Abstract
This study aimed to compare patterns of sedentary behaviour (SB) and physical activity (PA) in people following curative intent treatment for non-small cell lung cancer (NSCLC) with healthy controls. Participants 6–10 weeks following lobectomy for NSCLC and healthy controls wore two activity monitors for 7 days. Waking hours were divided into time spent in SB (<1.5 metabolic equivalent of tasks (METs)), light intensity PA (LIPA ≥ 1.5 to <3.0METs) and moderate-to-vigorous intensity PA (≥3.0METs). Daily steps were also recorded. Data were available in 20 participants with NSCLC (13 females; 68 ± 10 years) and 20 healthy controls (13 females; 69 ± 5 years). The NSCLC group accumulated a greater percentage of time in SB in uninterrupted bouts ≥30 minutes (49% vs. 42%; p = 0.048). Further, the NSCLC group spent a lower percentage of waking hours in LIPA (21 ± 9% vs. 26 ± 8%; p = 0.04) and accumulated a lower percentage of time in this domain in uninterrupted bouts ≥10 minutes (13% vs. 19%; p = 0.025). The NSCLC group also had a lower daily step count (8863 ± 3737 vs. 11,856 ± 3024 steps/day; p = 0.009). Time spent in moderate-to-vigorous intensity PA was similar in both groups (p = 0.92). People following curative intent treatment for NSCLC spend more time in prolonged bouts of SB at the expense of LIPA.
Keywords: Lung cancer, non-small cell, physical activity, sedentary behaviour, treatment, lobectomy
In both health and disease, there is increased interest in the role that time spent in sedentary behaviour (SB) and physical activity (PA) may play in health outcomes. The health benefits of participating in moderate-to-vigorous intensity PA (MVPA) have been well reported.1 Although undertaking MVPA is important, performing tasks at this intensity represents a small proportion of waking hours.2 SB is postures or behaviours undertaken during waking hours in sitting or a reclined posture, which require low energy expenditure (≤1.5 metabolic equivalent of tasks (METs)).3 Independent of the time spent in MVPA, increased time spent in SB is a risk factor for cardiometabolic disease.4 In addition to the total time spent in SB, prolonged uninterrupted bouts of SB are linked with deleterious health outcomes.4 These data have led to public health campaigns that seek to reduce total time in SB and interrupt SB every 30 minutes with light intensity PA (LIPA).5
In people with lung cancer, data on PA and SB are limited. Studies have reported low levels of PA in people with non-small cell lung cancer (NSCLC),6,7 however, these studies have not explored SB or the way in which time is accumulated in SB or PA performed at any intensity. Obtaining data on patterns of SB and PA in this population and comparing these data with those collected in healthy controls will allow health professionals to provide novel targets for rehabilitation interventions. Hence, the aim of this study was to compare patterns of SB and PA in people following curative intent treatment for NSCLC with healthy controls.
People were included if they were 6–10 weeks following lobectomy for NSCLC or, for those who required adjuvant chemotherapy, 4–8 weeks following chemotherapy completion. Age and gender-matched healthy controls, without spirometric evidence of airflow obstruction, were also recruited. The study was approved by Human Research Ethics Committees at three institutions (approval nos 2011/105, RA-11/033 and HR178/2011). Participants were asked to wear two activity monitors, for 7 consecutive days, during waking hours. SB and PA were assessed using the SenseWear armband (SAB; BodyMedia Inc., Pittsburgh, Pennsylvania, USA).8,9 Daily step count was measured using the StepWatch activity monitor (SAM; Cyma Corporation, Manchester, Connecticut, USA).10 Exposure variation analysis11 was undertaken, using data from the SAB, to calculate the proportion of waking hours spent in SB (<1.5 METs), LIPA (≥1.5 and <3 METs) and MVPA (≥ 3 METs).1 Time spent in SB was analysed in epochs of 0 to < 30 minutes and ≥ 30 minutes and time spent in LIPA and MVPA were analysed in epochs of 0 to <10 minutes and ≥10 minutes.
Characteristics of the two groups are presented in Table 1. Comparison of the percentage of waking hours spent in SB, LIPA and MVPA between groups are presented in Figure 1. Table 2 shows the patterns of accumulation of SB, LIPA and MVPA. Daily step count was lower in the NSCLC group compared with healthy controls (8863 ±3737steps/day vs. 11,856 ± 3024 steps/day; p = 0.009).
