Abstract
Background:
In order to most appropriately allocate healthcare and research funding for cancer, it is important to have accurate population-based incidence data. The Saudi Cancer Registry (SCR) provides such information, covering the time period from 1994 to the present day. The current report concerns an overview of cancer incidence statistics for Saudi Arabia in 2012.
Methods:
The SCR collects data from healthcare facilities throughout the Kingdom of Saudi Arabia. All newly diagnosed cases of cancer are recorded, with information on site and histology. For the present report, age-standardised and age-specific incidence rates (ASR, AIR, respectively) were calculated, with attention to gender-specific and regional differences.
Results:
The total number of incident cases of cancer identified by the SCR in 2012 was 14,336, with 6,791 (47.5%) among males and 7,545 (52.6%) among females. Of this total, 11,034 cases (76.9%) occurred in patients of Saudi origin. For Saudi males, the overall ASR (inc. all cancer sites) was 78.1 per 100,000 people, while that for females was 86.7. Incidence varied by region, with the Eastern region and Riyadh displaying the highest ASRs for both males and females, and Hail and Jazan displaying the lowest. Incidence varied by gender, with colorectal cancer (13.3%), non-Hodgkin lymphoma (NHL; 8.4%), and leukaemia (8.2%) being the most common types in males, and breast (25.8%), thyroid (11.7%), and colorectal cancers (9.3%) being the most common in females.
Conclusions:
This analysis of cancer incidence in Saudi Arabia demonstrated significant differences according to gender, age, and region of the Kingdom. The data should help ensure the most appropriate allocation of resources, with the aim of minimising the healthcare burden associated with cancer.
Keywords: Cancer, incidence, Saudi Arabia, registry
Introduction
There are many benefits to acquiring information regarding cancer incidence rates, and owing to the constant changes in diet and lifestyle, the availability of recent data is highly valuable. In terms of public health policy, knowledge regarding the most prevalent types of cancer can aid in optimising distribution of resources. Screening programmes, such as those for breast, cervical, and colorectal cancer have demonstrated mortality benefits (Hewitson et al., 2008; Sankaranarayanan, 2014; Nelson et al., 2016). However, use of available facilities in Saudi Arabia has been shown to be poor, and variable across regions (Almadi et al., 2015; El Bcheraoui et al., 2015). The ability to direct patient awareness initiatives towards the highest risk areas would therefore be beneficial (Abdelhadi, 2006; Ravichandran et al., 2011; Radi, 2013). Introduction of education programmes for reducing risk factors such as smoking, and improving diet and lifestyle may also be beneficial (Midhet and Sharaf, 2011). In addition to aiding prevention and diagnosis of cancer, accurate epidemiological data can also be used for allocation of funding for research on treatments.
Cancer registries enable the collection of data regarding the prevalence and incidence of different types of cancer, and the associated mortality. We established the ongoing Saudi Cancer Registry (SCR) in 1992 to define the population-based incidence of cancer throughout the 13 administrative regions of Saudi Arabia. Previous reports have demonstrated an increase in the burden of cancer over time, as is evident throughout the world. Furthermore, the relative incidences of different types of cancer have changed, highlighting the need for up-to-date information to be readily accessible. The most recent complete data set includes new cases of cancer during 2012. Here, we provided an overview the information that we have collected, compared the incidence rates for different types of cancer in terms of gender and regions of the Kingdom.
Materials and Methods
Organisational structure of the Saudi Cancer Registry
The SCR was established by the Ministry of Health in conjunction with representatives from the King Faisal Specialist Hospital and Research Centre, and the Medical Services Department of the Ministry of Defence and Aviation, the Ministry of Interior, the Ministry of National Guard, King Saud University, and King Faisal University. Five regional branches and five hospital-based offices were set up to ensure the quality and accuracy of data collection procedure throughout the Kingdom. All 13 administrative regions of Saudi Arabia were covered (Figure 1).
Figure 1.
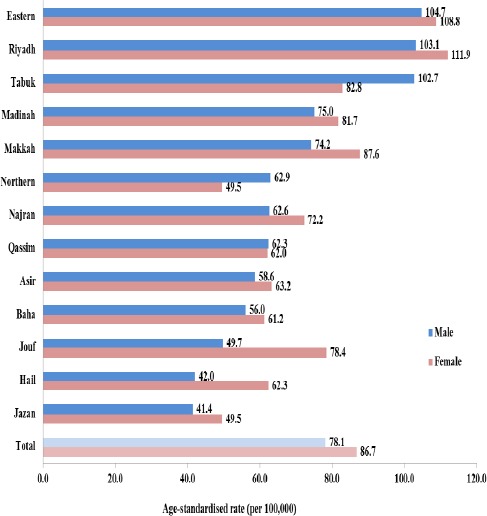
Total Incidence in 2012 by Region and Gender – Age-Standardised Rate. Legend, Incidence standardised to age distribution of the world population (Doll et al., 1966).
