Abstract
This reports a case of a low-energy ipsilateral femoral shaft and neck fracture in a 69-year-old woman with vitamin D deficiency, who was taking long-term steroids and bisphosphonates. This is a fracture more commonly associated with a high-energy trauma. However, with an ageing global population and an increasing prevalence of bone insufficiency, we predict the incidence of this presentation to increase. Long-term bisphosphonate therapy has been associated with bone insufficiency and an increased rate of delayed union, adding to the complexity of management in these patients. There is currently no consensus regarding the choice of optimal implant or fixation technique to treat this challenging fracture pattern. We discuss the considerations that led to our management approach of a non-overlapping dynamic hip screw and femoral shaft plate construct which achieved uneventful bone healing and a good functional outcome within the first year of follow-up.
Keywords: orthopaedics, orthopaedic and trauma surgery
Background
Atypical femoral shaft fracture patterns in low-energy falls have been associated with bone insufficiency caused by vitamin D deficiency and long-term use of bisphosphonates or steroids.1 Fractures of the femoral neck and ipsilateral shaft are commonly associated with high-energy trauma.2 However, association of an atypical femoral shaft and ipsilateral femoral neck fracture is less common. This is a case report of low-energy ipsilateral femoral shaft and neck fractures in a patient with vitamin D deficiency, who was taking long-term steroids and bisphosphonates. The aims are to describe this rare association, the management decision-making and outcomes from the case.
Case presentation
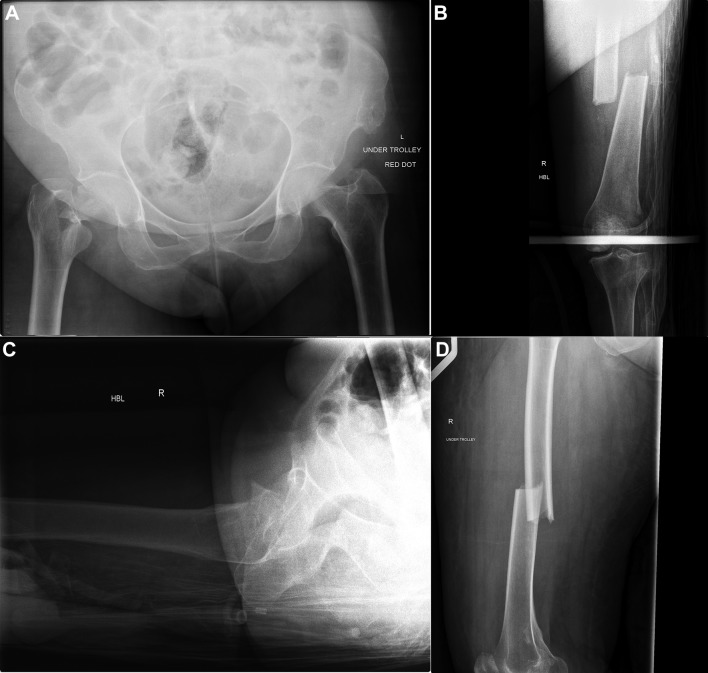
A 69-year-old woman was repatriated to our trauma unit from abroad 2 days following a mechanical fall from a standing height. She was known to have haemophilia (type C), chronic obstructive airway disease (COPD) and vitamin D deficiency secondary to renal insufficiency. She was taking long-term inhaled steroids for her COPD and alendronic acid. Radiographs from the date of injury showed a displaced basicervical fracture of the femoral neck and an ipsilateral transverse femoral diaphyseal fracture. The later displayed all the classical signs of an atypical fracture associated with long-term bisphosphonates: transverse fracture line along the lateral cortex, the presence of a medial spike, thickening of the femoral cortices, absence of comminution and location of the fracture distal to the lesser trochanter (figure 1A–D).3 4
Figure 1.
(A) AP pelvis demonstrating displaced intracapsular fracture. (B) AP femur displaying atypical features of the fracture. (C) Lateral hip. (D) Lateral femur. AP, anteroposterior.
