Description
A 70-year-old man was referred to plastic surgery with a progressively enlarging lesion to his forehead. A small nodule had been present since 30 years. The patient had presented to his general practitioner at the time and had been reassured that this was a sebaceous cyst which warranted no further attention. As the lesion continued to grow over the intervening years, the patient did not seek any further medical attention and concealed the lesion under a cap.
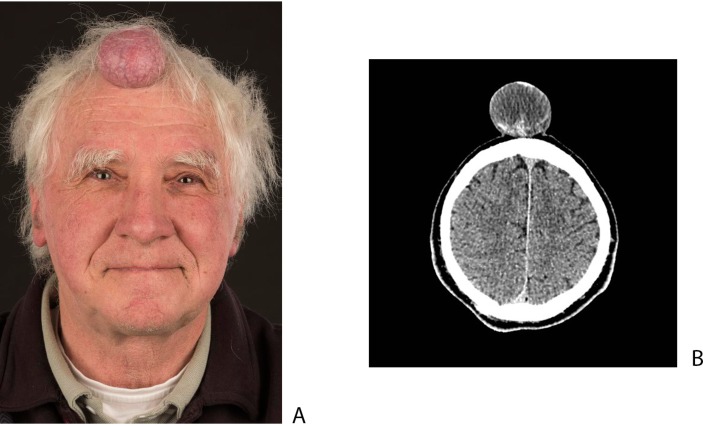
On examination, he had a 5×6×6 cm pedunculated, fleshy exophytic tumour on his central forehead (figure 1A), with further nodules each measuring 2–3 cm diameter dotted across his scalp.
Figure 1.
(A) Anterior view of the pedunculated forehead lesion. (B) Axial CT showing no intracranial component or bony erosion.
CT showed a heterogeneous midline scalp lesion abutting the outer table of the skull but with no evidence of intracranial extension (figure 1B). Duplex ultrasound showed a vascular cystic and solid lesion with low flow and some clumps of calcification. Initial differential diagnosis considered was a benign trichilemmal cyst or its malignant proliferating counterpart, a sebaceous cyst or a vascular malformation.
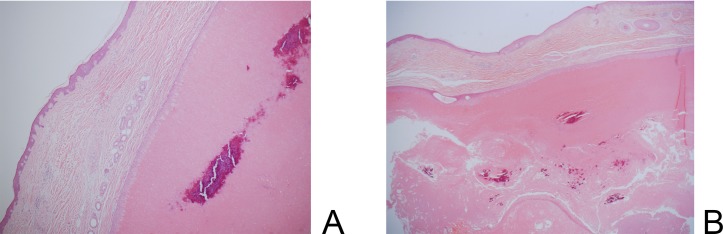
The lesions were excised to obtain a histological diagnosis. Histology confirmed completely excised benign trichilemmal cysts. The benign tumour showed a peripheral layer of cells with pale cytoplasm, the content of the cyst consisted of a keratinic homogeneous material. No atypia or multilobular proliferation was seen (figure 2). The malignant counterpart is the proliferating trichilemmal tumour which shows nuclear anaplasia and epidermoid keratinisation.
Figure 2.
(A) The wall of the trichilemmal cyst shows distinct palisading of the peripheral cell layer. The content of these cysts consists of homogeneous eosinophilic material. There are no malignant features. (B) Lower magnification image showing the overall tumour architecture (H&E staining).
Trichilemmal cysts (also known as pilar cysts) are the most common cysts of the scalp and arise from the outer root sheath of hair follicles. These are most common in women, and two-thirds of patients have multiple lesions. Unlike sebaceous cysts (with which they are frequently confused), trichilemmal cysts have no central punctum, an absent granular layer on histology and originates from outer root sheath as opposed to epithelium or hair follicle infundibulum. They also have a thicker cyst wall which is less susceptible to rupture. The vast majority of cases are benign; however, there is a potential for malignant transformation into malignant proliferating trichilemmal tumours.1 These are of low-metastatic potential and definitive treatment is by surgical excision.
Learning points.
Trichilemmal cysts are the most common cysts located on the scalp.
Most lesions are small, and large (>5 cm) exophytic lesions warrant excisional biopsy to exclude the rare chance of malignancy.
Footnotes
Contributors: MV and JW-S drafted and critically revised the article. MB processed the histopathology samples and provided the images, interpretation and a diagnosis. JW-S and SH-G were involved in the conception of the article and she was the overall consultant responsible for the patient. All the above authors were involved in the review and approval of the final published version.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Reference
- 1.Satyaprakash AK, Sheehan DJ, Sangüeza OP. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg 2007;33:1102–8. doi:10.1111/j.1524-4725.2007.33225.x [DOI] [PubMed] [Google Scholar]