Abstract
Cementoblastoma is a benign odontogenic neoplasm accounting for less than 0.69%–8% of all odontogenic tumours and is characterised by the presence of sheets of cementum-like tissue demonstrating large number of reversal lines. It shows an unlimited growth potential and a recurrence rate as high as 37.1%. It most commonly affects the permanent mandibular molars. This paper presents the third reported case of cementoblastoma affecting the deciduous maxillary posterior dentition. A 12-year-old male patient reported to the Department of Oral and Maxillofacial Pathology with a chief complaint of pain and swelling in relation to the deciduous maxillary left second molar.
Keywords: mouth, dentistry and oral medicine
Background
Originally described by Dewey in 1927, the first case of cementoblastoma was reported in 1930 by Norberg, as a true cementoma.1 2 Cementoblastoma is a benign odontogenic neoplasm accounting for less than 0.69%–8% of all odontogenic tumours.1 WHO defines it as ‘a neoplasm characterized by the formation of sheets of cementum-like tissue containing a large number of reversal lines and a lack of mineralization at the periphery of the mass or in the more active growth areas’.3 It typically presents as a hard cemental mass contiguous with the radicular cementum. Mandibular teeth are more commonly affected than the maxillary teeth (3:1). It shows a prevalence for the second and third decades of life.4 This paper highlights a rare case of cementoblastoma affecting the deciduous maxillary second molar in a 12-year-old Indian male.
Case presentation
A 12-year-old male presented with a chief complaint of pain and swelling in the left posterior region of the maxillary arch since 1 year. There was no reported history of orofacial trauma and medical history was unremarkable. Extraoral examination did not reveal any asymmetry. Intraoral examination revealed a diffuse, hard, lobulated swelling in relation to the roots of 65, measuring approximately 2.5×1 cm. The overlying mucosa appeared erythematous, and obliteration of the buccal vestibule was evident.
Investigations
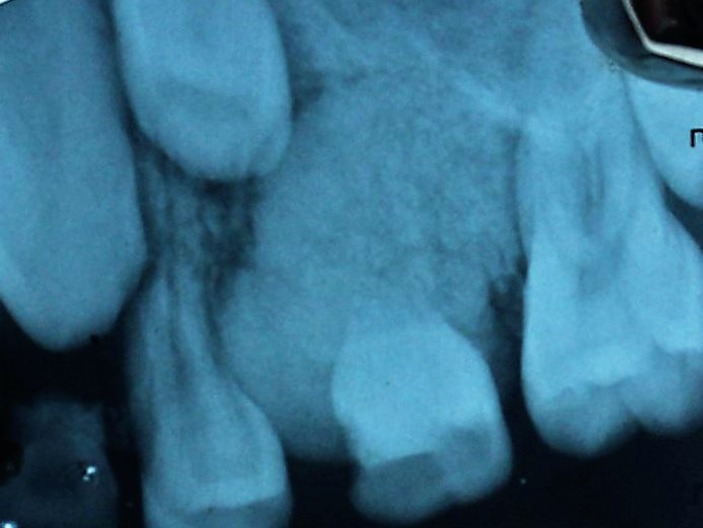
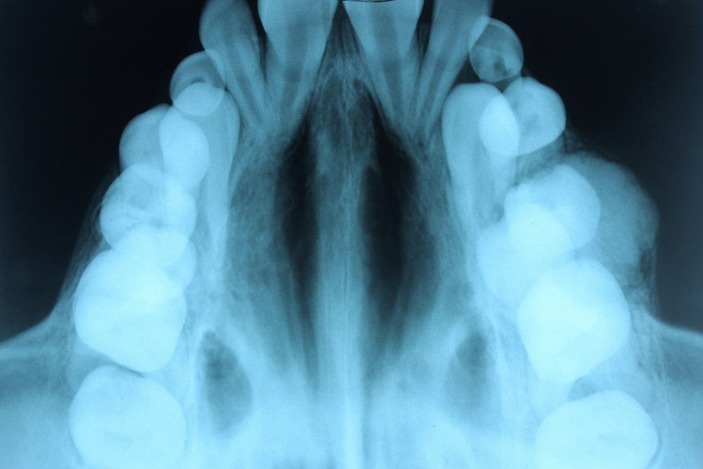
An intraoral periapical radiograph revealed a well-defined round radiopaque mass surrounded by a radiolucent band in relation to the roots of the deciduous maxillary left second molar. Root resorption of the involved tooth was evident (figure 1). True occlusal radiograph demonstrated localised expansion of the buccal cortical plate in relation to 65, the surface appeared lobulated (figure 2). Panoramic radiograph revealed a radiopaque mass attached to the roots of 65 and surrounded by a radiolucent band causing deviation of roots of 24 and 26. 25 appeared to be displaced superiorly (figure 3). 65 showed mild caries, however, all teeth in the left maxillary segment were vital following electric pulp testing.
