Abstract
Symptoms of internalizing disorders (depression, anxiety, somatic, trauma) are the major risk factors for suicide. Atypical suicide risk is characterized by people with few or no symptoms of internalizing disorders.
Objective
In persons screened at intake to alcohol or other drug (AOD) treatment, this research examined whether person fit statistics would support an atypical subtype at high risk for suicide that did not present with typical depression and other internalizing disorders.
Methods
Symptom profiles of the prototypical, typical, and atypical persons, as defined using fit statistics, were tested on 7,408 persons entering AOD treatment using the Global Appraisal of Individual Needs (GAIN; Dennis, 2003).
Results
Of those with suicide symptoms, the findings were as expected with the atypical group being higher on suicide and lower on symptoms of internalizing disorders. In addition, the atypical group was similar or lower on substance problems, symptoms of externalizing disorders, and crime and violence.
Conclusions
Person fit statistics were useful in identifying persons with atypical suicide profiles and in enlightening aspects of existing theory concerning atypical suicidal ideation.
Keywords: Atypical suicide, Rasch person fit, GAIN, diagnostic profile
1. Introduction
In screening for suicide, depression is regarded as the major risk factor (Joiner et al., 2005; Marttunen et al., 1991; Goldney and Pilowsky, 1981; Cohen-Sandler et al., 1982; Vandivort and Locke, 1979) but not sufficient to cause suicidal behavior (Apter et al., 1995). Substance abuse is a strong disinhibiting factor (Blumenthal, 1988; U.S. Public Health Service, 1999; Inskip et al., 1998; U.S. Public Health Service, 1999; Kendall, 1983). In adolescents with and without substance use disorders, higher levels of conduct disorder symptoms were associated with suicide, suicidal ideation and attempts (Brent et al., 1993; Shafii et al., 1988; Shafii et al., 1985; Apter et al., 1995).
Recent reviews (Bridge et al., 2006; Joiner, Jr. et al., 2005), however, describe a second category of risk for suicide without depression. Many have speculated that for this group suicide may be associated with dysregulated impulse control whereby there was little or no aforethought, planning or warning by way of psychiatric symptomatology (Brent, 1987; Brown et al., 1991; Cairns et al., 1988; Kost-Grant, 1983; O’Donnell et al., 1996; Simon, et al., 2001; Williams et al., 1980).
Marttunen, et al. (1998) found that suicide victims without a psychiatric disorder tended to come from less disturbed families, had shown less antisocial behavior, and had less frequently utilized health care and social services. Those without a psychiatric disorder more often communicated suicidal thoughts for the first time just before the suicide and had more discipline problems. Recent psychological autopsy studies found that suicidal communication was less frequently reported and that there was less treatment of psychiatric disorders in suicide victims than in controls (Portzky et al., 2005a,b; Portzky et al., 2008). Brent et al. (1993) concluded that even suicide victims without apparent psychiatric disorder still show some evidence of psychiatric risk factors compared with community controls.
1.1. Atypical Profile
Therefore, there is recognition of a subtype of suicide risk that is usually characterized by no/low depression, but the rest of the profile lacks empirical validation. Research designed to characterize this subgroup is sparse, sometimes contradictory, and not yet integrated into most theoretical work on the subject. Additionally, current screening methods are unable to conveniently make the distinction between typical persons with suicidal ideation (i.e., with depression) and atypical (i.e., without depression). The efficient identification of persons at risk for suicide with atypical profiles could broaden our screening criteria and increase the likelihood of identifying this at-risk group in a timely way (Frankenfield et al., 2000). Clarification of the symptom profiles for this atypical group may also provide empirical evidence to support or refute clinical reports and theory about this atypical subtype.
1.2. Suicide and Person Fit Statistics
Clearly, persons in the atypical profile would not fit the typical clinical pattern of persons whose suicide is associated with depression. Using the item response theory (IRT) psychometric technique of person fit statistics, it has been possible to interpret responses that do not fit expected patterns (Wright, 1979). In educational situations, person fit statistics have been used to reveal unusual patterns caused by: cheating, guessing, misscoring, boredom or inattention (Meijer, 2003).
Another potential application, which has been studied very little, is using IRT to identify persons with distinct, unexpected psychiatric response patterns. In this study, we used fit statistics to clarify atypical patterns in persons with suicidal ideation. The Internal Mental Distress Scale (IMDS) of the Global Appraisal of Individual Need (GAIN; Dennis et al., 2003; Conrad et al., 2009c) was used to define atypicals since the IMDS contains the internalizing disorders involved in theorizing about atypical suicide.
1.2.1. The Concept of Person Fit
Item response theory expects endorsement of items of increasing severity to be associated with increased pathology. The single parameter IRT or Rasch model has been characterized as follows with a pattern of 1’s and 0’s along a line indicating a person’s level on the construct, e.g., psychological distress, where a “1” refers to endorsement, agreement, or being correct whereas “0” refers to lack of endorsement, disagreement, or being incorrect.
![]()
The line of 1’s above indicates items that are common or easy, i.e., low severity, for the person to endorse, while the line of 0’s indicates items that are rarer or harder to endorse, i.e., high severity, that do not apply to the person. The zone of uncertainty, where 0’s and 1’s are equally probable, indicates the person’s level on the construct.
For example, in the assessment of depression, an item such as “thought about committing suicide,” represented by the enlarged and bolded 1 below, is typically a high severity item that may be endorsed by people who have already endorsed preceding, less severe depression symptoms such as “feeling depressed,” “loss of interest,” and “being afraid to go to sleep.”
![]()
The profile above would be typical of a person with depression and other indicators of psychological distress leading up to endorsement of items indicating suicide risk. A person with this pattern would score high on the measure because it would have so many 1’s. Since this conforms to expectations, the fit statistic value would be around 1.0
Conversely, a misfitting response pattern, such as that in the profile below, would be one where a person did not endorse less severe symptoms such as depression, loss of interest, and changes in sleep (indicated by zeroes at the less severe end), but did, unexpectedly, endorse high severity symptoms such as “thought about committing suicide,” (again, the bolded 1) and other suicidal ideation (the other items at the more severe end).
![]()
Therefore, the atypical pattern above is interpreted as a person at high risk for suicide, but who does not fit the profile expected both by theory and by the Rasch model. This pattern would be flagged as highly unexpected or misfitting with a fit statistic above 1.33 (Wilson, 2005). A person with this pattern would score low with only two items endorsed, like someone with mild depression, on the overall measure even though they endorsed two high severity suicide items.
