ABSTRACT
Medical facility statistics provide essential information to policymakers, administrators, academics, and practitioners in the field of health services. In Japan, the Health Statistics Office of the Director-General for Statistics and Information Policy at the Ministry of Health, Labour and Welfare is generating these statistics. Although the statistics are widely available in both Japanese and English, the methodology described in the technical reports are primarily in Japanese, and are not fully described in English. This article aimed to describe these processes for readers in the English-speaking world. The Health Statistics Office routinely conduct two surveys called the Hospital Report and the Survey of Medical Institutions. The subjects of the former are all the hospitals and clinics with long-term care beds in Japan. It comprises a Patient Questionnaire focusing on the numbers of inpatients, admissions, discharges, and outpatients in one month, and an Employee Questionnaire, which asks about the number of employees as of October 1. The Survey of Medical Institutions consists of the Dynamic Survey, which focuses on the opening and closing of facilities every month, and the Static Survey, which focuses on staff, facilities, and services as of October 1, as well as the number of inpatients as of September 30 and the total number of outpatients during September. All hospitals, clinics, and dental clinics are requested to submit the Static Survey questionnaire every three years. These surveys are useful tools for collecting essential information, as well as providing occasions to implicitly inform facilities of the movements of government policy.
Key Words: medical facility statistics; Ministry of Health, Labour and Welfare; Japan; policy making
INTRODUCTION
Medical facility statistics provide essential information for policymakers, administrators, academics, and practitioners in the field of health services. This information has accumulated in many databases worldwide, including those of the World Health Organization and Organisation for Economic Co-operation and Development.1,2) While developed countries have their own established systems of collecting such data, developing countries must develop their own systems to fit the infrastructure of their countries, in an inexpensive and reasonably accurate way that is linkable to current policymaking. Therefore, a description of the processes involved in collecting information from medical facilities might be useful for developing countries.
In Japan, the Health Statistics Office of the Director-General for Statistics and Information Policy at the Ministry of Health, Labour and Welfare (MHLW) is in charge of generating health facility statistics. Although the findings are available widely in both Japanese and English,3-5) the processes described in related technical reports by the government are all in Japanese; they are only rarely given in English. In addition, the Japanese documents are usually written in bureaucratic ways, meaning that the directly translated English manuscripts might be of limited use.
This article aimed to describe the processes involved in the government’s collection of information from medical facilities in Japan. The following descriptions are based mainly on Japanese government documents. The article also provides an explanation of the roles and limitations of the reported statistics as a reference for readers in the English-speaking world.
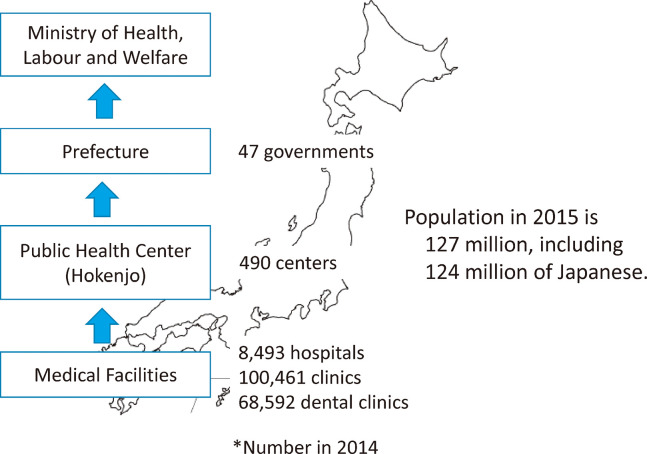
Japan conducts two surveys—the Hospital Report (Byouin Houkoku) and Survey of Medical Institutions (Iryoushisetsu Chousa). These questionnaires are sent from the medical facilities via the public health center (a local government authority, hokenjo in Japanese6,7)) to the MHLW (Fig. 1). Per the Medical Care Act (No. 205 of July 30, 1948) of Japan, Articles 1–5 define “hospital” as “a facility for the hospitalization of not less than 20 patients” and “clinic” as “a facility for the hospitalization of no more than 19 patients.” Following the Second World War, Japan had limited medical facilities, forcing rural medical facilities to provide inpatient services on a small scale, along with outpatient services. For regulation purposes, medical facilities with less than 20 beds were classified as “clinics.” Although these definitions might cause confusion among non-Japanese readers, the terms are used in this way throughout this article. As of 2014, 8,355 clinics out of 100,461 provided inpatient services. Inpatient beds in these clinics are further divided into long-term care beds and other beds.