Data collection
As a mandatory notifiable disease, the SCR had full access to data from all Ministry of Health and governmental hospitals, as well as private hospitals and clinics. Data were taken from patients’ medical records and assimilated by SCR-trained cancer registrars. The data included personal identification number, demographics, and tumour details. The primary site and histology of the malignancy were noted and classified according to the International Classification of Diseases for Oncology 3rd Edition, 2000 (ICD-O-3; World Health Organization). Quality control was performed by verifying the site of the malignancy, the morphology, staging, and case linkage (between tumour and patient).
Data management
For data analysis, the ICD-O-3 codes were converted to the corresponding ICD-10 codes (Table 1). Cases were excluded if their ICD-O-3 codes could not be converted, including carcinoma in situ (CIS) malignancies and haematopoietic disease.
Table 1.
The Ten Most Common Cancers amongst Saudis (New Cases in 2012)
| Total (11,034 cases) | % | Male (5,067 cases) | % | Female (5,967 cases) | % | |
|---|---|---|---|---|---|---|
| 1 | Breast | 14.2 | Colorectal | 13.3 | Breast | 25.8 |
| 2 | Colorectal | 11.1 | NHL | 8.4 | Thyroid | 11.7 |
| 3 | Thyroid | 8.1 | Leukaemia | 8.2 | Colorectal | 9.3 |
| 4 | Leukaemia | 6.8 | Liver | 6.8 | Leukaemia | 5.5 |
| 5 | NHL | 6.7 | Lung | 6.6 | NHL | 5.3 |
| 6 | Liver | 4.3 | Prostate | 5.7 | Corpus uteri | 5.3 |
| 7 | Lung | 4.2 | Hodgkin disease | 3.8 | Ovary | 3.2 |
| 8 | Hodgkin disease | 3.2 | Bladder | 3.8 | Hodgkin disease | 2.7 |
| 9 | Corpus uteri | 2.9 | Thyroid | 3.8 | Cervix uteri | 2.3 |
| 10 | Kidney | 2.8 | Kidney | 3.7 | Liver | 2.2 |
NHL, non-Hodgkin lymphoma
Incidence rate was defined as the rate at which new event occur in a population. It was calculated as the number of new cases of disease arising in a population over a defined time period, divided by the population at risk of developing that disease. Crude incidence rate for a cancer site is the total number of cases registered as a proportion of the total population. It denotes the approximate number of cases occurring in each 100,000 individuals. All rates are thus, expressed as per 100,000 population. Relative frequency was defined as the number of specific cancer cases registered relative to the total number of all cancer. It was expressed as a percentage. Cancer rank measure reflected the importance of a specific cancer site relative to other sites, in terms of the number of registrations. Ranking illustrates the most and least frequent cancer sites in a population according to their frequency. Average age-specific incidence rate (AIR) was defined as the number of cancer cases occurring during a specific period in a population of a specific age and sex group, divided by the number of mid-year population of that age and sex group. Age-standardized rate (ASR) was defined as the summary measure of a rate that a population would have if it had a standard age structure. The most frequently used standard population is the World Standard Population. The calculated incidence is known as the World Standardized Incidence Rate. The rate is expressed per 100,000 populations.
For each cancer site, the age-standardised incidence rate (ASR) per 100,000 people for diagnoses in 2012 was calculated for both sexes. The age distribution used was the standard world population (Table 2) (Doll et al., 1966). Data were collected for both Saudis and non-Saudis; however, the present report focused on incidence in patients of Saudi origin only. All cases abstracted and entered in CanReg program were reviewed by independent registrars for completeness and correctness of data according to attached source documents.
Table 2.