The most typical or “prototypical” persons would fit the model “too well” or have an unexpectedly perfect pattern with consecutive 1’s followed by consecutive 0’s. Since many of these will occur by chance in large samples, we regarded them as useful clinical models rather than as “fitting-too-well.”
1.2.2. Using Fit Statistics to Understand Psychiatric Behavior
As Meijer noted, “few studies illustrate systematically the use of these person fit statistics as a diagnostic tool” (p. 73, Meijer, 2003). Some research has used this strategy to examine construct applicability (Baumeister & Tice, 1988; Tellegen, 1988), personality trait structures (Reise & Waller, 1993), aberrant scores on MMPI scales (Birenbaum, 1986), “faking” on a personality test (Zickar & Drasgow, 1996), response distortion on personality scales during employee selection (Zickar & Robie, 1999), relationships between test-taking motivation and conscientiousness (Schmitt et al., 1999). A notable recent psychological example involved self-perception in a sample of 611 children. Combined information from person-fit indexes and from observation, interviews, and self-concept theory showed that similar score profiles may have different interpretations depending on the patterns (Meijer et al., 2008).
1.2.3. Statistics
Researchers have proposed several classes of person fit statistics to assess conformability of person responses to model assumptions (Meijer & Sijtsma, 2001; Levine & Rubin, 1979; Hulin et al., 1983; Reise & Flannery, 1996; Meijer, 2003) using 2 or 3 parameter IRT models. A residual-based approach developed in the Rasch model examines differences between responses and model expectations. A review showed that “sound person fit methods have been derived for the Rasch model . . . . “ (Meijer & Sijtsma, 2001, p. 129; Junker, 2001). We were most interested in the outlying or atypical persons. Therefore, the outfit statistics, i.e., the mean square (MNSQ) standardized response residuals with an expected value of 1.0, were used for persons since they are outlier sensitive (Wright and Stone, 1979; Wright and Masters, 1982).
2. Methods
2.1. Data Source
Data on 7,408 adolescents and adults (1,193 persons with suicidal ideation) were pooled from 77 substance abuse treatment studies. All data were collected during intake/screening using the GAIN (described below) as part of clinical practice or specific research studies under their respective voluntary consent procedures with identifiers subsequently encrypted before making the data available for analysis under the supervision of Chestnut’s Institutional Review Boards.
2.2. Participant Characteristics
Participants were screened at entry to alcohol or other drug (AOD) treatment with 67% male, 45% white, and 73% under age 18 (mean=19.9, s.d.=8.9). In the past year, 86% had substance disorders (e.g., abuse, dependence), 51% had internalizing disorders (e.g., somatic, depression, anxiety, trauma, suicide), 59% had externalizing disorders (ADHD, conduct disorders), and 59% had problems with crime or violence. Approximately 42% were entering residential treatment and 66% were involved in the criminal justice system. Table 1 gives the demographics by whether they self reported any suicidal ideation with every difference being significant at p<.001.
Table 1.
Sample Characteristics
| Without Suicidal Ideation (n=6,163) | With Suicidal Ideation (n=1,193) | Total (n=7,356) | |
|---|---|---|---|
| Male | 70.8% | 48.8% | 67.2% |
| Caucasian | 43.8% | 53.9% | 45.4% |
| African American | 27.5% | 17.6% | 25.9% |
| Hispanic | 11.4% | 8.3% | 10.9% |
| Mixed/Other | 17.4% | 20.2% | 17.8% |
| Under age 18 | 73.3% | 67.6% | 72.6% |
| Average Age | 19.7 | 20.9 | 19.9 |
| Any Substance Disorder | 84.8% | 93.4% | 86.2% |
| Any Internalizing Disorder | 41.2% | 99.6% | 50.6% |
| Any Externalizing Disorder | 54.7% | 82.4% | 59.2% |
| Any Crime/Violence | 56.1% | 71.1% | 58.6% |
| Residential Tx | 39.3% | 53.3% | 41.6% |
| Current legal involvement. | 67.3% | 60.3% | 66.1% |
Note: All differences were significant, p<.001
2.3. Measures
The GAIN is a comprehensive, biospychosocial, client self-report via interview (Dennis et al., 2003) with eight main sections (background, substance use, physical health, risk behaviors, mental health, environment, legal, and vocational). We examined 123 past-year yes/no questions from the GAIN’s General Individual Severity Scale (GISS), which has an alpha of .97 in both adolescents and adults. Confirmatory factor analysis shows (CFI=.92 and RMSEA=.06) that in addition to the second order factor or total score represented by GISS, responses can be represented by four main dimensions of variation: internalizing disorder symptoms, substance disorder symptoms, externalizing disorder symptoms, and crime/violence problems (Dennis et al., 2006).
2.3.1. Measures Used to Define Prototypical, Typical, and Atypical
The Internal Mental Distress Scale (IMDS) consists of 43 past year yes/no questions (alpha=.94) related to internalizing disorders (Conrad et al., 2009c). The IMDS subscales are (with number of questions and Cronbach’s alphas): Homicidal/Suicidal Thoughts (5 questions, .83), Depressive Symptoms (9 questions, .77), Anxiety/Fear Symptoms (12 questions, .77), Traumatic Stress (13 questions, .92), Somatic Symptoms (4 questions, .69). The suicide items, i.e., a homicide question was dropped, that are the focus of this paper are listed below in the order found in the GAIN:
Thought about ending your life or committing suicide?
Had a plan to commit suicide?
Gotten a gun, pills or other things to carry out your plan?
Attempted to commit suicide?
We note that, if a subject said no to the item, “thought,” the other three suicide items were not asked. This was because, in prior studies of the GAIN, less than 1% of persons endorsed the more severe suicide items without endorsing “suicidal thoughts” (Dennis et al., 2007).
2.3.2. Other GISS Measures Used in Validation
The Substance Problem Scale (SPS) consists of 16 past year yes/no questions (alpha=.90) related to any alcohol or drug use disorders, including abuse, dependence, substance induced health and psychiatric problems (Chan et al., 2008; Conrad et al., 2009b), based on DSM-IV-TR (American Psychological Association, 2000).
