Abstract
Objectives. To estimate changes in the prevalence of daily cannabis use among current, former, and never cigarette smokers from 2002 to 2014 in the United States.
Methods. The National Survey on Drug Use and Health is a nationally representative cross-sectional study conducted annually among persons aged 12 years and older in the United States.
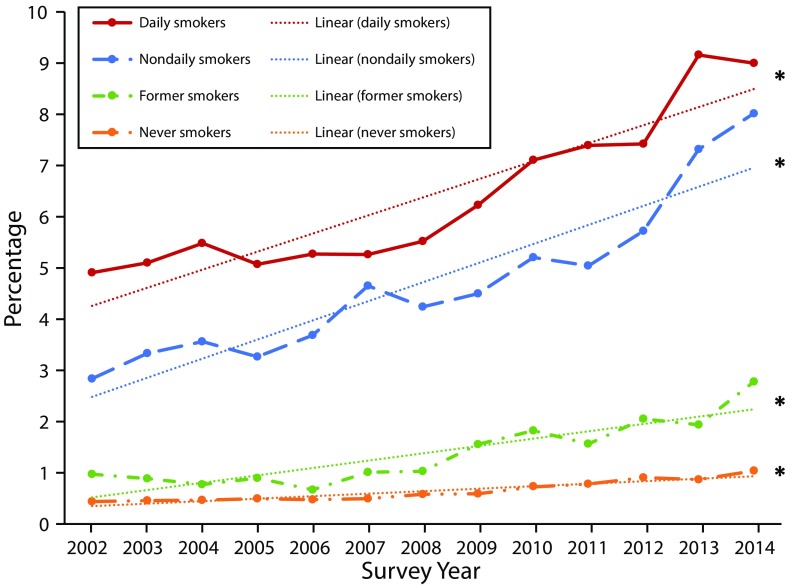
Results. Daily cannabis use occurs nearly exclusively among nondaily and daily cigarette smokers compared with former and never smokers (8.03%, 9.01%, 2.79%, 1.05%, respectively). Daily cannabis use increased over the past decade among both nondaily (8.03% [2014] vs 2.85% [2002]; linear trend P < .001) and daily smokers (9.01% [2014]; 4.92% [2002]; linear trend P < .001). Daily cannabis use increased most rapidly among former cigarette smokers (2.79% [2014] vs 0.98% [2002]; linear trend P < .001).
Conclusions. Daily cannabis use occurs predominantly among cigarette smokers in the United States. Daily cannabis use increased among current, former, and never smokers over the past decade, with particularly rapid increases among youth and female cigarette smokers. Future research is needed to monitor the observed increase in daily cannabis use, especially among youths and adults who smoke cigarettes.
Cigarette smoking remains the leading preventable cause of disease and premature mortality in the United States.1 There have been substantial declines in smoking prevalence over the past half century in the United States, although the rate of this decline has decelerated in recent years.2,3
Cannabis use is more common among people who smoke cigarettes than among those who do not.4–6 Studies show that cannabis use is associated with the persistence of cigarette smoking7,8 and relapse to smoking among former smokers.9 The inverse is also evident: the use of tobacco is associated with increased odds of cannabis dependence.10 Previous studies have not examined whether the prevalence of daily cannabis use has changed among cigarette smokers in the population over the past decade. Indeed, previous work suggests that heavy cannabis use is strongly related to cigarette smoking and nicotine dependence.5,11–13 In a recent study, Schauer et al. found an increase in past 30-day cannabis use among tobacco users from 2003 to 2012,6,14 as well as significant increases in co-use of past 30-day cannabis and tobacco use from 2003 to 2012 with differential increases by demographic group. Yet, it is not clear that previous studies examining occasional, any past-30 day, or any past-year cannabis use allow us to extrapolate to an accurate estimate of the relations between daily cannabis use and cigarette smoking. Understanding the degree to which daily cannabis use may be common among cigarette smokers is critical because previous findings suggest that any past month cannabis use is associated with smoking persistence and relapse7,9 coupled with previous estimates of high rates of cigarette smoking among cannabis users.14
We investigated the prevalence of daily cannabis use among nondaily, daily, former, and lifetime cigarette nonsmokers and whether these rates differ by demographic characteristics among those aged 12 years and older in the United States. Second, we estimated changes in the prevalence of daily cannabis use among nondaily, daily, former, and never cigarette smokers, overall and by demographic subgroups, from 2002 to 2014.
