Abstract
Objective
To measure the value the patients place on different aspects of person-centred care.
Design
We systematically identified four attributes of person-centred care. We then measured their value to 923 people with either chronic pain or chronic lung disease over three discrete choice experiments (DCEs) about services to support self-management. We calculated the value of each attribute for all respondents and identified groups of people with similar preferences using latent class modelling.
Setting
DCEs conducted online via a commercial survey company.
Participants
Adults with either chronic pain (two DCEs, n=517 and 206, respectively) or breathlessness due to chronic respiratory disease (n=200).
Results
Participants were more likely to choose services with higher level person-centred attributes. They most valued services that took account of a person’s current situation likelihood of selection increased by 16.9% (95% CI=15.4 to 18.3) and worked with the person on what they wanted to get from life (15.8%; 14.5 to 17.1). More personally relevant information was valued less than these (12.3%; 11.0 to 13.6). A friendly and personal communicative style was valued least (3.8%; 2.7 to 4.8). Latent class models indicated that a substantial minority of participants valued personally relevant information over the other attributes.
Conclusion
This is the first study to measure the value patients place on different aspects of person-centred care. Professional training needs to emphasise the substance of clinical communication—working responsively with individuals on what matters to them—as well as the style of its delivery.
Keywords: Quality in health care, Self management, person centred care, patient centered care, discrete choice experiment
Strengths and limitations of this study.
This is the first study to quantify the value which patients place on different aspects of person-centredness.
Person-centred care is a complex concept: we designed the attributes for the discrete choice experiments (DCEs) using a rigorous process involving both theoretical and empirical work followed by two cycles of development and testing.
Despite this, the study was limited to four attributes of person-centredness which inevitably cannot encompass the full richness of this concept.
We conducted three experiments, each with a version of the same core DCE, to reduce the risk that our results were biased by our choice of methods or population and to increase generalisability.
The experiments were sufficiently powered to identify and characterise sub-groups of patients with similar patterns of values.
Introduction
Person-centred care is key to high-quality healthcare.1 Person-centred care, along with its near-synonym patient-centred care, is a complex concept that has been analysed and operationalised in a number of overlapping ways for different contexts and purposes.1–7 One widely used definition summarises it as ‘respectful and responsive to individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions’.4 More theoretical analyses start from a consideration of patients as persons and what this means for how health services and staff should (ethically) relate to them.2 5 Although they use a variety of terms, they tend to emphasise the importance of recognising and taking into account each patients’ subjective experiences of health problems and healthcare, including how these fit into their personal biography or narrative and impact their self-identity; working with sensitivity to each patient’s particular situation, including their social relationships and material circumstances; and respecting and relating to each patient as a moral agent, for example, by sharing decision-making rather than imposing decisions about potential healthcare interventions.2–7
From a patient’s perspective, person-centred care can depend, among other things, on practitioners adopting an appropriate communication style, providing personally relevant information, taking appropriate account of their personal circumstances and working with them on what matters to them (or what they want to get from life).8 9 Of these, communication style is perhaps most often addressed in health professional training, although an emphasis on communication skills rather than deeper interpersonal attitudes and value commitments has been criticised.10 11 No studies have quantified how much different aspects of person-centred care matter to patients.
Alongside the emphasis on person-centred care, there is a drive to support people with long-term conditions to ‘self-manage’.12 13 Recent critiques of health services’ support for self-management have suggested that it is often delivered in ways that fall short of aspirations for person-centred care.14 First, services often rely on a ‘one-size-fits-all’ approach, although people have diverse capabilities and needs for support.15 Second, interventions and approaches are often influenced by professionals’ biomedical perspectives16 rather than what people value for living well with their conditions.16 Third, although much self-management support focuses on providing individuals with knowledge, skills and motivation, the barriers to effective self-management commonly lie in people’s broader social and material environments.17–20 Support for self-management, thus, provides an important context for the study of person-centred care.
We aimed to measure what matters to patients in relation to person-centred care by conducting a series of discrete choice experiments (DCEs) about services to support self-management for people with long-term conditions. We hypothesised that individuals would vary in how much they valued different aspects or person-centred care but did not specify a magnitude of difference or specify that any particular attribute would be consistently more highly valued.
Methods
DCEs enable researchers to measure individuals’ preferences by calculating the value they place on particular attributes.21 They involve participants completing a set of hypothetical choice tasks, each of which involves choosing between two or more alternatives. The alternatives are described in terms of multiple attributes, with levels which are systematically varied across the choice tasks. Participants’ responses are analysed to measure the influence of the different levels of attributes on choices.
We designed and used DCEs in three linked studies, two among people with chronic pain and one among people with breathlessness due to chronic respiratory disease. Both conditions are common and directly affect individuals through current symptoms. Self-management of these conditions requires adaptation to the limitations caused by the condition,16 but does not include technical tasks such as monitoring blood tests or treatment. Each of the three DCEs used the same attribute levels and set of choice tasks, with minor contextual changes to the wording. The second chronic pain DCE was similar to the first except that we excluded any reference to the cost of a service, to avoid potential bias of results due to cost.
