Abstract
Xeroderma pigmentosum (XP) is an autosomal recessive disorder associated with multiple oculocutaneous manifestations. We discuss a unique case of XP having bilateral ocular surface squamous neoplasia (OSSN) and periocular basal cell carcinoma. In the right eye, a large OSSN mass involving the ocular surface extensively along with intraocular invasion was noted, whereas in the left eye, the tumour mass was involving the limbus, and extending up to three clock hours. Because of extensive disease in the right eye, orbital exenteration was performed, and for the left eye, a wide excision of the mass with triple freeze thaw cryo application to the margins followed by amniotic membrane grafting was done. Basal cell carcinoma was noted around the medial canthus on both sides. The right-sided basal cell carcinoma was treated by wide excision followed by a forehead rotation flap and the left-sided lesion was managed with topical 5% imiquimod cream.
Keywords: ophthalmology, oncology
Background
Xeroderma pigmentosum (XP) is a rare genetic disorder characterised by defective DNA repair, causing increased susceptibility to various oculocutaneous malignancies.1 Patients with XP should be meticulously screened for such malignancies and managed promptly to prevent local spread and systemic metastasis. These cases are notorious for aggressive nature of the tumour and high chances of recurrences, thus necessitating a lifelong close follow-up. We discuss a case of XP that had bilateral ocular surface squamous neoplasia (OSSN) and medial canthal basal cell carcinoma (BCC), and was treated with a combination of surgery and chemotherapy.
Case presentation
A 9-year-old male child diagnosed with XP at the age of 4 years presented with a history of photophobia and a gradually increasing mass in both eyes, noted 6 months back. There was associated diminution of vision in the right eye. Family history was negative for the disease. The patient had undergone local excision of right-sided BCC along with reconstructive surgery using a forehead rotation flap performed by a maxillofacial surgeon. At presentation, the general physical examination showed multiple pigmented lesions all over the body with areas of hypopigmentation and desquamation (figure 1A). On palpation, right-sided preauricular lymph nodes were palpable. On ocular examination, the patient was extremely photophobic. Visual acuity in the right eye was perception of light with inaccurate projection of rays in all quadrants and 20/20 in the left eye. The right eye showed a gelatinous mass of 20 mmx15 mm, with pinkish spots extending from the medial canthus onto the entire cornea. The left eye showed a localised mass at the limbus involving up to three clock hours with dilated and tortuous feeder vessels. Other findings included a lower eyelid ectropion with marginal keratinisation in both eyes. A papulo-nodular lesion of 0.5 mm with surrounding crusting and pearly rolled edges was present on the left side below the medial canthus (figure 1B,C). On the right side, the forehead flap extended up to the nasal ala.
Figure 1.

(A) Child with xeroderma pigmentosum showing dry skin and hypopigmented and hyperpigmented patches over the face. (B) Right-sided forehead flap reconstruction for excised basal cell carcinoma. (C) Preoperative photograph under general anaesthesia showing an extensive ocular surface mass in the right eye, with a localised ocular surface mass and a nodular medial canthal mass in the left eye.
Investigations
Ultrasound biomicroscopy of the right eye revealed intraocular extension of the mass involving the ciliary body region.
Contrast-enhanced computed tomography scans revealed no orbital extension.
Whole body Positron Emission Tomography (PET)-CT scan was negative for any systemic metastasis.
Preauricular lymph node biopsy revealed reactive lymphadenitis without any evidence of tumour cells.
An incision biopsy from the right eye and left medial canthal nodular lesion confirmed OSSN in the right eye (figure 2A) and the nodular mass in the left medial canthus was confirmed as BCC (figure 2B).
Figure 2.