METHODS
The National Survey on Drug Use and Health (NSDUH) provides annual cross-sectional national data on the use of tobacco, other substance use, and mental health in the United States.15–23 A multistage area probability sample for each of the 50 states and the District of Columbia was conducted to represent the male and female civilian noninstitutionalized population of the United States aged 12 years and older. We obtained data from the 2002–2014 NSDUH public use data files for a combined sample size of 725 010 individuals. To increase the precision of estimates, African Americans, Hispanics, and young people were oversampled. Response rates for completed surveys ranged from 73% to 79%.
Participants aged 18 years and older provided informed consent, and parental permission and assent was obtained for individuals aged 12 to 17 years before the start of every interview. Participants were given a description of the study, read a statement describing the legislation regarding the confidentiality of any information provided by participants, and assured that participation in the study was voluntary. Surveys were administered by computer-assisted personal interviewing conducted by an interviewer and audio computer-assisted self-interviewing. Audio computer-assisted self-interviewing was designed to provide respondents with a private and confidential means of responding to questions and to increase honest reporting of illegal drug use and other sensitive behaviors. Respondents were offered US $30 for participation.
Sampling weights for the NSDUH were computed to control for unit-level and individual-level nonresponse and adjusted to ensure consistency with population estimates obtained from the US Census Bureau. To use data from the 13 years of combined data, a new weight was created upon aggregating the 13 data sets by dividing the original weight by the number of data sets combined. Additional information describing the complex sampling weight methodology for the NSDUH can be found elsewhere.22
Measures
Sociodemographic variables.
Sociodemographic variables for this study included gender, race/ethnicity (White, African American, Hispanic, other [i.e., Native American/Alaska Native, Native Hawaiian/Other Pacific Islander, Asian, more than 1 race]), age (12–17, 18=25, ≥ 26 years), and annual income (< $20 000, $20 000–$74 999, ≥ $75 000).
Cigarette smoking variables.
Current cigarette smoking status was assessed using the following questions: (1) “Have you ever smoked part or all of a cigarette?”; (2) “Have you smoked at least 100 cigarettes in your entire life?”; and (3) “During the past 30 days, have you smoked part or all of a cigarette?” We classified individuals who did not report smoking at least 100 cigarettes in their lifetime as never smokers. We classified individuals who reported smoking at least 100 cigarettes in their lifetime and at least 1 cigarette within the past 30 days as current smokers. We then subdivided current smokers on the basis of frequency of smoking using the following question: “During the past 30 days, that is, since [DATEFILL], on how many days did you smoke part or all of a cigarette?” We classified those who smoked 1 to 29 days of the past 30 days as current nondaily smokers and those who smoked all 30 of the past 30 days as current daily smokers. We classified individuals who reported smoking 100 cigarettes in their lifetime and reported smoking 0 cigarettes in the past 30 days as former smokers. Similar classification schemes have been used in previous research.24,25
We asked nondaily and daily smokers to report the number of cigarettes that they smoked per day: “On the days you smoked cigarettes during the past 30 days, how many cigarettes did you smoke per day, on average?” Response options for the included “1–15” versus “16+” cigarettes that they smoked per day.
Cannabis use variables.
Participants reported how long it had been since their last cannabis use. We categorized individuals reporting using cannabis “within the past 30 days” as past month users in a new dichotomous variable (any vs none). Participants indicating past month use reported the number of days they used cannabis in the last 30 days. We classified participants who reported using cannabis on 25 days or greater as “daily users.”25–29
Statistical Analysis
Data were weighted to reflect the complex design of the NSDUH sample and analyzed with Stata SE version 12.0.30 We used Taylor series estimation methods (Stata SVY commands) to obtain proper SE estimates for the cross-tabulations. First, we examined the combined prevalence of daily cannabis use by smoking statuses (nondaily, daily, former, and never smokers) from 2002 to 2014. We then examined the association between daily cannabis use with nondaily and daily cigarette smoking by demographic characteristics. Next, we examined the prevalence of daily cannabis use among the 4 smoking statuses across time from 2002 to 2014.
We assessed linear time trends of cannabis use and daily cannabis use using logistic regression models with continuous year as the predictor. We then used multivariable logistic regression to adjust for demographics (gender, age, race/ethnicity, income). Within these analyses, odds ratios (ORs) indicate the slopes of the increase and decrease (i.e., rapidity of change) in daily cannabis use between 2002 and 2014. Furthermore, we used models with year by smoking status interaction terms and F-tests to test the significance of these interactions to assess differential time trends (i.e., differences in the rapidity of change between smoking statuses).
Additionally, we tested interactions between year, smoking status, and selected demographic characteristics (gender, race/ethnicity, age); all were significant (all P < .01). Thus, we stratified analyses concerning the prevalence of daily cannabis use by the demographic characteristics. We used models with year by sociodemographic characteristic interaction terms and F-tests to test the significance of these interactions to assess differential time trends (i.e., differences in the rapidity of change between levels of the sociodemographic variables) within each of the 4 smoking statuses.