Development of the DCE
DCEs typically include attributes and levels which describe the process of care, and are easily defined (eg, consulting a doctor versus seeing a nurse) or easily quantified (eg, waiting for different lengths of times). In this study, we sought to value attributes which describe the nature of care—its person-centredness—which is less easily defined in single statements or which may be interpreted in different ways.22 To address this challenge and ensure that the DCE was valid and reliable, we followed best practice to design, develop and test the DCE through three stages: attribute selection, attribute testing and development and pilot survey. To do this, we drew on recent theoretical15 and empirical research,8 and conducted focus group discussions and think-aloud interviews23 in which participants talked through their responses to draft versions of the DCE. As there were far more possible combinations of attributes and levels than we could test, we designed the DCE to provide maximal statistical efficiency for a manageable length of questionnaire by applying D-efficient design with a Bayesian approach.24 This involved conducting a preliminary DCE with 117 participants in order to develop a ‘well-informed’ experimental design for the main study.
Attribute selection
We began the process of attribute selection from three starting points. First was the idea that the overall aim of support for self-management is to enable people ‘to live well with long-term conditions’.15 Second, we used the notion that person-centredness is primarily a matter of treating everyone ‘as a person’.2 Treating someone as a person includes recognising and responding to their individual characteristics and preferences. It also includes respecting them as a fellow human, recognition of their unique biography and identity and support their autonomy to shape and live their lives according to their own values rather than those of others. Third, we used a conceptual map of what matters to patients about how healthcare is delivered,8 which considers items in three categories: ‘what health services are like and do’, ‘how they relate to me’ and ‘what they enable me to do’.
We explored these, and other, ideas around person-centredness in relation to support for self-management in six focus groups, each comprising between five and seven individuals. Three groups involved people with chronic pain (members of two peer support groups and individuals recruited through a pain clinic), two groups involved non-clinical providers of support for self-management of long-term conditions and one group came from a multidisciplinary pain team (to provide professional triangulation of the patient perspective). Groups lasted between 40 and 65 min and began by open discussion, following a topic guide, about ways in which support for self-management may be made personal. Later in the groups, we presented six provisional attributes of person-centredness, each with two or three levels for discussion. Focus groups were audio-recorded, transcribed and analysed thematically. In conducting and analysing the focus groups, we did not aim for exhaustive recruitment or in-depth qualitative analysis. Rather the focus groups were used as sources of contextual and confirmatory (or disconfirming) data to be used—alongside our own and others’ conceptual work and empirical evidence—in developing the attributes and levels of the DCE.
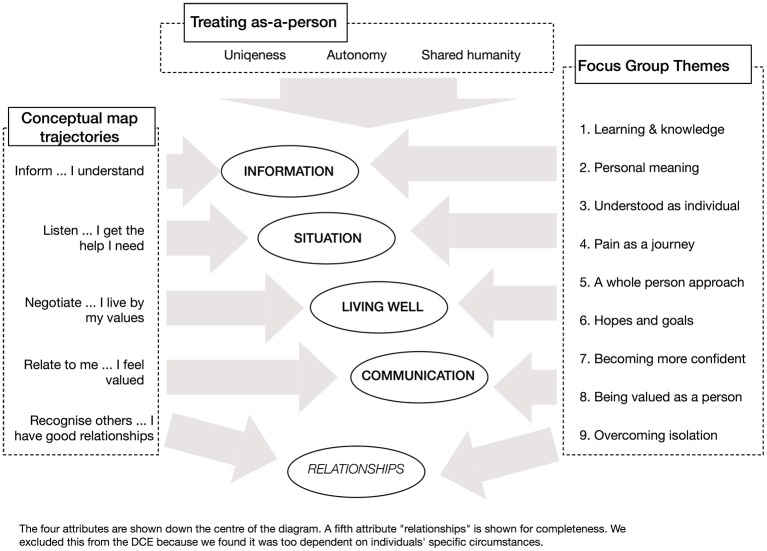
In the attribute selection phase, we recognised that the data from these different sources overlapped in various ways. For the DCE design, however, we needed a manageable number of well-differentiated (ideally potentially independent) attributes that described (aspects of) person-centredness from a patient’s perspective. We chose to focus on four aspects of person-centredness, summarised as information, situation, living well and communicative style. A simplified view of the relationship between these aspects and the developmental sources is shown in figure 1.
Figure 1.
Simplified illustration of mapping of different sources to final attributes. DCE, discrete choice experiment.
Attribute development and testing
We carried out two cycles of development and testing of attributes and their associated levels. Each cycle comprised three stages: drafting of attribute-level statements, cognitive testing of these statements using think-aloud interviews23 and evaluation of the think-aloud results. Statements were drafted and revised by all members of the research team in order that they would be broadly applicable and easily and consistently understood. We conducted think-aloud interviews with a total of 17 people with chronic pain, 6 of whom had participated in the focus groups; 10 took part in the first cycle and 7 in the second cycle. During the think-aloud interviews, participants completed a paper-based version of the DCE using the current attributes and were asked to describe their thoughts about the attributes and levels, and their decisions, as they did so. Think-aloud interviews were audio-recorded, transcribed and analysed to identify areas for clarification. Evaluation at the end of the first cycle led to revision of attribute-level statements to be used in the second cycle. In particular, we found that respondents experienced problems when three levels were assigned to each attribute. If these were neutral, high and very high, some people found the very high level excessive, and there was some variation in how people interpreted which of the two higher levels was better. However, if the levels were low (ie, actively not person-centred), neutral and high, people made choices to avoid the low rather choose between the two higher attributes. As we were interested in how people positively valued more person-centred care, rather than their negative valuing of impersonal care, we limited the levels for each attribute to two, designed to represent: neutral and high person-centredness.