Figure 1.
Intraoral periapical radiograph demonstrating radiopaque mass attached to the root of 65.
Figure 2.
True occlusal radiograph demonstrating the lobulated surface of tumour mass.
Figure 3.
Panaromic radiograph showing the radiopaque mass in relation to the root of 65, and root contours are not evident. Note the displacement of the adjacent teeth.
Differential diagnosis
Cementoblastoma, osteoblastoma, odontoma, periapical cemental dysplasia, hypercementosis and osteoma were considered in the differential diagnosis. Based on the clinical and radiographic evaluation, a provisional diagnosis of cementoblastoma was made.
Treatment
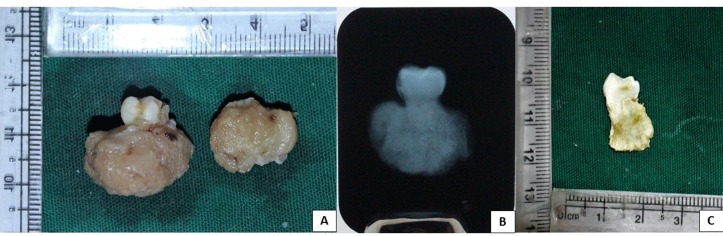
Complete surgical excision of the tumour mass along with extraction of 65 was performed under general anaesthesia. The mass was resected into two during surgery to facilitate removal. Gross examination of the excised specimen revealed two oval to round yellowish masses of hard tissues measuring approximately 2.2×1.4×1 cm and 1.7×1.2×0.7 cm. The larger mass was attached to the resorbed root. The specimen was sectioned and taken for decalcification. The cut section revealed loss of the normal root anatomy and replacement with the lesional tissue extending up to the cementoenamel junction (figure 4).
Figure 4.