Change in Age-Standardised Incidence Rate for Saudis Since the Start of the Saudi Cancer Registry (10 Most Common According to 2012 Data)
| 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | |||||||||||||||||||
| Colorectal | 4.2 | 4.3 | 3.5 | 3.8 | 4.1 | 4.8 | 4.9 | 5.3 | 6 | 7.3 | 8.3 | 10.2 | 9.6 | 9.4 | 9.2 | 11.6 | 9.9 | 11.3 | 11.1 |
| NHL | 6.6 | 5 | 5.5 | 5 | 6.2 | 6.1 | 5.4 | 5 | 5.2 | 6.4 | 6.2 | 6.5 | 6.7 | 7.1 | 6.2 | 7 | 6.2 | 6.4 | 6.2 |
| Leukaemia | 4.3 | 3.6 | 3.9 | 4.2 | 4.5 | 4 | 4.1 | 4.8 | 4.3 | 4 | 4.2 | 3.8 | 5 | 4.4 | 4.7 | 4.7 | 4.3 | 4.5 | 5 |
| Liver | 8.7 | 8.6 | 7.5 | 7.1 | 8.4 | 7.5 | 7.3 | 7.3 | 7.1 | 7.1 | 6.6 | 6.8 | 8.3 | 7.2 | 6.9 | 6.6 | 6.4 | 6.1 | 6.3 |
| Lung | 5.6 | 5.3 | 4.9 | 4.4 | 5.8 | 5.2 | 5 | 4.8 | 5 | 5.1 | 5.9 | 6.5 | 6.2 | 6.9 | 6 | 6 | 5.8 | 6.4 | 5.9 |
| Prostate | 4 | 3.9 | 3.8 | 2.9 | 3.9 | 3.5 | 4 | 4.4 | 4.3 | 4.5 | 5.7 | 6.4 | 6.3 | 5.7 | 5.9 | 6.3 | 5.5 | 6 | 5.3 |
| Hodgkin disease | 2.1 | 1.9 | 1.7 | 1.5 | 2.2 | 1.9 | 1.8 | 2.1 | 1.9 | 2 | 2.4 | 2.1 | 2.1 | 2.1 | 2.1 | 2.4 | 2.1 | 1.9 | 2 |
| Bladder | 4.6 | 4.3 | 3.4 | 3.2 | 3.8 | 3.7 | 3.9 | 3.4 | 3.5 | 4.1 | 4 | 3.7 | 4.2 | 3.5 | 3.7 | 4.1 | 3.6 | 3.3 | 3.2 |
| Thyroid | 2 | 1.5 | 1.5 | 1.8 | 1.9 | 1.7 | 1.6 | 1.6 | 1.9 | 1.7 | 1.8 | 1.6 | 2.1 | 1.9 | 2.1 | 2.2 | 2.3 | 2.2 | 2.7 |
| Kidney | 1.8 | 2 | 1.4 | 1.5 | 1.7 | 1.7 | 1.7 | 1.9 | 1.8 | 1.8 | 2.5 | 2.1 | 2.7 | 2.7 | 2.8 | 3.2 | 2.9 | 2.9 | 2.8 |
| Female | |||||||||||||||||||
| Breast | 13.3 | 13 | 13.2 | 12.5 | 13.8 | 12.4 | 13.5 | 12 | 13.9 | 14.6 | 16.1 | 18.4 | 18.1 | 20.5 | 20.3 | 23.4 | 24.9 | 23.4 | 22.1 |
| Thyroid | 5.5 | 5.2 | 4.7 | 4.9 | 5.8 | 5.6 | 4.8 | 4.7 | 4.8 | 6.3 | 5.7 | 6.2 | 6.6 | 6.4 | 7 | 8.1 | 7.5 | 8.1 | 8.3 |
| Colorectal | 3.9 | 4.4 | 4.2 | 4.2 | 3.9 | 5 | 4.4 | 5.4 | 5.3 | 5.9 | 6.7 | 7.3 | 8.3 | 7.6 | 8.5 | 9.7 | 9.2 | 9 | 9 |
| Leukaemia | 2.8 | 3.3 | 2.8 | 2.8 | 2.6 | 3.2 | 3.6 | 3.1 | 3.2 | 3.1 | 3.2 | 2.9 | 3.7 | 3.4 | 3.3 | 3.8 | 3.4 | 4 | 3.8 |
| NHL | 4.2 | 4.2 | 4.1 | 3.9 | 5 | 4.1 | 4.1 | 4.4 | 4.4 | 5 | 4.8 | 5.2 | 5.1 | 5.1 | 5.6 | 5.1 | 5.2 | 4.8 | 4.7 |
| Corpus uteri | 2.1 | 1.4 | 1.4 | 1.5 | 2 | 1.6 | 2.5 | 2 | 2.2 | 2.7 | 3 | 3.5 | 3.8 | 4 | 4 | 5.4 | 4.6 | 5.8 | 5.4 |
| Ovary | 2.9 | 3 | 2.7 | 3.1 | 3.1 | 2.3 | 2.2 | 2.4 | 2.2 | 2.4 | 2.4 | 3 | 2.9 | 2.6 | 3.2 | 3.1 | 3 | 3.1 | 3 |
| Hodgkin disease | 1.4 | 1.3 | 1 | 1.1 | 1.3 | 1.2 | 1.3 | 1.2 | 1.1 | 1.6 | 1.4 | 1.3 | 1.6 | 1.6 | 1.6 | 1.8 | 1.6 | 1.7 | 1.6 |
| Cervix uteri | 2.4 | 2.2 | 2.5 | 2.2 | 2.8 | 2 | 1.9 | 2 | 1.8 | 1.9 | 1.8 | 2.1 | 1.5 | 1.8 | 1.7 | 1.8 | 1.5 | 1.7 | 2.1 |
| Liver | 3.9 | 3 | 3.3 | 2.9 | 3.8 | 2.7 | 3.2 | 2.7 | 2.8 | 3.3 | 2.9 | 2.6 | 3.3 | 2.8 | 2.6 | 3 | 3.1 | 2.9 | 2.3 |
Incidence standardised to age distribution of the world population (Doll et al., 1966); NHL, non-Hodgkin lymphoma
The CanReg 4.33 software (International Agency for Research on Cancer [IARC]) was used to perform the analyses.