Fig. 1.
Route of medical facility statistics reporting.
HOSPITAL REPORT
The subjects of this survey were all hospitals (8,493 in 2014) and clinics with long-term care beds (1,125 clinics in 2014). It consists of the Patient Questionnaire (Kanja Hyo) and Employee Questionnaire (Jujisha Hyo). At present, there are no English versions of these questionnaires.
Patient questionnaire
This is a one-sheet report to be submitted monthly by the facility director to the government. The questionnaire includes questions on 1) the number of outpatient visits, 2) inpatient-days, 3) number of inpatients on the last day of the month, 4) number of admitted patients, and 5) number of discharged patients. For questions 2) to 5), facilities must specify the numbers for each of 5 ward categories (wards specific to psychiatric diseases, tuberculosis, other infectious diseases defined by Infectious Disease Act, and long-term care, and general wards for other miscellaneous diseases). Medical facilities with a computer system can create and submit this report automatically. From these data, the government can calculate the volumes of patients according to ward category.
One of the most important indices derived from this questionnaire is the average length-of-stay of inpatients. This is calculated for a given period using the following formula: (total inpatient days) / {0.5 × (admitted patients + discharged inpatients)}. When performing comparisons among regions or countries, one year is usually applied as the period for calculating the average length-of-stay.8) For health insurance claims in Japan, a three-month average length-of-stay is used to determine the level of fees for inpatient care.9)
Employee questionnaire
This is also a one-sheet report submitted through the same route to the government as the Patient Questionnaire. In this sheet, facilities must report the number of the employees as of October 1. Employees are classified into 31 categories, as shown in Table 1. For doctors and dentists, the questionnaire asks for the numbers of full-time personnel as well as the number of part-time personnel converted to full-time personnel. For pharmacists, public health nurses, midwives, nurses, and assistant nurses, the questionnaire asks about the total number of full-time and part-time personnel, as well as the number of converted full-time personnel. For all other types of personnel, only the converted numbers are asked about.
Table 1.
Employee categories in the Employee Questionnaire of the Hospital Report, governmental licensing, and number of personnel in each category (calculated from the Employee Questionnaire, Clinic Questionnaire, and Dental Clinic Questionnaire of the Static Survey of Medical Institutions) as of October 1, 2014.
| Category | License1 | Number2 | |
| 1. | Doctor | National | 340,964 |
| 2. | Dentist | National | 108,465 |
| 3. | Pharmacist | National | 51,999 |
| 4. | Public health nurse | National | 12,257 |
| 5. | Midwife | National | 29,072 |
| 6. | Nurse | National | 878,933 |
| 7. | Assistant nurse | Prefectural | 222,491 |
| 8. | Nurse assistant | No | 218,873 |
| 9. | Physical therapist | National | 77,140 |
| 10. | Occupational therapist | National | 42,136 |
| 11. | Orthoptist | National | 7,733 |
| 12. | Speech-language-hearing therapist | National | 14,252 |
| 13. | Artificial limb fitter | National | 104 |
| 14. | Dental hygienist | National | 107,924 |
| 15. | Dental technician | National | 11,445 |
| 16. | Clinical radiology technician | National | 50,960 |
| 17. | Clinical X-ray technician | Repealed3 | 1,355 |
| 18. | Clinical laboratory technician | National | 64,080 |
| 19. | Hygienic laboratory technician | Repealed4 | 330 |
| 20. | Clinical engineer | National | 23,741 |
| 21. | Masseur | National | 4,594 |
| 22. | Judo therapist | National | 4,172 |
| 23. | Registered dietitian nutritionist | National | 25,233 |
| 24. | Nutritionist | National | 6,854 |
| 25. | Psychiatric social worker | National | 10,505 |
| 26. | Certified social worker | National | 10,582 |
| 27. | Certified care worker | National | 57,773 |
| 28. | Other technician | No | 23,581 |
| 29. | Welfare worker | No | 10,619 |
| 30. | Clerical worker | No | 418,006 |
| 31. | Others (janitor, driver, etc.) | No | 131,958 |
1Licenses for medical professions administered by the Ministry of Health, Labour and Welfare or prefectural governments.