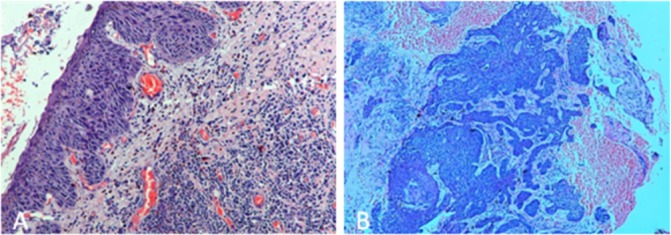
(A) Histopathological examination of the ocular surface mass biopsy showing a squamous cell carcinoma. (B) Medial canthal mass biopsy showing a basal cell carcinoma.
Treatment
The patient underwent a wide local excision of the left ocular surface mass with triple freeze cryotherapy of the free margins, followed by amniotic membrane grafting under general anaesthesia. The right eye was not amenable to enucleation as the mass was extensive; exenteration surgery of the right eye was performed under general anaesthesia. Postoperative histopathological evaluation revealed poorly differentiated squamous cell carcinoma with scleral breach and intraocular spread. The patient and caretakers were hesitant to undergo any further surgery and preferred medical management with close follow-up. Thus, BCC on the left side was managed with topical application of imiquimod cream in a concentration of 5% once daily for 5 days a week with 2 days off for a total duration of 8 weeks.
Outcome and follow-up
At 2 months follow-up, the exenterated orbit was healthy (figure 3). There was no evidence of tumour recurrence on the left-sided ocular surface mass on impression cytology. At the end of 5 months, there was a 60% reduction in the size of left-sided BCC, and by the seventh month, there was a 90% reduction in the tumour size (figure 4), suggesting an excellent response to topical 5% imiquimod cream.
Figure 3.

Postexenteration healthy orbit at 2 months follow-up.
Figure 4.

(A) Left nodular basal cell carcinoma at presentation. (B) Seven-month follow-up showing excellent response of nodular basal cell carcinoma to topical 5 % imiquimod cream.
Discussion
XP is an autosomal recessive disorder in which the patient has a defective DNA repair mechanism to the damage caused by UV radiation.2 It equally affects both genders with an incidence of 1:250 000.3 XP is six times more common in the Japanese population than others.4 It is due to a mutation in nucleotide excision repair that causes accumulation of damaged DNA leading to dry scaly skin, pigmentation, and an increased risk of ocular and cutaneous neoplasia. There is a 1000-fold increased risk of ocular surface malignancies in XP with a mean age of 8 years at presentation as compared with 60 years in the general population. When it occurs early, it tends to be more aggressive.5 A series by Kreamer et al and other reports have shown the incidence of malignant oculocutaneous neoplasms to be 40%–60% (squamous cell carcinoma being most common).6
OSSN is a broad term used for all premalignant and malignant epithelial lesions of the conjunctiva and cornea. OSSN is most commonly found in the interpalpebral region at or near the limbus. Localised well-defined tumours are treated by surgical excision with no touch technique using lamellar keratectomy and partial sclerectomy (if the sclera is involved), with cryotherapy on the conjunctival side.7 Topical chemotherapy with Mitomycin C (MMC) 0.04% or immunotherapy with interferon alpha can also be used. A recent case report of XP with bilateral OSSN was published in which the authors treated diffuse OSSN in one eye with topical chemotherapy using mitomycin-C (0.04%) and the large OSSN in the other eye with a combination of surgery and topical chemotherapy.8 They had also described two skin melanomas in their report which however did not receive any treatment. In our study, the right eye OSSN was extensive with intraocular spread, and was treated with exenteration surgery, while the left eye OSSN was treated with total excision using ‘no touch technique’ and application of cryotherapy to the conjunctival margins. Topical chemotherapy can, however, be used as an alternative to surgery in responsive tumours. The left-sided BCC in our study was managed medically using topical 5% imiquimod cream. Imiquimod is an immune modulator which acts through toll-like receptors 7 and 8 to produce cytokines and chemokines. These mediators stimulate both the innate and the adaptive immunity and induces apoptosis in tumour cells. There are few reports showing the efficacy of imiquimod in periocular tumours occurring in XP but there is no controlled study to confirm it.9 There is one case report by Giannotti et al in which imiquimod has been used in XP for treatment of skin tumours with resolution.10 Imiquimod cream is a good alternative to surgery for medial canthal BCC as surgical excision can damage the lacrimal system and reconstruction of defects needs grafts and flaps.11 In our case, right-sided BCC was treated by surgery and the left-sided BCC was treated with topical imiquimod, with a good response.