Results
Summary of overall cancer incidence in 2012
The total number of incident cases of cancer identified by the SCR in 2012 was 14,336, with 6,791 (47.5%) among males and 7,545 (52.6%) among females. Of this total, 11,034 cases (76.9%) occurred in patients of Saudi origin, 3,393 cases (22.9%) occurred in non-Saudis, and 120 cases (0.8%) occurred in patients with an unknown nationality. These latter two groups were excluded from the present analysis, along with 390 cases where the ICD-O-3 code could not be converted to an ICD-10 code.
Diagnosis of malignancy was confirmed histologically in 88.3% of the cases, and hematological and cytologically in 5.5% of cases. Clinically confirmed cases were 0.2%, tumor marker 0.1%, radiologically confirmed cases were 2.6%, cases confirmed by death certificate only were 2.5% and the method of diagnosis was unknown for 0.7% of the cases.
For Saudi males, the overall ASR (inc. all cancer sites) was 78.1 per 100,000 people, while that for females was 86.7. Cancer incidence varied by region; that is Eastern region and Riyadh displayed the highest ASRs for both males and females, but Hail and Jazan displayed the lowest incidence (Figure 1).
Higher incidence was found for males in the majority of regions; whereas, this trend reversed for Tabuk and the Northern region. Evaluating the incidence change from the start of the SCR in 1994, a general upward trend was observed for both males and females, although with significant fluctuations (Figure 2).
Figure 2.
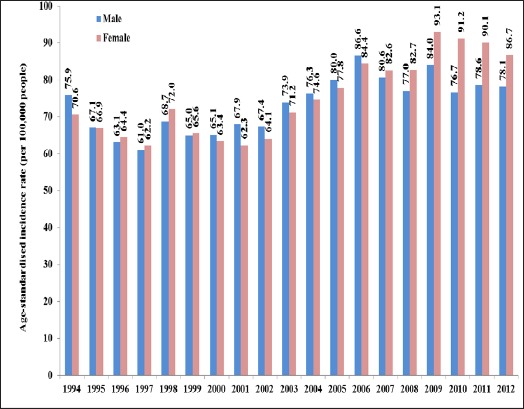
Change in Cancer Incidence with Time (All Sites). Legend, Incidence standardised to age distribution of the world population (Doll et al., 1966).
Most common cancers diagnosed in Saudis in 2012
By gender
For the total population of Saudis, the most common cancers diagnosed in 2012 were breast (14.2%), colorectal (11.1%) and thyroid (8.1%) (Table 1). Incidence varied by genderwhile colorectal (13.3%), non-Hodgkin lymphoma (NHL; 8.4%), and leukaemia (8.2%) being the most common for males, breast (25.8%), thyroid (11.7%), and colorectal (9.3%) being the most common for females.
By region
Incidence also varied greatly according to region (Figure 3). For Saudi males, the Eastern region and Riyadh had the highest ASRs for four out of the five most common cancers. The notable exception was the low incidence of liver cancer in the Eastern region (4.4 vs. 11.0 for highest), which was alongside a much higher rate of lung cancer in comparison to the other regions (12.0 vs. 7.2 for second highest). For women, trends were less evident. The highest ASRs for breast cancer were found in the Eastern region (32.6) and Jouf (31.6) butAsir (10.8) and Jazan (7.7) had the lowest ASRs. Other sites varied, but Riyadh was consistently among the top 3 regions with the highest rates.
Figure 3.
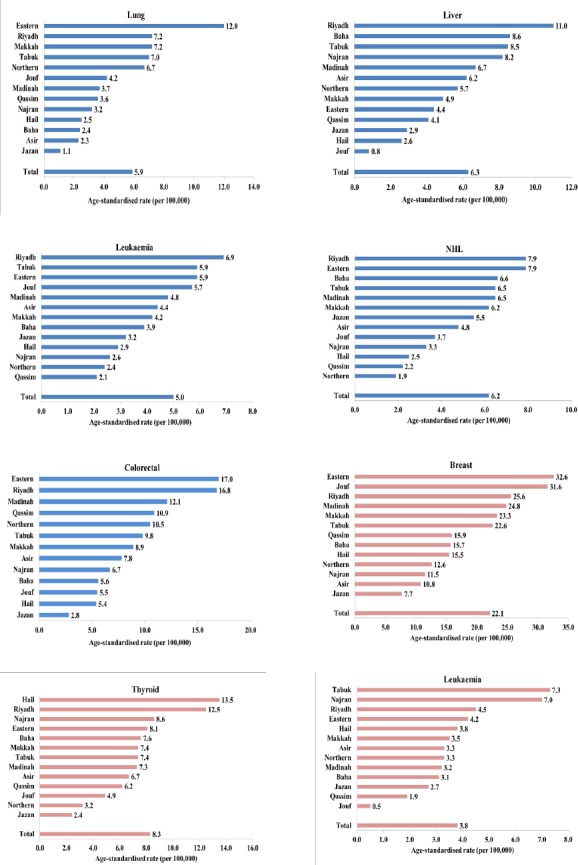
Five Most Common Cancer Types by Region and Gender – Age-Standardised Rate. Legend, Incidence standardised to age distribution of the world population (Doll et al., 1966)
By age
AIRs (per 100,000 people) were calculated for the five most commonly diagnosed cancers for males and females in 2012 (Figure 4). For males, incidence of each of the cancers remained fairly stable up to the age of 35 years. After this point, incidence increased exponentially, with the steepest slope being that for colorectal cancer, which reached a peak of 85.5 at 70–74 years. For children of 0–4 years, the AIR for leukaemia was higher (6.6) than that for the other top four cancers, which all had values ≤1.4. This particular cancer also increased to a lesser extent after the age of 35, reaching only 27.6 at age ≥ 75 years, which is in contrast to the 81.3 and 70.7 found for colorectal and lung cancer, respectively.