Final attribute wording
The four final person-centredness attributes and their levels are listed in table 1. The attributes were presented in relation to services to support self-management for chronic pain (DCEs 1 and 3) and chronic lung disease (DCE 2). In addition to the four person-centredness attributes, we also included a cost attribute in DCEs 1 and 2, presented as the cost per week for a 6 week programme. This had four levels ranging from £5 to £20 per week. We included the cost attribute in order to be able to estimate willingness to pay, a monetary measure of benefit. To address a concern that the inclusion of cost might bias the results, (in the UK the NHS does not charge patients for treatment at the point of consumption) we modified the design in our third DCE to exclude the cost attribute; this allowed us to compare responses with and without a cost attribute.
Table 1.
Attributes and levels for the discrete choice experiments (DCEs)
| Attribute label | Attribute description | Attribute levels |
| Information | By ‘information’ we mean information about pain,* the conditions that cause it, and the different ways there are of managing it | Provides everyone with the same information (NEUTRAL) Provides information that is relevant to you (HIGH) |
| Situation | By ‘current situation’, we mean things like where you live, who you live with, what resources you have, what you usually do for yourself and others, and how pain* currently affects that | Takes little account of your current situation (NEUTRAL) Makes suggestions that fit your current situation (HIGH) |
| Living well | By ‘what you want to get from life’, we mean the things that really matter to you, especially the kinds of things that you would like to achieve or to spend more time doing, and the kind of person that you want to be | Seems to think that everyone wants to get the same from life (NEUTRAL) Works with you on what you want to get from life (HIGH) |
| Communication | By ‘communication’, we mean the way that the support service might communicate with you | Communicates with you in a neutral professional way (NEUTRAL) Communicates with you in a friendly and personal way (HIGH) |
| Cost | Please assume that each support service will be provided once a week for 6 weeks | Costs £5 per week Costs £10 per week Costs £15 per week Costs £20 per week |
*Or breathlessness, depending on sample.
Content of the DCEs
The DCEs included 12 choice tasks per participant. Each choice task involved choosing between three service specifications with different attribute-level sets. The attributes and their levels are summarised in table 1 and an example of one choice task is displayed in online supplementary figure 1. Participants first selected their least preferred option and then selected their most preferred option—a best-worst scaling type 3 approach.25 The questionnaire also included questions about age, gender, domestic status, education, household income and self-rated overall health. Severity of chronic pain was assessed using the Chronic Pain Grade,26 and severity of chronic lung disease was assessed using the clinical chronic obstructive pulmonary disease (COPD) questionnaire.27
bmjopen-2016-015689supp003.jpg (2MB, jpg)
Participants and delivery of the DCEs
The DCEs and accompanying questions were delivered online through the research company Research Now. Participants were UK-based members of the company’s online panel who were aged ≥16 years, who had one or more self-reported conditions associated with chronic pain (eg, osteoarthritis and fibromyalgia) or breathlessness (eg, asthma and COPD) and whose response to screening questions indicated current pain or breathlessness. For chronic pain, the screening required affirmative responses to two questions based on an international definition of chronic pain28 : ‘Are you currently troubled by pain or discomfort, either all the time or on and off?’ and ‘Have you had this pain or discomfort for more than three months?’. For breathlessness, we required a score of two or more using the Royal College of Physicians 3-item questionnaire for asthma,29 which indicates respiratory symptoms most days with an impact on either activity or sleep. Each DCE was made available by the research company until the target number of eligible participants had completed it. The DCEs were conducted between May and August 2015.
Tests of data quality
We analysed the risk of individuals submitting low-quality data in three ways: serial non-participation, dominance and response time; these are detailed in the online supplementary methods. The primary analysis for each of the three DCEs included data from all participants; however, we also conducted a sensitivity analysis in which participants who failed two or more data quality tests were excluded.
bmjopen-2016-015689supp001.pdf (23.6KB, pdf)
Data analysis
Value of person-centredness attributes
We estimated the effects of higher person-centredness of each attribute on participants’ choices using logistic regression with a multinomial logit (MNL) model. For each attribute, we reported the direct choice elasticity (the absolute change in the probability of a service being chosen when the attribute was switched from a ‘neutral’ to ‘high’ level of person-centredness). The analysis was conducted separately for each DCE.
Patterns of similar value of person-centredness attributes
We explored patterns of preference using a latent class MNL(LC-MNL) model30 to produce a set of classes, each representing one pattern of valuation of the different attributes. We estimated six LC-MNL models including between two and eight classes and retained the model with the lowest Bayesian information criterion (BIC). We then sorted individuals into the different classes and examined associations between latent class membership and individuals’ data quality and personal characteristics (eg, gender and education level). For this analysis, we combined data from the first chronic pain DCE (including the cost attribute) and the breathlessness DCE.
Sample size
We set target sample sizes for the three DCEs of 500, 200 and 200 participants, respectively. To investigate average preferences, we required a minimum sample size of 82 respondents, based on the Louviere formulae for choice proportions.31 This was calculated using a baseline choice probability of 33%, accuracy level of 90%, confidence level of 95% and 12 tasks (observations) per respondent, with an attrition rate of 20% due to exclusion of individuals providing low-quality data. We recruited more than the minimum number in order to (1) improve sample representativeness and ((2) to obtain more statistical power to explore between respondents variability in their choices. The design of the DCE was carried out with Ngene 1.1.1 and the analysis was conducted with R 3.2.3.