Treatment
Surgical management of the femoral shaft fracture was performed through a lateral subvastus approach. Anatomical reduction was achieved with the aid of an Arbeitsgemeinschaft fur Osteosynthesefragen (AO) distractor and a 9-hole AxSOS Stryker plate was used for fixation. Subsequently, the femoral neck fracture was reduced by an open method using a bone hook placed on the anterior aspect of the base of the femoral neck. The fracture was stabilised using a 2-hole dynamic hip screw (DHS) with a derotation screw. Alendronic acid was discontinued and denosumab was commenced at discharge.
Outcome and follow-up
Postoperatively, she was managed with touch weight-bearing for 6 weeks and was able to fully weight-bear by 3 months. At 3, 6, 12 and 18 months review, she remained well without any adverse events and at final follow-up she had regained complete premorbid function. Radiologically at 1 year, there were no osteoarthritic changes of the hip or features suggestive of avascular necrosis of the femoral head, and the shaft fracture united satisfactorily (figure 2A–C).
Figure 2.
(A) AP femur demonstrating fixation with 9-hole AxSOS Stryker plate (1 year postoperatively). (B) AP pelvis demonstrating 2-hole DHS and derotation screw with no evidence of avascular necrosis of hip. (C) Lateral femur and lateral hip demonstrating dual implants with satisfactory union. AP, anteroposterior; DHS, dynamic hip screw.
Discussion
Ipsilateral fractures of the femoral neck and shaft are usually seen following high-energy injury mechanisms and are commonly due to axial compression and bending of the abducted femur.2 Historically, in the presence of a shaft fracture, 30% of femoral neck fractures were missed.5 However, through an increased awareness and the routine use of cross-sectional imaging, it is understood that the prevalence of this injury pattern is more common than initially documented.
Bisphosphonates are commonly prescribed for the treatment of osteoporosis, as they have shown to reduce the incidence of fragility fractures in both men and women.6 They have also been used in glucocorticoid-induced osteoporosis, Paget’s disease, hypercalcaemia and skeletal metastases. However, their use is not free of adverse effects. Atypical femoral shaft fracture patterns in low-energy falls have been associated with bone insufficiency caused by vitamin D deficiency and long-term use of bisphosphonates or steroids.1 3 A report by the American Society for Bone and Mineral Research produced major and minor criteria for the diagnosis of atypical subtrochanteric and diaphyseal femoral fractures (box).3
Box. American Society for Bone and Mineral Research (ASBMR) revised definition of atypical femoral diaphyseal fractures.
Major criteria
Fracture is the result of minimal trauma or occasionally can be without a history of trauma.
Fracture line is predominantly transverse along the lateral cortex and as oblique in orientation towards the medial cortex.
Complete fractures extend through both cortices and may be associated with medial spike, incomplete fractures involve the lateral cortex.
Fracture is usually non-comminuted or minimally communited.
The presence of periosteal or endosteal thickening of the lateral cortex at the fracture site (usually referred as ‘beaking’).
Minor criteria
Generalised increase in cortical thickness of the femoral diaphysis.
Unilateral or bilateral thigh/groin pain preinjury.
Bilateral incomplete femoral diaphyseal fractures.
Delayed fracture healing.
Bisphosphonate therapy has also been associated with an increased rate of delayed union in up to 56%, with significantly higher incidence in patients with long-term therapy and a higher incidence of non-union that necessitated further surgery (25% vs 13%).1 7
This report outlines a rare association of ipsilateral femoral neck and atypical diaphyseal fracture, an injury pattern usually seen in high-energy trauma. There is currently no consensus regarding the choice of optimal implant or fixation technique to treat this fracture pattern. The choice of treatment is debatable and, to a certain extent, depends on the preference of the individual surgeon. Each management option carries both benefits and significant risks which must be taken into account.
The five main operative stabilisation techniques considered include the following:
A combination of retrograde intramedullary nailing and DHS (‘rendezvous’ technique), indicated in very distally localised shaft fractures. The difficulties here are with placement of the DHS plate screws and the risk of a high-stress riser, if these are not perfect.
A long cephalomedullary nail (all-in-one device), optimal in unstable intertrochanteric and shaft or subtrochanteric fractures. This option risks failing to achieve perfect fixation of the femoral neck with a high chance of failure over a short period of time.
Two non-overlapping implants, that is, a DHS or cannulated screws for the hip fracture and a shaft plate for non-displaced proximal fractures. Again, there is a high risk of failure given a high-stress riser in osteoporotic bone.