The Behavioral Complexity Scale (BCS) consists of 33 past year yes/no questions (alpha=.91) related to externalizing disorders (Chan et al., 2008; Conrad et al., 2009d), including attention deficit, hyperactivity, impulsivity, and conduct disorder. Some items are typical of rash, spontaneous impulsiveness (Dawe and Loxton, 2004; Barrett and Patton, 1983).
The Crime and Violence Scale (CVS; alpha=.90) consists of 12 past year yes/no questions (Conrad et al., 2009a) related to increasingly violent strategies used for resolving interpersonal conflict (Strauss, 1990) in the past year and 19 drug related, property or interpersonal/violent crimes from the Federal Bureau of Investigation (1993).
2.4. Hypotheses
The objective of this study was to determine whether person fit statistics could be used to identify people with suicidal ideation with atypical symptom patterns vs. typical and prototypical patterns. Theoretical and Rasch model expectations defined “atypical” as persons that endorsed symptoms of suicidal ideation but did not endorse the less severe symptoms leading up to these using the Internal Mental Distress Scales. “Typical” were those persons with suicidal ideation that had symptoms of suicidal ideation and many symptoms leading up to these. “Prototypical” were those persons with suicidal ideation that had most or all of the symptoms leading up to suicidal ideation.
Specifically, the study addressed the following pattern of hypotheses: In persons with suicidal ideation, do the three response profiles identified using person fit statistics (atypical vs. typical vs. prototypical) evidence the hypothesized pattern of symptom levels presented in Table 2? We summarize the hypotheses in Table 2 as follows:
Table 2.
Persons with at Least One Suicide Symptom (N=1193): Expected Patterns of Symptom Levels on Variables of Interest Depending on Outfit Group Status.
| Outfit Groups | Results | ||||
|---|---|---|---|---|---|
| Hypothesized Ranking on Each Variable | Unadjusted | Adjusted | |||
|
| |||||
| Variables | Prototypical <.75 outfit MNSQ |
Typical .75 – 1.33 |
Atypical >1.33 outfit MNSQ |
See Fig 2 & Model 1 in Table 4 | See Table 4 Models 2 & 3 |
|
| |||||
| Suicide | High | High | High | Atypical highest | Atypical highest |
|
| |||||
| Depression | Highest | Medium | Lowest | As expected | As expected |
|
| |||||
| Somatic | Highest | Medium | Lowest | As expected | As expected |
|
| |||||
| Anxiety | Highest | Medium | Lowest | As expected | N.S. |
|
| |||||
| Trauma | Highest | Medium | Lowest | As expected | N.S. |
|
| |||||
| Substance Problems (SPS) | Similar | Similar | Similar | Atypical lower | Prototypical higher on Model 2 |
|
| |||||
| Externalizing Disorders (BCS), e.g., inattentive, impulsive | Similar | Similar | Similar | Atypical lower than Proto-typical | Atypical lower than Proto on Models 2& 3 |
|
| |||||
| Crime & Violence (CVS) | Similar | Similar | Similar | As expected | Atypical lower than Typical on Model 2 |
On the Suicide scale all three groups would score similarly, i.e., having high levels of suicide.
On Internalizing Disorders (IMDS) of Depression, Anxiety, Somatic, and Trauma, the three groups would be gradated with prototypical having highest levels, followed by typical, and atypical.
On the Substance Problem Scale (SPS), Behavior Complexity Scale (BCS) and Crime and Violence Scale (CVS), the three groups would score similarly. This was a test of the null hypothesis, i.e., no differences among groups, since the theory and evidence did not provide directional hypotheses.
Subsequent to the person fit analysis, logistic regression analyses were performed as a test of the sensitivity of the results to other factors such as age and gender.
2.5. Data Collection
All interviews were conducted by interviewers with 3 to 4 days of training followed by rigorous field-based certification procedures and ongoing supervision.
2.6. Analyses
2.6.1. Rasch Dichotomous Model
All GISS scales were analyzed with a Rasch dichotomous model (Rasch, 1960; Wright & Stone, 1979) with WINSTEPS statistical software (Linacre, 2007). The model estimates the probability that a respondent will choose a particular response category for an item as:
where Pni is the probability of respondent n endorsing item i, Pni+1 is the probability of respondent n not endorsing item i, Bn is the person measure of respondent n, Di is the difficulty of item i.
The Rasch MNSQ outfit statistic was used to quantify the degree to which a person’s response pattern was “atypical” given their overall score. Participants were then grouped into three levels called “outfit groups” using Wilson’s rule of thumb (Wilson, 2005): Atypical (outfit MNSQ above 1.33), typical (outfit from .75 to 1.33), and prototypical (outfit below .75). While our interest was primarily in the atypical group, we distinguished between the typical and prototypical subgroups to see if differences would be observed at one level but not at the other.
2.6.2. Power and Clinical Significance
Again, since the sample size was very large, even small group effects would be shown to be statistically significant. Therefore, to be conservative, we required clinical significance as well using the rule of thumb of half a standard deviation in analyses without statistical adjustments as a significant effect size in examining group differences (Norman et al., 2003).
2.6.3. Graphic, Descriptive and Regression Models
To provide perspective, the group with suicidal ideation was compared descriptively to the group with no suicidal ideation. Output was provided graphically whereby visual examination would reveal whether a difference of half a standard deviation were present. All items were anchored to the same measurement scale with the calibrations derived from the full analysis of the 123 GISS items. Since all items and subscales were calibrated on the same overarching scale, they could be compared to each other. For the principal analyses designed to explain atypical-typical-prototypical response patterns, only subjects that endorsed at least one suicide item were included. Descriptive statistics were provided in Table 3 to obtain more detail about the nature of the three outfit groups. In addition to the graphs, the bivariate relationships between each of the variables of interest and outfit group status were examined through a series of logistic regressions to provide statistics and significance (model 1 in Table 4).
Table 3.
