Abstract
Objectives. To evaluate the efficacy of an interactive, Web-based sexual health program (Health Education and Relationship Training [HEART]) for developing sexual assertiveness skills and enhancing sexual decision-making in adolescent girls.
Methods. Participants were 222 tenth-grade girls (mean age = 15.2; 38% White, 29% Hispanic, 25% Black) in the Southeastern United States who were randomized in fall 2015 to the HEART intervention or an attention-matched control. We assessed participants at pretest, immediate posttest, and 4-month follow-up.
Results. Both groups had similar demographic and sexual behavior characteristics at pretest. At immediate posttest, girls who completed the HEART program demonstrated better sexual assertiveness skills measured with a behavioral task, higher self-reported assertiveness, intentions to communicate about sexual health, knowledge regarding HIV and other sexually transmitted diseases (STDs), safer sex norms and attitudes, and condom self-efficacy compared with the control condition. At 4-month follow-up, group differences remained in knowledge regarding HIV and other STDs, condom attitudes, and condom self-efficacy.
Conclusions. This brief online sexual health program can improve short-term outcomes among adolescent girls and offers an exciting new option in the growing array of digital health interventions available to youths.
Trial Registration Number. NCT02579135.
Adolescent girls—particularly low-income, minority girls—are disproportionately affected by sexually transmitted diseases (STDs) and unintended pregnancy.1,2 As many as 1 in 4 sexually active adolescents has an STD,3 and nearly 250 000 adolescent girls give birth each year.1 Girls also may experience serious long-term consequences from untreated STDs. These include the risk of cervical cancer, infertility, and ectopic pregnancy,2,4 as well as psychosocial consequences such as increased stigma and shame.5
Efforts to improve girls’ sexual health outcomes have been under way for decades. At least 2 dozen efficacious sexual-risk reduction interventions have been identified.6 However, most programs utilize face-to-face delivery strategies that are time- and resource-intensive.7 As a result, many vulnerable youths are not receiving the sexual education and skills training that could improve their sexual health.
Recently there has been a movement to utilize Internet-based, digital technologies to create sexual health programs that can be broadly disseminated with greater efficiency.8,9 These approaches use technology-based platforms (e.g., computers, tablets, smartphones) as the primary mechanism for reaching and engaging youths in prevention of HIV and other STDs. Online programs offer many benefits, including the relative ease and low cost of administration, increased fidelity to intervention delivery, and opportunities for amplified user interactivity and customization.10,11 Several studies have shown that technology-based programs for the prevention of HIV and other STDs have comparable efficacy to face-to-face programs.8,12 Given the nearly ubiquitous use of technology among adolescents,13 online approaches are also a highly relevant medium for connecting with youths who are at risk for HIV and other STDs and unplanned pregnancy.
In an effort to increase access to sexual education, our team developed a brief Web-based program for girls called HEART (Health Education and Relationship Training).14 This theory-based program provides motivation enhancement, skill-building, and information about HIV and other STDs and unplanned pregnancy and has a unique focus on developing sexual communication and assertiveness skills. Sexual communication is a robust predictor of safer sexual behavior, including condom use.15 Although a number of in-person interventions target these skills,16 our team was not aware of any technology-based programs that specifically focus on developing sexual assertiveness. Importantly, recent studies comparing in-person assertiveness role-plays to computerized role-plays have found evidence for greater skill development in computerized role-plays.17 In addition, computerized role-plays provide a controlled environment for learning skills that are difficult or embarrassing. This practice is a crucial first step in the development of complex interpersonal skills, such as sexual negotiation.18
We examined the efficacy of HEART in a randomized controlled trial. We hypothesized that girls who completed HEART would demonstrate greater sexual assertiveness skills, safer sexual attitudes, knowledge regarding HIV and other STDs, and sexual self-efficacy relative to an attention-matched control. The second purpose was to test whether treatment effects would be sustained over a 4-month follow-up. We conducted supplemental analyses to examine differences in effects by race/ethnicity and sexual activity status.