2 Equivalent to full-time employees.
3 in 1983.
4 in 2011.
Facilities must also report the number of employees in the Clinic Questionnaire and Dental Clinic Questionnaire of the Static Survey of Medical Institutions. The total numbers of employees according to their professions (listed in Table 1) are calculated using information from all three questionnaires. They are available at http://www.mhlw.go.jp/toukei/saikin/hw/iryosd/14/dl/1-4.pdf as of August 19, 2017.
Note that the artificial limb fitter and judo therapist (bonesetter) are professionals potentially unique to Japan. Furthermore, the registered dietitian nutritionist is considered a higher position compared to the nutritionist. Although acupuncturists (108,537 in 2014) and moxa-cauterizers (106,642 in 2014) are professionals licensed by the MHLW, they are not included in this questionnaire, as they rarely work at a hospital or clinic. Instead, they tend to open their own offices with the permission of the government.
SURVEY OF MEDICAL INSTITUTIONS
This survey comprises the Dynamic Survey, which focuses on the opening and closing of facilities, and the Static Survey, which focuses on staff, facilities, and services as of October 1; the number of inpatients as of September 30; and the total number of outpatients in September. All hospitals, clinics, and dental clinics are subjects of this survey.
Dynamic Survey of Medical Institutions (Iryoushisetsu Doutai Chousa)
Those who request permission to open or close a medical facility must submit the necessary documents to the local government where the facility is located. The Dynamic Survey form is one of these documents. It includes the name and address of the facility, the category of the founder (e.g., nation, local government, cooperation, or private), names of clinical departments, number and category of inpatient beds, number of medical professionals (including doctors, dentists, pharmacists, nurses, assistant nurses, and dental hygienists), and the applicability of health insurance. Based on these documents, prefectural governments report the number of opened/closed facilities to the MHLW every month.
Static Survey of Medical Institutions (Iryoushisetsu Seitai Chousa)
Medical facilities must submit the Static Survey, a self-administered questionnaire, every three years. There are three versions of this questionnaire: Hospital Questionnaire, Clinic Questionnaire, and Dental Clinic Questionnaire. The English version of the Static Survey in 2008 is available at http://www.mhlw.go.jp/english/database/db-hss/mi.html.
The Japanese version of the Hospital Questionnaire in 2014 was a 4-page questionnaire. The questions are listed in Table 2. Questions 7, 16, and 26 were not included in the 2008 version; however, the 2008 questionnaire did contain an additional question on whether a regular clinical pathological conference was held (yes or no).
Table 2.
Questions of the Hospital Questionnaire from the Static Survey of Medical Institutions, 2014.
