Abstract
Weight stigma is pervasive, and a number of scholars argue that this profound stigma contributes to the negative effects of weight on psychological and physical health. Some lay individuals and health professionals assume that stigmatizing weight can actually motivate healthier behaviors and promote weight loss. However, as we review, weight stigma is consistently associated with poorer mental and physical health outcomes. In this article we propose a social identity threat model elucidating how weight stigma contributes to weight gain and poorer mental and physical health among overweight individuals. We propose that weight-based social identity threat increases physiological stress, undermines self-regulation, compromises psychological health, and increases the motivation to avoid stigmatizing domains (e.g., the gym) and escape the stigma by engaging in unhealthy weight loss behaviors. Given the prevalence of overweight and obesity in the US, weight stigma thus has the potential to undermine the health and wellbeing of millions of Americans.
Introduction
Weight stigma is pervasive and intensifying (Andreyeva, Puhl, & Brownell, 2008; Vartanian, Pinkus, & Smyth, 2014), and by some indicators occurring at rates comparable to gender and race-based mistreatment (Puhl, Andreyeva, & Brownell, 2008). Overweight and obese individuals face discrimination and devaluation from employers (Roehling, Roehling, & Pichler, 2007), customer service representatives (King, Shapiro, Hebl, Singletary, & Turner, 2006), health care workers (Hebl & Xu, 2001), the media (Ata & Thompson, 2010), and even family members and romantic partners (Boyes & Latner, 2009; Puhl & Brownell, 2006). Further, overweight and obese individuals are widely stereotyped to be lazy, weak-willed, and uninterested in their own health (Puhl & Heuer, 2009). A number of scholars now argue that this profound stigma and discrimination contributes to the negative effects of weight on mental and physical health (Bacon & Aphramor, 2011; Meunnig, 2008; Puhl & Heuer, 2009). Thus, with more than two-thirds of US adults now classified as overweight or obese (Odgen, Carol, Kit, & Flegal, 2014), weight stigma has the potential to compromise the health and wellbeing of millions of Americans. Here we propose a social identity threat model that elucidates how weight-stigmatizing experiences contribute to weight gain and poor mental and physical health among overweight and obese individuals. We first discuss the widespread (yet unfounded) assumption that stigmatizing weight will motivate healthier behaviors and engender weight loss. We then describe how the psychological, physiological, and motivational consequences of weight-based social identity threat actually contribute to weight gain and poor health among overweight and obese individuals.
Weight Stigma as a Public Health Tool
Lay individuals and health professionals alike often regard stigma as a way to motivate behavior change and promote healthier behaviors (Bayer, 2008). Stigmatizing tactics have figured prominently, for example, in anti-smoking campaigns seen over the past two decades (Stuber, Galea & Link, 2008). The apparent success of that effort led some to call for similar stigma-based campaigns to promote weight loss among heavy individuals (Callahan, 2013a, 2013b). The Strong4Life campaign from Children's Healthcare Atlanta provides a prime example of the use of weight stigma in public health campaigns. Strong4Life first garnered national attention in 2012 for its childhood obesity advertisements that harshly portrayed unhappy overweight children with tag lines such as “It's hard to be a little girl when you're not” and “Fat prevention begins at home. And the buffet line.” More recently, Strong4Life released an anti-obesity public service announcement that opens with an obese man on a gurney and then proceeds to “rewind” through a lifetime of sedentary behavior and unhealthy eating that lead him to this point. Both campaigns rely on stereotypical portrayals of the obese as depressed, lazy, and lacking self-control. These campaigns also distill the complex etiology of obesity down to individual choices, perpetuating simplistic ideas about the controllability of weight and presumably exacerbating the blame directed at overweight and obese individuals (Saguy, Frederick, & Gruys, 2014).
Health policy scholar Daniel Callahan (2013a, 2013b) has gone so far as to explicitly lobby for the use of “lite” forms of stigma and social pressure in the fight against obesity. Such a proposition hinges on the assumption that stigmatizing and shaming excess weight will in fact motivate healthier behavior among overweight individuals and thus is acceptable because it is “for their own good.” This assumption, however, stands in stark contrast to the growing literature on the effects weight stigma. Little evidence exists to indicate that stigmatizing experiences will lead to weight loss among overweight individuals (Vartanian & Smyth, 2013; but see Latner, Wilson, Jackson, & Stunkard, 2009). Rather, there is growing evidence that weight stigmatizing experiences promote weight gain over time (Hunger & Tomiyama, 2014; Jackson, Beeken, & Wardle, 2014; Sutin & Terraciano, 2013). Further, as we highlight below, existing research shows that weight stigma is not only psychologically but physically harmful (Puhl & Heuer, 2009, 2010). We propose that weight stigma results in detrimental psychological and physical outcomes because it threatens the social identity of overweight and obese individuals.
Weight Stigma as a Social Identity Threat
A social identity is the portion of an individual's self-concept derived from perceived membership in a social category or social group. Social identities can be achieved (e.g., being a professor) or ascribed (e.g., being African-American), as well as valued (e.g., being a doctor) or devalued (e.g., being an alcoholic). In the case of weight, when people categorize themselves as being an overweight or fat person, or believe that others categorize them as such, it becomes a social identity that is shared with others also perceived to be overweight. Note that individuals who categorize themselves as overweight may not psychologically identify with being fat, that is, see their weight as a central part of their self-concept. Nonetheless, they may still be concerned that they will be viewed through a stereotypical lens and thus devalued, mistreated, or negatively judged because of their weight (Shapiro & Neuberg, 2007; Steele, Spencer, & Aronson, 2002).