RESULTS
Daily and nondaily cigarette smokers were significantly more likely to use cannabis daily than were never smokers (OR = 4.47; [95% confidence interval (CI) = 4.15, 4.82]; OR = 7.61; [95% CI = 7.09, 8.17], respectively) in every demographic group. The relationships between daily and nondaily cigarette smoking and daily cannabis use differed significantly by age, gender, marital status, race, and income (Table 1). The strength of the relationships varied, but all were robust and statistically significant. In terms of differences by demographic strata, the relationship between daily and nondaily cigarette smoking and daily cannabis use was stronger among females than among males, among youths aged 12 to 17 years than among older age groups, among never married and widowed, divorced, or separated versus married, and among the highest income group versus the lowest income group.
TABLE 1—
Association of Daily Cannabis Use With Daily and Nondaily Cigarette Smoking, by Demographic Characteristics: National Survey on Drug Use and Health, United States, 2002–2014
| Unadjusted Prevalence of Daily Cannabis Use |
Nondaily Cigarette Smoking Versus No Cigarette Smoking |
Daily Cigarette Smoking Versus No Cigarette Smoking |
||||||
| Characteristic | Total Sample, % (95% CI) | Non–cigarette Smoker, % (95% CI) | Nondaily Cigarette Smoker, % (95% CI) | Daily Cigarette Smoker, % (95% CI) | ORa (95% CI) | Pintb | ORa (95% CI) | Pintb |
| Total sample | 1.91 (1.86, 1.96) | 0.85 (0.82, 0.89) | 4.74 (4.51, 4.99) | 6.31 (6.09, 6.55) | 4.47 (4.15, 4.82) | 7.61 (7.09, 8.17) | ||
| Gender | ||||||||
| Male (Ref) | 2.79 (2.71, 2.87) | 1.32 (1.26, 1.39) | 5.94 (5.58, 6.33) | 8.28 (7.94, 8.63) | 3.87 (3.55, 4.23) | 6.51 (5.99, 7.08) | ||
| Female | 1.08 (1.03, 1.14) | 0.44 (0.40, 0.47) | 3.13 (2.83, 3.47) | 4.14 (3.87, 4.42) | 6.58 (5.69, 7.62) | < .001 | 10.93 (9.77, 12.22) | < .001 |
| Age, y | ||||||||
| 12–17 (Ref) | 1.27 (1.22, 1.33) | 0.55 (0.51, 0.59) | 11.17 (11.05, 11.24) | 21.01 (20.87, 21.33) | 22.70 (20.08, 25.67) | 51.35 (45.28, 58.24) | ||
| 18–25 | 5.60 (5.47, 5.73) | 2.49 (2.37, 2.60) | 10.40 (9.93, 10.89) | 15.46 (15.05, 15.88) | 4.24 (3.95, 4.55) | < .001 | 7.23 (6.81, 7.68) | < .001 |
| ≥ 26 | 1.35 (1.30, 1.41) | 0.64 (0.60, 0.69) | 2.75 (2.47, 3.06) | 4.32 (4.08, 4.57) | 3.14 (2.75, 3.58) | < .001 | 5.54 (5.01, 6.13) | < .001 |
| Marital status | ||||||||
| Married (Ref) | 0.84 (0.78, 0.90) | 0.44 (0.39, 0.49) | 1.99 (1.64, 2.41) | 3.06 (2.77, 3.37) | 4.23 (3.40, 5.26) | 6.77 (5.90, 7.78) | ||
| Widowed, divorced, or separated | 1.46 (1.32, 1.61) | 0.63 (0.54, 0.74) | 2.07 (1.98, 2.13) | 3.95 (3.48, 4.49) | 2.78 (2.09, 3.69) | < .001 | 5.55 (4.46, 6.90) | < .001 |
| Never married | 3.72 (3.63, 3.82) | 1.61 (1.54, 1.69) | 8.30 (7.92, 8.70) | 12.67 (12.30, 13.05) | 4.77 (4.43, 5.15) | < .001 | 8.55 (7.96, 9.19) | < .001 |
| Income, $ | ||||||||
| < 20 000 (Ref) | 2.87 (2.74, 3.01) | 1.30 (1.19, 1.42) | 5.68 (5.20, 6.21) | 7.32 (6.86, 7.82) | 3.92 (3.38, 4.55) | 6.44 (5.69, 7.28) | ||
| 20 000–74 999 | 1.96 (1.89, 2.03) | 0.86 (0.0.80, 0.91) | 4.69 (4.34, 5.06) | 6.14 (5.84, 6.46) | 4.61 (4.08, 5.19) | .051 | 7.43 (6.97, 8.60) | .011 |
| ≥ 75 000 | 1.23 (1.15, 1.31) | 0.62 (0.56, 0.69) | 0.62 (0.56, 0.69) | 5.49 (5.03, 5.99) | 5.07 (4.30, 5.97) | .007 | 9.07 (7.78, 10.57) | < .001 |
| Race/ethnicity | ||||||||
| White (Ref) | 1.99 (1.93, 2.04) | 0.84 (0.79, 0.89) | 4.96 (4.64, 5.31) | 6.09 (5.84, 6.34) | 4.62 (4.18, 5.10) | 7.33 (6.75, 7.96) | ||
| Black | 2.38 (2.23, 2.55) | 1.25 (1.12, 1.39) | 5.07 (4.93, 5.18) | 8.07 (7.94, 8.19) | 3.55 (2.83, 4.44) | .26 | 6.89 (5.83, 8.15) | .14 |
