Abstract
At least 5% of all intensive care unit patients require prolonged respiratory support. Multiple factors have been suggested as possible predictors of successful respiratory weaning so far. We sought to verify whether the Acute Physiology and Chronic Health Evaluation II (APACHE II) can predict freedom from prolonged mechanical ventilation (PMV) in patients treated in a regional weaning centre. The study group comprised 130 consecutive patients (age; median (interquartile range): 71 (62–77) years), hospitalized between 1 January 2012, and 31 December 2013. APACHE II score was assessed based on the worst values taken during the first 24 hours after admission. Glasgow coma scale was excluded from calculations due to the likely influence of sedative agents. The outcome was defined as freedom from mechanical ventilation, with or without tracheostomy on discharge. Among survivors (n = 115), 88.2% were successfully liberated from mechanical ventilation and 60.9% from tracheostomy. APACHE II failed to predict freedom from mechanical ventilation (area under the receiver–operating characteristic curve [AUROC] = 0.534; 95% confidence interval [CI]: 0.439–0.628; p = 0.65) and tracheostomy tube removal (AUROC = 0.527; 95% CI: 0.431–0.621; p = 0.63). Weaning outcome was unrelated to the aetiology of respiratory failure on admission (p = 0.41). APACHE II cannot predict weaning outcome in patients requiring PMV.
Keywords: Prolonged mechanical ventilation, weaning, outcome, APACHE score, prediction
Introduction
The Acute Physiology and Chronic Health Evaluation II (APACHE II) scale includes 12 physiological and laboratory parameters and two disease-related variables.1 Due to its complexity, the final score corresponds with the disease severity.1,2 Although APACHE II has become the most recognized and universal tool used to predict mortality in patients admitted to the intensive care unit (ICU),2 its utility was also confirmed in several other scenarios, including surgery and internal medicine.3,4 Furthermore, several studies emphasized the predictive role of this scoring system in patients with respiratory failure.5,6
While it is estimated that up to 75% of all ICU patients require mechanical ventilation,7 half of them experience difficult weaning, and at least 5% require prolonged respiratory support.8 Weaning centres were established more than 20 years ago for treatment of subjects who cannot be easily liberated from mechanical ventilation.9 Currently, these specialized units succeed in respiratory weaning in most cases10,11; however, the ultimate outcome in a patient requiring weaning depends on a plethora of factors, both respiratory and non-respiratory.12,13 None of the available scales or scores has been validated for clinical outcome prediction in this setting. This prompted us to investigate whether APACHE II score can predict freedom from prolonged mechanical ventilation (PMV) in patients treated in a regional weaning centre.
Material and methods
This retrospective analysis included 130 consecutive patients admitted to a regional weaning centre between 1 January 2012, and 31 December 2013.
Indications for admission to a weaning centre were in agreement to the German Respiratory Society guidelines.14 Treatment strategy and weaning procedures were implemented according to the nationwide recommendations,14 after adjustment to local standards, as previously described.15
Basic demographic and clinical data were retrieved from medical records. Laboratory data were recorded on the day of admission. Physiological data were recorded in a 3-hour-long intervals during the first day. The APACHE II score was calculated based on the worst values taken during the first 24 hours after admission. To eliminate possible confounding effect of analgesic and sedative agents, we excluded Glasgow coma scale (GCS) from scoring (baseline median Richmond Agitation–Sedation scale of -1 points; interquartile range (IQR) -2 to +1).
The primary outcome in this study was freedom from mechanical ventilation, regardless of the need for tracheostomy. We additionally assessed the number of patients who had a tracheostomy tube removed before discharge.
Statistical analysis
Statistical analysis was performed using MedCalc Statistical Software version 14.8.1 (MedCalc Software bvba, Ostend, Belgium). Continuous variables are expressed as median and IQR. Qualitative variables are expressed as numbers (percentage). The normality of distribution was verified using the Shapiro–Wilk test. Inter-group differences for quantitative variables were assessed using Mann–Whitney U test. The area under the receiver–operating characteristic curve (AUROC) was calculated to determine the ability of the APACHE II score to predict weaning outcome. A p value <0.05 was considered significant.
