ikeda H, Yagishita K, Kurihara Y, Sekiya I. Arthroscopic evaluation of the articular cartilage after anterior cruciate ligament reconstruction: a short-term prospective study of 105 patients. Arthroscopy, 2004; 20: 474-481. [DOI] [PubMed]
- 2).Oiestad BE, Holm I, Engebretsen L, Aune AK, Gunderson R, Risberg MA. The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc, 2013; 21: 942-949. [DOI] [PubMed]
- 3).Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M. Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury--a prospective cohort study. Osteoarthritis Cartilage, 2009; 17: 284-290. [DOI] [PubMed]
- 4).Oksman A, Dmytruk V, Proust J, Mabit C, Charissoux JL, Arnaud JP. Patellar chondropathy prevalence at anterior cruciate ligament reconstruction: analysis of 250 cases. Orthop Traumatol Surg Res, 2009; 95: 36-39. [DOI] [PubMed]
- 5).Devereaux MD, Lachmann SM. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br J Sports Med, 1984; 18: 18-21. [DOI] [PMC free article] [PubMed]
- 6).Levy AS, Lohnes J, Sculley S, LeCroy M, Garrett W. Chondral delamination of the knee in soccer players. Am J Sports Med, 1996; 24: 634-639. [DOI] [PubMed]
- 7).Ota S, Nakashima T, Morisaka A, Ida K, Kawamura M. Comparison of patellar mobility in female adults with and without patellofemoral pain. J Orthop Sports Phys Ther, 2008; 38: 396-402. [DOI] [PubMed]
- 8).Singerman R, White C, Davy DT. Reduction of patellofemoral contact forces following anterior displacement of the tibial tubercle. J Orthop Res, 1995; 13: 279-285. [DOI] [PubMed]
- 9).Malempati C, Jurjans J, Noehren B, Ireland ML, Johnson DL. Current Rehabilitation Concepts for Anterior Cruciate Ligament Surgery in Athletes. Orthopedics, 2015; 38: 689-696. [DOI] [PubMed]
- 10).Beynnon BD, Uh BS, Johnson RJ, Abate JA, Nichols CE, Fleming BC, Poole AR, Roos H. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med, 2005; 33: 347-359. [DOI] [PubMed]
- 11).Harner CD, Irrgang JJ, Paul J, Dearwater S, Fu FH. Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med, 1992; 20: 499-506. [DOI] [PubMed]
- 12).Ota S, Ward SR, Chen Y-j, Tsai Y-j, Powers CM. Concurrent criterion-related validity and reliability of a clinical device used to assess lateral patellar displacement. J Orthop Sports Phys Ther, 2006; 36: 645-652. [DOI] [PubMed]
- 13).Skalley TC, Terry GC, Teitge RA. The quantitative measurement of normal passive medial and lateral patellar motion limits. Am J Sports Med, 1993; 21: 728-732. [DOI] [PubMed]
- 14).Holmes SW, Jr., Clancy WG, Jr. Clinical classification of patellofemoral pain and dysfunction. J Orthop Sports Phys Ther, 1998; 28: 299-306. [DOI] [PubMed]
- 15).Vaquero J, Vidal C, Medina E, Baena J. Arthroscopic lysis in knee arthrofibrosis. Arthroscopy, 1993; 9: 691-694. [DOI] [PubMed]
- 16).Jerosch J, Aldawoudy AM. Arthroscopic treatment of patients with moderate arthrofibrosis after total knee replacement. Knee Surg Sports Traumatol Arthrosc, 2007; 15: 71-77. [DOI] [PubMed]
- 17).Conlan T, Garth WP, Jr., Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am, 1993; 75: 682-693. [DOI] [PubMed]
- 18).Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med, 1998; 26: 59-65. [DOI] [PubMed]
- 19).Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res, 1998: 174-182. [DOI] [PubMed]
- 20).Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc, 1994; 2: 19-26. [DOI] [PubMed]
- 21).Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am, 2007; 89: 1749-1755. [DOI] [PubMed]
- 22).Fulkerson J, ed. Disorder of the patellofemoral joint. 4th ed. 2004, Lippincott Williams & Wilkins: Philadelpia.
- 23).Merican AM, Iranpour F, Amis AA. Iliotibial Band Tension Reduces Patellar Lateral Stability. J Orthop Res, 2009; 27: 335-339. [DOI] [PubMed]
- 24).Salzmann GM, Weber TS, Spang JT, Imhoff AB, Schottle PB. Comparison of native axial radiographs with axial MR imaging for determination of the trochlear morphology in patients with trochlear dysplasia. Arch Orthop Trauma Surg, 2010; 130: 335-340. [DOI] [PubMed]
- 25).Seitlinger G, Scheurecker G, Hogler R, Labey L, Innocenti B, Hofmann S. The position of the tibia tubercle in 0 degrees -90 degrees flexion: comparing patients with patella dislocation to healthy volunteers. Knee Surg Sports Traumatol Arthrosc, 2014; 22: 2396-2400. [DOI] [PubMed]
- 26).Geenen E, Molenaers G, Martens M. Patella alta in patellofemoral instability. Acta Orthop Belg, 1989; 55: 387-393. [PubMed]
- 27).Amis AA, Senavongse W, Bull AMJ. Patellofemoral kinematics during knee flexion-extension: An in vitro study. J Orthop Res, 2006; 24: 2201-2211. [DOI] [PubMed]
- 28).Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. J Orthop Sports Phys Ther, 2003; 33: 639-646. [DOI] [PubMed]
- 29).Ota S, Nakashima T, Morisaka A, Omachi T, Ida K, Kawamura M. Is latero-medial patellar mobility related to the range of motion of the knee joint after total knee arthroplasty? Man Ther, 2010; 15: 574-578. [DOI] [PubMed]