Overweight and obese individuals are well aware that being overweight is culturally devalued, and of the pervasive negative stereotypes that accompany this social identity (Puhl, Moss-Racusin, Schwartz, & Brownell, 2008). This awareness makes overweight individuals vulnerable to experiencing weight based social identity threat (Major & O'Brien, 2005; Major, Eliezer & Rieck, 2012; Steele, et al., 2002). Weight-based social identity threat is a situationally-triggered psychological state in which an individual is concerned that they have been or will be devalued, discriminated against, rejected, or negatively stereotyped because of their weight. Weight-based social identity threat can be activated in situations in which discrimination is directly experienced, such as being told by others that one should lose weight; suspected, such as wondering whether a job rejection was due to one's weight; or anticipated, such as when one first meets a potential dating partner. Weight-based social identity threat can also be activated by messages and behaviors that explicitly or implicitly devalue or justify devaluation of overweight people, such as “fat jokes” or media coverage about the costs to society of obesity. The source of threat in these situations stems from the individual's awareness that he or she may be categorized as overweight, and as a result be the target of the stereotypes and devaluation associated with this social category. Thus, people must believe they are overweight or believe others see them as overweight to experience weight-based identity threat. Importantly, overweight individuals who do not categorize themselves as overweight may still experience stigmatization, -- that is, they may be devalued, mistreated or negatively judged because of their weight. However, these individuals would be unlikely to experience weight-based social identity threat.
A large body of research has demonstrated how stigma and social identity threat based on race/ethnicity, gender, and sexual orientation can get “under the skin” to influence mental and physical health (for reviews, see Lick, Durso, & Johnson, 2013; Major, Mendes, & Dovidio, 2013; Pascoe & Smart Richman, 2009; Williams & Mohammad, 2009). Drawing on this work, we propose that weight-based social identity threat causes psychological and physiological stress, reduces self-control resources that are essential for regulating healthy behaviors, and increases the motivation to avoid and escape stigma. When experienced chronically, these effects conspire to undermine psychological and physical health and contribute to weight gain, thus ironically perpetuating the source of the stigmatization. We discuss each of these effects in turn.
Weight Stigma is Physiologically Stressful
A growing body of research demonstrates that experiencing weight-based social identity threat is physiologically stressful. Major, Eliezer and Rieck (2012) found that overweight women asked to speak about their positive dating qualities while being videotaped evidenced greater cardiovascular (CV) reactivity than overweight women delivering a similar audiotaped speech and thin women in either condition. Although they did not assess weight stigma directly, Matthews, Salomon, Kenyon, and Zhou (2005) found that adolescents who reported mistreatment on the basis of their physical appearance or body had elevated ambulatory blood pressure throughout the day. Although CV reactivity is presumed to contribute to the development of cardiovascular disease (Chida & Steptoe, 2010), measuring blood pressure reactivity alone may not sufficiently characterize the CV risks associated with chronic stigma-related activation. Research examining the cardiovascular effects of weight stigma would benefit from incorporating CV measures that facilitate differentiating between adaptive and maladaptive cardiovascular responses (Blascovich & Mendes, 2010; Hilmert & Kvascnicka, 2010). Vascular resistance is thought to be an important factor in reactivity-induced damage to the CV system (Lovallo & Gerin, 2003) and can be measured in concert with blood flow and cardiac performance to assess threatened (versus challenged) psychophysiological responses (Blascovich & Mendes, 2010).
Weight stigma also increases activation of the hypothalamic-pituitary-adrenal (HPA) axis, one of the body's stress-responsive systems whose primary output is the hormone cortisol (Dickerson & Kemeny, 2004). Cortisol is an important mediator of stress-induced eating (Newman, O'Connor, & Conner, 2007), specifically stimulating a drive for high fat and high sugar foods (Adam & Epel, 2007). Increased cortisol production also promotes the storage of excess energy as adipose fat tissue (Bjorntorp, 2001). Thus, weight-based social identity threat can initiate an involuntary physiological stress response that increases unhealthy food consumption, promotes fat deposition, and contributes to weight gain (for a detailed discussion of weight stigma and cortisol, see Tomiyama, 2014). In a cross-sectional study, Tomiyama and colleagues (2014) found an association between weight stigma experiences and morning serum cortisol levels as well as the cortisol awakening response. There is also experimental support for the effect of weight-based social identity threat on cortisol production (Himmelstein, Incollingo Belsky, & Tomiyama (2014). In a mock shopping task, self-perceived overweight women who were rejected from participating in the shopping task based on their weight showed elevated cortisol levels compared to self-perceived overweight women not exposed to such rejection and women who did not perceive themselves as overweight.
Schvey, Puhl, and Brownell (2014) similarly found that women who watched a weight-stigmatizing video exhibited greater negative emotions (e.g., anxiety) and elevated cortisol levels compared to those who watched a neutral video. Surprisingly, this effect emerged regardless of participants' weight status. Their manipulation, which involved extended exposure to a weight-stigmatizing video, may have led thinner women to be concerned about the possibility of being mistreated themselves should they gain weight, thus initiating similar emotional and psychobiological processes as those experienced by heavier women. Additional research is warranted to delineate the conditions under which weight-stigmatizing content (which we propose is identity-threatening for heavy individuals) may also negatively impact the psychological and physical health of thinner individuals.