METHODS
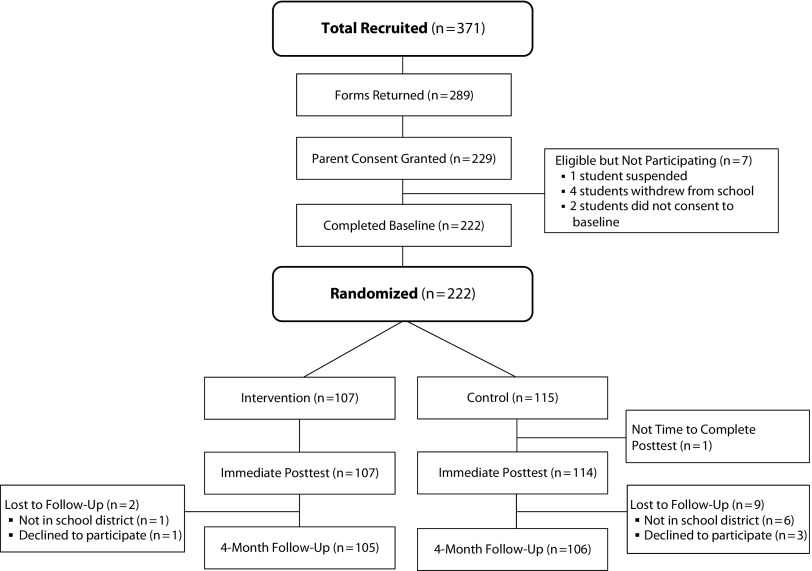
In fall 2015, we recruited participants from 4 rural, low-income high schools in the southeastern United States. We recruited all 10th-grade girls (n = 371) with active parental consent and student assent. As indicated in Figure 1, 78% of youths returned a parental consent form, and 79% of those parents granted consent. The final sample included 222 girls who received parental consent and assented to participate in the study who completed the pretest assessment and were randomized to study conditions.
FIGURE 1—
Study Flow Diagram: Assessment of Web-Based Sexual Health Program Among Tenth-Grade Girls: Southeastern United States, 2015
Design and Procedures
After consent and assent were obtained, we collected pretest and immediate posttest data from students 1 school at a time over approximately 6 weeks. First, participants completed a computerized pretest survey in a group-based classroom setting with ample room between seats and privacy dividers. Next, participants were randomly assigned to either the HEART program or an attention-matched program called Growing Minds (described subsequently). An investigator independent of the study team conducted random assignment by using random sampling and allocation procedures in SPSS version 22 (IBM, Somers, NY). Randomization was stratified within school and based on participants’ sexual activity status (obtained during pretest).
After randomization, research staff coordinated with school personnel to have youths complete the intervention and immediate posttest assessment during school time in individual sessions in private rooms. During the posttest assessment, participants completed an abbreviated computerized survey as at pretest and also completed an audio-recorded role play to assess behavioral skills in sexual assertiveness (described later in the “Behavioral assessment of sexual assertiveness skills” section). Because of feasibility issues of completing testing with each participant individually in a school-based setting, we were only able to assess behavioral skills at the immediate posttest. At 4-month follow-up, participants completed all outcome measures via computerized surveys in a group-based classroom setting.
Participants received $10 for returning their parental consent form, regardless of whether consent was granted. In addition, participants received $10 for the pretest, $30 for the intervention and immediate posttest, and $10 for the 4-month follow-up.
Description of HEART
HEART is an interactive, skills-focused intervention designed for digital delivery in 1 sitting lasting approximately 45 minutes. A full description can be found elsewhere.14,19 Program content is grounded in psychological and health behavior change theories, including the Reasoned Action Model20 and Fuzzy Trace Theory.21 The program includes 5 modules that can be completed on a computer, tablet, or smartphone device. The program targets 5 areas of sexual decision-making:
safer sex motivation,
knowledge regarding HIV and other STDs,
sexual norms and attitudes,
safer sex self-efficacy, and
sexual communication skills.
Modules are taught within a sexual health paradigm emphasizing personal values, positive aspects of sexuality, and the importance of competent interpersonal skills, as well as risk reduction.22 Inside each module, users receive age-appropriate audio and video clips, tips from other adolescents, interactive games and quizzes, infographics, and skill-building exercises with self-feedback given in real time.
Communication self-efficacy and assertiveness skills are emphasized throughout the program, but particularly in the communication module. In this module, users receive didactic training and modeling from same-age peers. Users can also practice skills through an audio-recording and playback feature whereby they respond to hypothetical scenarios of sexual pressure from a partner depicted with a prerecorded male voice. Girls record and rate their own responses and continue practicing until they become more comfortable. Our previous work has shown that the digital HEART program is highly acceptable and engaging.19
Description of Control Program
Growing Minds is an attention-matched online intervention that focuses on cultivating academic and social growth mindsets.23 This program was adapted from other mindset-based intervention work.24 It is delivered via a Web-based platform and lasts approximately 45 minutes.
Growing Minds includes 5 modules that are comparable to HEART in format and materials (see material available as a supplement to the online version of this article at http://www.ajph.org). Program content covers key components typically incorporated into mindset work, such as providing evidence of the malleable nature of academic and social success. In addition, it includes 2 unique components: (1) teaching about growth mindsets, and (2) incorporating role models to reinforce growth mindset messages and strengthen attitude change. Both HEART and Growing Minds required a similar degree of active participation. In both programs, girls actively clicked links and completed activities in one module before proceeding to the next. Furthermore, both programs took approximately the same amount of time and included similarly engaging content, such as videos and quizzes.
Measures
Participant characteristics.