Bivariate Analyses With Outfit Groups a In The Subset With Suicidal Ideation
| Variable | Outfit Group
|
Mean/Total % | ||
|---|---|---|---|---|
| Prototypical N=176 |
Typical N=546 |
Atypical N=471 |
||
| Mean Age (SD)** | 24.59 (11.47) | 20.49 (8.92) | 19.90 (9.40) | 20.86 (9.65) |
| Gender | ||||
| Males | 42.6% | 51.1% | 48.4% | 48.8% |
| Females | 57.4% | 48.9% | 51.6% | 51.2% |
| Ethnicity* | ||||
| African-American | 22.2% | 16.3% | 17.4% | 17.6% |
| Caucasian | 55.1% | 57.5% | 49.1% | 53.9% |
| Hispanic | 8.0% | 7.0% | 10.1% | 8.3% |
| Mixed/Other | 14.8% | 19.2% | 23.4% | 20.2% |
| Employed* | 42.9% | 40.9% | 33.4% | 38.2% |
| Substance Use Disorder (present vs. absent)* | 97.1% | 94.0% | 91.2% | 93.4% |
| Internalizing Disorder (present vs. absent) | 100% | 99.6% | 99.4% | 99.6% |
| Externalizing Disorder (present vs. absent)** | 94.3% | 85.9% | 73.9% | 82.4% |
| Crime/Violence (present vs. absent) | 68.1% | 71.4% | 71.9% | 71.1% |
| Residential Treatment** | 62.1% | 48.7% | 55.3% | 53.3% |
| Diagnosed w. Mental Disorder | 100.0% | 98.2% | 94.3% | 96.9% |
| Cur. Crim. Just. Involvement | 55.7% | 60.3% | 62.0% | 60.3% |
| Fam. Hist. Psychological Prob. | 70.2% | 62.6% | 60.6% | 63.0% |
| Fam. Hist. Drug Use | 70.2% | 72.0% | 74.3% | 72.6% |
|
| ||||
| Past Yr Suicide Any Symptoms | 100.0% | 100.0% | 100.0% | 100.0% |
| Suicidal Thoughts | 100.0% | 100.0% | 99.8% | 99.9% |
| Got gun to carry out plan** | 17.0% | 21.1% | 53.5% | 33.3% |
| Had a plan to commit suicide** | 23.9% | 28.0% | 68.8% | 43.5% |
| Attempted Suicide** | 19.9% | 25.5% | 61.8% | 39.0% |
| Past Yr Depression | ||||
| Feeling Tired/No Energya** | 100.0% | 79.0% | 55.0% | 71.0% |
| Moving/Talking Slowerb** | 59.2% | 33.7% | 27.0% | 33.6% |
| No Energy/Losing Interest in Friends/Workc** | 98.1% | 72.6% | 61.4% | 73.6% |
Note:
Based on a total number of cases = 662
Total number of cases = 561
Total number of cases = 531
p<.05,
p<.01
Table 4.
Logistic regression analyses comparing outfit groupsa in the subset with suicidal ideation
| Unadjusted, Model 1 Estimates (confidence intervals) |
Full, Model 2 c Estimates (confidence intervals) |
Sensitivity, Model 3 d Estimates (confidence intervals) |
||||
|---|---|---|---|---|---|---|
| Variables b | Atypical vs. Prototypical | Atypical vs. Typical | Atypical vs. Prototypical | Atypical vs. Typical | Atypical vs. Prototypical | Atypical vs. Typical |
| Suicide | 2.362 (2.006–2.783) | 1.936 (1.756–2.133) | 4.801 (3.373–6.835) | 3.348 (2.863–3.916) | None | None |
| Depression | 0.181 (0.136–0.240) | 0.605 (0.549–0.668) | 0.129 (0.080–0.209) | 0.377 (0.314–0.453) | 0.209 (0.149–0.293) | 0.598 (0.525–0.682) |
| Somatic | 0.437 (0.378–0.504) | 0.773 (0.717–0.834) | 0.462 (0.333–0.640) | 0.769 (0.678–0.871) | 0.600 (0.483–0.744) | 0.866 (0.786–0.955) |
| Anxiety | 0.492 (0.428–0.565) | 0.782 (0.722–0.847) | 1.066 (0.775–1.467) | 1.099 (0.950–1.271) | 0.944 (0.751–1.187) | 1.068 (0.950–1.202) |
| Trauma | 0.724 (0.667–0.785) | 0.913 (0.867–0.960) | 1.075 (0.888–1.300) | 0.961 (0.884–1.046) | 1.096 (0.961–1.251) | 1.020 (0.954–1.090) |
| Substance Problem Scale | 0.670 (0.599–0.749) | 0.881 (0.827–0.940) | 1.275 (1.023–1.589) | 1.038 (0.936–1.150) | 1.012 (0.862–1.188) | 0.992 (0.915–1.077) |
| Behavioral Complexity Scale | 0.680 (0.603–0.768) | 0.859 (0.807–0.915) | 0.627 (0.485–0.810) | 0.929 (0.837–1.030) | 0.794 (0.658–0.956) | 0.923 (0.847–1.005) |
| Crime/Violence | 0.902 (0.821–0.991) | 0.940 (0.881–1.003) | 1.013 (0.796–1.288) | 0.880 (0.785–0.988) | 1.046 (0.880–1.243) | 0.987 (0.901–1.082) |
| Gender e | 0.791 (0.558–1.122) | 1.114 (0.870–1.425) | 0.696 (0.329–1.474) | 1.001 (0.702–1.427) | 1.126 (0.656–1.931) | 1.381 (1.042–1.830) |
| Racef | 0.739 (0.481–1.135) | 1.080 (0.776–1.503) | 1.849 (0.677–5.050) | 1.607 (0.995–2.595) | 1.727 (0.825–3.615) | 1.378 (0.924–2.053) |
| Ageg | 0.338 (0.236–0.484) | 0.756 (0.575–0.993) | 0.965 (0.370–2.512) | 1.289 (0.809–2.053) | 0.823 (0.415–1.632) | 0.931 (0.641–1.352) |
| History of victimization | 0.385 (0.212–0.697) | 0.787 (0.565–1.096) | 2.152 (0.635–7.296) | 1.476 (0.897–2.429) | 2.631 (1.036–6.679) | 1.338 (0.900–1.990) |
| Past Year Mental Health Treatment Received | 1.445 (1.018–2.050) | 1.271 (0.990–1.633) | 1.845 (0.866–3.928) | 0.967 (0.676–1.382) | 1.950 (1.118–3.402) | 1.593 (1.198–2.118) |
| Past Year Substance Abuse Treatment Received | 0.768 (0.541–1.090) | 0.987 (0.768–1.269) | 0.612 (0.283–1.324) | 1.045 (0.727–1.503) | 0.751 (0.429–1.316) | 0.990 (0.739–1.326) |
Outfits: most typical < .75, typical .75–1.33, atypical = > 1.33
Bold are p<.05. Significance is indicated if the confidence interval (in parentheses) does not include 1.0. Above 1.0 means atypical is higher; below 1.0 means atypical is lower.