Table 1.
Participant characteristics.
| Variables | NSCLC group (n = 20) mean ± SD | Healthy controls (n = 20) mean ± SD | p Value | ||
|---|---|---|---|---|---|
| Age (year) | 68 ± 10 | 69 ± 5 | 0.67 | ||
| Height (cm) | 165 ± 13 | 167 ± 6 | 0.36 | ||
| Weight (kg) | 72 ± 21 | 71 ± 14 | 0.82 | ||
| BMI (kg m−2) | 26 ± 6 | 25 ± 4 | 0.79 | ||
| Smoking (pack·years) | 35 ± 17 | 0.3 ± 0.9 | <0.001 | ||
| FEV1 (L) | 1.69 ± 0.50 | 2.68 ± 0.54 | <0.001 | ||
| FEV1 (% predicted) | 67 ± 17 | 103 ± 15 | <0.001 | ||
| FVC (L) | 2.74 ± 0.74 | 3.44 ± 0.75 | <0.001 | ||
| FVC (% predicted) | 81 ± 10 | 99 ± 15 | <0.001 | ||
| n | % | n | % | ||
| Gender, male/female | 7/13 | 35/65 | 7/13 | 35/65 | 0.92 |
| Smoking status | |||||
| Current smoker | 1 | 5 | 0 | 0 | 0.34 |
| Ex-smoker | 16 | 80 | 2 | 10 | <0.001 |
| Never smoked | 3 | 15 | 18 | 90 | <0.001 |
| COPD | 11 | 55 | 0 | 0 | <0.001 |
| Other comorbidities | |||||
| Hypertension | 11 | 55 | 2 | 10 | <0.001 |
| Stable ischaemic heart disease | 3 | 15 | 1 | 5 | 0.25 |
| Diabetes Mellitus | 3 | 15 | 1 | 5 | 0.25 |
| Dyslipidaemia | 5 | 25 | 6 | 30 | 0.38 |
| GORD | 3 | 15 | 1 | 5 | 0.39 |
| Hypothyroidism | 2 | 10 | 3 | 15 | 0.62 |
| Type of NSCLC | |||||
| Adenocarcinoma | 14 | 70 | |||
| Squamous cell carcinoma | 5 | 25 | |||
| Large cell carcinoma | 1 | 5 | |||
| NSCLC stage | |||||
| I | 15 | 75 | |||
| II | 3 | 15 | |||
| IIIA | 2 | 10 | |||
| Types of surgery | |||||
| Open | 8 | 40 | |||
| VATS | 12 | 60 | |||
| Adjuvant chemotherapy | 2 | 10 | |||
BMI: body-mass index; COPD: chronic obstructive pulmonary disease; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; GORD: gastro-oesophageal reflux disease; MVV: maximum voluntary ventilation; NSCLC: non-small cell lung cancer; SD: standard deviation; VATS: video-assisted thoracoscopic surgery.
Figure 1.
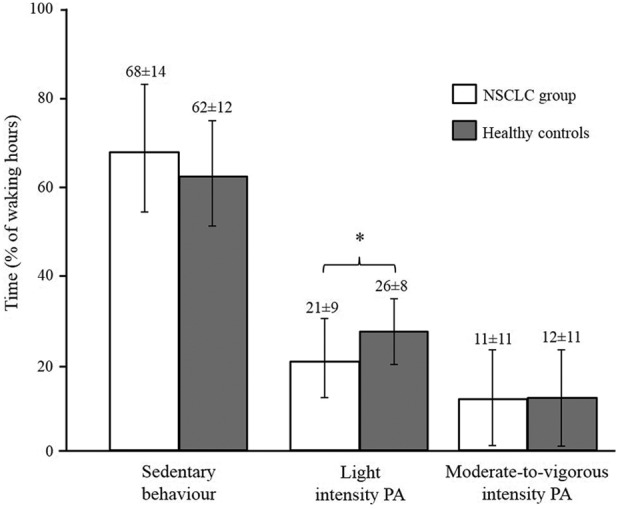
Comparison of the time, expressed as a percentage of waking hours, spent in, LIPA and moderate-to-vigorous intensity physical activity between groups. Data are expressed as mean ± standard deviation. NSCLC: non-small cell lung cancer; PA: physical activity; SB: sedentary behaviour; LIPA: light-intensity physical activity. *p = 0.04.