Patient involvement
Representatives from two patient groups were members of the study management group (although only one was able to participate actively throughout). The development of the study was informed by prior and contemporaneous research exploring patients’ views on what constituted person-centred care. We used the focus group and think-aloud stages to ensure that the content of the DCEs addressed key issues for patients in a comprehensible way. Two patient groups assisted with recruitment to the focus group and think-aloud stages.
Ethics
The study was approved by the North of Scotland Research Ethics Service (reference 14/NS/0075). Participants in the developmental stages all provided informed consent to take part. Consent for participants in the DCEs was managed by Research Now.
Results
Participant characteristics
About 517 individuals completed the main chronic pain DCE (DCE1); 200 individuals completed the breathlessness DCE (DCE2) and 206 completed the chronic pain (no-cost) DCE (DCE3). Their key characteristics are listed in table 2 and in online supplementary table 1. Across the three DCEs, between 10% and 20% of participants had experience of self-management support through a professional programme (eg, pain management or pulmonary rehabilitation) or a peer support group.
Table 2.
Participant characteristics
| Discrete choice experiment | Chronic Pain (DCE1) | Breathlessness (DCE2) | Chronic Pain (DCE3) |
| n=517 (%) | n=200 (%) | n=206 (%) | |
| Gender | |||
| Male | 176 (34) | 86 (43) | 99 (48) |
| Female | 341 (66) | 114 (57) | 107 (52) |
| Age, years | |||
| <40 | 61 (12) | 42 (21) | 23 (11) |
| 40–49 | 92 (18) | 43 (22) | 31 (15) |
| 50–59 | 129 (25) | 48 (24) | 62 (30) |
| 60–69 | 157 (30) | 43 (22) | 79 (38) |
| ≥70 | 78 (15) | 24 (12) | 16 (8) |
| Marital status | |||
| Single | 86 (17) | 25 (13) | 30 (15) |
| Married/legal partnership | 333 (64) | 137 (69) | 142 (69) |
| Separated/Widowed | 98 (19) | 38 (19) | 34 (17) |
| Education | |||
| No formal qualifications | 32 (6) | 15 (8) | 12 (6) |
| Secondary/high school | 243 (47) | 87 (44) | 90 (45) |
| University/College degree | 220 (43) | 89 (45) | 91 (46) |
| Other | 22 (4) | 9 (4.5) | 13 (7) |
| Household income | |||
| ≤£10 399/year | 64 (12) | 21 (11) | 26 (13) |
| £10 400–20 799/year | 140 (27) | 36 (18) | 46 (22) |
| £20 800–36 399/year | 158 (31) | 33 (17) | 63 (31) |
| £36 400–51 999/year | 61 (12) | 62 (31) | 30 (15) |
| ≥£1000/week (≥£52 000) | 40 (8) | 32 (16) | 21 (10) |
| Prefer not to say | 54 (10) | 16 (8) | 20 (10) |
| Employment | |||
| Employed/working | 182 (35) | 97 (49) | 77 (37) |
| Retired | 198 (38) | 55 (28) | 66 (32) |
| Long-term sick or disabled | 70 (14) | 13 (7) | 48 (23) |
| Other not employed | 67 (13) | 35 (18) | 15 (7) |
| Self-rated health status | |||
| Very good | 21 (4) | 10 (5) | 4 (2) |
| Good | 154 (30) | 62 (31) | 46 (22) |
| Fair | 226 (44) | 88 (44) | 90 (44) |
| Bad | 97 (19) | 37 (19) | 53 (26) |
| Very bad | 19 (4) | 3 (2) | 13 (6) |
bmjopen-2016-015689supp002.pdf (44.1KB, pdf)
DCE data quality
Results for the individual tests for the risk of low-quality data are shown in table 3. Overall data quality were good: 714 participants failed no tests (77.4 .%), 160 failed one (17.3%), 37 failed two (4.0%) and 12 (1.3%) failed all three. There was no difference in data quality between studies (χ2=9.34, p=0.15). The most common indicator of potentially low-quality data was (short) response time.
Table 3.
Tests for risk of low-quality discrete choice experiment (DCE) data
| Discrete choice experiment |
Chronic pain
(DCE1) |
Breathlessness
(DCE2) |
Chronic pain (DCE3) | Overall | ||||
| n=517 (%) | n=200 | n=206 | n=923 | |||||
| Incidence of individual low-quality criteria | ||||||||
| Serial non-participation | 7 | 1.4 | 5 | 2.5 | 5 | 2.4 | 17 | 1.8 |
| Dominance | 56 | 10.8 | 28 | 14.0 | 31 | 15.0 | 115 | 12.5 |
| Response time | 74 | 14.3 | 33 | 16.5 | 28 | 13.6 | 135 | 14.6 |
| Cumulative tests failed per individual | ||||||||
| One or more test failed | 115 | 22.2 | 53 | 26.1 | 44 | 21.4 | 209 | 22.6 |
| Two or more tests failed | 19 | 3.7 | 17 | 8.4 | 16 | 7.8 | 49 | 5.3 |
| All three tests failed | 3 | 0.6 | 5 | 2.5 | 4 | 1.9 | 12 | 1.3 |
Value of person-centredness attributes
In each DCE, there was a clear and consistent difference between attributes in their estimated values. Table 4 shows the results for each of the DCEs: the attributes for which a higher level of person-centredness was most valued were situation (taking account of a person’s current situation) and living well (working with them on what they wanted to get from life). More personally relevant information (contrasted with the same information for everyone) was valued less than these and a friendly and personal communicative style (contrasted with a neutral professional style) was valued least. Overall, higher person-centredness of the situation and living well attributes were valued four times more than higher person-centredness of communicative style. The similarity of findings between the two DCEs with a cost attribute in different conditions suggests that the findings are not condition specific, and the similarity between these two and the second pain DCE suggests that asking people about paying for services did not substantially affect preferences. The sensitivity analysis reported in supplementary table S2 shows that excluding those participants who failed at least two of the data quality tests had minimal effects on the results.