N of cases = 1193
Model 2 was adjusted for all variables
Model 3 was adjusted for all variables, except suicide
Female (=1), Male (=0)
African American (=1), Non-African American (=0)
Age>=18 (=1), Age<18 (=0)
The variables, suicide, depression, anxiety, trauma, somatic, substance problems, behavioral complexity, crime/violence, gender, race, age, history of victimization, past year mental health treatment received, past year substance abuse treatment received, were subsequently entered into a full multivariate, binomial logistic regression analysis (model 2, in Table 4), i.e., atypical vs. typical, then atypical vs. prototypical. This tested whether controlling/adjusting for factors, such as age and gender, would affect the results. As a sensitivity analysis, the suicide scale of the IMDS was dropped, and all of the previous variables were reentered (model 3 in Table 4) to examine whether, if we did not control statistically for the variation in suicidal ideation, the results would change.
3. Results
3.1. Rasch Analysis of GAIN Scales
IMDS item calibrations (n = 43) and person measures (n = 7,408) were estimated with a small proportion of missing data. Specifically, 98.6 percent answered at least 37 items. Results supported the theoretical construct with high person reliability (analogous to Cronbach’s alpha except that extreme scores were excluded) at .89, alpha=.94, and unidimensionality with no item fit statistics outside reasonable bounds. The person standard deviation was 1.58 logits. Therefore, the half standard deviation criterion for clinical significance was .8 logit. All GISS scales were found to be of good conformance to the model (Conrad et al., 2009a,b,c,d; Conrad et al., 2007; Riley et al., 2007).
3.2. Examples of Typical and Atypical Cases
To illustrate, we provide two cases below as in section 1.2.1. The four suicidal items are bolded both in numbers and words below:
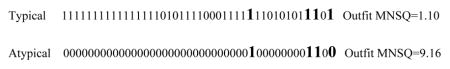
ThoughtsCommittingSuicide, PlanToCommitSuicide, AttemptedSuicide, GotGunEtcToCarryOut
The Typical case endorsed most symptoms of depression, anxiety, somatic, and trauma leading up to endorsement of the suicide symptoms. In the Atypical case, the only items endorsed were three of the four suicidal items.
3.3. Full Sample on Suicide vs. No Suicide Items Endorsed
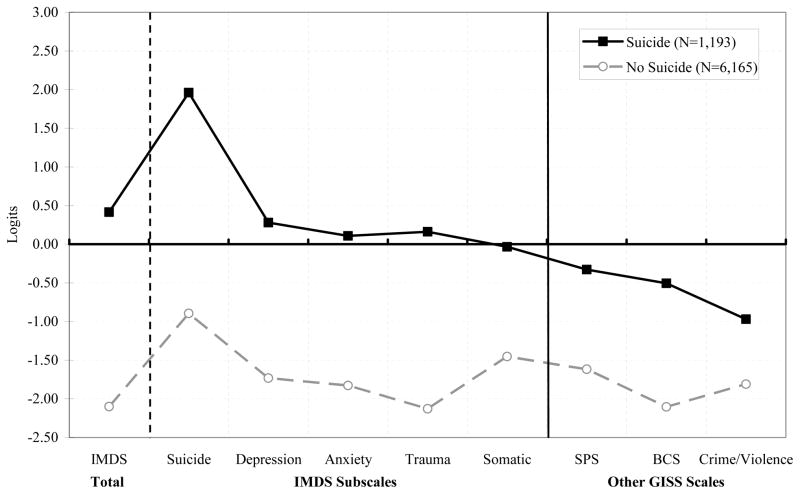
In Figure 1, we compared the group of persons that endorsed at least one suicide item (n=1,193) with the group endorsing no suicide items (n=6,165). The total IMDS, on the left, is followed by its five subscales, followed by other GISS scales as potential alternative explanations for suicidality. The suicide risk group was significantly higher on the total IMDS as well as each of the IMDS subscales related to depression, somatic, anxiety, and trauma. Additionally, the suicide group was higher on substance problems and behavioral complexity which assessed externalizing disorders including inattentive, hyperactivity and impulsiveness, and conduct disorders. It was not higher on crime and violence where it was about equal to the no suicide group. As was expected, persons with suicidal ideation tended to be equal or significantly higher on all types of symptomatology.
Figure 1.
Comparison of Suicide Group vs. No Suicide Group on GISS Scales
3.4. Suicide Subset
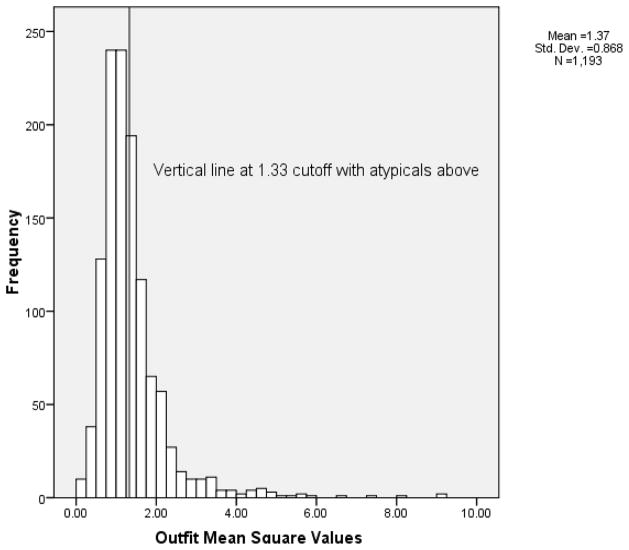
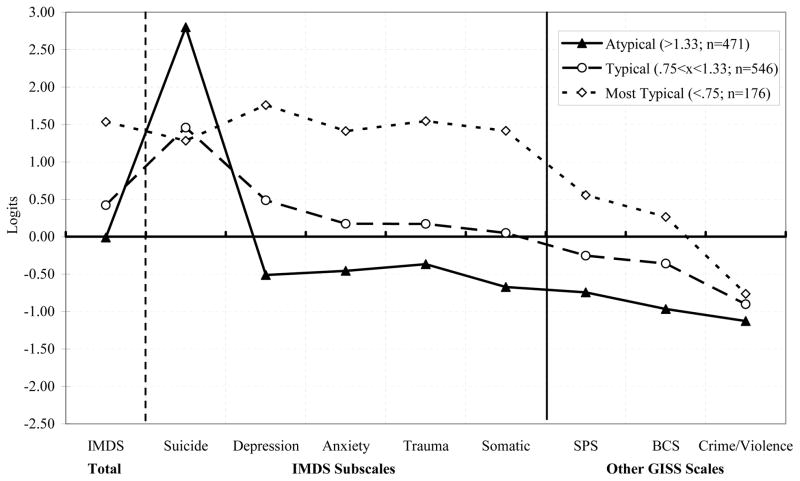
Next we tested the study hypotheses (Table 2) on the same variables for only those persons that endorsed at least one of the four suicide items, n=1,193. Figure 2 displays the outfit mean square values for persons with suicidal ideation whereby the atypical group (n=471, just under 40%) was defined as those above the 1.33 cutoff indicating high outfit mean square. In Figure 3, this atypical group was significantly higher than the other groups on suicide symptoms endorsed and significantly lower than the typical and prototypical groups on the total IMDS and the depression, somatic, anxiety, and trauma subscales. The atypical group was lower than the prototypical group on the Substance Problems Scale (SPS), but only in the unadjusted model that is presented in Figure 2 (Table 4, Model 1 contains corresponding confidence intervals and statistical significance for Figure 2). The direction on Substance Problems switched in the adjusted models, and all but one comparison was non-significant. The atypical group was lower than the prototypical group on Externalizing Disorders (BCS) in both unadjusted and adjusted models. Moreover there was no significant difference between the atypical and prototypical outfit groups on the Crime and Violence Scale.