Results
The final analysis comprised 130 patients in median age of 71 (IQR 62–77) years. All patients were previously hospitalized in medical/surgical ICU and/or high dependency post-operative care units for a median time of 22 (IQR 15–33) days. There were 87 (66.9%) males in the study group. The APACHE II (excluding GCS) median score was 11 (IQR 9–14) points. The aetiology of respiratory failure requiring mechanical ventilation is presented in Table 1. Post-operative respiratory insufficiency was the most frequent reason of PMV (n = 76, 58.5%). Among them, 51 patients underwent cardiac surgery (including isolated coronary, n = 24; isolated valve procedure, n = 7; coronary + valve, n = 9; aortic aneurysm, n = 9; other, n = 2) and 17 subjects gastrointestinal surgery. All patients were in American Society of Anesthesiologists Physical Status Classification System classes II and III. Emergency surgery was performed in 43 (i.e. 56.6% of 76) patients.
Table 1.
Aetiology of respiratory failure.
| Main condition | % |
|---|---|
| Post-operative | 58.5 |
| Pneumonia | 13.8 |
| COPD exacerbation | 5.4 |
| Post-cardiac arrest syndrome | 5.4 |
| Stroke/intracranial bleeding | 5.3 |
| Post-traumatic | 4.7 |
| Circulatory failure | 3.1 |
| Others | 3.8 |
COPD: Chronic obstructive pulmonary disease.
On admission, 112 (86%) patients were ventilated by tracheostomy and 18 (14%) had an endotracheal tube. One patient required synchronized intermittent mandatory ventilation, 38 were on bi-level positive airway pressure ventilation (BIPAP) and 91 on continuous positive airway pressure support (CPAP). Baseline blood gas analysis findings with basic ventilator’s settings are shown in Table 2. Median arterial oxygen partial pressure/fraction of inspired oxygen ratio was 233 (IQR 185–289) mmHg.
Table 2.
Baseline blood gas analysis findings and ventilator’s settings.
| Parameter | Median (IQR) |
|---|---|
| Blood gas analysis | |
| pH | 7.47 (7.42–7.50) |
| PaO2 (mmHg) | 94.5 (81.0–116.0) |
| SpO2 (%) | 98 (96–99) |
| PaCO2 (mmHg) | 43.0 (37.0–49.0) |
| HCO3 − (mmol/l) | 30.2 (27.8–33.6) |
| BE (mmol/l) | 7.0 (4.1–10.2) |
| ScvO2 (%) | 69 (64–75) |
| Lactate concentration (mmol/l) | 0.98 (0.81–1.23) |
| Ventilator’s settings | |
| FiO2 | 0.40 (0.40–0.45) |
| Respiratory ratio (1/minute)a | 14 (12–14) |
| PEEP (mbar) | 7.0 (6.0–8.0) |
| PS (mbar) | 12.0 (10.0–14.0) |
| Inspiratory pressure (mbar)a | 22.0 (19.0–24.0) |
IQR: interquartile range; BE: base excess; FiO2: fraction of inspired oxygen; PaCO2: arterial carbon dioxide partial pressure; PaO2: arterial oxygen partial pressure; PEEP: positive end-expiratory pressure; PS: pressure support; ScvO2: central venous oxygen saturation; SpO2: arterial oxygen saturation; HCO3 −: bicarbonate.
aFor patients on synchronized intermittent mandatory ventilation/bi-level positive airway pressure ventilation (n = 39).
Median hospital stay in a weaning centre was 28 (IQR 20–39) days. Fifteen subjects died, and 115 patients were successfully discharged. Among survivors, 102 (i.e. 88.2% of 115) patients remained independent of mechanical ventilation. Forty-five subjects had tracheostomy at discharge, and 13 of them required ventilatory support. Seventy patients were fully weaned (with withdrawal of an endotracheal/tracheostomy tube; i.e. 60.9% of 115; Figure 1).
Figure 1.
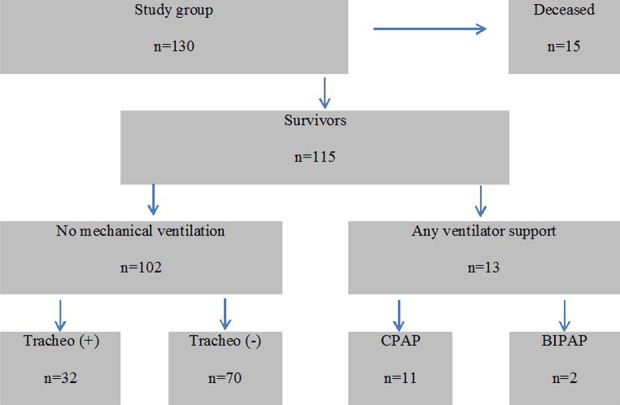
Patients’ flow chart by weaning outcome.