| Hispanic | 1.44 (1.33, 1.56) | 0.73 (0.64, 0.82) | 3.96 (3.81, 4.15) | 6.67 (6.53, 6.79) | 5.31 (4.22, 6.69) | < .001 | 10.96 (8.84, 13.57) | < .001 |
| Other | 1.30 (1.18, 1.43) | 0.60 (0.48, 0.74) | 3.76 (3.62, 3.89) | 6.01 (5.20, 6.94) | 4.98 (3.49, 7.09) | < .001 | 9.59 (6.72, 13.69) | < .001 |
Note. CI = confidence interval; OR = odds ratio. ORs reflect associations within each level of sociodemographic variables, comparing nondaily and daily cigarette smoking with nonsmoking.
Adjusted for all other variables listed in the table and calendar year (categorical).
P value for multiplicative interaction of demographic by smoking categories on daily cannabis use, e.g., OR = 6.58 for nondaily vs no cigarettes in women is significantly different (Pint < .001) compared with the OR = 3.87 in men.
For race/ethnicity, there was no difference in the strength of the relationship between cigarette smoking and daily cannabis use between White and African American respondents; the relationships were stronger among Hispanic and other race/ethnicity group respondents than among White respondents. For instance, among Hispanic smokers (vs nonsmokers) the relationship between daily cannabis use and cigarette smoking was significantly stronger than among White individuals (OR = 10.96; [95% CI = 8.84, 13.57] vs OR = 7.73; [95% CI = 6.75, 7.96]; P < .001, respectively). The relationship was also significantly stronger among females than among males (OR = 10.93; [95% CI = 9.77, 12.22] vs OR = 6.51; [95% CI = 5.99, 7.08]; P < .001, respectively).
The strength of the relationship between cigarette smoking and daily cannabis use was particularly strong among youths aged 12 to 17 years. The ORs suggest that nondaily and daily cigarette smoking in youths is associated with a 23-fold and 51-fold increase in likelihood of using cannabis daily, respectively.
Daily Cannabis Use by Cigarette Smoking Status
Daily cannabis use increased significantly in the US population across all smoking statuses from 2002 to 2014: current daily (4.92% vs 9.01%), nondaily (2.85% vs 8.03%), former (0.98% vs 2.79%), and never cigarette smokers (0.45% vs 1.05%; Figure 1; Table A [available as a supplement to an online version of this article at http://www.ajph.org]). These trends remained significant after adjusting for a range of covariates.
FIGURE 1—
Prevalence of Daily Cannabis Use Over Time and Linear Time Trends, by Cigarette Smoking Status: National Survey on Drug Use and Health, United States, 2002–2014
*Linear trend P < .05.
However, the rate of the increase differed significantly by smoking group in several cases. Specifically, the increase in rate of daily cannabis use was significantly more rapid among nondaily smokers (adjusted OR [AOR] = 1.10; 95% CI = 1.08, 1.12) than among daily smokers (AOR = 1.07; 95% CI = 1.06, 1.09) and more rapid among former smokers (AOR = 1.12; 95% CI = 1.10, 1.15) than among never smokers (AOR = 1.08; 95% CI = 1.07, 1.10).
Daily Cannabis Use by Gender
Daily cannabis use increased significantly among both genders in all smoking status groups. Among never smokers, daily cannabis use increased faster among females (AOR = 1.13; 95% CI = 1.10, 1.16) than among males (AOR = 1.06; 95% CI = 1.05, 1.08), and females showed a 3-fold increase in prevalence of daily cannabis use over this period (Table B [available as a supplement to an online version of this article at http://www.ajph.org]).
There were no differences in the rate of change over time by gender among daily, nondaily, and former smokers.