Table 4.
Multinomial logit analysis: higher versus neutral level of person-centredness by attribute and by discrete choice experiment (DCE)
| Discrete choice experiment | Chronic pain (DCE1) |
Breathlessness (DCE2) |
Chronic Pain (DCE3) |
|||
| Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | |
| Regression coefficient | ||||||
| Information | 0.65 | (0.58 to 0.73) | 0.60 | (0.47 to 0.72) | 0.93 | (0.79 to 1.07) |
| Situation | 0.91 | (0.82 to 0.99) | 0.90 | (0.76 to 1.05) | 1.43 | (1.23 to 1.63) |
| Living well | 0.85 | (0.78 to 0.92) | 0.81 | (0.68 to 0.93) | 1.19 | (1.04 to 1.35) |
| Communication | 0.21 | (0.15 to 0.26) | 0.21 | (0.12 to 0.30) | 0.31 | (0.20 to 0.42) |
| Cost* | −0.06 | (−0.07 to −0.05) | −0.06 | (−0.07 to −0.04) | – | – |
| Choice elasticity (in %) | ||||||
| Information | 12.3 | (11.0 to 13.6) | 10.6 | (8.3 to 12.9) | 15.0 | (12.9 to 17.0) |
| Situation | 16.9 | (15.4 to 18.3) | 16.1 | (13.6 to 18.6) | 21.9 | (19.3 to 24.5) |
| Living well | 15.8 | (14.5 to 17.1) | 14.6 | (12.5 to 16.7) | 19.4 | (17.2 to 21.6) |
| Communication | 3.8 | (2.7 to 4.8) | 4.2 | (2.6 to 5.8) | 5.4 | (3.5 to 7.2) |
| Cost | −1.1 | (−1.2 to −0.9) | −1.0 | (−1.3 to −0.8) | ||
| Model statistics | ||||||
| Individuals | 517 | 200 | 206 | |||
| Observations | 12 408 | 4800 | 4944 | |||
| Parameters | 5 | 5 | 4 | |||
| Log likelihood | −12 004 | −4739 | −4542 | |||
| BIC | 24 054 | 9520 | 9117 | |||
*Coefficient for increase by £1 in cost of service
BIC, Bayesian Information Criterion.
Patterns of similar value of person-centredness attributes
The latent class analysis included 717 participants. The optimal model had four classes. The results are shown in table 5; the upper part shows the regression coefficients for the five attributes of each class and the lower part the association of each class with demographic, economic and data quality variables. On the basis of the features of individuals allocated probabilistically to the four classes, we characterised them as follows: Class 1 - ‘Situation/living well dominant’: this was the largest group (n=286, 39.9%) and had a similar pattern of coefficients to the aggregate study population. Class 2 - ‘Information dominant’: this group (n=137, 19.1%) valued personalised information more highly than other characteristics. Class 3 - ‘Cost minimisers’: this group (n=126, 17.6%) showed the strongest aversion to cost with weak preferences for person-centredness of the attributes. More than a third of this group were fast responders to items suggesting that rather than weighing up choices, they made choices heuristically, driven by cost; members of this group were more likely than the other groups to have a low income (<£15 600 pa). Although the coefficients for the person-centredness attributes were smaller in this class compared with classes 1 and 2, they were still significantly positive and followed a similar pattern to the overall sample results. Class 4 - ‘Inconsistent data’: this group (n=168, 23.4%) showed no strong preference for person-centredness in the attributes and had a weakly positive coefficient for cost which was unexpected as it implies a willingness to pay more for less valued attributes. Members of this group were much more likely to fail tests of data quality than those in other groups, suggesting that these results may represent failure to comprehend tasks (the dominance test) or quickly ‘clicking through’ answers without considering them (the response time test).
Table 5.