A combination of antegrade reamed intramedullary nailing and cancellous screw fixation of the femoral neck (Miss-a-nail technique).8 This technique is technically very challenging and there are very limited salvage options in the event of intraoperative failure.
A hemiarthroplasty of the hip with a shaft plate, particularly where there is a high risk of avascular necrosis of the femoral head. The difficulties with this technique would be ensuring stable fixation in a low-femoral neck fracture and concerns about the inevitable stress riser between the implant and the plate.
Some authors advocate stabilising the femoral neck fracture first to avoid the risk of displacement at the time of fixation of the shaft.2 9 However, others favour fixation of the shaft first, which would then enable better control of the leg during reduction manoeuvres and would aid safer anatomical reduction of the neck fracture.5 In our case, as the femoral head was at risk of developing avascular necrosis, we anticipated a possible need for early total hip replacement. The presence of intramedullary (IM) nail as opposed to a femoral plate would preclude us from performing a total hip replacement (THR) without explanting the nail. Also, reaming and impaction caused by retrograde nailing could displace the neck fracture even when it is adequately stabilised.2 9 In our case, as the femoral neck fracture orientation was basicervical, DHS offered a greater biomechanical advantage compared with cannulated screw fixation.
Conclusion
This case outlines a non-overlapping DHS and femoral shaft plate construct for an atypical femoral diaphysial and ipsilateral neck fracture achieving uneventful healing and good functional outcome within the first year of follow-up.
Although intramedullary nailing is the current recommendation for the treatment of isolated femoral shaft fractures, this case suggests that these can be successfully treated with non-overlapping implants when associated with ipsilateral femoral neck fracture. The use of shaft compression plating is a good option to obtain bone-on-bone contact and promote healing with improved outcomes.
Learning points.
Understand that ipsilateral femoral neck and shaft fractures can occur in low-energy trauma in certain populations.
Identifying femoral neck fracture in the presence of a femoral shaft fracture, as well as having an awareness of the features of an atypical femoral shaft fracture is important.
A fixation method should be tailored to the individual patient as there are often multiple options to achieve a satisfactory outcome.
With an ageing population, use of long-term bisphosphonates is increasing. The incidence of this challenging group of fractures is, therefore, likely to increase.
Footnotes
Contributors: All the authors made individual and substantial contributions towards the writing of this case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kang JS, Won YY, Kim JO, et al. Atypical femoral fractures after anti-osteoporotic medication: a Korean multicenter study. Int Orthop 2014;38:1247–53. 10.1007/s00264-013-2259-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boulton CL, Pollak AN. Special topic: ipsilateral femoral neck and shaft fractures--does evidence give us the answer? Injury 2015;46:478–83. 10.1016/j.injury.2014.11.021 [DOI] [PubMed] [Google Scholar]
- 3.Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American society for bone and mineral research. J Bone Miner Res 2014;29:1–23. 10.1002/jbmr.1998 [DOI] [PubMed] [Google Scholar]
- 4.Lenart BA, Lorich DG, Lane JM, et al. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med 2008;358:1304–6. 10.1056/NEJMc0707493 [DOI] [PubMed] [Google Scholar]
- 5.Wu CC, Shih CH. Ipsilateral femoral neck and shaft fractures. Retrospective study of 33 cases. Acta Orthop Scand 1991;62:346–51. [DOI] [PubMed] [Google Scholar]
- 6.Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the fracture intervention trial long-term extension (FLEX): a randomized trial. JAMA 2006;296:2927–38. 10.1001/jama.296.24.2927 [DOI] [PubMed] [Google Scholar]
- 7.Yue B, Ng A, Tang H, et al. Delayed healing of lower limb fractures with bisphosphonate therapy. Ann R Coll Surg Engl 2015;97:333–8. 10.1308/003588415X14181254789321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiss DA, Sima W, Brien WW. Ipsilateral fractures of the femoral neck and shaft. J Orthop Trauma 1992;6:159–66. 10.1097/00005131-199206000-00005 [DOI] [PubMed] [Google Scholar]
- 9.Hak DJ, Mauffrey C, Hake M, et al. Ipsilateral femoral neck and shaft fractures: current diagnostic and treatment strategies. Orthopedics 2015;38:247–51. 10.3928/01477447-20150402-05 [DOI] [PubMed] [Google Scholar]