Figure 4.
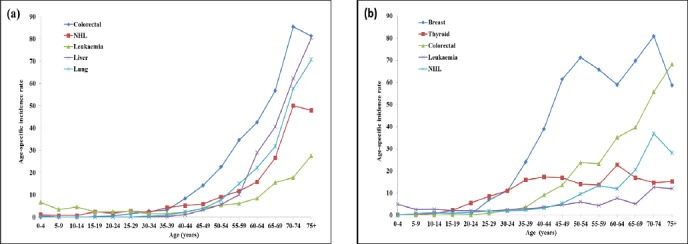
Five Most Common Cancer Types – Age-Specific Incidence Rates. Legend: Age-specific incidence rates for five most common cancer types according to percentage of total cases. (a) male; (b) female; NHL, non-Hodgkin lymphoma
For females, thyroid cancer incidence started to increase at age of 15–19 years, reaching a peak of 22.7 at 60–64 years. Breast cancer incidence rose steeply from the age of 20–24 years to 50–54 years. It then decreased slightly before rising again to reach a peak of 80.9 at 70–74 years. The AIR for leukaemia followed the same trend in women as for men, with a value of 4.9 for children aged 0–4 years, rising to a maximum of 12.6 at 70–74 years.
Changes in incidence of the ten most common cancers during the SCR
For Saudi males, there were few trends in incidence over the years from 1994 to 2012 (Table 2). The ASR of colorectal cancer, being the most common, remained at a relatively stable rate of 4–5 per 100,000 people up to 2000. After this point, it increased to a peak of 11.6 in 2009 and plateauing at 11.3 and 11.1 in 2011 and 2012. Lung cancer incidence appeared to drop between 2011 and 2012 (6.4 to 5.9), while liver cancer underwent a gradual decrease from 8.7 in 1994 to 6.3 in 2012. The other forms that made up the top ten most common fluctuated within 2.5 per 100,000 people.
For Saudi females, a number of cancers increased in rate during SCR up to 2012 (Table 2). The greatest increase was for breast cancer, rising from 13.3 to 22.1 during this time. The other cancers that increased were thyroid (5.5 to 8.3), colorectal (3.9 to 9.0), and corpus uteri (2.1 to 5.4). As was found for male Saudis, liver cancer incidence decreased gradually from 1994 to 2012 (3.9 to 2.3), while none of the other top ten most common cancers in females decreased to any great extent during this time.
Discussion
This comprehensive analysis of cancer incidence in Saudi Arabia demonstrated significant differences with respect to gender, age, and region. These findings can contribute to allocate the resources purposefully for cancer incidence control.
According to International Agency for Research on Cancer (IARC), the overall cancer incidence in Saudi Arabia in 2012 (male: 78.1; female: 86.7 [per 100,000 people]) was found to be much lower than global cancer prevalence (male: 204.9; female: 165.2 [per 100,000 people]). However, it should be noted that the IARC data were based on incidence projections rather than exact number of cases within 2012. When looking at the countries in the region surrounding Saudi Arabia, a number were found to have similar overall incidence, including the United Arab Emirates (UAE), Kuwait, Yemen, and Oman (International Agency for Research on Cancer, 2012c; 2012b; 2012j; 2012i; 2012f; 2012a; 2012e; 2012d) . On the other hand, Iraq, Iran and Jordan had much higher rates (Mohagheghi et al., 2009; International Agency for Research on Cancer, 2012c; 2012b). While incidence rates fluctuated from 1994 to 2012, there was a general increasing trend concerning all cancer types.