Table 2.
Patterns of accumulation of SB, light and moderate-to-vigorous intensity PA.a
| Variables | NSCLC group (n = 20) | Healthy controls (n = 20) | p Value |
|---|---|---|---|
| Percentage of total time in SB accumulated in bouts ≥30 minutes | 49 (42–65) | 42 (30–58) | 0.048 |
| Percentage of total time in LIPA accumulated in bouts ≥10 minutes | 13 (5–21) | 19 (13–29) | 0.025 |
| Percentage of total time in moderate-to-vigorous PA accumulated in bouts ≥10 minutes | 30 (17–40) | 26 (13–50) | 0.45 |
NSCLC: non-small cell lung cancer; PA: physical activity; SB: sedentary behaviour; LIPA: light-intensity physical activity.
aData are expressed as median (interquartile range).
The results demonstrate that, compared to healthy controls, people following curative intent treatment for NSCLC took fewer steps each day. Although there was no difference in total time spent in SB, the NSCLC group accumulated a greater proportion of time in SB in prolonged, uninterrupted periods. They also spent less time in LIPA and accumulated less time in this domain in uninterrupted bouts ≥10 minutes. In summary, people following curative intent treatment for NSCLC spend more time in prolonged bouts of SB at the expense of LIPA. Interventions for this population should aim at breaking up time spent in prolonged periods SB with LIPA and increasing the time spent in bouts ≥10 minutes of LIPA.
Acknowledgements
VC is supported by the Curtin Strategic International Research Scholarship (CSIRS) and Lung Institute of Western Australia (LIWA) PhD Top-up Scholarship.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study received funding from Sir Charles Gairdner Hospital Research Advisory Committee (grant number: 2011/12/013).
References
- 1. Garber CE, Blissmer B, Deschenes MR, et al. American college of sports medicine position stand. quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011; 43: 1334–1359. [DOI] [PubMed] [Google Scholar]
- 2. Hill K, Gardiner P, Cavalheri V, et al. Physical activity and sedentary behaviour: applying lessons to chronic obstructive pulmonary disease. Intern Med J 2015; 45(5): 474–482. [DOI] [PubMed] [Google Scholar]
- 3. Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab 2012; 37: 540–542. [DOI] [PubMed] [Google Scholar]
- 4. Healy GN, Matthews CE, Dunstan DW, et al. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J 2011; 32: 590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Owen N, Sugiyama T, Eakin EE, et al. Adults’ sedentary behavior determinants and interventions. Am J Prev Med 2011; 41: 189–196. [DOI] [PubMed] [Google Scholar]
- 6. Granger CL, McDonald CF, Irving L, et al. Low physical activity levels and functional decline in individuals with lung cancer. Lung Cancer 2014; 83: 292–299. [DOI] [PubMed] [Google Scholar]
- 7. Granger CL, Denehy L, McDonald CF, et al. Physical activity measured using global positioning system tracking in non-small cell lung cancer: an observational study. Integr Cancer Ther 2014; 13: 482–492. [DOI] [PubMed] [Google Scholar]
- 8. Hill K, Dolmage TE, Woon L, et al. Measurement properties of the SenseWear armband in adults with chronic obstructive pulmonary disease. Thorax 2010; 65: 486–491. [DOI] [PubMed] [Google Scholar]
- 9. Cavalheri V, Donaria L, Ferreira T, et al. Energy expenditure during daily activities as measured by two motion sensors in patients with COPD. Respir Med 2011; 105: 922–929. [DOI] [PubMed] [Google Scholar]
- 10. Cindy Ng LW, Jenkins S, Hill K. Accuracy and responsiveness of the stepwatch activity monitor and ActivPAL in patients with COPD when walking with and without a rollator. Disabil Rehabil 2012; 34: 1317–1322. [DOI] [PubMed] [Google Scholar]
- 11. Straker L, Campbell A, Mathiassen S, et al. Capturing the pattern of physical activity and sedentary behavior: exposure variation analysis of accelerometer data. J Phys Act Health. 2014; 11: 614–625. [DOI] [PubMed] [Google Scholar]