Daily Cannabis Use by Race/Ethnicity
Daily cannabis use increased among all daily, nondaily, former, and never smokers of all race/ethnicity groups, without any significant differences in the rate of change between groups (Table C [available as a supplement to an online version of this article at http://www.ajph.org]).
Notably, daily cannabis use increased 5-fold among nondaily, former, and never smokers of other race/ethnicity.
Daily Cannabis Use by Age
Daily cannabis use increased significantly among daily cigarette smokers in all age groups (Table D [available as a supplement to an online version of this article at http://www.ajph.org]); the fastest rates of increase were among those aged 26 years and older (AOR = 1.10; 95% CI = 1.08, 1.12) versus aged 12 to 17 years (AOR = 1.04; 95% CI = 1.02, 1.07) and 18 to 25 years (AOR = 1.04; 95% CI = 1.03, 1.05). The highest prevalence of daily cannabis use—by contrast—was among those aged 12 to 17 years with 27.6% of daily smokers aged 12 to 17 years using cannabis daily in 2014. In 2014, 20.33% of those aged 18 to 25 years who were daily cigarette smokers used cannabis daily, with a considerably lower proportion (7.12%) of daily cannabis use among daily cigarette smokers aged 26 years and older.
Among nondaily cigarette smokers, daily cannabis use increased in all age groups, again with the fastest rate of change among those aged 26 years and older (AOR = 1.13; 95% CI = 1.09, 1.16), followed by aged 18 to 25 years (AOR = 1.09; 95% CI = 1.07, 1.10) and 12 to 17 years (AOR = 1.06; 95% CI = 1.03, 1.09). Among nondaily cigarette smokers, daily cannabis use was considerably lower (12.5%) among those aged 12 to 17 years (vs 27.6% among daily cigarette smokers), although daily cannabis use was reported by 17.34% of nondaily cigarette smokers aged 18 to 25 years in 2014.
DISCUSSION
The study has several key findings. First, daily cannabis use appears to occur nearly exclusively among cigarette smokers in the United States. Specifically, averaged over 2002 to 2014, the prevalence of daily cannabis use is approximately 10 times higher among cigarette smokers than among never smokers. Less than 1% of never cigarette smokers use cannabis daily, whereas 11.05% of cigarette smokers (nondaily smokers: 4.74%; daily smokers: 6.31%) use cannabis daily.
Second, the prevalence of daily cannabis use increased significantly among daily (4.92% vs 9.01%), nondaily (2.85% vs 8.03%), former (0.98% vs 2.79%), and never (0.45% vs 1.05%) cigarette smokers from 2002 to 2014. Yet, the rate of increase in daily cannabis use was most rapid among former cigarette smokers. Although the overall prevalence of daily cannabis use remains relatively low among non–cigarette smokers compared with cigarette smokers, the number of people affected is substantial; non–cigarette smokers comprise the largest segment of the population (former smokers: 20.03%; never smokers: 58.61%).
Third, the prevalence of daily cannabis use by smoking status differed by demographic group. The disparities in these relationships were particularly notable by age, gender, and race/ethnicity.
The mechanisms underlying the relationship between tobacco and cannabis use are not clear, but because of the high rate of co-use, this topic is being intensely studied.31 Overlaps in the neurobiological systems involved with nicotine and cannabis (e.g., activation of the mesolimbic dopaminergic system) and cannabinoid receptors appear to mediate the rewarding effects of nicotine.31–33 In fact, cannabinoid agents have been proposed as potential treatments for nicotine dependence.32 Substitution has been defined as a conscious choice to substitute 1 drug for another, as described among medical marijuana patients.34,35 In this case, use of tobacco and cannabis together may be driven by attempts to use 1 drug to alleviate some of the potential negative effects or consequences of the other drug.
Persons who quit smoking cigarettes may substitute cannabis to lessen withdrawal symptoms, using an alternative substance that is viewed as less addictive, less harmful, and carrying less stigma. With regard to withdrawal, some preclinical and clinical data suggest that cannabis use attenuates the experience of nicotine withdrawal.36,37 Also, both cannabis and nicotine are typically used by the same route of administration (i.e., inhalation) and are often used simultaneously through blunts or joints, which increases the amount of tetrahydrocannabinol inhaled.37,38 Preclinical research suggests that tetrahydrocannabinol increases the rewarding value of nicotine,39 and numerous cannabis users report using tobacco to extend and enhance the effects of cannabis.39,40 One laboratory study showed that persons receiving nicotine through a transdermal patch, compared with a placebo patch, reported increased effects from cannabis, including a higher heart rate and self-rating of being “stimulated” and “high.”31
Complementarity is generally defined as the case when 2 drugs are used together at high rates, as tobacco and cannabis are, because of a desire to experience synergistic effects of the drugs. This is another potential explanatory mechanism for high levels of use of both substances. In addition, there is evidence that cannabis and tobacco have somewhat contrasting effects on cognition. Specifically, cannabis can have negative effects on cognition,41–43 whereas nicotine can have positive effects on cognition44 and nicotine may be used as an attempt to attenuate cannabis-related negative cognitive effects.44–46 It is also conceivable that a pattern of use may begin as substitution and transform into complementarity. Furthermore, it is possible that a number of psychosocial, individual, and environmental factors influence co-use, especially with the changes in cannabis legal status and the increasing stigma associated with cigarette use. Future research that can investigate pathways that incorporate the reciprocal effects of neurobiological, psychosocial, psychological, and environmental factors will likely be needed to gain a better understanding of these mechanisms.