Figure 2.
Outfit Mean Square Values for Persons with Suicidal Ideation; Atypicals Were Above 1.33 Cutoff
Figure 3.
Comparison of Atypical, Typical and Prototypical Groups for Suicide Subset
3.5. Correlates of Outfit Groups
In Table 3, no variables had as strong relationships with outfit groups as the individual suicide and depression symptoms. Therefore, the IMDS symptoms appeared be accounting for the typical vs. atypical distinction. The examination of the individual symptoms of suicide and depression reinforced the finding that the atypical profile was endorsing more serious suicide symptoms than the typical and prototypical. The symptom, “Had a plan to commit suicide,” was endorsed by 69% of the atypical group, 28% of the typical group, and 24% of the prototypical group. “Attempted suicide” was endorsed by 62% of the atypical group, 26% of the typical group, and 20% of the prototypical group.
3.6. Regression Analyses
Table 4 presents the results of three logistic regression models in pairwise comparison of the three outfit groups: atypical vs. typical, and atypical vs. prototypical. In all, the typical and the prototypical groups were set to 1 as the reference group in comparison to atypical. To be significant the confidence interval (in parentheses) does not include 1.0. Above 1.0 indicates atypical is higher; below 1.0 means atypical is lower. Model 1 is the bivariate, unadjusted regression of the outfit groups on all variables (same as Figure 2). Most of these bivariate significant differences became non-significant in the Model 2 multivariate, i.e., adjusted, analyses.
In Model 2, where all variables were entered to test whether each had an independent effect while controlling for the others, the atypical group was clearly more suicidal than the other two groups. The atypical group was also less depressed and had fewer somatic complaints, and there was the suggestion that the atypical group was actually lower on Externalizing Disorders (BCS) but not on Crime and Violence. The atypical group was also higher in Substance Problems, a reversal from Model 1, but this did not hold up in Model 3. Age became non-significant when controlling for other factors. Again, it was lower depression and somatic complaints that explained the atypical. Externalizing Disorders were lower for atypicals vs. prototypicals and Crime and Violence was still about equal.
In Model 3, as a sensitivity analysis, suicide was dropped from the analysis and the significant predictors were depression and somatic where the atypical group was still significantly lower. Model 3 also indicated weak significance for history of victimization and gender. However, the suggestion that past year mental health treatment was higher for the atypical group echoes the finding in Model 1 and may merit further investigation. Variables such as age and gender were not significant when controlling for the psychological characteristics.
4. Discussion
In the full sample, persons that endorsed at least one suicide symptom corresponded with the literature suggesting that on average those with suicidal ideation tend to have greater psychiatric pathology than those without suicidal ideation. We then subset to those with any suicidal ideation to test hypotheses H1, H2, and H3. Contrary to our expectations in H1 that all three groups would be similar on the suicide subscale, the atypical group was significantly “higher” than the typical or prototypical group (2.8 vs. 1.3 vs. 1.0 logits).
Consistent with our expectations in H2, the atypical group was significantly lower than the typical or prototypical groups on the Depression scale. The pattern was the same in the univariate and multivariate (adjusted) models. Though slightly less marked, this pattern also held for the IMDS overall and its subscales (i.e., anxiety, trauma, somatic) in a univariate model. In a multivariate model, however, the results were no longer statistically significant for anxiety and trauma.
It is worth noting that this atypical group actually represented 40% of persons with at least one suicide symptom. While this percentage is partly a function of the MNSQ criterion of 1.33 used to define the group (the higher the criterion, the smaller the group would be), this pattern of symptoms and the prevalence of non-depressed people with suicide symptoms was roughly consistent with prior reports (Brent et al., 1993) and anecdotes from clinical experience. It should also be noted that even though the atypical group was lowest of the three suicidal ideation groups on internalizing disorders, the atypicals were still higher (Figure 3) than those who did not endorse any suicide symptoms (Figure 1).
As expected for H3, the three groups were similar on substance problems. The analysis failed to reject the null hypothesis that the atypical group would be similar to the typical group in Externalizing Disorders and in Crime and Violence. There was some evidence that the atypical group was lower than only the prototypical group in Externalizing Disorders in clinical significance as well as in both adjusted regression models. There was also some evidence that the atypical group was lower on Crime and Violence in one of the regression models (Model 2).
4.1. Strengths and Limitations
This was a large sample study so the findings were not likely due to chance variation. The Rasch model provided fit statistics suited to the task of identifying atypical respondents. Additionally, the GAIN scales were well grounded in DSM symptoms and psychiatric theory.
It should be noted that over half the sample was involved in the justice system, and all were presenting to a substance abuse treatment program for screening. While this is a large and important group, the limits of generalizability for these findings should be noted. Finally, we recognize that the risk factors for suicide are multiple and convergent. Many other important risk factors were not explored that could shed light on this atypical group (e.g., a recent personal crisis, personality disorder, family discord, access to a gun, etc.).