Weight-based social identity threat may also impact more basic biological processes related to physical health. For example, Tomiyama and colleagues (2014) found a correlation between perceived weight stigma and F2-isoprostanes, a marker of oxidative stress (see also Szanton et al., 2011). Oxidative stress is a pathogenic cellular aging process that contributes to the development of obesity-related diseases such as hypertension and insulin resistance (Basu, 2008). Likewise, Sutin, Stephan, Suchetti, and Terreciano (2014) found that experiencing weight discrimination was positively correlated with C-reactive protein, a marker of inflammation and risk factor for cardiovascular disease and diabetes (Haffner, 2006). Oxidative stress and inflammation perturb multiple biological systems in the body, and may be conceptualized as downstream mediators of the effect of stress-related physiological activation on health.
Although adaptive in the short-term, chronic activation of the stress systems can result in allostatic load (McEwen, 1998). Allostatic load refers to the cumulative wear and tear on the body that is caused by repeated over-activation of physiological systems associated with adapting to stressors. Allostatic load is assumed to be a common biological pathway leading from stress to multiple health outcomes often linked to obesity, including cardiovascular disease, diabetes, strokes, ulcers, decreased immune functioning, and cancers (McEwen, 1998). Our claim that stress associated with weight-based identity threat contributes to allostatic load is consistent with evidence that diseases associated with obesity (e.g., hypertension, heart disease) are typically stress-related diseases as well as with evidence that weight-related diseases are most prevalent among groups who are the most stigmatized by being overweight (i.e., younger individuals, Whites, and women; Meunnig, 2008).
Weight Stigma Undermines Self-Regulation and Executive Functioning
Coping with the stress generated by weight-based social identity threat undermines overweight individuals' executive functioning and impairs their subsequent capacity for self-control over eating. Regulating the stress, negative emotions, intrusive thoughts, and interpersonal anxieties triggered by weight stigma is effortful. People may try, for example, to suppress activated stereotypes and negative emotions (Johns, Inzlicht, & Schmader, 2008), and/or compensate for negative stereotypes by working harder to make a good impression (e.g., Shelton, Richeson, & Salvatore, 2005; Miller, Rothblum, Felicio, & Brand, 1995). These responses make demands on cognitive resources involved in executive functions responsible for complex goal-directed behavior (Hofmann, Schmiechel, & Baddeley, 2012). According to process models of executive attention and self-control, actions that require effortful self-control cause a temporary shift in attentional and motivational processes that undermine subsequent attempts at self-regulation (Inzlicht & Schmeichel, 2012). Numerous studies confirm that contending with situations where one fears being a target of negative stereotypes or prejudice undermines performance on subsequent tasks requiring executive control, such as working memory tasks (e.g., operation span tasks; Schmader, Johns, & Forbes, 2008), inhibition tasks (e.g., the Stroop task; Inzlicht, McKay, & Aronson, 2006), and regulating the intake of tempting but unhealthy food (Inzlicht & Kang, 2010).
This aspect of our model has found empirical support using a variety of designs and measures. Major and colleagues (2012) found that overweight women tasked with delivering a videotaped speech about their qualities as a dating partner showed greater interference on the Stroop task compared to overweight women delivering an audiotaped speech or average weight women in either condition. Major, Hunger, Bunyan, and Miller (2014) found that self-perceived overweight women consumed more high-calorie snack foods after reading an article about the potential for weight-based discrimination compared to overweight women who read a neural topic or women who did not perceive themselves as overweight. Overweight women in the weight-stigmatizing condition also reported feeling less capable of regulating their food intake in the future than other women. Likewise, Schvey, Puhl, & Brownell (2011) found that overweight and obese women (but not average weight women) consumed more snack foods after viewing a compilation of weight-stigmatizing television and movie clips compared to those who watched neutral nature clips. Other findings also support the idea that weight-based identity threat undermines executive resources needed to regulate diet. For example, Brochu and Dovidio (2014) found that when weight-related stereotypes were activated prior to completing an online meal selection task, overweight (but not average weight) participants ordered significantly more calories compared to those in the control condition. Weight stigma is also related to more extreme reforms of dysregulated eating. For example, perceived weight-based discrimination and teasing are related to increased binge eating (Almeida, Savoy, & Boxer, 2011; Durso, Latner, & Hayashi, 2012; Haines, Neumark-Sztainer, Eisenberg, & Hannan, 2006).
It is also likely that weight-based social identity threat undermines self-regulatory resources necessary to maintain regular physical activity, although direct evidence for this proposition remains limited. There is experimental evidence to suggest that exposure to a weight-stigmatizing message alters exercise-related intentions and self-efficacy (Seacat & Mickelson, 2009), which are important components of successful self-regulation (Carver & Scheier, 1998). Overweight women subtly primed with the stereotype that heavy women are likely to have poor health habits subsequently had lower exercise and dietary health intentions than overweight women not primed with this stereotype, and this effect was partially mediated through decreased exercise and dietary self-efficacy (Seacat & Mickelson, 2009). Other research has found that weight-related criticism is associated with less physical activity among children (Faith, Leone, Ayers, Heo, & Pietrobelli, 2002) and weight-stigmatizing experiences are associated with decreased exercise among adults (Wott and Carels, 2010; but see Pearl, Puhl, & Dovido, 2014). Although findings such as these highlight the important role of weight stigma in physical activity, is unclear if findings such as these emerged as a result of diminished self-regulation, increased motivation to avoid stigma (see below), or some combination thereof. We hope that future research guided by our model will unpack precisely how weight-based social identity threat leads to decreased physical activity.