Coefficients for preferences and class membership for 4 groups from latent class logit modelling (data pooled from patients in DCE1 and DCE2)
| Latent Class | Class 1: situation/living well | Class 2: information | Class 3: cost dominant | Class 4: inconsistent | ||||
| Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | |
| Preferences* | ||||||||
| Information | 0.80 | (0.72 to 0.88) | 1.95 | (1.78 to 2.13) | 0.24 | (0.14 to 0.35) | 0.01 | (−0.07 to 0.10) |
| Situation | 2.08 | (1.95 to 2.21) | 0.98 | (0.84 to 1.12) | 0.31 | (0.18 to 0.44) | 0.18 | (0.08 to 0.28) |
| Living well | 1.82 | (1.70 to 1.94) | 0.78 | (0.65 to 0.90) | 0.44 | (0.32 to 0.55) | 0.25 | (0.16 to 0.33) |
| Communication | 0.45 | (0.37 to 0.52) | 0.23 | (0.10 to 0.36) | 0.11 | (0.01 to 0.21) | 0.11 | (0.03 to 0.20) |
| Cost | −0.06 | (−0.07 to −0.06) | −0.05 | (−0.06 to −0.04) | −0.25 | (−0.27 to −0.23) | 0.02 | (0.01 to 0.02) |
| Class membership† | ||||||||
| Constant | – | – | −0.77 | (−1.71 to 0.17) | 1.00 | (0.15 to 1.85) | 0.45 | (−0.38 to 1.27) |
| DCE2‡ | – | – | −0.21 | (−0.75 to 0.32) | −0.02 | (−0.53 to 0.49) | 0.07 | (−0.40 to 0.54) |
| Relationship: Single§ | – | – | −0.16 | (−0.69 to 0.36) | −0.37 | (−0.89 to 0.15) | −0.10 | (−0.58 to 0.39) |
| Education: University¶ | – | – | 0.20 | (−0.29 to 0.69) | −0.05 | (−0.54 to 0.43) | 0.01 | (−0.44 to 0.46) |
| Job status: Not working** | – | – | −0.18 | (−0.97 to 0.62) | −0.08 | (−0.82 to 0.67) | −0.30 | (−1.02 to 0.41) |
| Job status: Retired** | – | – | −0.15 | (−0.72 to 0.43) | −0.59 | (−1.17 to −0.01) | −0.81 | (−1.36 to −0.27) |
| Job status: Disabled** | – | – | 0.31 | (−0.67 to 1.29) | 0.08 | (−0.82 to 0.99) | −0.15 | (−1.00 to 0.70) |
| Perceived health: Fair†† | – | – | −0.05 | (−0.59 to 0.49) | −0.44 | (−0.96 to 0.08) | −0.09 | (−0.59 to 0.41) |
| Perceived health: Poor†† | – | – | −0.58 | (−1.33 to 0.16) | −1.06 | (−1.78 to −0.34) | −0.45 | (−1.11 to 0.21) |
| Gender: Female‡‡ | – | – | −0.10 | (−0.61 to 0.42) | −0.82 | (−1.31 to −0.33) | −0.62 | (−1.08 to −0.16) |
| Income: £15 600-£31 1999 | – | – | 0.24 | (−0.46 to 0.95) | −0.61 | (−1.22 to 0.01) | −0.10 | (−0.70 to 0.50) |
| Income: £31200+§§ | – | – | 0.40 | (−0.34 to 1.15) | −1.15 | (−1.88 to −0.43) | −0.12 | (−0.78 to 0.53) |
| Income: Not prepared to say§§ | 0.93 | (0.08 to 1.78) | −0.19 | (−1.02 to 0.64) | −0.13 | (−1.03 to 0.78) | ||
| Class share | N | % | N | % | N | % | N | % |
| Predicted membership | 286 | 39.9% | 137 | 19.1% | 126 | 17.6% | 168 | 23.4% |
| Data quality* | ||||||||
| Serial Non-participation (n=12) | 0 | – | 0 | – | 0 | – | 12 | 100% |
| Dominance (n=84) | 11 | 13.1% | 6 | 7.1% | 2 | 2.4% | 65 | 77.4% |
| Response time (n=107) | 4 | 3.7% | 9 | 8.4% | 46 | 43.0% | 48 | 44.9% |
*In the Preferences and Data quality sections, only the dominant values are highlighted in bold.
† In the Class membership section, statistically significant coefficients are highlighted in bold.
‡Compared with DCE1.
§Compared with married/co-habiting.
¶Compared with no university education.
**Compared with working.
††‘Bad’ or ‘very bad’ self-rated health compared with ‘good’ or ‘very good’.
‡‡Compared with male.
§§Compared with <£15 600 per annum.
Discussion
Patients valued two aspects of person-centredness more highly than others. These were attention to their personal situation and orientation to what matters to them for living well. A substantial minority valued personal relevance of information provision most highly. A more friendly and personal communicative style was consistently valued least.
This is the first study, to our knowledge, to use discrete choice experiments in health services research to examine such highly personal attributes of healthcare delivery. DCEs, which are widely used in economics, represent the most appropriate method to answer our research question. Neither simpler questionnaire surveys nor qualitative research, despite its invaluable depth and theoretical rigour, can quantify values for preferences. Observational studies of practice would be vulnerable to multiple confounders and outcomes may be only weakly connected to processes.32 The attributes were developed from prior theoretical and empirical work and refined and tested through a series of stages following best practices for DCE development. By using an online panel, we obtained large samples: in the case of the chronic pain DCEs, participants had similar characteristics to an earlier population cohort study.33 However, we do not have information on non-responders; this is a limitation of the study, and future studies using online panels should ensure they collect this information. We conducted three separate DCEs with overlapping designs to establish generalisability beyond a single condition and to ensure that the findings were not an artefact of including a cost attribute. The large sample size and use of best-worst scaling allowed us to conduct latent class analysis and define four categories, with two in particular demonstrating contrasting but highly plausible preference types.
Although robustly derived and tested, the four attributes, even at the higher levels of person-centredness, do not add up to a complete account of person-centred care.1–4 6 It is possible that the wording of attribute descriptions may have biased the results by creating a larger ‘gap’ between the neutral and higher levels of person-centredness for some attributes than others. We attempted to minimise this by careful testing of the wording in the development stages and by only offering choices between neutral and higher levels so as to avoid negative values for particularly poor forms of practice (values for avoiding loss are typically weighted differently from values for potential gains34). We acknowledged the possibility that the data would contain systematic error introduced by the challenge of completing the DCE. Rather than simply eliminate data of low quality (and potentially introduce bias due to the choice of quality criteria), we chose first to include all data in the primary analysis, second to conduct a sensitivity analysis in which data with high risk of low quality were excluded, and third to conduct the latent class analysis which identified a group of patents with inconsistent and weak preferences which included many of the individuals who met criteria for low-quality data. While our findings make it clear that some aspects of person-centred care do matter more than others, they act as a starting point for further enquiry including where sufficiency thresholds lie (as described above, we compared enhanced attributes against neutral, not negative ones); whether particular combinations of features are important; and whether preferences change over the course of illness or in different healthcare contexts. These may require different study designs and interpretive approaches.