The most common types of cancer for Saudi men were colorectal, NHL, and leukaemia. Colorectal cancer was the third most frequently diagnosed one in the world in 2012 (International Agency for Research on Cancer, 2012h), and was consistently among the third most commonly diagnosed cancer in most Middle East countries, including Jordan (International Agency for Research on Cancer, 2012e), the UAE (International Agency for Research on Cancer, 2012c), Kuwait (International Agency for Research on Cancer, 2012e), Bahrain (International Agency for Research on Cancer, 2012j), and Oman (International Agency for Research on Cancer, 2012f). The incidence rates of colorectal cancer have increased during SCR, reaching a peak in 2009. However, the data from 2012 show a plateau indicating that the situation may be improving . Future research should be carefully targeted in order to determine whether this particular year is an anomaly or colorectal cancer incidence indeed stopped increasing in that year. In contrast with the majority of other countries, prostate cancer was the 6th most commonly diagnosed cancer among Saudi males (ASR: 5.3 per 100,000 people), which is much lower than the world overall incidence rate of prostate cancer (ASR: 30.6) (International Agency for Research on Cancer, 2012h) indicating the superiority of prostate specific antigen (PSA) screening. One encouraging finding is that the incidence of liver cancer has decreased steadily from 1994 to 2012. This is likely linked to the decline in prevalence of viral hepatitis, a significant risk factor for this disease (Abdo and Sanai, 2015). A major contributory factor to this decline is probably the establishment of the Ministry of Health hepatitis vaccination program, which was introduced for all newly born babies in 1989 (Al-Faleh et al., 1993). Despite this, the decline in the prevalence of viral hepatitis occurred in all age groups. Improvement of health care services, and strict infection control polices may also contribute to reduction in cases of viral hepatitis.
For Saudi women, breast cancer was by far the most common type of cancer diagnosed in 2012, as in the rest of the world (International Agency for Research on Cancer, 2012g). Furthermore, its incidence has risen significantly from 1994, the first year of the SCR, a trend that is likely to continue as the population ages. These findings highlight the importance of screening programs and health education to enable early identification and treatment of breast malignancies. One study in Saudi Arabia found that many women are not taking advantage of the available screening services (El Bcheraoui et al., 2015), while another study demonstrated inadequate awareness of the disease (Radi, 2013). As was found for males, colorectal cancer was one of the most commonly diagnosed cancers in females in 2012, which is again in agreement with other countries of the region (International Agency for Research on Cancer, 2012d; 2012b; 2012a) and the world overall (International Agency for Research on Cancer, 2012g). Incidence of colorectal cancer peaked in 2009, but did not decrease greatly since then, indicating that this form of cancer is an ongoing problem. Accordingly, screening programs promotion is suggested again for early identification (Almadi et al., 2015). The increasing incidence of thyroid cancer in females is also notable. The ASR for 2012 was the highest since the SCR began, while the incidence in males has been increasing slowly since 1994. As the second most commonly diagnosed cancer in Saudi females, this type of cancer is likely to become a significant healthcare burden with increasing incidence. While a family history of thyroid cancer and being female are non-modifiable risk factors, there are a number of modifiable factors that should be addressed, including being overweight and consuming a diet low in iodine (Hussain et al., 2013). As for males, liver cancer has undergone a decrease in incidence, reaching an ASR of just 2.3 per 100,000 people.
For Saudi males, incidence of each of the five most commonly diagnosed cancers in 2012 increased with age from approximately 40 years old onwards. Colorectal cancer underwent the steepest increase, more than doubling from age 40 years to 50 years. As a result of the aging of the population, this form of cancer could become a significant healthcare burden in the near future, again highlighting the importance of screening.
Colorectal cancer incidence also increased with age in females, again from approximately 40 years onwards. Breast cancer, on the other hand, started to increase in incidence from the younger age of 20–25 years. Mammography screening is routinely available for women over the age of 50 years, while breast self-examination is an important practice for women of all ages. However, knowledge of these detection measures is poor in Saudi Arabia (Radi, 2013; El Bcheraoui et al., 2015; Al-Zalabani et al., 2016). For breast cancer, it is apparent from the SCR data that the disease is generally diagnosed in a relatively younger population compared to age specific incidence in Western populations (International Agency for Research on Cancer, 2012f; 2012a).
The incidence of cancer varied greatly depending on the administrative region of Saudi Arabia. The Eastern region and Riyadh displayed the highest rates. This might be due to better availability of advanced medical services in the capital of Riyadh, but is also likely related to the presence of oil industry in the Eastern province (Al-Ahmadi and Al-Zahrani, 2013). Jazan, the poorest region of the Kingdom, was found to have the lowest incidence, in both males and females.
There were notable gender differences in cancer incidence, with females generally having higher ASRs, in particular in Jouf and Hail. In contrast, in Tabuk and the Northern region, incidence was higher for males.
In general, Riyadh and the Eastern region displayed the highest incidences of the top five most commonly diagnosed cancers in Saudi males. This was with the exception of liver cancer, which was diagnosed less frequently in the Eastern region, perhaps indicating that this area had been more successful than others in reducing the prevalence of viral hepatitis. This could be a result of the hospitals in this area being more organised and modern. However, the incidence of lung cancer was particularly high in this region which is likely linked to the petroleum and chemical industries based there.