Weight stigma Compromises Psychological Health
Evidence that experiencing weight stigma is associated with poorer psychological outcomes is well established and has been reviewed extensively elsewhere (Puhl & Heuer, 2009). Indeed, many of the psychological effects routinely attributed to carrying excess weight – such as low self-esteem, greater depression and anxiety, and poorer quality of life – result more from the stigma faced by overweight individuals than from the weight itself (Carr, Friedman, & Jaffe, 2007; Hunger & Major, 2014). Hatzenbuehler, Keyes, and Hasin (2009) performed a comprehensive analysis of the effects of perceived weight discrimination on mental health. Using a nationally representative sample of overweight and obese individuals, Hatzenbuehler and colleagues found that those who had experienced any weight discrimination during the previous 12 months, compared to those who had not, were twice as likely to have current mood and anxiety disorder diagnoses and nearly 50% more likely to have a substance use disorder. Moreover, individuals who reported weight discrimination were three times as likely to be in the highest quartile of perceived stress. Importantly, these effects held when controlling for BMI, highlighting the importance of social treatment rather than objective weight status, per se. Research from other large-scale epidemiological studies has likewise shown that experiencing weight-based mistreatment is associated with lower self-acceptance, a construct analogous to self-esteem (Carr & Friedman, 2005). Hunger and Major (2014) found that weight stigma mediated the negative relationship between BMI and psychological wellbeing (i.e., self-esteem, depression, and quality of life). Interestingly, concerns about stigma emerged as a stronger predictor of health than did perceptions of discrimination, although these two components of weight stigma were strongly correlated.
We propose that weight-based social identity threat undermines mental health in part because it threatens the fundamental need for social connection (Baumeister & Leary, 1995). Recent experiments bolster this claim. Major and colleagues (2012) found that overweight women who were asked to deliver a speech about why they would be a good dating partner – a domain in which excess weight is acutely stigmatized – exhibited greater stress emotions when asked to speak while being videotaped versus audiotaped. Using a similar paradigm, Blodorn, Major, Hunger, and Miller (2014) found that this effect was mediated by concerns about social rejection. Specifically, overweight women who thought they could be seen while giving a speech about their positive dating qualities reported greater concerns about being rejected than overweight women who thought they could not be seen. Increased rejection concerns in turn predicted greater stress, increased shame, and decreased self-esteem. Weight was unrelated to psychological outcomes among women who thought they could not be seen. Interestingly, Blodorn and colleagues did not find evidence for weight-based social identity threat among men. Overweight men did not anticipate more social rejection when seen than unseen, possibly because men face less weight-related stigma than women do in the dating context (Fikkan & Rothblum, 2012). Further experimental research is needed to clarify how responses to weight-based identity threat can contribute to the development of clinically significant psychological problems (Hatzenbuehler et al., 2009), and to further delineate the domains in which men and women may differentially experience weight-based social identity threat.
Weight Stigma Increases Motivation to Avoid Stigma
One response to social identity threat is to avoid domains in which encountering stigma is likely to occur (Steele et al., 2002). However, for overweight individuals, some of the domains in which stigma is most commonly experienced are also those that can promote health and wellbeing. For example, experiencing weight stigma predicts an increased motivation to avoid exercising, particularly in public settings (Vartanian & Shaprow, 2008), and this effect is most pronounced among individuals who have internalized negative weight-related attitudes and societal beauty norms (Vartanian & Novak, 2011). Although motivation to avoid exercise is negatively related to self-reported exercise behavior, additional research is needed to examine the relationship between weight stigma and exercise avoidance using more ecologically valid methodologies (e.g., experiencing sampling; Seacat, Dougal, & Roy, 2014; Vartanian, Pinkus, & Smyth, 2014). Experienced and anticipated weight stigma may also contribute to health-care underutilization and avoidance. High levels of explicit and implicit weight biases among medical trainees and professionals are well-documented (Phelan et al., 2014; Sabin, Marini, & Nosek, 2012), including those specializing in obesity (Schwartz, Chambliss, Brownell, Blair, & Billington, 2003). Health care professionals are cited as a frequent source of weight-stigmatizing encounters (Puhl & Brownell, 2006), and obese patients report feeling disrespected, criticized, and blamed for their health problems by their physicians (Anderson & Wadden, 2004; but see Chang, Asch, & Werner, 2010). As a result, overweight and obese individuals may be less likely to engage in age-appropriate preventative care compared to their thin peers (e.g., cancer screening; Puhl & Heuer, 2010), putting them at additional risk for compromised health. Although stigma-related weight concerns are often cited as a reason for delaying or avoiding treatment (Amy, Aalborg, Lyons, & Keranen, 2006; Drury & Louis, 2002), direct support for this premise remains somewhat limited (Puhl & Heuer, 2009).
Experiencing or anticipating weight-based mistreatment may also undermine health by fostering social isolation. As discussed above, weight-based social identity threat leads to concerns of rejection (Blodorn et al., 2014), which may undermine existing close relationships and circumvent the formation of new social bonds. Rather than being a stable source of social support, research suggests that family members and close others are often a source of weight stigma for heavy individuals (Puhl & Brownell, 2006; Puhl et al., 2008). This could have a negative impact on overweight and obese individuals' health given the well-established effects of social support, social integration, and interaction quality on mental and physical health (Cohen, 2004). Research is needed to examine the extent to which weight-based social identity threat compromises social relationships and leads to avoidance of interpersonal relationships.