We found the atypical to be substantially higher on suicidal ideation including plans and reported attempts. This was a large proportion of misfitting persons that corresponded with a meaningful clinical syndrome. Even if these atypicals were due to transient suicidal ideation, this is still dangerous and important to detect.
Conclusions
Using a large sample, results supported the expectation that the atypical profile with suicidal ideation was indeed present and associated with relatively low depression. Persons with the atypical profile also tended to endorse more serious suicide symptoms than the typical and prototypical who endorsed any suicidal ideation. Additionally, the atypical profile was not higher on externalizing disorders such as inattentiveness, impulsivity, and conduct disorders or with substance problems or crimes and violence. Therefore, person fit statistics successfully identified persons who conform to the prevailing diagnostic pattern for atypical suicide. Perhaps most significant clinically is that the use of person fit statistics with the GAIN may be able to rapidly red-flag persons at high risk for suicide who are less likely to be identified using the usual screening methods alone (e.g., having a high score on the IMDS). It also does more than just screening for suicide risk separately because most common approaches to treating suicide risk assume the person has depression. The use of person fit statistics identifies a subgroup with atypical presentations that do not include depression and for whom depression treatments are probably inappropriate. Therefore, differentiating atypicals may help to treat high-risk individuals more rapidly and appropriately. Future research should further explore the predictive validity of person fit statistics in research on suicide as well as in other clinical applications.
Acknowledgments
This development of this paper was supported by the Center for Substance Abuse Treatment (CSAT), Substance Abuse and Mental Health Services Administration (SAMHSA) contract 270-2007-0191 using data provided by the following grants and contracts from CSAT (TI11320, TI11324, TI11317, TI11321, TI11323, TI11874, TI11424, TI11894, TI11871, TI11433, TI11423, TI11432, TI11422, TI11892, TI11888, TI013313, TI013309, TI013344, TI013354, TI013356, TI013305, TI013340, TI130022, TI03345, TI012208, TI013323, TI14376, TI14261, TI14189,TI14252, TI14315, TI14283, TI14267, TI14188, TI14103, TI14272, TI14090, TI14271, TI14355, TI14196, TI14214, TI14254, TI14311, TI15678, TI15670, TI15486, TI15511, TI15433, TI15479, TI15682, TI15483, TI15674, TI15467, TI15686, TI15481, TI15461, TI15475, TI15413, TI15562, TI15514, TI15672, TI15478, TI15447, TI15545, TI15671, TI11320, TI12541, TI00567; Contract 207-98-7047, Contract 277-00-6500, 270-2003-0006 the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (R01 AA 10368), the National Institute on Drug Abuse (NIDA) (R37 DA11323; R01 DA018183), the Illinois Criminal Justice Information Authority (95-DB-VX-0017), the Illinois Office of Alcoholism and Substance Abuse (PI 00567), the Interventions Foundation’s Drug Outcome Monitoring Study (DOMS), and the Robert Wood Johnson Foundation’s Reclaiming Futures (45054, 45059, 45060, 45053, 47266). The authors wish to thank Rod Funk for data base and statistical support, Ling Jin for support with figure development, Karen Conrad for editorial review. The opinions are those of the authors and do not reflect official positions of the government, other funders or principal investigators of the individual studies.
Contributor Information
Kendon J. Conrad, Professor of Health Policy and Administration, University of Illinois at Chicago, School of Public Health (M/C 923), 1603 West Taylor Street, Chicago, IL 60612-4310
Nikolaus Bezruczko, Measurement and Evaluation Consulting, Chicago, IL
Ya-Fen Chan, Research Scientist, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761, USA
Barth Riley, Research Scientist, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761, USA
Guy Diamond, Associate Professor, University of Pennsylvania School of Medicine, Director, Center for Family Intervention Science, Children’s Hospital of Philadelphia, 34th and Civic Center Bl., Philadelphia, PA 19104
Michael L. Dennis, Senior Research Psychologist and GAIN Coordinating Center Director, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761, USA
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV-TR) 4. Washington, DC: American Psychiatric Association; 2000. revision ed. [Google Scholar]
- American Society of Addiction Medicine. Patient placement criteria for the treatment for substance-related disorders. 2. Chevy Chase, MD: American Society of Addiction Medicine; 2001. [Google Scholar]
- Anderson RN. Deaths: leading causes for 2000. Natl Vital Stat Rep. 2002;50(16):1–85. [PubMed] [Google Scholar]
- Apter A, Gothelf D, Orbach I, Weizman R, Ratzoni G, Hareven D, Tyano S. Correlation of suicidal and violent behavior in different diagnostic categories in hospitalized adolescent patients. J Amer Acad Child Adolesc Psychiatry. 1995;34(7):912–918. doi: 10.1097/00004583-199507000-00015. [DOI] [PubMed] [Google Scholar]
- Barratt ES, Patton JH. Impulsivity: Cognitive, behavioral, and psychophysiological correlates. In: Zuckerman M, editor. Biological bases of sensation seeking, impulsivity, and anxiety. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. pp. 77–122. [Google Scholar]
- Baumeister RF, Tice DM. Metatraits. J Personality. 1988;56:571–598. [Google Scholar]
- Birenbaum M. Comparing the effectiveness of several IRT based appropriateness measures in detecting unusual response patterns. Educ Psychol Meas. 1985;45:523–534. [Google Scholar]
- Birenbaum M. Effect of dissimulation motivation and anxiety on response pattern appropriateness measures. Applied Psychol Meas. 1986;10:167–174. [Google Scholar]
- Blumenthal SJ. Suicide: A guide to risk factors, assessment, and treatment of suicidal patients. Med Clinics North Am. 1988;72:937–971. doi: 10.1016/s0025-7125(16)30754-4. [DOI] [PubMed] [Google Scholar]