We collected data on age, race/ethnicity, sexual orientation, and parent educational status. We assessed sexual activity with 2 items (yes or no): one about any experience with sexual activity, including “sexual touching, oral sex, and/or sexual intercourse,” and a second about vaginal intercourse. We classified girls who responded yes to either item as sexually active. Among those who reported intercourse, we assessed condom use at last sexual intercourse and history of pregnancy.
Behavioral assessment of sexual assertiveness skills.
We assessed assertiveness skills at refusing unwanted sexual activity and negotiating condom use with an audio-recorded role-play methodology adapted from a validated behavioral assessment.25 During this assessment, participants listened and responded out loud to 3 role-play simulations as if they were in the situation (see material available as a supplement to the online version of this article at http://www.ajph.org for instructions, scenario wording, scoring, and validity information). Responses were recorded, transcribed, and rated on 3 dimensions based on an established coding system25,26: (1) refusal of unsafe behavior, (2) providing a reason for the refusal, and (3) verbal assertiveness (range for each code: 0 = absent; 1 = moderate; 2 = high). Four trained coders blinded to study condition coded the responses (interrater reliability = 84%). We averaged scores to obtain an index of sexual assertiveness skills. We excluded data from 24 participants who did not follow directions (n = 3 intervention; n = 21 control). There were no differences at pretest on any outcome variable between girls who were retained versus those who were excluded on the assertiveness assessment.
Sexual assertiveness.
We assessed self-reported sexual assertiveness with 3 items from the Multidimensional Sexual Self-Concept Scale.27 Items such as “I’m very assertive about the sexual aspects of my life,” were rated on a scale (from 1 = “strongly disagree” to 5 = “strongly agree”; Cronbach α = 0.69).
Knowledge.
We assessed knowledge regarding HIV and other STDs with 12 items (e.g., “STDs usually have noticeable symptoms, like itching or burning.”). Participants rated each item as “true,” “false,” or “don’t know.” Responses were recoded as 0 for incorrect (including “don’t know”) or 1 for correct. We summed scores to reflect the total number of correct answers to questions assessing knowledge regarding HIV and other STDs (possible range = 0–12).
Intentions.
We assessed intentions to use condoms and to communicate about sex with items from the AIDS Risk Behavior Assessment.28 One item asked the likelihood of using condoms in the future, with scores from 0% and 100% to represent the percentage of sexual encounters in which a participant would use condoms if they had sex in the next 3 months. In addition, 3 items captured the likelihood of communicating with a partner in the next 3 months about (1) sexual limits and boundaries, (2) STDs and pregnancy, and (3) condom use. Options ranged from 0% to 100% to indicate the likelihood of communicating with a partner. We averaged scores to create a composite; higher scores indicated greater likelihood of sexual communication (α = 0.84).
Sexual self-efficacy.
We used the validated Self-Efficacy for HIV Prevention Scale29 to assess communication self-efficacy and condom self-efficacy. Seven items assessed confidence communicating about sexual topics (e.g., “How sure are you that you could talk to your partner about safer sex?”). Three items assessed confidence obtaining and using condoms (e.g., “How sure are you that you could have condoms available when you need them?”). Participants responded from 1 for “couldn’t do it” to 4 for “very sure,” with higher scores indicating greater confidence in communicating about sex (α = 0.82) or obtaining and using condoms (α = 0.66).
Condom attitudes.
We assessed participants’ attitudes about condoms with the 3-item effect on sexual experiences subscale of the Condom Attitudes Scale Adolescent Version30 (e.g., “Condoms take away the pleasure of sex.”), with responses on a scale (from 1 = “strongly disagree” to 5 = “strongly agree”; α = 0.74).
Condom norms.
We used the 3-item condom norm subscale from the Sexual Risk Behavior Beliefs and Self-Efficacy Scale for adolescents31 to assess participants’ perceptions of their peers’ views of condom use (with responses from 1 = “strongly disagree” to 5 = “strongly agree” to items such as “Most teenagers believe condoms should always be used if a person my age has sex.” [α = 0.87]).
Analysis Plan
First, we used descriptive statistics to summarize sociodemographic variables and pretest levels of each outcome variable. To establish pretest equivalence, we assessed differences between groups with the t test for continuous variables and the χ2 test for categorical variables. Second, we conducted attrition analyses with the χ2 test to examine retention at the 4-month follow-up by study condition. Third, to assess the effectiveness of the HEART intervention from pretest to immediate posttest, we used linear regression analyses to compute adjusted means and mean differences between intervention and control groups. We included an indicator for school to adjust for clustering by school. For each outcome, the corresponding pretest measure was included as a covariate; 1 exception was for the behavioral assessment of assertiveness skills, as this was only completed at posttest. Fourth, to assess the effectiveness of HEART from pretest through 4-month follow-up, we used linear generalized estimating equation models to control for repeated within-subject measurements. We adjusted models for school as well as the corresponding pretest measure for each outcome. We used robust standard errors, and specified an exchangeable working correlation matrix. Finally, we included supplemental moderation analyses to examine if intervention effects were moderated by race/ethnicity or sexual activity status. To do this, we utilized the same linear regressions from step 3, and included the appropriate interaction terms. For primary analyses, we calculated a Cohen’s d value as an indication of effect size. We completed analyses with SPSS version 24 (IBM, Somers, NY).