Weight Stigma Increases Motivation to Escape Stigma
Weight-based social identity threat may also increase the motivation to escape the stigma by losing weight, at the same time that it decreases the capacity to do so. Common responses to weight stigma include exercise avoidance (see above), refusal to diet (Myers & Rosen, 1999; Puhl & Brownell, 2006), and increased food intake (Major et al., 2014; Schvey et al., 2011). However, in the face of pervasive weight stigma and difficulties with sustained weight loss, heavy individuals sometimes attempt to diet and/or engage in unhealthy or disordered behaviors in an attempt to shed their stigma. Indeed, among teen boys and girls, weight-related teasing is associated with disordered eating behaviors such as skipping meals or taking diet pills (Neumark-Sztainer, Falkner, Story, Perry, Hannan, & Mulert, 2002). Weight teasing also prospectively predicts greater engagement in unhealthy weight control behaviors and increased likelihood of dieting among girls and binge eating among boys (Haines, et al., 2006). Although temporary weight loss may be achieved through such efforts, long term maintenance of weight loss is difficult if not impossible to achieve (Mann, Tomiyama, Lew, Westling, Chatman, & Samuels, 2007; Tomiyama, Alhstrom, & Mann, 2013). Furthermore, there is good evidence among adults that dieting actually predicts weight gain rather than weight loss over time. In a systemic review of caloric restriction research, Mann and colleagues (2007) conservatively estimated that 33-67% of dieters end up gaining more weight than they initially lost through dieting. They also noted that this likely underestimates weight gain due to dieting because of methodological issues (e.g., follow-up length, selective attrition) that bias the literature toward demonstrating the efficacy of dieting. Consistent with this claim, engaging in dieting behaviors prospectively predicts weight gain up ten years later among adolescents (Neumark, Wall, Story, & Standish, 2012).
Relationship to other Theoretical Accounts
Two recent papers also highlight the implications of weight stigma for weight gain and weight retention (Brewis, 2014; Tomiyama, 2014). Tomiyama's (2014) model converges with ours in proposing that experiences with weight stigma are stressful and promote eating and weight gain. However, her model focuses primarily on direct physiological pathways (i.e., cortisol-induced eating and fat deposition) and “comfort eating” as pathways through which this occurs, and direct experiences of weight stigma. Our social identity threat model also emphasizes how suspected and anticipated weight stigma can undermine health, and also highlights how chronic activation (and dysregulation) of the stress systems contributes to poor health through allostatic load.
Brewis (2014) proposes four ways in which experiences with weight stigma can lead to weight gain and contribute to the maintenance of obesity. Two of these pathways are common to our model: direct behavioral changes (e.g., altering the exercise, eating, and healthcare patterns of overweight individuals) and indirect effects of increased psychosocial stress. The other two pathways are unique to Brewis' model – changes in social relationships that alter health behaviors and socioeconomic consequences of weight-based discrimination. So too is her consideration of intergenerational effects (e.g., maternal stigma-related stress leading to weight gain in offspring). These novel mechanisms deserve increased empirical attention, as they highlight important extra-individual consequences of weight stigma that can undermine the mental and physical health of heavy individuals.
Summary and Conclusions
Although stigma is sometimes justified as way to encourage weight loss and motivate healthier behaviors among overweight individuals, growing evidence suggests that such efforts are likely to backfire. Rather than being an effective solution to obesity, weight stigma functions to threaten the social identity of overweight and obese individuals, initiating a cascade of psychological and physiological mechanisms with negative implications for mental and physical health. By increasing stress processes, undermining executive control and self-regulation, and increasing the motivation to avoid and/or escape stigma, weight-based social identity threat contributes to and exacerbates obesity-associated diseases (Meunnig, 2008) and promotes weight gain and retention (Hunger & Tomiyama, 2014; Jackson et al., 2014; Sutin & Terriciano, 2013). We believe our social identity threat model cogently frames the existing literature and will help guide future hypothesis-driven research.
Empirical and theoretical interest in weight stigma has grown dramatically since Puhl and Heuer (2009) published their seminal paper. Although their review remains important and timely, we believe that the next generation of weight stigma research can benefit from investigating theory-driven questions using an expanded methodological toolbox. Past research has done an excellent job documenting the prevalence and scope of weight stigma, and highlighting its numerous psychological and physical health correlates. We must now turn our focus toward better understanding the processes through which weight stigma can “get under the skin” to compromise psychological and physical health. This can be achieved through methodologically-rich research programs that combine the capacity to make causal claims that accompanies experimental designs with the external and ecological validity that comes with well-designed longitudinal and experience-sampling studies. Given the prevalence of overweight and obesity, and the evidence linking weight stigma to poor health, we hope our model motivates research aimed at further understanding and ultimately redressing weight stigmatization.
Figure 1.
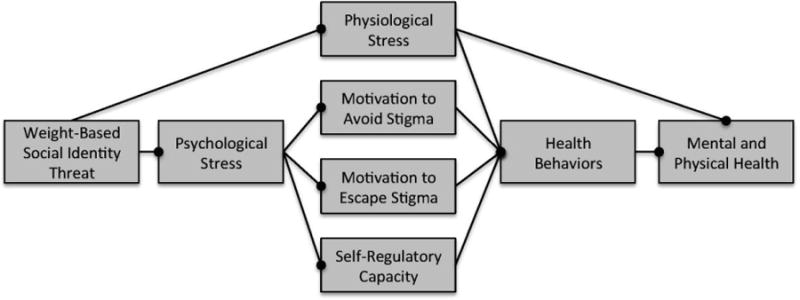
Theoretical model depicting the processes through which weight-based social identity threat contributes to poor mental and physical health.