| Question | |
|---|---|
| 1. | Address of institution |
| 2. | Name of institution |
| 3. | Not practicing (suspended, not in practice for a year or longer, or not in practice for less than one year) |
| 4. | Category of founder (27 categories) |
| 5. | Sanctioned inpatient beds by ward category1 |
| 6. | Applicability of health insurance (yes/no) |
| 7. | Notice of emergency services to the public (yes/no) |
| 8. | Clinical specialty (43 categories such as internal medicine, surgery, etc.) |
| 9. | Total number of outpatients in September and inpatients on September 30 for the above 43 categories |
| 10. | Number of male and female doctors converted into full-time personnel for the above 43 categories |
| 11. | Number of first-visit patients and patients out of office hours in September |
| 12. | Number of prescriptions in September |
| 13. | Number of medical doctor residents as of October 1 |
| 14. | Number of personnel working for discharge support as of October 1 |
| 15. | Number of personnel assisting doctors with clerical jobs as of October 1 |
| 16. | Number of personnel working in childcare in ward as of October 1 |
| 17. | Level of emergency care (primary, secondary, tertiary, or no services) |
| 18. | Smoking cessation treatment and obstetric services by midwife (yes/no) |
| 19. | Outsourcing (i.e., meals, disinfection, maintenance of medical equipment, laboratory tests, maintenance of medical gases, cleaning, patient transfer) |
| 20. | Displayed office hours |
| 21. | Measures against passive smoking |
| 22. | Nursery for employees |
| 23. | Electronic ordering system (yes/no) |
| 24. | Medical image management system (Picture Archiving and Communication System) |
| 25. | Electric medical chart |
| 26. | Storage and usage of electric data |
| 27. | Telemedicine/remote medical support system |
| 28. | Patient safety: general, infectious disease control, equipment, and drugs |
| 29. | Provision of home care services |
| 30. | Special medical care utilities: ICU, SCU, MFICU, sterilized room, radiotherapy room, outpatient chemotherapy room, NICU, GCU, PICU, and negative pressure room |
| 31. | Numbers of beds in palliative care ward and number of patients treated by palliative care team |
| 32. | Number of patients that received specific tests (bone mineral quantification, bronchial endoscopy, upper gastrointestinal endoscopy, colonoscopy, serial angiography, mammography, scintigraphy, PET, CT, MRI, and 3D-image processing) |
| 33. | Number of surgical operations (17 categories), including childbirth (yes/no) with number of doctors and midwives, and whether there is an in-hospital midwifery center (yes/no) |
| 34. | Number of patients and equipment for radiotherapy |
| 35. | Dental equipment |
| 36. | Numbers of autopsies and patients who died in September |
| 37. | Training program for newly employed nurses |
| 38. | Shift-work and number of ward nurses according to ward category1 |
1 Wards for psychiatric diseases, tuberculosis, other infectious diseases, long-term care, and others.
The Clinic Questionnaire in 2014 was also a 4-page questionnaire. Questions 13, 15, 16, 22, 23, 24, 30, 31, 36, 37, and 38 of the Hospital Questionnaire (see Table 2) were not included in 2014 Clinic Questionnaire, whereas the following questions were included: main clinical specialty, using the same 43 categories as those of the Hospital Questionnaire; main services (consisting of 9 categories, e.g., general practice, consultation, blood sampling and provision, health checkup, hemodialysis); practices at a limited period (e.g., a clinic to open at ski season); a specific computer for making health insurance claims; registration as a home care supporting clinic; number of employees in the same form as the Employee Questionnaire of the Hospital Report; and number of childcare staff (there were a total of 1,080 full-time converted persons as of October 1, 2014). In addition, the 2014 survey asked about internet availability because the government was preparing to introduce a computer reporting system for the Survey of Medical Institutions.
The Dental Clinic Questionnaire in 2014 was a 2-page questionnaire that contained the items listed in Table 3. Since dental clinics are not included as subjects of the Hospital Report, this questionnaire asks about the number of employees in 10 specific dental professions. In 2014, there were a total of be 72,419 dental practice assistants (based on converted full-time employees). The 2014 survey also asked about internet availability.
Table 3.
Questions in Dental Clinic Questionnaire of Static Survey of Medical Institution, 2014.
| Question | |
|---|---|
| 1. | Address of institution |
| 2. | Name of institution |
| 3. | Not practicing (suspended, not in practice for a year longer, or not in practice for less than one year) |
| 4. | Category of founder (26 categories) |
| 5. | Sanctioned inpatient beds |
| 6. | Applicability of health insurance (yes/no) |
| 7. | Category of services (dental, orthodontic, pediatric, and/or dental surgery) |
| 8. | Total number of patients in September |
| 9. | Total number of prescriptions in September, and number of male and female doctors converted into full time-personnel according to the above 43 categories |
| 10. | Community services |
| 11. | Emergency service |
| 12. | Office hours |
| 13. | Location where dental materials are made (domestic or abroad) |
| 14. | Measures against passive smoking |
| 15. | Computer availability for insurance claims |
| 16. | Availability of electric medical charts |
| 17. | Patient safety management |
| 18. | Dental/X-ray equipment |
| 19. | Room for dental materials (yes/no) |
| 20. | Implants |
| 21. | Possession of dental amalgam |
| 22. | Home services |
| 23. | Number of employees (full-time and part-time converted to full-time) according to their profession (dentist, doctor, dental hygienist, dental technician, pharmacist, nurse, assistant nurse, dental practice assistant, clerical worker, and others) as of October 1 |
MEDICAL CARE PLAN (IRYOU KEIKAKU)
The information on medical facilities obtained from the above surveys are essential for many fields, such as infectious disease control; maternal and child health; health services for the elderly, the disabled, and those with psychiatric diseases; and rural health. An example illustrating the necessity of this information can be found in the Medical Care Plan (MCP) stated in the Medical Care Act.