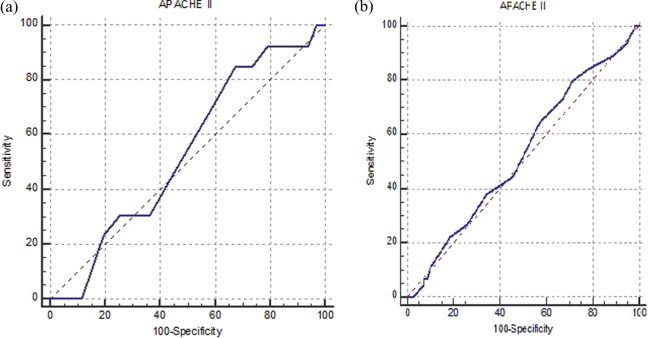
The APACHE II score values did not differ between patients who were independent of mechanical ventilation (median = 11 points; IQR 8–14) and those who still required respiratory support (median = 11 points; IQR 10–14.25; p = 0.68). It also did not differ between subjects with/without tracheostomy or those requiring CPAP/BIPAP on discharge (Table 3). The APACHE II failed to predict freedom from mechanical ventilation (AUROC = 0.534; 95% CI: 0.439–0.628; p = 0.65) and removal of tracheostomy tube (AUROC = 0.527; 95% CI: 0.431–0.621; p = 0.63; Figure 2). Weaning outcome was unrelated to the aetiology of respiratory failure on admission (p = 0.41; Figure 3).
Table 3.
APACHE II score and weaning outcome.a
| APACHE II | Weaned (+) | Weaned (−) | ||
|---|---|---|---|---|
| Tracheo (+) | Tracheo (−) | CPAP | BIPAP | |
| Points | 11 (9–13.5) | 11 (8–14) | 10 (8–11) | 12 (11.25–15) |
APACHE II: Acute Physiology and Chronic Health Evaluation II; CPAP: continuous positive airway pressure support; BIPAP: bi-level positive airway pressure ventilation.
aall p values > 0.05.
Figure 2.
Prediction of ventilatory independence (a) with or without tracheostomy and (b) without tracheostomy by APACHE II score. APACHE II: Acute Physiology and Chronic Health Evaluation II.
Figure 3.
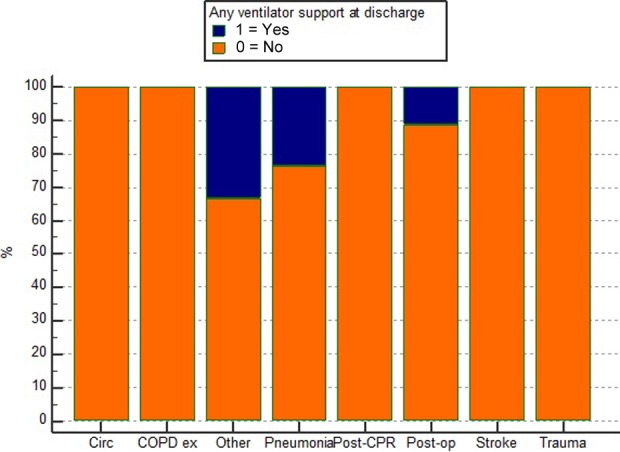
Ventilatory independence (with or without tracheostomy) by aetiology of respiratory failure.
Discussion
This study demonstrates that APACHE II failed to predict successful weaning from PMV. Since APACHE II was exclusively studied in patients of multidisciplinary ICUs and high dependency units, little is known about its diagnostic utility in patients treated in weaning centres. This scoring system is the most commonly used tool for outcome prediction worldwide. It is well known by almost all staff members, including physicians, nurses, physical therapist and social workers. Also, there is no single predictor of clinical outcome in PMV patients, as it depends on multiple respiratory and non-respiratory factors. Therefore, in this short research, we aimed to assess the ability of the APACHE II scoring system to predict successful weaning.