Upon examining the relationship between daily cannabis use and cigarette smoking by demographic subgroups, we found significant and robust relationships for all subgroups, but the strength of the relationships differed significantly by subgroup. The most striking disparity was by age, specifically among youths aged 12 to 17 years. Although the prevalence of daily cannabis use was almost nonexistent among those aged 12 to 17 years who have never smoked cigarettes (i.e., 0.65%), 27.6% of adolescent daily cigarette smokers and 12.52% adolescent nondaily cigarette smokers reported daily cannabis use. We are not aware of previous reports that have illustrated that daily cannabis use in youths occurs nearly entirely among those who also use cigarettes.
In addition to age, we found several other differences for demographic subgroups. Although the prevalence of daily cannabis use was higher among men than among women, the relationship between cigarette smoking and daily cannabis use was stronger among women than among men and the prevalence of daily cannabis use increased significantly more rapidly among women than among men over time. The strength of the relationship between cigarette smoking and daily cannabis use also increased with income, with the strongest relationship among those with incomes of $75 000 and higher, although the relationship among those with $20 000 and lower was still robust. Future in-depth work is needed to understand these shifting trends by gender and income.
Limitations
Limitations of this study should be considered. First, the level of cannabis use on a certain day is not known, and therefore this may vary considerably. Further, cannabis use was measured by self-report without biological verification and is therefore subject to report bias. Thus, level of consumption is not known and may vary considerably.
Second, the mode of administration of cannabis is not fully detailed. In future work, understanding whether the relations between cigarette smoking and cannabis use is related to route of administration of cannabis or tobacco would be helpful both from a public health perspective in assessing prevalence trends and in furthering efforts to understanding the mechanisms of this relationship.
Additionally, because of the repeated cross-sectional nature of the NSDUH, we are unable to explore changes within the same individuals over time. Yet, the data do not allow observation of potentially important trends over time at the population level.
Conclusions
Because of the strong relationship between cigarette and cannabis co-use, and operating under the premise that increased daily cannabis use could be contributing to the deceleration in smoking prevalence in the United States, our primary goal was to investigate the relationship between cigarette smoking and daily cannabis use and to examine whether daily cannabis use has increased among smokers over time. We found that daily cannabis use has increased significantly among nondaily smokers and daily smokers. Yet, the rate of increase was most rapid among non–cigarette smokers.
The rate of increase of daily cannabis use among nondaily cigarette smokers was slightly higher than among daily cigarette smokers; and recent results suggest that whereas daily smoking continues to decline rapidly, nondaily smoking is not declining as rapidly and may be increasing in some groups. It is conceivable that this stunted decline in cigarette use is owing, in part, to the substantial increase in daily cannabis use in this group. Other work has recently found that nondaily smokers also appear to have higher levels of depression and other substance use, suggesting they are a group who requires further study.47
We also found that although the relative prevalence of daily cannabis use among non–cigarette smokers is low compared with that among smokers, the rate of increase in nonsmokers is faster than it is among smokers. Previously, some work has found that cigarette use may be a gateway into other drug use behavior, including cannabis.48 Yet, recent work suggests that (1) more permissive attitudes toward marijuana may mitigate this gateway effect, or (2) cannabis may serve as a gateway to cigarette use.49 Because recreational cannabis has recently been legalized in a growing number of US states, nonsmokers may represent a new group at considerable risk for high-frequency cannabis use in the years ahead.
ACKNOWLEDGMENTS
The work was funded by (grant/award 2R01DA20892).
HUMAN PARTICIPANT PROTECTION
The study was deemed “exempt” according to federal regulations, under 45 CFR 46.101 (b) by the Institutional Review Board of Queens College, The City University of New York.