(A) Excisional biopsy of the lesion revealing two bits of hard tissue. The tumour mass is attached to the roots of the deciduous maxillary second molar. (B) Radiographic image of the excised specimen on an intraoral periapical film. (C) Cut section of the same showing the connection of the mass to the tooth root.
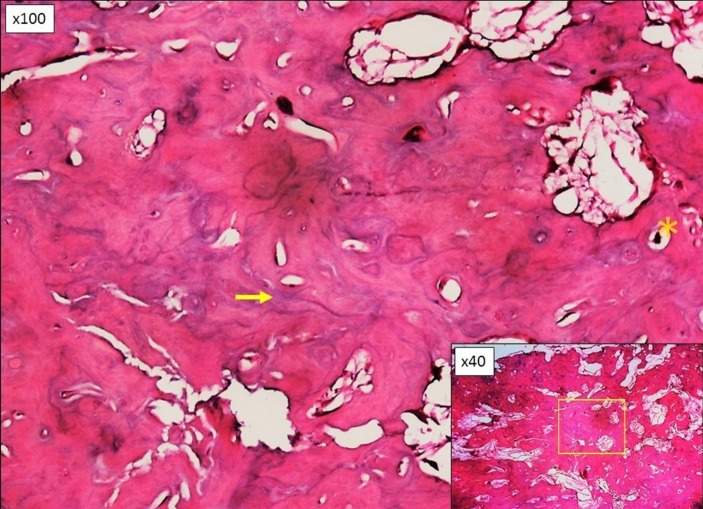
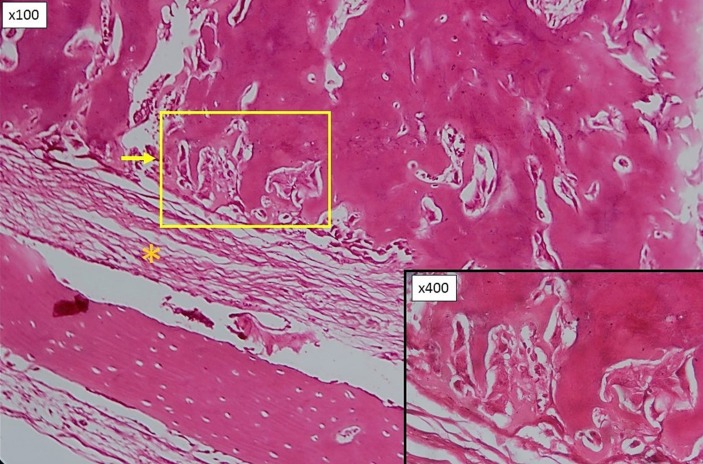
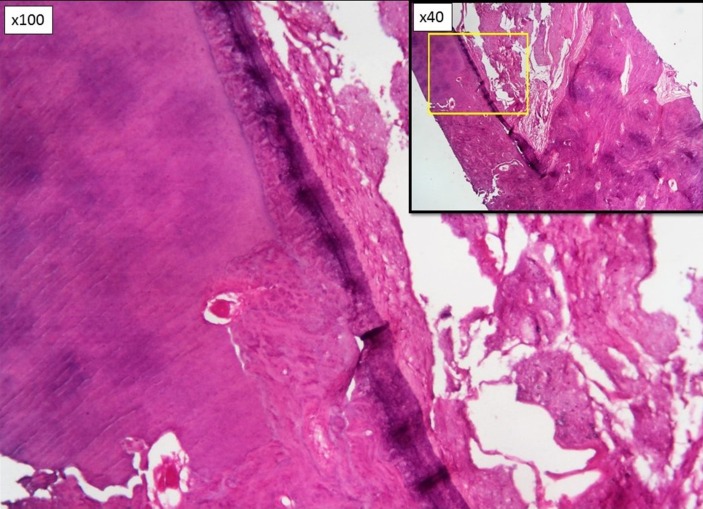
On histopathological examination, the tumour was composed of dense, irregularly lamellated, osteocementum-like tissue showing lacunae with entrapped cells and numerous basophilic reversal lines (figure 5). The periphery of the mass showed cementum-like tissue arranged in parallel fashion lined by active cementoblasts. The lesion was surrounded by a well-defined fibrous capsule (figure 6). Figure 7 shows the fusion of the tumorous tissue to the tooth root. There has been no recurrence of the lesion more than 12 months following surgery.
Figure 5.
Photomicrograph demonstrating sheets of cementum-like tissue containing irregular lacunae, entrapped cells (indicated by asterisk) and numerous reversal lines (indicated by arrow). (H&E, original magnification x100, inset: x40).
Figure 6.
Photomicrograph showing cementum-like tissue arranged in parallel fashion at the periphery and surrounded by a fibrous capsule (indicated by asterisk). (H&E, original magnification x100, inset: x400).
Figure 7.
Photomicrograph revealing the connection of the tumorous mass to the resorbed root. (H&E, original magnification x100, Inset: x40).