Before the onset of the study, we conducted a power calculation to determine the appropriate sample size. We designed the study to have 80% power at a .05 significance level to detect differences in primary outcomes, assuming an effect size of 0.5 and a correlation of 0.4 between assessments. Final enrollment (n = 222) exceeded our target sample size (n = 150).
RESULTS
At pretest, sample characteristics were similar in treatment and control groups (Table 1). Approximately 40% of the sample was sexually active and 23% had engaged in vaginal intercourse at pretest. There was 1 statistically significant difference between the treatment and control groups at pretest: girls in the treatment group had more positive condom attitudes than girls in the control group. There were no other differences at pretest on demographic, attitudinal, or behavioral factors, including self-reported sexual assertiveness.
TABLE 1—
Sample Characteristics at Pretest Assessment Among Tenth-Grade Girls: Southeastern United States, 2015
| Characteristics | Project HEART, No. (%) or Mean ±SD (n = 107) | Growing Minds, No. (%) or Mean ±SD (n = 115) | Pa |
| Sociodemographics | |||
| White race/ethnicity | 38 (35.5) | 45 (39.1) | .62 |
| Black race/ethnicity | 29 (27.1) | 25 (21.7) | .33 |
| Hispanic race/ethnicity | 31 (28.9) | 34 (29.6) | .96 |
| Heterosexual sexual orientation | 84 (78.5) | 92 (80.0) | .74 |
| Mother’s education < high school | 21 (19.6) | 28 (24.3) | .38 |
| Currently in a relationship | 56 (52.3) | 55 (47.8) | .59 |
| Sexual behaviors | |||
| Ever engaged in sexual activity | 43 (40.2) | 48 (41.7) | .89 |
| Ever had vaginal sex | 26 (24.2) | 25 (21.7) | .62 |
| Had vaginal sex past 3 mo | 15 (14.0) | 13 (11.3) | .57 |
| Condom use at last sexb | 15 (57.7) | 16 (64.0) | .77 |
| Ever been pregnant | 1 (0.9) | 2 (1.7) | .62 |
| Primary outcomesc | |||
| Communication intentions (0–100) | 70.9 ±32.1 | 70.3 ±31.4 | .89 |
| Communication self-efficacy (1–4) | 3.6 ±0.5 | 3.5 ±0.5 | .11 |
| Secondary outcomes | |||
| Sexual assertiveness self-report (1–5) | 3.0 ±0.9 | 3.0 ±0.8 | .86 |
| HIV and STD knowledge (1–12) | 6.8 ±2.0 | 7.1 ±2.0 | .35 |
| Condom attitudes (1–5) | 3.6 ±0.8 | 3.4 ±0.6 | .043 |
| Condom norms (1–5) | 3.6 ±1.1 | 3.5 ±1.0 | .56 |
| Condom self-efficacy (1–4) | 2.3 ±0.8 | 2.2 ±0.8 | .12 |
| Condom intentions (0–100) | 92.2 ±23.5 | 90.1 ±24.1 | .52 |
Note. HEART = Health Education and Relationship Training; STD = sexually transmitted disease.
Difference test was the χ2 test for categorical variables and the t test for continuous variables.
Percentage based on sexually active adolescents.
Sexual assertiveness skills were assessed at immediate posttest only with a behavioral task.
No participants were lost between pretest and immediate posttest, though 1 participant in the control group ran out of time to complete the immediate posttest measures. At the 4-month follow-up, 95% of participants (n = 211) were retained in the study (98% intervention; 92% control; χ2 = 4.18; P = .04). Differences in attrition between study conditions were primarily attributable to the fact that 6 girls in the control condition transferred school districts versus 1 girl in the intervention condition (Figure 1). There were no differences at pretest on any outcome variable between girls who were retained versus those who were lost to follow-up.
As shown in Table 2, immediately following the intervention, participants who completed HEART demonstrated better sexual assertiveness skills measured with a behavioral task compared with youths who completed Growing Minds (Cohen’s d = 0.28). Because sexual assertiveness skills were only assessed at posttest, we conducted a sensitivity analysis whereby we repeated the linear regression model while controlling for pretest levels of self-reported assertiveness. Behavioral sexual assertiveness skills remained statistically significantly different between groups at posttest in this analysis. At posttest, treatment participants also reported higher self-reported sexual assertiveness, sexual communication intentions, knowledge regarding HIV and other STDs, condom norms, condom attitudes, and condom self-efficacy compared with control participants (all Ps < .05). The effect sizes of these outcomes were small to moderate (Cohen’s ds = 0.33–0.78); however, the effect on sexual knowledge was particularly strong (Cohen’s d = 4.78).