Acknowledgments
This research was supported by NIH Grant 5R01HL112818-02 to Brenda Major.
References
- Adam TC, Epel ES. Stress, eating, and the reward system. Physiology & Behavior. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. International Journal of Obesity. 2006;30:147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- Anderson DA, Wadden TA. Bariatric surgery patients' views of their physicians' weight-related attitudes and practices. Obesity Research. 2004;12:1587–1595. doi: 10.1038/oby.2004.198. [DOI] [PubMed] [Google Scholar]
- Almeida L, Savoy S, Boxer P. The role of weight stigmatization in cumulative risk for binge eating. Journal of Clinical Psychology. 2011;67:278–292. doi: 10.1002/jclp.20749. [DOI] [PubMed] [Google Scholar]
- Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discimination among Americans, 1995-1996 through 2004-2006. Obesity. 2008;16(5):1129–1134. doi: 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutrition Journal. 2011;10:1–13. doi: 10.1186/1475-2891-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu S. F2-isoprostanes in human health and diseases: From molecular mechanisms to clinical implications. Antioxidants & Redox Signaling. 2008;10:1405–1434. doi: 10.1089/ars.2007.1956. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117:497–529. doi: 10.1037/0033-2909.117.3.497. [DOI] [PubMed] [Google Scholar]
- Bayer R. Stigma and the ethics of public health: not can we but should we. Social Science & Medicine. 2008;67:463–472. doi: 10.1016/j.socscimed.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obesity Reviews. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- Blascovich J, Mendes WB. Social psychophysiology and embodiment. In: Fiske ST, Gilbert DT, editors. The Handbook of Social Psychology. 5th. New York: Wiley; 2010. [Google Scholar]
- Blodorn A, Major B, Hunger JM, Miller CT. Expecting to be rejected: A mechanism underlying the negative psychological effects of weight-based social identity threat. Unpublished manuscript 2014 [Google Scholar]
- Brewis AA. Stigma and the perpetuation of obesity. Social Science & Medicine. 2014;118:152–158. doi: 10.1016/j.socscimed.2014.08.003.. [DOI] [PubMed] [Google Scholar]
- Brochu PM, Dovidio JF. Would you like fries (380 calories) with that? Menu labeling mitigates the impact of weight-based stereotype threat on food choice. Social Psychological and Personality Science. 2014;5:414–421. doi: 10.1177/1948550613499941. [DOI] [Google Scholar]
- Boyes AD, Latner JD. Weight stigma in existing romantic relationships. Journal of Sex & Marital Therapy. 2009;35:282–293. doi: 10.1080/00926230902851280. [DOI] [PubMed] [Google Scholar]
- Callahan D. Obesity: Chasing an elusive epidemic. Hastings Center Report. 2013a;43:40–43. doi: 10.1002/hast.114. [DOI] [PubMed] [Google Scholar]
- Callahan D. Children, stigma, and obesity. JAMA Pediatrics. 2013b;167:791–792. doi: 10.1001/jamapediatrics.2013.2814.. [DOI] [PubMed] [Google Scholar]
- Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. Journal of Health and Social Behavior. 2005;46:244–259. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- Carr D, Friedman MA, Jaffe K. Understanding the relationship between obesity and positive and negative affect: the role of psychosocial mechanisms. Body Image. 2007;4:165–177. doi: 10.1016/j.bodyim.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. New York: Cambridge University Press; 1998. [Google Scholar]
- Chang VW, Asch DA, Werner RM. Quality of care among obese patients. JAMA. 2010;303:1274–1281. doi: 10.1001/jama.2010.339. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status a meta-analysis of prospective evidence. Hypertension. 2010;55:1026–1032. doi: 10.1161/hypertensionaha.109.146621. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676.. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130:355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Gruenewald TL, Kemeny ME. When the social self is threatened: Shame, physiology, and health. Journal of Personality. 2004;72:1192–1216. doi: 10.1111/j.1467-6494.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- Drury A, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. Journal of the American Academy of Nurse Practitioners. 2002;14:554–561. doi: 10.1111/j.1745-7599.2002.tb00089.x. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, Hayashi K. Perceived discrimination is associated with binge eating in a community sample of non-overweight, overweight, and obese adults. Obesity Facts. 2012;5:869–880. doi: 10.1159/000345931. [DOI] [PubMed] [Google Scholar]
- Faith MS, Leone MA, Ayers TS, Heo M, Pietrobelli A. Weight criticism during physical activity, coping skills, and reported physical activity in children. Pediatrics. 2002;110:e23–e23. doi: 10.1542/peds.110.2.e23. [DOI] [PubMed] [Google Scholar]
- Fikkan JL, Rothblum ED. Is fat a feminist issue? Exploring the gendered nature of weight bias. Sex Roles. 2012;66:575–592. doi: 10.1007/s11199-011-0022-5. [DOI] [Google Scholar]
- Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ. Weight teasing and disordered eating behaviors in adolescents: Longitudinal findings from Project EAT (Eating Among Teens) Pediatrics. 2006;117:e209–e215. doi: 10.1542/peds.2005-1242. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity. 2009;17:2033–2039. doi: 10.1038/oby.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebl M, Xu J. Weighing the care: Physicians' reactions to the size of a patient. International Journal of Obesity. 2001;25:1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- Hilmert CJ, Kvasnicka LR. Blood pressure reactivity and emotional responses to stress: Perspectives on cardiovascular reactivity. Social and Personality Psychology Compass. 2010;4:470–483. doi: 10.1111/j.1751-9004.2010.00275.x. [DOI] [Google Scholar]