The MCP is devised by prefectural governments based on the conditions of each prefecture, according to MHLW policy. The MCP was introduced in 1985, and has developed along with the amendments to the Medical Care Act. The items that must be described in the MCP are outlined by the MHLW;10,11) the items stipulated in 2014 are listed in Table 4. Among these items, those pertaining to the Vision on Regional Medical Services (Chiiki Iryou Kousou) were newly added as items 7 and 8. These items focus on the (1) estimation of demands for medical services and inpatient beds in the year 2025, according to the type of general wards (explained below), and (2) strategies to develop systems that can supply the necessary amount of services to fit this estimation.
Table 4.
Items to be described in the Medical Care Plan according to the instructions of the Ministry of Health, Labour and Welfare in 2014.
| Item | |
|---|---|
| 1. | Treatment and prevention of five diseases (cancer, apoplexy, acute myocardial infarction, diabetes mellitus, and psychiatric disease) |
| 2. | Supply of the following medical services |
| a) Emergency services | |
| b) Services at disaster | |
| c) Rural services | |
| d) Perinatal services | |
| e) Pediatric services including child emergency care | |
| f) Services that the governor judges as necessary based on incidence of disease | |
| 3. | Goals of the items 1 and 2 |
| 4. | Networks among medical facilities to realize items 1 and 2; roles of each facility and rules for assuring the networks |
| 5. | Promotion of information provision on facilities’ roles in the network |
| 6. | Assurance of medical services at patients’ homes and under similar situations |
| 7. | Vision on Regional Medical Services |
| a) Number of inpatient beds necessary in the future according to their type1 | |
| b) Amount of services for home care and similar situations necessary in the future | |
| 8. | Promotion of networks and specialization for a defined ward type, aiming to achieve the Vision on Regional Medical Services |
| 9. | Promotion of information provision by ward type1 |
| 10. | Assurance to employ the necessary numbers of doctors, dentists, pharmacists, nurses, and other medical professionals |
| 11. | Assurance of patients’ safety |
| 12. | Appropriate location of medical facilities that considers the roles of each facility, including hospitals that support regional medical services |
| 13. | Determination of second medical service areas2 |
| 14. | Determination of tertiary medical service areas3 |
| 15. | Standard inpatient beds |
| 16. | Matters necessary to assure medical service provision |
1 Types are for inpatients, and are classified into advanced acute stage, acute stage, recovery stage, and chronic stage.
2 The areas for secondary medical services provision.
3 The areas made for tertiary medical services provision.
To realize the Vision on Regional Medical Services,12) prefectural governments request that medical facilities specify and report on each type of general ward (classified as highly acute stage, acute stage, recovery stage, and chronic stage). This reporting system is called the Ward Role Report (Byoushou Kinou Houkoku Seido)13)
COMMENTS
Although there are documents in Japanese describing the methods and process used to collect medical facility statistics in Japan, few are available in English. The findings obtained from government surveys are available on the MHLW English homepage (http://www.mhlw.go.jp/english/), including the Handbook of Health and Welfare Statistics, but these are mainly in the form of Tables4) and do not explain the processes in data collection. Even a simple translation of this information from Japanese to English can be difficult for Japanese authorities. In particular, they do not have sufficient personnel to complete this task. In addition, since these documents are written for those with an understanding of the Japanese medical system, the exact contents of directly translated documents can be difficult for foreign readers to understand. Accordingly, articles providing additional explanation of the background and relevant comments are necessary to translate this information to the foreign professionals in this field. This is the reason for the present article.