TABLE 2—
Safer Sex Intervention Effects on Primary and Secondary Outcomes at Immediate Posttest Among Tenth-Grade Girls: Southeastern United States, 2015
| Effects at Immediate Posttesta |
||||||
| Outcomes | Intervention, Mean ±SD | Control, Mean ±SD | No. for Analysis | Difference | P | Effect Sizeb |
| Primary outcomes | ||||||
| Sexual assertiveness skillsc (0–2) | 1.2 ±0.4 | 1.1 ±0.4 | 198 | 0.1 | .047 | 0.28 |
| Communication intentions (0–100) | 87.0 ±22.5 | 78.5 ±27.9 | 220 | 8.5 | < .001 | 0.33 |
| Communication self-efficacy (1–4) | 3.6 ±0.5 | 3.5 ±0.5 | 221 | 0.1 | .32 | 0.11 |
| Secondary outcomes | ||||||
| Sexual assertiveness self-report (1–5) | 3.6 ±0.8 | 3.1 ±0.8 | 208 | 0.5 | < .001 | 0.60 |
| HIV and STD knowledge (1–12) | 10.1 ±1.5 | 7.0 ±2.0 | 221 | 3.1 | < .001 | 4.78 |
| Condom attitudes (1–5) | 4.1 ±0.8 | 3.5 ±0.7 | 221 | 0.6 | < .001 | 0.78 |
| Condom norms (1–5) | 3.9 ±0.9 | 3.6 ±1.0 | 219 | 0.3 | .003 | 0.35 |
| Condom self-efficacy (1–4) | 2.8 ±0.8 | 2.3 ±0.8 | 219 | 0.5 | < .001 | 0.43 |
| Condom intentions (0–100) | 93.6 ±21.1 | 92.1 ±22.1 | 214 | 1.5 | .79 | 0.03 |
Note. STD = sexually transmitted disease.
Linear regression results, controlling for pretest level of each variable and school.
Cohen’s d standardized difference in covariance adjusted means between treatment group and control group.
Sexual assertiveness skills were assessed only at immediate posttest; thus, pretest levels were not controlled in this model.
At 4-month follow up, several intervention effects remained (Table 3). Girls who completed HEART had statistically significantly greater knowledge regarding HIV and other STDs, more positive condom attitudes, and greater condom self-efficacy at 4 months compared with girls in the control group (Cohen’s ds = 0.56, 0.45, and 0.30, respectively). The group differences that we initially observed in communication intentions, self-reported assertiveness, and condom norms had diminished by 4 months.
TABLE 3—
Safer Sex Intervention Effects on Primary and Secondary Outcomes at 4-Month Follow-Up Among Tenth-Grade Girls: Southeastern United States, 2015
| Effects at 4-Month Follow-Upa |
|||||
| Outcomes | Intervention, Mean ±SD | Control, Mean ±SD | Difference | P | Effect Sizeb |
| Primary outcomes | |||||
| Communication intentions (0–100) | 78.6 ±28.0 | 76.2 ±28.6 | 2.4 | .35 | 0.11 |
| Communication self-efficacy (1–4) | 3.6 ±0.5 | 3.6 ±0.5 | 0.0 | .28 | 0.12 |
| Secondary outcomes | |||||
| Sexual assertiveness self-report (1–5) | 3.4 ±0.9 | 3.3 ±0.9 | 0.1 | .08 | 0.19 |
| HIV and STD knowledge (1–12) | 8.2 ±2.0 | 7.4 ±2.0 | 0.8 | < .001 | 0.56 |
| Condom attitudes (1–5) | 4.1 ±0.8 | 3.7 ±0.8 | 0.4 | < .001 | 0.45 |
| Condom norms (1–5) | 3.3 ±1.0 | 3.4 ±1.0 | −0.1 | .53 | 0.07 |
| Condom self-efficacy (1–4) | 2.7 ±0.9 | 2.5 ±0.8 | 0.2 | .007 | 0.30 |
| Condom intentions (0–100) | 87.3 ±28.2 | 88.0 ±26.7 | −0.7 | .87 | 0.02 |
Note. STD = sexually transmitted disease.
Generalized estimating equation results, with control for clustering by school and pretest score on each variable.
Cohen’s d standardized difference in covariance adjusted means between treatment group and control group.