Cancer incidence for Saudi females was also high in Riyadh, while having a large ASR for each of the top five most commonly diagnosed cancers. The Eastern region had the highest incidence of breast cancer and, similar to the males, colorectal cancer was frequently diagnosed. Incidence of thyroid cancer in Saudi females was strikingly high in the Hail region. It is possible that the genetic risk of such malignancies has accumulated; however, environmental factors should not be ruled out. It is interesting that this high incidence of thyroid cancer was not noted in a previous report regarding the period from 2001 to 2008, where the ASR for Hail was of an intermediate magnitude among the other regions (Alghamdi et al., 2015). This finding suggests a large increase in the incidence of thyroid cancer in this area over the four years from 2008 to 2012. Incidence of leukaemia was found to be high in the Saudi females living in the Tabuk and Najran regions. An earlier report, including data from the SCRshowed that Najran had the highest ASR for leukaemia in females from 2001 to 2008; however, the incidence for Tabuk was low in comparison (Alghamdi et al., 2014) suggesting a significant increase in the rate of leukaemia diagnoses in this latter region of the Kingdom.
A notable limitation to this report is the age distribution that was used for standardising the incidence data. Use of the world standard allows for comparisons between different countries; however, it may distort the actual situation. A further issue when making comparisons with other countries is the use of projections by the IARC for estimating cancer incidence in 2012. Such practice relies on the accuracy of trends over a relatively short period of time. As we have seen in our data, fluctuations in incidence were common.
In conclusion, although the incidence of cancer in Saudi Arabia is lower than that of many other countries, as well as the overall global population, it has risen significantly over the last two decades. The most commonly diagnosed cancers were those for which screening programmes are already in place; however, use of such facilities appears to be inadequate. Improving the use of such tests could greatly reduce the morbidity and mortality associated with cancer by enabling earlier diagnosis and initiation of treatment. While individual types of cancer have their own risk factors, there are a number that are common to many different forms. These include a poor diet, a sedentary lifestyle, and obesity, all of which are increasing in prevalence in Saudi Arabia (Al-Hazzaa et al., 2011; Ng et al., 2011). Initiatives to educate people on these risks, as well as the provision of support for making the necessary lifestyle changes, could have a significant impact on cancer incidence.
Supplementary Table 1.
ICD-10 Codes Used in the Present Analysis
| Site | Codes |
|---|---|
| Stomach | C16 |
| Colorectal | C18–20 |
| Liver | C22 |
| Lung | C33–34 |
| Breast | C50 |
| Cervix uteri | C53 |
| Corpus uteri | C54 |
| Ovary | C56 |
| Prostate | C61 |
| Kidney | C64 |
| Bladder | C67 |
| Thyroid | C73 |
| Hodgkin disease | C81 |
| Non-Hodgkin lymphoma | C82–85; C96 |
| Leukaemia | C91–95 |
Supplementary Table 2.
Standard World Age Distribution Used for Calculating ASR
| Site | Codes |
|---|---|
| Stomach | C16 |
| Colorectal | C18–20 |
| Liver | C22 |
| Lung | C33–34 |
| Breast | C50 |
| Cervix uteri | C53 |
| Corpus uteri | C54 |
| Ovary | C56 |
| Prostate | C61 |
| Kidney | C64 |
| Bladder | C67 |
| Thyroid | C73 |
| Hodgkin disease | C81 |
| Non-Hodgkin lymphoma | C82–85; C96 |
| Leukaemia | C91–95 |
Legend: From (Doll et al., 1966)
References
- Abdelhadi MS. Breast cancer awareness campaign:will it make a difference? J Family Community Med. 2006;13:115–8. [PMC free article] [PubMed] [Google Scholar]
- Abdo AA, Sanai FM. Viral hepatitis in Saudi Arabia. An unfinished story. Saudi Med J. 2015;36:785–6. doi: 10.15537/smj.2015.7.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Ahmadi K, Al-Zahrani A. NO(2) and cancer incidence in Saudi Arabia. Int J Environ Res Public Health. 2013;10:5844–62. doi: 10.3390/ijerph10115844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Faleh FZ, Ayoola EA, Al-Jeffry M, et al. Integration of hepatitis B vaccine into the expanded program on immunization:The Saudi Arabian experience. Ann Saudi Med. 1993;13:231–6. doi: 10.5144/0256-4947.1993.231. [DOI] [PubMed] [Google Scholar]
- Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, et al. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. Int J Behav Nutr Phys Act. 2011;8:140. doi: 10.1186/1479-5868-8-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Zalabani AH, Alharbi KD, Fallatah NI, et al. Breast cancer knowledge and screening practice and barriers among women in Madinah, Saudi Arabia. J Cancer Educ. 2016 doi: 10.1007/s13187-016-1057-7. DOI 10.1007/s13187-016-1057-7. [DOI] [PubMed] [Google Scholar]