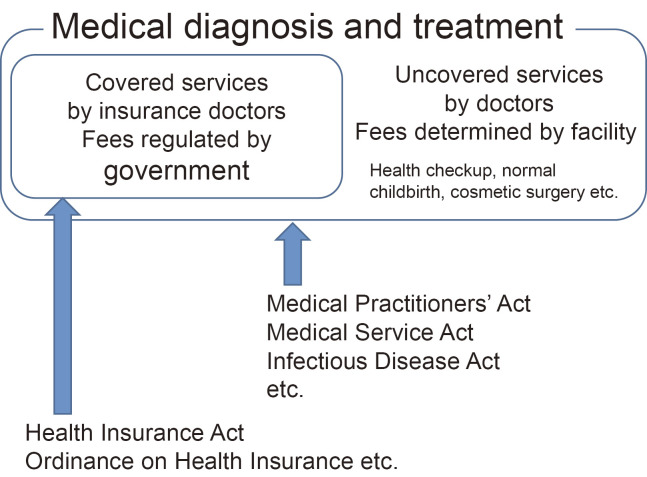
Japanese health care systems are largely based on the health insurance system.14,15) With a few exceptions, all facilities participate in health insurance (Fig. 2). There are various laws, ordinances, and operational rules concerning health insurance, such as the Health Insurance Act and Ordinance on Health Insurance. Since the fees claimed for the health insurance funds are based on the structure (e.g., ratio of nurses to inpatients, presence of an infection control committee, special units such as intensive care units) and processes (e.g., issuing receipt of out-of-pocket payment and note on items for payment, written schedules for admission services, extra charges for inpatient rooms) in the facility, the information must be submitted to a special committee, who examines the appropriateness of the claims. In addition, there are authorities affiliated with the MHLW that investigate misconduct made in these claims for insurance funds. Inconsistencies in medical facility statistics and health insurance claims can be easily detected by the local authority. Therefore, the accuracy of medical facility statistics is partly guaranteed by the processing of insurance fee claims.
Fig. 2.
Medical services covered and uncovered by health insurance in Japan.
The Health Statistics Office of the Director-General for Statistics and Information Policy at the MHLW is also conducting surveys on patients and medical professionals. Both these surveys complement the information provided by the medical facility statistics. The Patient Survey (Kanja Chousa) is conducted every three years at the same time as the Survey of Medical Institutions, collecting information on patients such as sex, birth date, address, source of payment (solely out-of-pocket, health insurance, long-term insurance, or public fund), diagnosis, and admitted wards. The Survey of Physicians, Dentists, and Pharmacists (Ishi Shikaishi Yakuzaishi Chousa) is a biannual survey aiming to obtain data on the jobs of these three professions at the end of the year. Each professional has his or her own registered identification number, and is given follow up surveys until his or her death. The questionnaire asks about name, address, birthday, registered identification number, type of job (e.g., clinical practice, administration, education, research, no job), and name of workplace, if any. By contrast, the Employee Questionnaire does not include any information that can be used to identify individuals, and targets only professionals working at medical facilities.
The Hospital Report and Survey of Medical Institutions appear to have several roles. Their original role was to routinely collect basic information on the quantity, distribution, capacity, and technology level of medical facilities. This information is essential for comparisons among different regions and countries. Through these comparisons, the appropriate amount and quality of medical service supply can be realized and examined. These surveys also provide occasions to collect additional information necessary for policymaking related to current problems, such as hepatitis B and C virus infection among those with hepatic diseases (chronic hepatitis, cirrhosis, and liver cancer) and the necessity of networking through the computerization of medical facilities in Japan. Through these surveys, facility directors can implicitly realize the requested standard of their facilities and any new movements in government regulations, allowing them time for preparation in order to survive in Japan’s competitive health care market. In this way, the surveys can facilitate the improvement of medical services.
The limitations of these surveys are as follows. First, they are all based on self-administered questionnaires, rather than actual inspection. However, the responses seem accurate because the questionnaires must be submitted to the local government that has jurisdiction over the facilities. Second, the number of questions in each survey is restricted to reduce burden on the facilities. Only information necessary for the monitoring, evaluation, and planning of government policies is collected. Third, these surveys mainly request summary data. The methods/definitions of these summary data might be slightly different among the facilities, and might include errors, but the effects can be limited.