We conducted supplemental moderation analyses to examine if intervention effects were similar across racial/ethnic groups and for sexually active youths. We conducted analyses by race/ethnicity among the 202 girls who were White (n = 83), Black (n = 54), or Hispanic (n = 65). For all outcomes but one, intervention effects were similar across ethnic groups: the only difference was in knowledge regarding HIV and other STDs. Hispanic youths who completed HEART showed greater improvement in knowledge regarding HIV and other STDs from pretest (mean = 6.0; SD = 1.9) to posttest (mean = 10.1; SD = 1.4) than did White youths (pretest mean = 7.3; SD = 2.0; posttest mean = 10.3; SD = 1.3; b = 1.0; SE = 0.5; P = .038) and Black youths (pretest mean = 7.0; SD = 1.5; posttest mean = 10.0; SD = 1.4; b = 1.2; SE = 0.5; P = .023). There were no other differences in intervention effectiveness by race/ethnicity. Analyses by sexual activity status also demonstrated similarities between groups: sexual activity status did not moderate any intervention effect. In addition, when analyses were rerun only within the sample of sexually active youths (n = 91), the same pattern of significant findings emerged for sexual assertiveness skills, communication intentions, knowledge regarding HIV and other STDs, condom attitudes, condom self-efficacy, and sexual assertiveness self-report (all Ps < .05).
We conducted 1 final analysis to examine the impact of the HEART intervention on condom use behavior. Specifically, we examined changes in condom use at last sexual intercourse between pretest and 4-month follow-up for girls who engaged in intercourse at both time points (n = 43) by using a logistic regression analysis that controlled for pretest condom use and school. The study was not powered to detect statistically significant changes in condom use; however, we included the analysis to estimate an effect size for use in future studies. Results of the logistic regression were in the direction of better condom use for those in the HEART intervention compared with the control, though this effect was not significant (odds ratio = 1.85 [95% confidence interval = 0.45, 7.56]; dCox = 0.37).
DISCUSSION
The burden of STDs and unintended pregnancy among youths—both from a public health perspective and from the perspective of each adolescent who must navigate the consequences of these sexual health issues—requires ongoing, innovative prevention approaches. We found that girls who completed HEART, a new 45-minute digital sexual health program, demonstrated more effective behavioral skills in sexual assertiveness and higher self-reported assertiveness compared with girls completing a control program. Participants also reported immediate increases in knowledge regarding HIV and other STDs, safer sexual attitudes and norms, greater sexual communication intentions, and increased self-efficacy for obtaining and using condoms compared with a control group. Importantly, the strength of these findings did not differ by race/ethnicity or sexual activity status, indicating that the intervention was equally effective for a diverse sample of youths. At 4-month follow-up, girls who completed the intervention retained greater knowledge regarding HIV and other STDs, more positive condom attitudes, and greater condom self-efficacy; however, there were no longer statistically significant group differences in communication intentions, self-reported assertiveness, or condom norms.
There are many benefits of utilizing interactive digital technologies to engage youths with prevention messages. These include increased fidelity to program content, reduced costs, and the potential for broad dissemination.10,11 Furthermore, recent studies comparing computer-based communication skill training to in-person training have found evidence for greater skill development via computerized administration.17 Given these possible benefits, we were encouraged to find immediate differences in attitudes, self-efficacy, and assertiveness skills after a brief online intervention, with effect sizes comparable to more time-intensive in-person interventions.16 In the short term, this program could be useful, either as a stand-alone intervention or as a supplement to existing evidence-based sexual health curricula that are more time- and resource-intensive.6
However, several of these treatment effects had diminished within 4 months—a common finding among sexual health interventions for youths.32 This suggests that added material or modifications are necessary to enhance the potency of the HEART program. Sexual assertiveness and negotiation skills are difficult skills to learn and master—even for adults33; thus, youths will likely need ongoing modeling and opportunities to practice and refine these skills beyond what a 45-minute intervention can provide. Furthermore, whereas computerized administration may help youths learn skills in a controlled environment, it is likely that ongoing practice in “real-life” settings will help them sustain communication skills over time. In addition, as adolescents develop and their sexual interests and experiences change, providing ongoing sexual health resources and opportunities to practice the communication skills that can support healthy sexuality is critical.22 Future research should expand the HEART intervention and evaluate program impacts on behavior change over time.