Discussion
Benign cementoblastoma of the jaws is defined as a true neoplasm of cementum or cementum-like tissue affecting the tooth root.5 The 2005 WHO classification included cementoblastoma under the category of benign odontogenic tumour of the ectomesenchyme with or without involvement of the odontogenic epithelium.6 Cementoblastoma has been updated and included in the 2017 WHO classification of odontogenic tumours.7 It is considered to be the only true neoplasm of cementum (true cementoma),8 other lesions of cemental origin or showing cementum-like material microscopically are enlisted in box. It most commonly affects the mandibular teeth (79.5%) with permanent mandibular first molar being the most commonly involved tooth.5 9 The present case is the third reported case of cementoblastoma affecting the deciduous dentition in the maxillary arch, and the first reported case showing involvement of a single deciduous maxillary molar. Urs et al reported the second case, wherein involvement of the deciduous maxillary molars (54, 55) was described.10 Comparison of the case presented by Urs et al and the present case, which are the only reported cases of cementoblastoma solely affecting the deciduous dentition in the maxillary arch is provided in table 1. Ohki et al reported a case of cementoblastoma affecting multiple permanent and deciduous teeth in the right maxillary quadrant (55, 14, 15, 16, 17).11 Only 15 cases of cementoblastoma involving the deciduous dentition have been reported so far, including the present case.8 10–22 Involvement of impacted, unerupted and multiple teeth has also been documented.11 23 Its prevalence is not influenced by gender.24 The condition is most commonly seen in young adults, 73% of the cases have been reported in patients under the age of 30 years and 50% of the cases occurring in patients less than 20 years of age.5 24 Cementoblastoma grows slowly, having a growth rate of 0.5 cm per year. The affected tooth is vital and often painful.25 Unresponsiveness to vitality tests may be noticed in teeth with vital pulp. This occurs because the tumour mass disrupts the normal neural impulse transmission, as it encompasses the root apex.11
Box. Cemental pathoses.
Developmental conditions
Concrescence
Cleidocranial dysplasia
Odontoma (complex and compound)
Fibro-osseous lesions
-
Cemento-osseous dysplasia
Focal cemento-osseous dysplasia
Florid cemento-osseous dysplasia
-
Neoplastic
Gigantiform cementoma
Cemento-ossifying fibroma
Neoplasms
Cementoblastoma
Reactive lesions
Peripheral cemento-ossifying fibroma
Inflammatory conditions
Hypercementosis
Ankylosis
Atypical external root resorption
Metabolic diseases
Hypophosphatasia
Lesions showing cementum-like deposits
Odontogenic tumours
Table 1.
Reported cases of cementoblastoma solely affecting the deciduous dentition in the maxillary arch
| Present case, 2017 | Urs et al10 | |
| Age | 12 years | 10 years |
| Gender | Male | Male |
| Teeth involved | 65 | 54, 55 |
| Root resorption | Present | NR |
| Displacement of adjacent teeth | Present | Present |
| Expansion of cortical plates | Present | Present |
| Size of the excised mass | 2.2×1.7 cm | 2.3×2 cm |
| Recurrence | Absent (1-year follow-up) | Absent (2-year follow-up) |
NR, not reported.
Most of the cases remain asymptomatic, pain and swelling are the commonly noted symptoms.25 Aggressive cementoblastoma cases have also been reported showing features of cortical expansion, perforation, maxillary sinus involvement, displacement of adjacent teeth and invasion of pulp chambers and root canals.24 Brannon et al have reported a recurrence rate as high as 37.1%. Although the findings were not statistically significant, younger mean age and larger mean size were noted in the recurrent cases.9
Characteristic radiographic appearance is that of a radiopaque mass attached to the tooth root surrounded by a peripheral radiolucent band. Root resorption and loss of tooth contour may be seen.4 Grossly, a round to ovoid, well-circumscribed mass of hard, calcified, tan-coloured tissue surrounds the root of the affected tooth surrounded by a soft-tissue capsule.2
Histopathologically, cementoblastoma consists of dense masses of acellular cementum-like tissue in a fibrous, sometimes rather vascular stroma that may contain multinucleated cells.6 Cemental trabeculae in areas of active growth are bordered by a layer of cementoblasts. The characteristic feature of cementoblastoma is the presence of prominent basophilic reversal lines giving it a pagetoid appearance.2 Irregular lacunae housing the entrapped cementocytes are seen.26 At the periphery, the cemental layer may be oriented at right angles, and surrounded by a soft-tissue cellular layer resembling capsule.27