- Himmelstein MS, Incollingo Belsky AC, Tomiyama AJ. The weight of stigma: The effects of BMI and perceived body weight on cortisol reactivity to experiencing weight stigma. Obesity. doi: 10.1002/oby.20959. in press. [DOI] [PubMed] [Google Scholar]
- Hofmann W, Schmeichel BJ, Baddeley AD. Executive functions and self-regulation. Trends in Cognitive Sciences. 2012;16:174–180. doi: 10.1016/j.tics.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Hunger JM, Major B. Health Psychology. 2014. Weight stigma mediates the association between BMI and self-reported psychological and physical health. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunger JM, Tomiyama AJ. Weight labeling and obesity: A longitudinal study of girls aged 10 to 19 years. JAMA Pediatrics. 2014;168:579–580. doi: 10.1001/jamapediatrics.2014.122. [DOI] [PubMed] [Google Scholar]
- Inzlicht M, Kang SK. Stereotype threat spillover: How coping with threats to social identity affects aggression, eating, decision making, and attention. Journal of Personality and Social Psychology. 2010;99:467–481. doi: 10.1037/a0018951. [DOI] [PubMed] [Google Scholar]
- Inzlicht M, McKay L, Aronson J. Stigma as ego depletion how being the target of prejudice affects self-control. Psychological Science. 2006;17:262–269. doi: 10.1111/j.1467-9280.2006.01695.x. [DOI] [PubMed] [Google Scholar]
- Jackson SE, Beeken RJ, Wardle J. Perceived discrimination and changes in weight, waist circumference, and weight status. Obesity. 2014 doi: 10.1002/oby.20891. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns M, Inzlicht M, Schmader T. Stereotype threat and executive resource depletion: Examining the influence of emotion regulation. Journal of Experimental Psychology: General. 2008;137:691–705. doi: 10.1037/a0013834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King EB, Shapiro JR, Hebl MR, Singletary SL, Turner S. The stigma of obesity in customer service: a mechanism for remediation and bottom-line consequences of interpersonal discrimination. Journal of Applied Psychology. 2006;91:579–593. doi: 10.1037/0021-9010.91.3.579. [DOI] [PubMed] [Google Scholar]
- Latner JD, Wilson T, Jackson ML, Stunkard AJ. Greater history of weight-related stigmatizing experience is associated with greater weight loss in obesity treatment. Journal of Health Psychology. 2009;14:190–199. doi: 10.1177/1359105308100203. [DOI] [PubMed] [Google Scholar]
- Lovallo WR, Gerin W. Psychophysiological reactivity: mechanisms and pathways to cardiovascular disease. Psychosomatic Medicine. 2003;65:36–45. doi: 10.1097/01.PSY.0000033128.44101.C1. [DOI] [PubMed] [Google Scholar]
- Major B, O'Brien LT. The social psychology of stigma. Annual Review of Psychology. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- Major B, Eliezer D, Rieck H. The psychological weight of weight stigma. Social Psychological and Personality Science. 2012;3:651–658. doi: 10.1177/1948550611434400. [DOI] [Google Scholar]
- Major B, Hunger JM, Bunyan D, Miller CT. The ironic effects of weight stigma. Journal of Experimental Social Psychology. 2014;51:74–80. doi: 10.1016/j.jesp.2013.11.009. [DOI] [Google Scholar]
- Mann T, Tomiyama AJ, Westling E, Lew A, Samuels B, Chatman J. Medicare's search for effective obesity treatments: Diets are not the answer. American Psychologist. 2007;62:220–233. doi: 10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Salomon K, Kenyon K, Zhou F. Unfair treatment, discrimination, and ambulatory blood pressure in black and white adolescents. Health Psychology. 2005;24:258–265. doi: 10.1037/0278-6133.24.3.258. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Miller CT, Rothblum ED, Felicio D, Brand P. Compensating for stigma: Obese and nonobese women's reactions to being visible. Personality and Social Psychology Bulletin. 1995;21:1093–1106. doi: 10.1177/01461672952110010. [DOI] [Google Scholar]
- Muennig P. The body politic: the relationship between stigma and obesity-associated disease. BMC Public Health. 2008;8:128. doi: 10.1186/1471-2458-8-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers A, Rosen JC. Obesity stigmatization and coping: Relation to mental health symptoms, body image, and self-esteem. International Journal of Obesity. 1999;23:221–230. doi: 10.1038/sj.ijo.0800765. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. International Journal of Obesity. 2002;26:123–131. doi: 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, Standish AR. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. Journal of Adolescent Health. 2012;50:80–86. doi: 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman E, O'Connor DB, Conner M. Daily hassles and eating behavior: The role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32:125–132. doi: 10.1016/j.psyneuen.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl RL, Puhl RM, Dovidio JF. Differential effects of weight bias experiences and internalization on exercise among women with overweight and obesity. Journal of Health Psychology. 2014 doi: 10.1177/1359105313520338. [DOI] [PubMed] [Google Scholar]