Making support for self-management more person-centred involves working on a complex cluster of attitudes and practices. This study shows that people place a high value on support that pays attention to their particular situation and on the orientation of support to what matters to them for living well with their condition. We also found that people vary in the value they place on different aspects of person-centredness and for a substantial minority the provision of personally relevant information was the most valued attribute. One striking finding was that the least valued aspect of person-centredness was that of adopting a ‘friendly and personal’ communicative tone compared with a more neutral professional one. This is important, given the current/conventional emphasis on communication skills training for professionals, which has only infrequently been challenged.10 35 Our findings lend support to the view that person-centred communication needs to be underpinned by a broad sense of purpose that orients its content to enable the person to act in their situation and towards what matters to them in life. Without that kind of purpose, attention to the style of communication is unlikely to achieve the responsiveness or scope for patient’s engagement that is sought. While our study was limited to support for self-management, the findings are likely to be more widely generalisable; recent work in acute settings has shown that patients rate communication which focuses on purpose, even when it has little or no emotional engagement, as excellent.11
In the introduction, we described person-centred care as a complex concept with multiple aspects. Our findings of heterogeneity in the valuation of four of these aspects (our attributes) make it clear that individuals vary in which features of person-centred care matter to them most. One size does not fit all and providers need to be conscious of this. These differences were not associated with broad social or demographic features. An emphasis on ‘treating as a person’—recognising and cultivating an individual’s ‘person-al’ capabilities2—leads to some challenging issues. It is not clear how this can be achieved, and it is quite possible that individuals and their healthcare providers have conflicting priorities and values. Despite these challenges, the values which patients place on these attributes emphasise the importance for healthcare of providing person-centred (or ‘person-supportive’)2 care.
Conclusion
The aspects of person-centred support for self-management that people with long-term conditions most value are attention to their personal situation and an orientation to what matters to them in life. Investment in training to improve professionals’ skills must address the substance of clinical communication—working responsively with individuals on what matters to them—as well as its style.
Supplementary Material
Acknowledgments
We wish to thank the members of Aberdeen & District Fibromyalgia support group and Grampian Pain Support for encouraging participation in the study and particularly to two of their members who took active roles as members of the study management committee.
Footnotes
Contributors: The study was conceived by CDB, MR, AME and VAE. All authors were involved in the planning, design, conduct and reporting of the study. TP conducted the focus groups and think-aloud studies and carried out the initial analysis of these. CDB and VAE led the wording of attributes and NK conducted the analysis of DCE results. All authors contributed to the writing and revision of the manuscript. CDB is guarantor for the study.
Funding: The study was funded by the Health Foundation (reference THF 7264) and sponsored by the University of Aberdeen. Neither funder nor sponsor had any involvement in the conduct or reportingof the study.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethics approval: North of Scotland Research Ethics Services.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data may be available from the authors on request.
References
- 1. Epstein RM, Fiscella K, Lesser CS, et al. . Why the nation needs a policy push on patient-centered health care. Health Aff 2010;29:1489–95. 10.1377/hlthaff.2009.0888 [DOI] [PubMed] [Google Scholar]
- 2. Entwistle VA, Watt IS. Treating patients as persons: a capabilities approach to support delivery of person-centred care. Am J Bioeth 2013;13:29–39. 10.1080/15265161.2013.802060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berwick DM. What ‘patient-centred should mean: confessions of an extremist. Health Aff 2009;28:w555–w565. 10.1377/hlthaff.28.4.w555 [DOI] [PubMed] [Google Scholar]
- 4. Institute of Medicine. crossing the Quality Chasm: a New Health System for the 21st Century. Washington, D.C: National Academy Press, 2001. [PubMed] [Google Scholar]
- 5. Ekman I, Swedberg K, Taft C, et al. . Person-centered care--ready for prime time. Eur J Cardiovasc Nurs 2011;10:248–51. 10.1016/j.ejcnurse.2011.06.008 [DOI] [PubMed] [Google Scholar]
- 6. Leplege A, Gzil F, Cammelli M, et al. . Person-centredness: conceptual and historical perspectives. Disabil Rehabil 2007;29:1555–65. 10.1080/09638280701618661 [DOI] [PubMed] [Google Scholar]
- 7. McCormack B, McCance TV. Development of a framework for person-centred nursing. J Adv Nurs 2006;56:472–9. 10.1111/j.1365-2648.2006.04042.x [DOI] [PubMed] [Google Scholar]