REFERENCES
- 1.2012 Global Progress Report on Implementation of the WHO Framework Convention on Tobacco Control. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 2.Results From the 2013 National Survey on Drug Use and Health: Summary of Findings. Rockville, MD: Substance Abuse Mental Health Services Administration; 2014. [Google Scholar]
- 3.Trends in Current Cigarette Smoking Among High School Students and Adults, United States, 1965–2011. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 4.Agrawal A, Lynskey MT. Tobacco and cannabis co-occurrence: does route of administration matter? Drug Alcohol Depend. 2009;99(1–3):240–247. doi: 10.1016/j.drugalcdep.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinberger AH, Funk AP, Goodwin RD. A review of epidemiologic research on smoking behavior among persons with alcohol and illicit substance use disorders. Prev Med. 2016;92:148–159. doi: 10.1016/j.ypmed.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M. Assessing the overlap between tobacco and marijuana: trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addict Behav. 2015;49:26–32. doi: 10.1016/j.addbeh.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Ramo DE, Liu H, Prochaska JJ. Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clin Psychol Rev. 2012;32(2):105–121. doi: 10.1016/j.cpr.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goodwin RD, Sheffer CE, Chartrand H et al. Drug use, abuse, and dependence and the persistence of nicotine dependence. Nicotine Tob Res. 2014;16(12):1606–1612. doi: 10.1093/ntr/ntu115. [DOI] [PubMed] [Google Scholar]
- 9.Weinberger AH, Copeland J, Platt JM, Goodwin RD. Is cannabis use associated with increased risk of initiation, persistence, and relapse to cigarette smoking? Longitudinal data from a representative sample of US adults. J Clin Psychiatr. doi: 10.4088/JCP.17m11522. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hindocha C, Shaban NCD, Freeman TP et al. Associations between cigarette smoking and cannabis dependence: a longitudinal study of young cannabis users in the United Kingdom. Drug Alcohol Depend. 2015;148:165–171. doi: 10.1016/j.drugalcdep.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Degenhardt L, Hall W, Lynskey M. Alcohol, cannabis and tobacco use among Australians: a comparison of their associations with other drug use and use disorders, affective and anxiety disorders, and psychosis. Addiction. 2001;96(11):1603–1614. doi: 10.1046/j.1360-0443.2001.961116037.x. [DOI] [PubMed] [Google Scholar]
- 12.Redner R, White TJ, Harder VS, Higgins ST. Vulnerability to smokeless tobacco use among those dependent on alcohol or illicit drugs. Nicotine Tob Res. 2014;16(2):216–223. doi: 10.1093/ntr/ntt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez-Quintero C, Pérez de los Cobos J, Hasin D et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115(1–2):120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M. Differences in tobacco product use among past month adult marijuana users and nonusers: findings from the 2003–2012 National Survey on Drug Use and Health. Nicotine Tob Res. 2016;18(3):281–288. doi: 10.1093/ntr/ntv093. [DOI] [PubMed] [Google Scholar]
- 15.Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2004–2011 [data files and codebook]. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
- 16.Reliability of Key Measures in the National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. [PubMed] [Google Scholar]
- 17.Results From the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. [Google Scholar]
- 18.Results From the 2006 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- 19.Results From the 2011 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 20.Results From the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 21.Harrison LD, Martin SS, Enev T, Harrington D. Comparing Drug Testing and Self-Report of Drug Use Among Youths and Young Adults in the General Population. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- 22.Hunter S, Feder M, Granger B, Piper L, Chromy J. 2005 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. [PubMed] [Google Scholar]
- 23.Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Methodological Summary and Definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 24.Trosclair A, Dube SR. Smoking among adults reporting lifetime depression, anxiety, anxiety with depression, and major depressive episode, United States, 2005–2006. Addict Behav. 2010;35(5):438–443. doi: 10.1016/j.addbeh.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 25.Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149(1):232–244. doi: 10.1016/j.drugalcdep.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Budney AJ, Vandrey RG, Hughes JR, Moore BA, Bahrenburg B. Oral delta-9-tetrahydrocannabinol suppresses cannabis withdrawal symptoms. Drug Alcohol Depend. 2007;86(1):22–29. doi: 10.1016/j.drugalcdep.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 27.Moore BA, Budney AJ. Relapse in outpatient treatment for marijuana dependence. J Subst Abuse Treat. 2003;25(2):85–89. doi: 10.1016/s0740-5472(03)00083-7. [DOI] [PubMed] [Google Scholar]