- Phelan SM, Dovidio JF, Puhl RM, Burgess DJ, Nelson DB, Yeazel MW, et al. Ryn M. Implicit and explicit weight bias in a national sample of 4,732 medical students: The medical student CHANGES study. Obesity. 2014;22:1201–1208. doi: 10.1002/oby.20687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: Prevalence and comparison to race and gender discrimination in America. International Journal of Obesity. 2008;32:992–1000. doi: 10.1038/ijo.2008.22. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Brownell KD. Confronting and coping with weight stigma: An investigation of overweight and obese adults. Obesity. 2006;14:1802–1815. doi: 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. Obesity stigma: Important considerations for public health. American Journal of Public Health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Education Research. 2008;23:347–358. doi: 10.1093/her/cym052. [DOI] [PubMed] [Google Scholar]
- Roehling MV, Roehling PV, Pichler S. The relationship between body weight and perceived weight-related employment discrimination: The role of sex and race. Journal of Vocational Behavior. 2007;71:300–318. doi: 10.1016/j.jvb.2007.04.008. [DOI] [Google Scholar]
- Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PloS One. 2012;7:e48448. doi: 10.1371/journal.pone.0048448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saguy AC, Frederick D, Gruys K. Reporting risk, producing prejudice: How news reporting on obesity shapes attitudes about health risk, policy, and prejudice. Social Science & Medicine. 2014;111:125–133. doi: 10.1016/j.socscimed.2014.03.026. [DOI] [PubMed] [Google Scholar]
- Schmader T, Johns M, Forbes C. An integrated process model of stereotype threat effects on performance. Psychological Review. 2008;115:336–356. doi: 10.1037/0033-295X.115.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seacat JD, Dougal SC, Roy D. A daily diary assessment of female weight stigmatization. Journal of Health Hsychology. 2014 doi: 10.1177/1359105314525067. [DOI] [PubMed] [Google Scholar]
- Shapiro JR, Neuberg SL. From stereotype threat to stereotype threats: Implications of a multi-threat framework for causes, moderators, mediators, consequences, and interventions. Personality and Social Psychology Review. 2007;11:107–130. doi: 10.1177/1088868306294790. [DOI] [PubMed] [Google Scholar]
- Shelton JN, Richeson JA, Salvatore J. Expecting to be the target of prejudice: Implications for interethnic interactions. Personality and Social Psychology Bulletin. 2005;31:1189–1202. doi: 10.1177/0146167205274894. [DOI] [PubMed] [Google Scholar]
- Schvey NA, Puhl RM, Brownell KD. The impact of weight stigma on caloric consumption. Obesity. 2011;19:1957–62. doi: 10.1038/oby.2011.204. [DOI] [PubMed] [Google Scholar]
- Schvey NA, Puhl RM, Brownell KD. The stress of stigma: exploring the effect of weight stigma on cortisol reactivity. Psychosomatic Medicine. 2014;76:156–62. doi: 10.1097/PSY.0000000000000031. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Chambliss HON, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obesity Research. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- Steele CM, Spencer SJ, Aronson J. Contending with group image: The psychology of stereotype and social identity threat. Advances in Experimental Social Psychology. 2002;34:379–439. doi: 10.1016/S0065-2601(02)80009-0. [DOI] [Google Scholar]
- Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Social Science & Medicine. 2008;67:420–430. doi: 10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Stephan Y, Suchetti M, Terreciano A. Perceived weight discrimination and C-reactive protein. Obesity. 2014 doi: 10.1002/oby.20789. Advanced online publication. [DOI] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A. Perceived weight discrimination and obesity. PLoS One. 2013;8:e70048. doi: 10.1371/journal.pone.0070048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama AJ. Weight stigma is stressful: A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite. 2014;82:8–15. doi: 10.1016/j.appet.2014.06.108. [DOI] [PubMed] [Google Scholar]
- Tomiyama AJ, Ahlstrom B, Mann T. Long-term effects of dieting: Is weight loss related to health? Social and Personality Psychology Compass. 2013;7:861–877. [Google Scholar]
- Tomiyama AJ, Epel ES, McClatchey TM, Poelke G, Kemeny ME, McCoy SK, Daubenmier J. Associations of weight stigma with cortisol and oxidative stress independent of adiposity. Health Psychology. 2014;33:862–867. doi: 10.1037/hea0000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartanian LR, Novak SA. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity. 2011;19:757–762. doi: 10.1038/oby.2010.234. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Pinkus R, Smyth JM. The phenomenology of weight stigma in everyday life. Journal of Contextual Behavioral Science. 2014;3:196–202. doi: 10.1016/j.jcbs.2014.01.003. [DOI] [Google Scholar]
- Vartanian LR, Shaprow JG. Effects of weight stigma on exercise motivation and behavior: A preliminary investigation among college-aged females. Journal of Health Psychology. 2008;13:131–138. doi: 10.1177/1359105307084318. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Smyth JM. Primum non nocere: Obesity stigma and public health. Journal of Bioethical Inquiry. 2013;10:49–57. doi: 10.1007/s11673-012-9412-9. [DOI] [PubMed] [Google Scholar]
- Wott CB, Carels RA. Overt weight stigma, psychological distress and weight loss treatment outcomes. Journal of Health Psychology. 2010;15:608–614. doi: 10.1177/1359105309355339. [DOI] [PubMed] [Google Scholar]