- 8. Entwistle V, Firnigl D, Ryan M, et al. . Which experiences of health care delivery matter to service users and why? A critical interpretive synthesis and conceptual map. J Health Serv Res Policy 2012;17:70–8. 10.1258/jhsrp.2011.011029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ryan M, Kinghorn P, Entwistle VA, et al. . Valuing patients’ experiences of healthcare processes: towards broader applications of existing methods. Soc Sci Med 2014;106:194–203. 10.1016/j.socscimed.2014.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wright EB, Holcombe C, Salmon P. Doctors’ communication of trust, care, and respect in breast Cancer: qualitative study. BMJ 2004;328:864 10.1136/bmj.38046.771308.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Young B, Hill J, Gravenhorst K, et al. . Is communication guidance mistaken? qualitative study of parent-oncologist communication in childhood Cancer. Br J Cancer 2013;109:836–43. 10.1038/bjc.2013.413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1–7. 10.1207/S15324796ABM2601_01 [DOI] [PubMed] [Google Scholar]
- 13. Townsend A, Wyke S, Hunt K, Self-managing HK. Self-managing and managing self: practical and moral dilemmas in accounts of living with chronic illness. Chronic Illn 2006;2:185–94. 10.1177/17423953060020031301 [DOI] [PubMed] [Google Scholar]
- 14. Kendall E, Rogers A. Extinguishing the social?: state sponsored self‐care policy and the chronic disease self‐management Programme. Disabil Soc 2007;22:129–43. 10.1080/09687590601141535 [DOI] [Google Scholar]
- 15. Entwistle VA, Cribb A. Enabling people to live well. London: The Health Foundation, 2013. [Google Scholar]
- 16. Taylor SJC, Pinnock H, Epiphaniou E, et al. . A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: prisms – Practical systematic RevIew of Self-Management Support for long-term conditions. Health Serv Deliv Res 2014;2:1–580. 10.3310/hsdr02530 [DOI] [PubMed] [Google Scholar]
- 17. Morgan HM, Entwistle VA, Cribb A, et al. . We need to talk about purpose: a critical interpretive synthesis of health and social care professionals’ approaches to self-management support for people with long-term conditions. Health Expect 2017;20 10.1111/hex.12453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dowrick C, Kokanovic R, Hegarty K, et al. . Resilience and depression: perspectives from primary care. Health 2008;12:439–52. 10.1177/1363459308094419 [DOI] [PubMed] [Google Scholar]
- 19. Hinder S, Greenhalgh T. ‘This does my head in’. Ethnographic study of self-management by people with diabetes. BMC Health Serv Res 2012;12:6963 10.1186/1472-6963-12-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sinding C, Miller P, Hudak P, et al. . Of time and troubles: patient involvement and the production of health care disparities. Health 2012;16:400–17. 10.1177/1363459311416833 [DOI] [PubMed] [Google Scholar]
- 21. Clark MD, Determann D, Petrou S, et al. . Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics 2014;32:883–902. 10.1007/s40273-014-0170-x [DOI] [PubMed] [Google Scholar]
- 22. Epstein RM, Franks P, Fiscella K, et al. . Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med 2005;61:1516–28. 10.1016/j.socscimed.2005.02.001 [DOI] [PubMed] [Google Scholar]
- 23. Ryan M, Watson V, Entwistle V. Rationalising the ‘irrational’: a think aloud study of discrete choice experiment responses. Health Econ 2009;18:321–36. 10.1002/hec.1369 [DOI] [PubMed] [Google Scholar]
- 24. Ferrini S, Scarpa R. Designs with a priori information for nonmarket valuation with choice experiments: a Monte Carlo study. J Environ Econ Manage 2007;53:342–63. 10.1016/j.jeem.2006.10.007 [DOI] [Google Scholar]
- 25. Lancsar E, Louviere J, Donaldson C, et al. . Best worst discrete choice experiments in health: methods and an application. Soc Sci Med 2013;76:74–82. 10.1016/j.socscimed.2012.10.007 [DOI] [PubMed] [Google Scholar]
- 26. Von Korff M, Ormel J, Keefe FJ, et al. . Grading the severity of chronic pain. Pain 1992;50:133–49. 10.1016/0304-3959(92)90154-4 [DOI] [PubMed] [Google Scholar]
- 27. van der Molen T, Willemse BW, Schokker S, et al. . Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes 2003. 1:13 10.1186/1477-7525-1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. InternationalAssociation for the Study of Pain. Classificationof chronic pain. Pain 1986:1–226. [Google Scholar]
- 29. Pearson MG, Bucknall CE. Measuring clinical outcome in asthma: a patient focused approach. London: Royal College of Physicians, 1999. [Google Scholar]
- 30. Greene WH, Hensher DA. A latent class model for discrete choice analysis: contrasts with mixed logit. Transportation Research Part B: Methodological 2003;37:681–98. 10.1016/S0191-2615(02)00046-2 [DOI] [Google Scholar]
- 31. Louviere JH, D.A.; Swait JD. Stated choice methods: analysis and application. Cambridge: Cambridge University Press, 2000. [Google Scholar]
- 32. Lilford RJ, Brown CA, Nicholl J. Use of process measures to monitor the quality of clinical practice. BMJ 2007;335:648–50. 10.1136/bmj.39317.641296.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Elliott AM. Chronic pain in the community: its prevalence impact and natural history PhD Thesis, University of Aberdeen: Universityof Aberdeen, 2000. [Google Scholar]
- 34. Kahneman D, Tversky A. Prospect Theory: an analysis of decision under risk. Econometrica 1979;47:263–91. 10.2307/1914185 [DOI] [Google Scholar]
- 35. Salmon P, Young B. The validity of education and guidance for clinical communication in Cancer care: evidence-based practice will depend on practice-based evidence. Patient Educ Couns 2013;90:193–9. 10.1016/j.pec.2012.04.010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-015689supp003.jpg (2MB, jpg)
bmjopen-2016-015689supp001.pdf (23.6KB, pdf)
bmjopen-2016-015689supp002.pdf (44.1KB, pdf)