A few limitations are worth considering. First, we recruited a school-based sample of girls from the southeastern United States; results may not generalize to out-of-school youths or girls in other parts of the country. Second, because of logistical considerations, we only assessed behavioral assertiveness skills at immediate posttest. We, thus, could not establish that groups were equivalent on this measure at pretest or model changes in these skills over time. Given the promising results of this trial, we plan to extend this work in a larger, longitudinal sample of youths and examine possible behavior change in condom use. Third, all assessments occurred in school; although we emphasized confidentiality and put procedures in place to protect privacy and encourage honest responding, students still may have underreported their sexual behavior in this context. Finally, this program was designed specifically for adolescent girls. We chose to focus on girls for initial intervention development because, compared with boys, girls are at increased risk for STDs and are more heavily reliant on verbal negotiation for condom use.34 Yet we recognize it is critical to involve boys in sexual education efforts. A prime focus for future studies will be to extend HEART to boys, particularly young men who have sex with men who are at heightened risk for HIV.35,36
With these limitations in mind, this study also has several notable strengths. These include the rigorous assessment with a randomized trial, the inclusion of a behavioral index of assertiveness skills, and the focus on sexual communication skill development within an online delivery platform. Importantly, when we compare HEART to in-person programs with communication outcomes, our program has similar impacts.16 In addition, we found the effects of this program to be largely consistent for White, Black, and Hispanic youths and for sexually active and non–sexually active youth. With these findings, the HEART program holds the potential to be an exciting addition to the growing array of digital sexual health interventions available to youths.
ACKNOWLEDGMENTS
This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health (R00 HD075654, K24 HD069204), the North Carolina State College of Humanities and Social Sciences Research Office, and the University of North Carolina at Chapel Hill Center for AIDS Research (P30 AI50410). Funding for technical expertise was provided by the University of North Carolina Communication for Health Applications and Interventions Core, a National Institutes of Health–funded facility (P30 DK56350, P30 CA16086).
Note. Views expressed in this article are those of the authors and do not necessarily reflect those of the National Institutes of Health.
HUMAN PARTICIPANT PROTECTION
All study procedures were approved by the North Carolina State University institutional review board.
Footnotes
See also Bull, p. 18.
REFERENCES
- 1.Centers for Disease Control and Prevention. About teen pregnancy. 2016. Available at: http://www.cdc.gov/teenpregnancy/about/index.htm. Accessed October 4, 2017.
- 2. Sexually transmitted disease surveillance. Atlanta, GA: Centers for Disease Control and Prevention; 2015.
- 3.Forhan SE, Gottlieb SL, Sternberg MR et al. Prevalence of sexually transmitted infections among female adolescents aged 14 to 19 in the United States. Pediatrics. 2009;124(6):1505–1512. doi: 10.1542/peds.2009-0674. [DOI] [PubMed] [Google Scholar]
- 4.Haggerty CL, Gottlieb SL, Taylor BD, Low N, Xu F, Ness RB. Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis. 2010;201(suppl 2):S134–S155. doi: 10.1086/652395. [DOI] [PubMed] [Google Scholar]
- 5.Hood JE, Friedman AL. Unveiling the hidden epidemic: a review of stigma associated with sexually transmissible infections. Sex Health. 2011;8(2):159–170. doi: 10.1071/SH10070. [DOI] [PubMed] [Google Scholar]
- 6.Goesling B, Colman S, Trenholm C, Terzian M, Moore K. Programs to reduce teen pregnancy, sexually transmitted infections, and associated sexual risk behaviors: a systematic review. J Adolesc Health. 2014;54(5):499–507. doi: 10.1016/j.jadohealth.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 7. Evidence-based programs at-a-glance. Washington, DC: Office of Adolescent Health; 2016.
- 8.Bailey JV, Murray E, Rait G et al. Interactive computer-based interventions for sexual health promotion. Cochrane Database Syst Rev. 2010;(9):CD006483. doi: 10.1002/14651858.CD006483.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Buhi ER. Digital health and AJPH: the time has come! Am J Public Health. 2015;105(3):420. doi: 10.2105/AJPH.2015.302585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lightfoot M, Woods WJ. The online space presents a unique opportunity for psychological sciences to improve the health of youth. Am Psychol. 2013;68(9):888–889. doi: 10.1037/a0035051. [DOI] [PubMed] [Google Scholar]
- 11.Chou WY, Prestin A, Lyons C, Wen KY. Web 2.0 for health promotion: reviewing the current evidence. Am J Public Health. 2013;103(1):e9–e18. doi: 10.2105/AJPH.2012.301071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23(1):107–115. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- 13.Lenhart A, Duggan M, Perrin A, Stepler R, Rainie H, Parker K. Teens, social media & technology overview 2015. Washington, DC: Pew Research Center; 2015. [Google Scholar]