CONCLUSION
This article described the processes used for obtaining medical facility statistics in Japan. These statistics are mainly based on the Hospital Report and Survey of Medical Institutions. Besides collecting routine basic information, these surveys obtain information related to current policymaking. Thus, they are a useful tool not only to collect essential information, but also to provide occasions to implicitly inform facilities of the future movements of the government.
ACKNOWLEDGMENTS
N.H. was a short-term specialist of the Japan International Cooperation Agency (JICA) in 2017, who was dispatched to the Republic of the Union of Myanmar. This article was created during the preparation of seminars for officers of the Departments of Medical Services and Public Health, Ministry of Health and Sports, Myanmar in March and July 2017.
COMPETING INTERESTS
The authors declare that no competing interests exist.
REFERENCES
- 1).World Health Organization. Global health observatory (GHO) data. http://www.who.int/gho/database/en/. Accessed on September 9, 2017.
- 2).OECD Health Statistics 2017. http://www.oecd.org/els/health-systems/health-data.htm. Accessed on September 9, 2017.
- 3).Anonymous. Medical facility. In: Kokumin Eisei no Dokou. Kosei no Shihyo, Vol.63 No.9. pp.221-227, 2016, Health, Labour and Welfare Statistical Association, Tokyo (in Japanese).
- 4).Director-General for Statistics and Information Policy, Ministry of Health, Labour and Welfare. Part 1 Population and households Chapter 2 Healthcare. In: Handbook of Health and Welfare Statistics 2015. 2016, Health, Labour and Welfare Statistics Association, Tokyo.
- 5).Tatara K, Okamoto E. 5 Physical and human resources. In: Health Systems in Transition, Japan: Health system review, edited by Allin S, Matsuda R. pp.83-94, 2009, WHO Regional Office for Europe, Copenhagen.
- 6).Katsuda N, Hinohara Y, Tomita K, Hamajima N. Structure and roles of public health centers (hokenjo) in Japan. Nagoya J Med Sci, 2011; 73: 59-68. [PMC free article] [PubMed]
- 7).Katsuda N, Hirosawa T, Reyer JA, Hamajima N. Roles of public health centers (hokenjo) in tuberculosis control in Japan. Nagoya J Med Sci, 2015; 77: 19-28. [PMC free article] [PubMed]
- 8).Hashimoto H, Ikegami N, Shibuya K, Izumida N, Noguchi H, Yasunaga H, et al Cost containment and quality of care in Japan: is there a trade-off? Lancet, 2011; 378: 1174-1182. [DOI] [PubMed]
- 9).Iwasaki M. Chapter 3 Admission. In: Rule and Base of Medical Service Payment. pp.117-196, 2016, Medica Publication Inc., Osaka (in Japanese).
- 10).Director General of Health Policy Bureau, Ministry of Health, Labour and Welfare. Medical care plan. Health Policy Bureau 0331-57, March 31, 2017. Ministry of Health, Labour and Welfare, Tokyo (in Japanese).
- 11).Takayama Y, Matsushita K. Technical assistance to prefectural governments to promote effective use of health data: A data manual for development of community health care plans and the PDCA. J Natl Inst Public Health, 2014; 63: 512-521.
- 12).Committee for Guideline on Drafting Vision on Regional Medical Services. Guideline on Drafting Vision on Regional Medical Services. 2015, Ministry of Health, Labour and Welfare, Tokyo (in Japanese).
- 13).Ministry of Health, Labour and Welfare. Manual of Ward Role Report. 2016, Ministry of Health, Labour and Welfare, Tokyo (in Japanese).
- 14).Ikegami N, Yoo B-K, Hashimoto H, Matsumoto M, Ogata H, Babazone A, et al Japanese universal health coverage: evolution, achievement, and challenges. Lancet, 2011; 378: 1106-1115. [DOI] [PubMed]
- 15).Ikegami N, Anderson GE. In Japan, all-payer rate setting under tight government control has proved to be an effective approach to containing costs. Health Aff (Millwood), 2012; 31: 1049-1056. [DOI] [PubMed]