The number of PMV patients liberated from mechanical ventilation has increased in the last decade in Germany.16 Ventilator weaning requires sophisticated and individualized care. On the one hand, the dangers of mechanical ventilation make it an imperative to wean patients at the earliest possible time.17 On the other hand, premature weaning and extubation can trigger significant respiratory distress, which can cause setbacks in the patient’s clinical course, including reinstitution of ventilator support and hemodynamic instability.17 These factors correspond with higher mortality and prolonged ICU length of stay.18 Therefore, following the current guidelines,14 we avoided an aggressive approach for early extubation, as reflected by a slightly longer weaning period, when compared to the existing literature data.9,19,20 Possibly, this approach resulted in a considerably high level of ventilator independency. Weaning success was achieved in 88.2% of survivors, with 60.9% being discharged without tracheostomy. These findings are consistent with the latest statistics from experienced weaning units.21,22 It’s worth mentioning that Damuth et al.23 in a comprehensive review found that weaning outcomes were worse in studies from the United States than from Europe, with pooled frequency of liberation from mechanical ventilation of 50% (US data: 47% vs. international data: 63%).
Proper staffing, well-defined short-term and long-term goals and attention to psychological and social problems represent crucial determinants of weaning success.
Many clinical parameters have been proposed as predictors of weaning outcome so far. Although those related to the physiologic status of the respiratory system are rather useful in patients being ventilated for shorter time periods,24 a broad spectrum of non-pulmonary factors may influence weaning in PMV.12,13 Several investigators confirmed the usefulness of the APACHE II scoring in the prediction of weaning success25,26; however, our results are in line with the findings from a few experienced weaning units.11,19,27 We recognize four key explanations of this discrepancy. One is a relatively small study group. The second is heterogeneity of subjects – each centre has specific admission criteria and a unique patient group in terms of their demographics, principal diagnoses and comorbidities. Third, none of the scoring systems is universal for all patients.28 Finally, Safavi and Honarmand29 revealed that the need of MV might be predicted better by the APACHE III (AUROC = 0.89) than the APACHE II (AUROC = 0.74) score, suggesting the potential role of this novel scoring system.
Study limitations
Three possible limitations of this study raise concern. First, our analysis is based on a single-centre retrospective data. On the one hand, the external validity of our findings is therefore limited and cannot be extrapolated to a wider international population. On the other hand, retrospective analysis enables the most powerful data from single-centre observations. In weaning units, it is an acknowledged method to present the results because they usually constitute low-volume facilities, treating chronic subjects. Second, we did not include comprehensive data regarding sedation protocols and spontaneous breathing trials. However, all weaning procedures were standardized and consistent with current guidelines.14 Finally, we lack follow-up data regarding the rates of hospital readmissions, reinstitution of MV and long-term mortality.
Conclusions
Although APACHE II scale has been verified as an acknowledged predictor of mortality in the ICU setting, it cannot predict weaning from PMV.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13: 818–829. [PubMed] [Google Scholar]
- 2. Zimmerman JE, Kramer AA. A history of outcome prediction in the ICU. Curr Opin Crit Care 2014; 20: 550–556. [DOI] [PubMed] [Google Scholar]
- 3. Hong S, Wang S, Xu G, et al. Evaluation of the POSSUM, p-POSSUM, o-POSSUM, and APACHE II scoring systems in predicting postoperative mortality and morbidity in gastric cancer patients. Asian J Surg. Epub ahead of print 23 September 2015. DOI: 10.1016/j.asjsur.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 4. Cho JH, Kim TN, Chung HH, et al. Comparison of scoring systems in predicting the severity of acute pancreatitis. World J Gastroenterol 2015; 21: 2387–2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fadaizadeh L, Tamadon R, Saeedfar K, et al. Performance assessment of acute physiology and chronic health evaluation II and simplified acute physiology score II in a referral respiratory intensive care unit in Iran. Acta Anaesthesiol Taiwan 2012; 50: 59–62. [DOI] [PubMed] [Google Scholar]