Learning points.
Xeroderma pigmentosum patients have an increased risk of oculocutaneous malignancies, so any suspected lesions should be evaluated properly and managed accordingly.
Topical imiquimod cream can be considered as an alternative treatment to surgery in basal cell carcinoma.
The patient should be educated and counselled for long-term regular follow-up due to a high recurrence rate of malignancies and rapid progression of existing tumours.
Acknowledgments
Dr Seema Sen, MD Professor of Ocular Pathology Dr Rajendra Prasad Centre for Ophthalmic Sciences, AIIMS, New Delhi for histopathologic examination and analysis of biopsy specimens.
Footnotes
Contributors: RA, BC, MIA and AP was involved in drafting, analysis, literature review and editing of this report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Robbins JH, Kraemer KH, Lutzner MA, et al. . Xeroderma pigmentosum. An inherited diseases with sun sensitivity, multiple cutaneous neoplasms, and abnormal DNA repair. Ann Intern Med 1974;80:221–48. [DOI] [PubMed] [Google Scholar]
- 2.James WD, Elston D, Berger T. Andrew’s diseases of the skin: clinical dermatology: Elsevier Health Sciences, 2011. [Google Scholar]
- 3.Lehmann AR, McGibbon D, Stefanini M. Xeroderma pigmentosum. Orphanet J Rare Dis 2011;6:70 10.1186/1750-1172-6-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei Q, Li L, Chen D. DNA repair, genetic instability, and cancer. World scientific, 2007. [Google Scholar]
- 5.Gupta N, Sachdev R, Tandon R. Ocular surface squamous neoplasia in xeroderma pigmentosum: clinical spectrum and outcome. Graefes Arch Clin Exp Ophthalmol 2011;249:1217–21. 10.1007/s00417-011-1679-8 [DOI] [PubMed] [Google Scholar]
- 6.Kraemer KH, Lee MM, Scotto J. Xeroderma pigmentosum. Cutaneous, ocular, and neurologic abnormalities in 830 published cases. Arch Dermatol 1987;123:241–50. [DOI] [PubMed] [Google Scholar]
- 7.Sarici AM, Arvas S, Pazarli H. Combined excision, cryotherapy, and intraoperative mitomycin C (EXCRIM) for localized intraepithelial and squamous cell carcinoma of the conjunctiva. Graefes Arch Clin Exp Ophthalmol 2013;251:2201–4. 10.1007/s00417-013-2437-x [DOI] [PubMed] [Google Scholar]
- 8.Kalamkar C, Radke N, Mukherjee A, et al. . Xeroderma pigmentosum with bilateral ocular surface squamous neoplasia and review of the literature. BMJ Case Rep 2016;2016:bcr20172016215364 10.1136/bcr-2016-215364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Macedo EM, Carneiro RC, de Lima PP, et al. . Imiquimod cream efficacy in the treatment of periocular nodular basal cell carcinoma: a non-randomized trial. BMC Ophthalmol 2015;15:35 10.1186/s12886-015-0024-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giannotti B, Vanzi L, Difonzo EM, et al. . The treatment of basal cell carcinomas in a patient with xeroderma pigmentosum with a combination of imiquimod 5% cream and oral acitretin. Clin Exp Dermatol 2003;28:33–5. [DOI] [PubMed] [Google Scholar]
- 11.Karabulut GO, Kaynak P, Ozturker C, et al. . Imiquimod 5% cream for the treatment of large nodular basal cell carcinoma at the medial canthal area. Indian J Ophthalmol 2017;65:48–51. 10.4103/ijo.IJO_958_16 [DOI] [PMC free article] [PubMed] [Google Scholar]