- 14.Widman L, Golin CE, Noar SM, Massey J, Prinstein MP. ProjectHeartForGirls.com: development of a Web-based HIV/STD prevention program for adolescent girls emphasizing sexual communication skills. AIDS Educ Prev. 2016;28(5):365–377. doi: 10.1521/aeap.2016.28.5.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Widman L, Noar SM, Choukas-Bradley S, Francis D. Adolescent sexual health communication and condom use: a meta-analysis. Health Psychol. 2014;33(10):1113–1124. doi: 10.1037/hea0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson BT, Scott-Sheldon LJ, Huedo-Medina TB, Carey MP. Interventions to reduce sexual risk for human immunodeficiency virus in adolescents: a meta-analysis of trials, 1985–2008. Arch Pediatr Adolesc Med. 2011;165(1):77–84. doi: 10.1001/archpediatrics.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamilton G, Ortega R, Hochstetler V, Pierson K, Lin P, Lowes S. Teaching communication skills to hospice teams: comparing the effectiveness of a communication skills laboratory with in-person, second life, and phone role-playing. Am J Hosp Palliat Care. 2014;31(6):611–618. doi: 10.1177/1049909113504481. [DOI] [PubMed] [Google Scholar]
- 18.Edgar T, Noar SM, Freimuth VS, editors. Communication Perspectives on HIV/AIDS for the 21st Century. New York, NY: Lawrence Erlbaum; 2008. [Google Scholar]
- 19.Widman L, Golin CE, Kamke K, Massey J, Prinstein MP. Feasibility and acceptability of a Web-based HIV/STD prevention program for adolescent girls targeting sexual communication skills. Health Educ Res. 2017;32(4):343–352. doi: 10.1093/her/cyx048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fishbein M, Ajzen I. Predicting and Changing Behavior: The Reasoned Action Approach. New York, NY: Psychology Press; 2010. [Google Scholar]
- 21.Reyna VF. A theory of medical decision making and health: fuzzy trace theory. Med Decis Making. 2008;28(6):850–865. doi: 10.1177/0272989X08327066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fortenberry JD. The evolving sexual health paradigm: transforming definitions into sexual health practices. AIDS. 2013;27(suppl 1):S127–S133. doi: 10.1097/QAD.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 23.Burnette J, Russel VM, Hoyt C, Ordivas K, Widman L. An online growth mindset intervention in a sample of rural adolescent girls. Br J Educ Psychol. doi: 10.1111/bjep.12192. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burnette JL, Finkel EJ. Buffering against weight gain following dieting setbacks: an implicit theory intervention. J Exp Soc Psychol. 2012;48(3):721–725. [Google Scholar]
- 25.Forsyth AD, Carey MP, Fuqua RW. Evaluation of the validity of the Condom Use Self-Efficacy Scale (CUSES) in young men using two behavioral simulations. Health Psychol. 1997;16(2):175–178. doi: 10.1037//0278-6133.16.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gordon CM, Carey MP, Carey KB. Effects of a drinking event on behavioral skills and condom attitudes in men: implications for HIV risk from a controlled experiment. Health Psychol. 1997;16(5):490–495. doi: 10.1037//0278-6133.16.5.490. [DOI] [PubMed] [Google Scholar]
- 27.Snell WE., Jr . The multidimensional sexual self-concept questionnaire. In: Davis CM, Yarber WL, Baurerman R, Schreer G, Davis SL, editors. Sexuality-Related Measures: A Compendium. 2nd ed. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 28.Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: links to psychopathology and peer relationships. J Am Acad Child Adolesc Psychiatry. 2001;40(6):642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown LK, Hadley W, Donenberg GR et al. Project STYLE: a multisite RCT for HIV prevention among youths in mental health treatment. Psychiatr Serv. 2014;65(3):338–344. doi: 10.1176/appi.ps.201300095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.St Lawrence JS, Reitman D, Jefferson KW, Alleyne E, Brasfield TL, Shirley A. Factor structure and validation of an adolescent version of the Condom Attitude Scale: an instrument for measuring adolescents’ attitudes toward condoms. Psychol Assess. 1994;6(4):352–359. [Google Scholar]
- 31.Basen-Engquist K, Mâsse LC, Coyle K et al. Validity of scales measuring the psychosocial determinants of HIV/STD-related risk behavior in adolescents. Health Educ Res. 1999;14(1):25–38. doi: 10.1093/her/14.1.25. [DOI] [PubMed] [Google Scholar]
- 32.Bangi A, Dolcini MM, Harper GW, Boyer CB, Pollack LM. Psychosocial outcomes of sexual risk reduction in a brief intervention for urban African American female adolescents. J HIV AIDS Soc Serv. 2013;12(2):146–159. doi: 10.1080/15381501.2013.768949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Byers ES. Beyond the birds and the bees and was it good for you?: Thirty years of research on sexual communication. Can Psychol. 2011;52(1):20–28. [Google Scholar]
- 34.Amaro H, Raj A. On the margin: power and women’s HIV risk reduction strategies. Sex Roles. 2000;42(7-8):723–749. [Google Scholar]
- 35.Centers for Disease Control and Prevention. HIV among youth. 2017. Available at: https://www.cdc.gov/hiv/group/age/youth. Accessed October 4, 2017.
- 36.Koenig LJ, Hoyer D, Purcell DW, Zaza S, Mermin J. Young people and HIV: a call to action. Am J Public Health. 2016;106(3):402–405. doi: 10.2105/AJPH.2015.302979. [DOI] [PMC free article] [PubMed] [Google Scholar]