Radiographic differential diagnoses of a periapical radiopaque mass include cementoblastoma, osteoblastoma, odontoma, periapical cemento-osseous dysplasia (PCOD), hypercementosis, condensing osteitis and osteoma. Correlation of the clinical, radiographic and histopathological features is required to narrow down the differential diagnosis.4
Several overlapping clinical, radiographic and histological features have been discussed between cementoblastoma and osteoblastoma of the jaws. Cementoblastoma was thus considered to be a subtype of osteoblastoma. However, the two differ in origin. Cementoblastoma is an odontogenic tumour recapitulating the stages of odontogenesis, whereas osteoblastoma is a benign tumour of the bone.9 Osteoblastoma is usually not associated with teeth, whereas cementoblastoma is continuous with the cemental layer. Histologically, overlapping features are seen in both the lesions. Presence of plump and pleomorphic cementoblasts, numerous mitotic figures and the presence of numerous reversal lines favour a diagnosis of cementoblastoma.4
Odontoma is considered to be a benign mixed odontogenic tumour, most commonly seen in association with an impacted tooth. An odontoma presents as a sharply marginated radiopaque mass usually pericoronal in location, with a low attenuation halo. It may rarely be seen in close proximity to the tooth root, but is generally not attached to it. Microscopically, the two differ significantly.28 Unlike cementoblastoma, odontoma shows the presence of normal-appearing enamel or enamel matrix, dentin, pulp tissue and cementum that may or may not exhibit a normal relation to one another.27
PCOD is a reactional and non-neoplastic process developing in the periapical area of vital teeth. It is characterised by replacement of the normal bone with fibrous tissue and metaplastic bone, most commonly affecting the mandibular anterior teeth in middle-aged African-American women. Radiographically, the cementoblastic and the mature forms of PCOD closely resemble cementoblastoma, however, in PCOD the lesional tissue does not directly fuse to the tooth root.28 29 Histopathologically, the cementoblastic stage shows a mixture of spherical calcifications and irregularly shaped deposits of osteoid and mineralised bone. The mature form is composed predominantly of coalesced spherical calcifications and sclerotic mineralised bone with scant connective tissue.30
Hypercementosis is an idiopathic non-neoplastic condition characterised by excessive cementum deposition over the normal radicular cementum.31 It may be associated with periapical pathoses. In hypercementosis, root appears bulbous due to thickening of the cementum layer and is surrounded by a thin radiolucent rim. This radiolucent rim is reminiscent of the periodontal ligament. Whereas in cementoblastoma, the soft-tissue capsule surrounding the lesional tissue presents as a thick radiolucent band.31 32 An intact lamina dura may be seen in hypercementosis.31 In contrast to cementoblastoma, the microscopic appearance of hypercementosis is of concentric layers of cellular cementum, frequently showing numerous resting lines, deposited directly over the root cementum.27
Condensing osteitis represents areas of bone sclerosis that surrounds the apices of premolars and molars following pulpitis or pulpal necrosis. Radiological presentation is that of poorly marginated sclerotic lesion surrounding the roots of carious teeth.28 Remodelling and sclerosis of bone are the typical microscopic features.33
Osteoma is a benign tumour of the osteoblasts, presenting as an expansile exophytic lesion. Most commonly involves the paranasal sinuses in the head and neck region with maxillary sinus being the most favoured location. Intraosseous involvement is rare, although if present is not related to the teeth. Radiographically, it presents as a radiopaque mass without a perilesional halo.28 Histopathologically, it is composed of either normal compact or cancellous bone, foci of cartilage may be found.27
The treatment of choice is complete removal of the lesion with extraction of the associated tooth or teeth.34 Curettage and peripheral ostectomy have been advocated due to the high recurrence rate. Conservative treatment modalities include removal of the tumour mass along with endodontic treatment of the affected teeth.5 34
Learning points.
Cementoblastoma affecting the deciduous teeth is a rare phenomenon; however, it should be considered in the differential diagnoses of radiopaque masses of periapical region.
Presence of a thick radiolucent band is an important parameter to differentiate cementoblastoma from the atypical hypercementosis.
Although it shows a slow growth potential, a high recurrence rate is noted. Thus, complete surgical excision should be performed, along with the extraction of the involved teeth. Strict follow-up protocol should be observed.