- 6. Aydoğdu M, Ozyilmaz E, Aksoy H, et al. Mortality prediction in community-acquired pneumonia requiring mechanical ventilation; values of pneumonia and intensive care unit severity scores. TuberkToraks 2010; 58: 25–34. [PubMed] [Google Scholar]
- 7. Kübler A, Maciejewski D, Adamik B, et al. Mechanical ventilation in ICUs in Poland: a multi-center point-prevalence study. Med Sci Monit 2013; 19: 424–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peñuelas O, Frutos-Vivar F, Fernández C, et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am J Respir Crit Care Med 2011; 184: 430–437. [DOI] [PubMed] [Google Scholar]
- 9. Dasgupta A, Rice R, Mascha E, et al. Four-year experience with a unit for long-term ventilation (respiratory special care unit) at the Cleveland Clinic Foundation. Chest 1999; 116: 447–455. [DOI] [PubMed] [Google Scholar]
- 10. Rose L, Fraser IM. Patient characteristics and outcomes of a provincial prolonged-ventilation weaning centre: a retrospective cohort study. Can Respir J 2012; 19: 216–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mamary AJ, Kondapaneni S, Vance GB, et al. Survival in patients receiving prolonged ventilation: factors that influence outcome. Clin Med Insights Circ Respir Pulm Med 2011; 5: 17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seneff MG, Zimmerman JE, Knaus WA, et al. Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest 1996; 110: 469–479. [DOI] [PubMed] [Google Scholar]
- 13. Clark PA, Lettieri CJ. Clinical model for predicting prolonged mechanical ventilation. J Crit Care 2013; 28: 880e1–7. [DOI] [PubMed] [Google Scholar]
- 14. Schönhofer B, Geiseler J, Dellweg D, et al. Prolonged weaning: S2k-guideline published by the German Respiratory Society. Pneumologie 2014; 68: 19–75. [DOI] [PubMed] [Google Scholar]
- 15. Rojek-Jarmuła A, Hombach R, Gierek D, et al. A single-centre seven-year experience with mechanical ventilation weaning. Anaesthesiol Intensive Ther 2015; 47: 204–209. [DOI] [PubMed] [Google Scholar]
- 16. Schönhofer B, Geiseler J, Pfeifer M, et al. WeanNet: a network of weaning units headed by pneumologists. Pneumologie 2014; 68: 737–742. [DOI] [PubMed] [Google Scholar]
- 17. Shaikh H, Morales D, Laghi F. Weaning from mechanical ventilation. Semin Respir Crit Care Med 2014; 35: 451–468. [DOI] [PubMed] [Google Scholar]
- 18. McConville JF, Kress JP. Weaning patients from the ventilator. N Engl J Med 2012; 367: 2233–2239. [DOI] [PubMed] [Google Scholar]
- 19. Pilcher DV, Bailey MJ, Treacher DF, et al. Outcomes, cost and long term survival of patients referred to a regional weaning centre. Thorax 2005; 60: 187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lone NI, Walsh TS. Prolonged mechanical ventilation in critically ill patients: epidemiology, outcomes and modelling the potential cost consequences of establishing a regional weaning unit. Crit Care 2011; 15: R102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barchfeld T, Dellweg D, Böckling S, et al. Weaning from long-term mechanical ventilation: data of a single weaning center from 2007 to 2011. Dtsch Med Wochenschr 2014; 139: 527–533. [DOI] [PubMed] [Google Scholar]
- 22. Oehmichen F, Ketter G, Mertl-Rötzer M, et al. Weaning from prolonged mechanical ventilation in neurological weaning units: an evaluation of the German Working Group for early neurorehabilitation. Nervenarzt 2012; 83: 1300–1307. [DOI] [PubMed] [Google Scholar]
- 23. Damuth E, Mitchell JA, Bartock JL, et al. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med 2015; 3: 544–553. [DOI] [PubMed] [Google Scholar]
- 24. Sporn PH, Morganroth ML. Discontinuation of mechanical ventilation. Clin Chest Med 1988; 9: 113–126. [PubMed] [Google Scholar]
- 25. Schönhofer B, Guo JJ, Suchi S, et al. The use of APACHE II prognostic system in difficult-to-wean patients after long-term mechanical ventilation. Eur J Anaesthesiol 2004; 21: 558–565. [DOI] [PubMed] [Google Scholar]
- 26. Matic I, Titlic M, Dikanovic M, et al. Effects of APACHE II score on mechanical ventilation; prediction and outcome. Acta Anaesthesiol Belg 2007; 58: 177–183. [PubMed] [Google Scholar]
- 27. Quinnell TG, Pilsworth S, Shneerson JM, et al. Prolonged invasive ventilation following acute ventilatory failure in COPD: weaning results, survival, and the role of noninvasive ventilation. Chest 2006; 129: 133–139. [DOI] [PubMed] [Google Scholar]
- 28. Gluck EH. Predicting eventual success or failure to wean in patients receiving long-term mechanical ventilation. Chest 1996; 110: 1018–1024. Erratum in: Chest 1997; 111: 836. [DOI] [PubMed] [Google Scholar]
- 29. Safavi M, Honarmand A. Comparison of infection probability score, APACHE II, and APACHE III scoring systems in predicting need for ventilator and ventilation duration in critically ill patients. Arch Iran Med 2007; 10: 354–360. [PubMed] [Google Scholar]