- 28.Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. 2003;112(3):393–402. doi: 10.1037/0021-843x.112.3.393. [DOI] [PubMed] [Google Scholar]
- 29.Whitlow CT, Liguori A, Livengood LB et al. Long-term heavy marijuana users make costly decisions on a gambling task. Drug Alcohol Depend. 2004;76(1):107–111. doi: 10.1016/j.drugalcdep.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 30.StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 31.Rabin RA, George TP. A review of co-morbid tobacco and cannabis use disorders: possible mechanisms to explain high rates of co-use. Am J Addict. 2015;24(2):105–116. doi: 10.1111/ajad.12186. [DOI] [PubMed] [Google Scholar]
- 32.Gamaleddin IH, Trigo JM, Gueye AB et al. Role of the endogenous cannabinoid system in nicotine addiction: novel insights. Front Psychiatry. 2015;6:41. doi: 10.3389/fpsyt.2015.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kohut SJ. Interactions between nicotine and drugs of abuse: a review of preclinical findings. Am J Drug Alcohol Abuse. 2017;43(2):155–170. doi: 10.1080/00952990.2016.1209513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Vital signs: current cigarette smoking among adults aged ≥ 18 years with mental illness—United States, 2009–2011. MMWR Morb Mortal Wkly Rep. 2013;62(5):1–7. [PMC free article] [PubMed] [Google Scholar]
- 35.Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduct J. 2009;6(1):35. doi: 10.1186/1477-7517-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walsh Z, Callaway R, Belle-Isle L et al. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int J Drug Policy. 2013;24(6):511–516. doi: 10.1016/j.drugpo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Balerio GN, Aso E, Berrendero F, Murtra P, Maldonado R. Delta9-tetrahydrocannabinol decreases somatic and motivational manifestations of nicotine withdrawal in mice. Eur J Neurosci. 2004;20(10):2737–2748. doi: 10.1111/j.1460-9568.2004.03714.x. [DOI] [PubMed] [Google Scholar]
- 38.Van der Kooy F, Pomahacova B, Verpoorte R. Cannabis smoke condensate II: influence of tobacco on tetrahydrocannabinol levels. Inhal Toxicol. 2009;21(2):87–90. doi: 10.1080/08958370802187296. [DOI] [PubMed] [Google Scholar]
- 39.Panlilio LV, Zanettini C, Barnes C, Solinas M, Goldberg SR. Prior exposure to THC increases the addictive effects of nicotine in rats. Neuropsychopharmacology. 2013;38(7):1198–1208. doi: 10.1038/npp.2013.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tullis LM, Dupont R, Frost-Pineda K, Gold MS. Marijuana and tobacco: a major connection? J Addict Dis. 2003;22(3):51–62. doi: 10.1300/J069v22n03_05. [DOI] [PubMed] [Google Scholar]
- 41.D’Souza DC, Perry E, MacDougall L et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29(8):1558–1572. doi: 10.1038/sj.npp.1300496. [DOI] [PubMed] [Google Scholar]
- 42.Morrison PD, Zois V, McKeown DA et al. The acute effects of synthetic intravenous Delta-9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol Med. 2009;39(10):1607–1616. doi: 10.1017/S0033291709005522. [DOI] [PubMed] [Google Scholar]
- 43.Broyd SJ, van Hell HH, Beale C, Yücel M, Solowij N. Acute and chronic effects of cannabinoids on human cognition—a systematic review. Biol Psychiatry. 2016;79(7):557–567. doi: 10.1016/j.biopsych.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 44.Heishman SJ, Kleykamp BA, Singleton EG. Meta-analysis of the acute effects of nicotine and smoking on human performance. Psychopharmacology (Berl) 2010;210(4):453–469. doi: 10.1007/s00213-010-1848-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schuster RM, Mermelstein RJ, Hedeker D. Ecological momentary assessment of working memory under conditions of simultaneous marijuana and tobacco use. Addiction. 2016;111(8):1466–1476. doi: 10.1111/add.13342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schuster RM, Crane NA, Mermelstein R, Gonzalez R. Tobacco may mask poorer episodic memory among young adult cannabis users. Neuropsychology. 2015;29(5):759–766. doi: 10.1037/neu0000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jacobsen LK, Pugh KR, Constable RT, Westerveld M, Mencl WE. Functional correlates of verbal memory deficits emerging during nicotine withdrawal in abstinent adolescent cannabis users. Biol Psychiatry. 2007;61(1):31–40. doi: 10.1016/j.biopsych.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 48.Weinberger AH, Gbedemah M, Wall MM et al. Depression among non-daily smokers compared to daily smokers and never-smokers in the United States: an emerging problem. Nicotine Tob Res. 2017 doi: 10.1093/ntr/ntx009. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peters EN, Budney AJ, Carroll KM. Clinical correlates of co-occurring cannabis and tobacco use: a systematic review. Addiction. 2012;107(8):1404–1417. doi: 10.1111/j.1360-0443.2012.03843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]