- Alghamdi IG, Hussain II, Alghamdi MS, et al. The incidence rate of thyroid cancer among women in Saudi Arabia:an observational descriptive epidemiological analysis of data from Saudi Cancer Registry 2001-2008. J Immigr Minor Health. 2015;17:638–43. doi: 10.1007/s10903-014-0044-5. [DOI] [PubMed] [Google Scholar]
- Alghamdi IG, Hussain II, Alghamdi MS, et al. The incidence of leukemia in Saudi Arabia. Descriptive epidemiological analysis of data from the Saudi Cancer Registry 2001-2008. Saudi Med J. 2014;35:674–83. [PubMed] [Google Scholar]
- Almadi MA, Mosli MH, Bohlega MS, et al. Effect of public knowledge, attitudes, and behavior on willingness to undergo colorectal cancer screening using the health belief model. Saudi J Gastroenterol. 2015;21:71–7. doi: 10.4103/1319-3767.153814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R, Payne P, Waterhouse JAH. Cancer Incidence in Five Continents. I. Berlin: Spinger; 1966. [Google Scholar]
- El Bcheraoui C, Basulaiman M, Wilson S, et al. Breast cancer screening in Saudi Arabia:free but almost no takers. PLoS One. 2015;10:0119051. doi: 10.1371/journal.pone.0119051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewitson P, Glasziou P, Watson E, et al. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult):an update. Am J Gastroenterol. 2008;103:1541–9. doi: 10.1111/j.1572-0241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- Hussain F, Iqbal S, Mehmood A, et al. Incidence of thyroid cancer in the Kingdom of Saudi Arabia 2000-2010. Hematol Oncol Stem Cell Ther. 2013;6:58–64. doi: 10.1016/j.hemonc.2013.05.004. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. GLOBOCAN Estimated Cancer Incidence, Mortality and Prevalence Worldwide (Europe;male) [Online] 2012a. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=62968&title=Europe&sex=1&type=0&stat=0&window=1&sort=0&submit=%C2%A0Execute .
- http://globocan.iarc.fr/Data/GLOBOCAN_AT_46842601.txt .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Iraq;female) [Online] 2012b. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=92368&title=Iraq&sex=2&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Iraq;male) [Online] 2012c. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=92368&title=Iraq&sex=1&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Jordan;female) [Online] 2012d. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=98400&title=Jordan&sex=2&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Jordan;male) [Online] 2012e. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=98400&title=Jordan&sex=1&type=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Kuwait;female) [Online] 2012f. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=103414&title=Kuwait&sex=2&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (World;female) [Online] 2012g. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=224900&title=World&sex=2&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (World;male) [Online] 2012h. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=224900&title=World&sex=1&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Yemen;female) [Online] 2012i. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=225887&title=Yemen&sex=2&type=0&stat=0 .
- International Agency for Research on Cancer. GLOBOCAN estimated cancer incidence, mortality and prevalence worldwide (Yemen;male) [Online] 2012. Available: http://globocan.iarc.fr/old/age-specific_table_r.asp?selection=225887&title=Yemen&sex=1&type=0&stat=0 .
- Midhet FM, Sharaf FK. Impact of health education on lifestyles in central Saudi Arabia. Saudi Med J. 2011;32:71–6. [PubMed] [Google Scholar]
- Mohagheghi MA, Mosavi-Jarrahi A, Malekzadeh R, et al. Cancer incidence in Tehran metropolis:the first report from the Tehran population-based cancer registry 1998-2001. Arch Iran Med. 2009;12:15–23. [PubMed] [Google Scholar]
- Nelson HD, Fu R, Cantor A, et al. Effectiveness of breast cancer screening:Systematic review and meta-analysis to update the 2009 U.S. preventive services task force recommendation. Ann Intern Med. 2016;164:244–55. doi: 10.7326/M15-0969. [DOI] [PubMed] [Google Scholar]
- Ng SW, Zaghloul S, Ali HI, et al. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Gulf states. Obes Rev. 2011;12:1–13. doi: 10.1111/j.1467-789X.2010.00750.x. [DOI] [PubMed] [Google Scholar]
- Radi SM. Breast cancer awareness among Saudi females in Jeddah. Asian Pac J Cancer Prev. 2013;14:4307–12. doi: 10.7314/apjcp.2013.14.7.4307. [DOI] [PubMed] [Google Scholar]
- Ravichandran K, Al-Hamdan NA, Mohamed G. Knowledge, attitude, and behavior among Saudis toward cancer preventive practice. J Family Community Med. 2011;18:135–42. doi: 10.4103/2230-8229.90013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Health. 2014;80:412–7. doi: 10.1016/j.aogh.2014.09.014. [DOI] [PubMed] [Google Scholar]