Footnotes
Contributors: SN: conception and design, conduct, literature search, data acquisition, data analysis, manuscript preparation, manuscript editing, manuscript review. SS: conception and design, data acquisition, data analysis, manuscript preparation. AS: conception and design, conduct, manuscript editing, manuscript review. AD: conception and design, conduct, manuscript editing, manuscript review.
Competing interests: None declared.
Patient consent: Guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sankari LS, Ramakrishnan K. Benign cementoblastoma. J Oral Maxillofac Pathol 2011;15:358–60. 10.4103/0973-029X.86725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huber AR, Folk GS. Cementoblastoma. Head Neck Pathol 2009;3:133–5. 10.1007/s12105-008-0099-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kramer IR, Pindborg JJ, Shear M. World Health Organization, International Histological Classification of Tumors Histological typing of odontogenic tumors. 2nd edn New York: Springer-Verlag, 1992:23. [Google Scholar]
- 4.Shastry S, Thoondla M, Gupta S, et al. Benign cementoblastoma. Indian J Oral Sci 2012;3:165–7. 10.4103/0976-6944.111181 [DOI] [Google Scholar]
- 5.Solomon MC, Rehani S, Valiathan M, et al. Benign cementoblastoma involving multiple deciduous and permanent teeth of the maxilla: a case report. Oral Maxillofac Path J 2012;3:258–63. [Google Scholar]
- 6.Barnes L, Eveson JW, Reichart P, et al. World Health Organization classification of tumours: pathology and genetics, head and neck tumours. Lyon: IARC Press, 2005. [Google Scholar]
- 7.Wright JM, Vered M. Update from the 4th edition of the world health organization classification of head and neck tumours: odontogenic and maxillofacial bone tumors. Head Neck Pathol 2017;11:68–77. 10.1007/s12105-017-0794-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nuvvula S, Manepalli S, Mohapatra A, et al. Cementoblastoma relating to right mandibular second primary molar. Case Rep Dent 2016;2016:1–5. 10.1155/2016/2319890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brannon RB, Fowler CB, Carpenter WM, et al. Cementoblastoma: an innocuous neoplasm? A clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:311–20. 10.1067/moe.2002.121993 [DOI] [PubMed] [Google Scholar]
- 10.Urs AB, Singh H, Rawat G, et al. Cementoblastoma solely involving maxillary primary teeth--a rare presentation. J Clin Pediatr Dent 2016;40:147–51. 10.17796/1053-4628-40.2.147 [DOI] [PubMed] [Google Scholar]
- 11.Ohki K, Kumamoto H, Nitta Y, et al. Benign cementoblastoma involving multiple maxillary teeth: report of a case with a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97:53–8. 10.1016/j.tripleo.2003.08.012 [DOI] [PubMed] [Google Scholar]
- 12.Chaput A, Marc A. Un cas de c’ementome localis’e sur une molaire temporaire. SSO Schweiz Monatsschr Zahnheilkd 1965;75:48–52. [PubMed] [Google Scholar]
- 13.Vilasco J, Mazère J, Douesnard JC, et al. [A case of cementoblastoma]. Rev Stomatol Chir Maxillofac 1969;70:329–32. [PubMed] [Google Scholar]
- 14.Zachariades N, Skordalaki A, Papanicolaou S, et al. Cementoblastoma: review of the literature and report of a case in a 7 year-old girl. Br J Oral Maxillofac Surg 1985;23:456–61. 10.1016/0266-4356(85)90031-2 [DOI] [PubMed] [Google Scholar]
- 15.Herzog S. Benign cementoblastoma associated with the primary dentition. J Oral Med 1987;42:106–8. [Google Scholar]
- 16.Papageorge MB, Cataldo E, Nghiem FT. Cementoblastoma involving multiple deciduous teeth. Oral Surg Oral Med Oral Pathol 1987;63:602–5. 10.1016/0030-4220(87)90236-2 [DOI] [PubMed] [Google Scholar]
- 17.Cannell H. Cementoblastoma of deciduous tooth. Oral Surg Oral Med Oral Pathol 1991;71:648 10.1016/0030-4220(91)90379-Q [DOI] [PubMed] [Google Scholar]
- 18.Schafer TE, Singh B, Myers DR. Cementoblastoma associated with a primary tooth: a rare pediatric lesion. Pediatr Dent 2001;23:351–3. [PubMed] [Google Scholar]
- 19.Lemberg K, Hagström J, Rihtniemi J, et al. Benign cementoblastoma in a primary lower molar, a rarity. Dentomaxillofac Radiol 2007;36:364–6. 10.1259/dmfr/58249657 [DOI] [PubMed] [Google Scholar]
- 20.Vieira AP, Meneses JM, Maia RL. Cementoblastoma related to a primary tooth: a case report. J Oral Pathol Med 2007;36:117–9. 10.1111/j.1600-0714.2007.00465.x [DOI] [PubMed] [Google Scholar]
- 21.de Noronha Santos Netto J, Marques AA, da Costa DO, et al. A rare case of cementoblastoma associated with the primary dentition. Oral Maxillofac Surg 2012;16:399–402. 10.1007/s10006-011-0309-2 [DOI] [PubMed] [Google Scholar]
- 22.Monti LM, Souza AM, Soubhia AM, et al. Cementoblastoma: a case report in deciduous tooth. Oral Maxillofac Surg 2013;17:145–9. 10.1007/s10006-012-0347-4 [DOI] [PubMed] [Google Scholar]
- 23.Mogi K, Belal E, Kano A, et al. Benign cementoblastoma. Case report. Aust Dent J 1996;41:9–11. 10.1111/j.1834-7819.1996.tb05647.x [DOI] [PubMed] [Google Scholar]
- 24.Ahmad F, Singh D, Gupta P, et al. A case report of cementoblastoma affecting mandibular molar. J Dentofac Sci 2014;3:55–9. [Google Scholar]
- 25.Sharma N. Benign cementoblastoma: a rare case report with review of literature. Contemp Clin Dent 2014;5:92–4. 10.4103/0976-237X.128679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Milani CM, Thomé CA, Kamikawa RSS, et al. Mandibular cementoblastoma: case report. Open Journal of Stomatology 2012;02:50–3. 10.4236/ojst.2012.21009 [DOI] [Google Scholar]
- 27.Rajendran R, Sivapathasundharam B. Shafer’s textbook of oral pathology. 7th edn New Delhi: Elsevier, 2012. [Google Scholar]
- 28.Curé JK, Vattoth S, Shah R. Radiopaque jaw lesions: an approach to the differential diagnosis. Radiographics 2012;32:1909–25. 10.1148/rg.327125003 [DOI] [PubMed] [Google Scholar]
- 29.Dagistan S, Goregen M, Çakur B, et al. Cemento-osseeous dysplasias. Rev Clín Pesq Odontol 2007;3:43–9. [Google Scholar]
- 30.Senia ES, Sarao MS. Periapical cemento-osseous dysplasia: a case report with twelve-year follow-up and review of literature. Int Endod J 2015;48:1086–99. 10.1111/iej.12417 [DOI] [PubMed] [Google Scholar]
- 31.Napier Souza L, Monteiro Lima Júnior S, Garcia Santos Pimenta FJ, et al. Atypical hypercementosis versus cementoblastoma. Dentomaxillofac Radiol 2004;33:267–70. 10.1259/dmfr/30077628 [DOI] [PubMed] [Google Scholar]
- 32.White SC, Pharoah MJ. Oral radiology: principles and interpretation. 5th edn St Louis, USA: Mosby, an imprint of Elsevier, 2004:380–1. [Google Scholar]
- 33.Razavi SM, Kiani S, Khalesi S. Periapical lesions: a review of clinical, radiographic, and histopathologic features. Avicenna J Dent Res 2015;7:e19435. [Google Scholar]
- 34.Costa FW, Pereira KM, Magalhães Dias M, et al. Maxillary cementoblastoma in a child. J Craniofac Surg 2011;22:1910–3. 10.1097/SCS.0b013e31822ea6e8 [DOI] [PubMed] [Google Scholar]