- Brent DA. Correlates of the medical lethality of suicide attempts in children and adolescents. J Amer Acad Child Adolesc Psychiatry. 1987;26:87–91. doi: 10.1097/00004583-198701000-00017. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper J, Moritz G, Baugher M, Allman C. Suicide in adolescents with no apparent psychopathology. J Amer Acad Child Adolesc Psychiatry. 1993;32:494–500. doi: 10.1097/00004583-199305000-00002. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, Schweers J, Balach L, Baugher M. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry. 1993;32(3):521–9. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Brown LK, Overholser J, Spirito A, Fritz GK. The correlates of planning in adolescent suicide attempts. J Amer Acad Child Adolesc Psychiatry. 1991:95–99. doi: 10.1097/00004583-199101000-00014. [DOI] [PubMed]
- Cairns RB, Peterson G, Neckerman HJ. Suicidal-behavior in aggressive adolescents. J Clin Child Psychol. 1988;17:298–309. [Google Scholar]
- Chan YF, Dennis ML, Funk RR. Prevalence and comorbidity co-occurrence of major internalizing and externalizing disorders among adolescents and adults presenting to substance abuse treatment. J Subst Abuse Treatment. 2008;34:13–24. doi: 10.1016/j.jsat.2006.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Sandler R, Berman AL, King RA. A follow-up study of hospitalized suicidal children. J Amer Acad Child Adolesc Psychiatry. 1982;21:398–403. doi: 10.1016/s0002-7138(09)60945-6. [DOI] [PubMed] [Google Scholar]
- Conrad KJ, Conrad KM, Dennis ML, Riley BB, Chan YF, Funk R. Validation of the Crime and Violence Scale (CVS) to the Rasch Measurement Model, GAIN Methods Report 1.1. Chicago, IL: Chestnut Health Systems; 2009a. [Accessed March 4, 2009]. Retrieved from http://www.chestnut.org/li/gain/psychometric_reports/Conrad et al 2009 CVS RaschReport.pdf. [Google Scholar]
- Conrad KJ, Conrad KM, Dennis ML, Riley BB, Funk R. Validation of the Substance Problem Scale (SPS) to the Rasch Measurement Model, GAIN Methods Report 1.1. Chicago, IL: Chestnut Health Systems; 2009b. Retrieved from http://www.chestnut.org/li/gain/psychometric_reports/Conrad et al 2009 SPS Report.pdf. [Google Scholar]
- Conrad KJ, Conrad KM, Dennis ML, Riley BB, Funk R. Validation of the Internal Mental Distress Scale (IMDS) to the Rasch Measurement Model, GAIN Methods Report 1.1. Chicago, IL: Chestnut Health Systems; 2009c. [Accessed March 4, 2009]. Retrieved from http://www.chestnut.org/li/gain/psychometric_reports/Conrad et al 2009 IMDS Rasch Report.pdf. [Google Scholar]
- Conrad KJ, Conrad KM, Dennis ML, Riley BB, Funk R. Validation of the Behavioral Complexity Scale (BCS) to the Rasch Measurement Model, GAIN Methods Report 1.1. Chicago, IL: Chestnut Health Systems; 2009d. [Accessed March 4, 2009]. Retrieved from http://www.chestnut.org/li/gain/psychometric_reports/Conrad_et_al_2009_BCS_Rasch_Report.pdf. [Google Scholar]
- Conrad KJ, Dennis ML, Bezruczko N, Funk R, Riley B. Substance Use Disorder Symptoms: Evidence of Differential Item Functioning by Age. J Appl Meas. 2007;8(4):373–387. [PMC free article] [PubMed] [Google Scholar]
- Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Behav Rev. 2004;28:343–351. doi: 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Chan YF, Funk R. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing, and substance use disorders and crime/violence problems among adolescents and adults. Am J Addictions. 2006;15:80–91. doi: 10.1080/10550490601006055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Foss M, Scott C. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 2007;31:585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Prog Plan. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs: Administration Guide for the GAIN and Related Measures. Bloomington, IL: Chestnut Health Systems; 2003. [Accessed March 6, 2008]. Retrieved from http://www.chestnut.org/li/gain. [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale--Preliminary report. Psychopharmacol Bull. 1973;9:13–28. [PubMed] [Google Scholar]
- Federal Bureau of Investigation. Uniform Crime Reports. Washington DC: 1993. [Accessed May 23, 2006]. Available at: http://www.fbi.gov/ucr. [Google Scholar]
- Frankenfield DL, Keyl PM, Gielen A, Wissow LS, Werthaner L, Baker SP. Adolescent patients -- healthy or hurting? Missed opportunities to screen for suicide risk in the primary care setting. Arch Pediatr Adolesc Med. 2000;154:162–168. doi: 10.1001/archpedi.154.2.162. [DOI] [PubMed] [Google Scholar]
- Goldney RD, Pilowsky I. Depression in young women who have attempted suicide. Aust N Z J Psychiatry. 1981;14:203–211. doi: 10.3109/00048678009159380. [DOI] [PubMed] [Google Scholar]
- Hulin CL, Drasgow F, Parsons C. Item Response Theory: Applications to psychological measurement. Homewood, IL: Dow & Jones Irwin; 1983. [Google Scholar]
- Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Brit J Psychiatry. 1998;172:35–37. doi: 10.1192/bjp.172.1.35. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Brown JS, Wingate LR. The Psychology and Neurobiology of Suicidal Behavior. Ann Rev Psychol. 2005;56:287–314. doi: 10.1146/annurev.psych.56.091103.070320. [DOI] [PubMed] [Google Scholar]
- Junker B. On the interplay between nonparametric and parametric IRT with some thoughts about the future. In: Boomsma A, van Duijn MAJ, Snijders TAB, editors. Essays on Item Response Theory. New York: Springer-Verlag; 2001. pp. 247–276. [Google Scholar]
- Kendall RE. Alcohol and suicide. Subst Alcohol Actions Misuse. 1983;4(2–3):121–7. [PubMed] [Google Scholar]
- King DW, King LA, Fairbank JA, Schlenger WE, Surface CR. Enhancing the precision of the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: An application of item response theory. Psychol Assess. 1993;5:457–471. [Google Scholar]
- Kost-Grant BL. Self-inflicted gunshot wounds among Alaska Natives. Pub Health Rep. 1983;98:72–8. [PMC free article] [PubMed] [Google Scholar]
- Levine MV, Rubins DB. Measuring the appropriateness of multiple-choice test scores. J Educ Stat. 1979;4:269–290. [Google Scholar]
- Li MF, Olejnik S. The power of Rasch person-fit statistics in detecting unusual response patterns. App Psychol Meas. 1997;21:215–231. [Google Scholar]
- Linacre JM. What do infit and outfit, mean-square and standardized mean? Rasch Meas Trans. 2002;16(2):878. [Google Scholar]
- Linacre JM. A user’s guide to WINSTEPS. Chicago: Mesa Press; 2007. [Google Scholar]
- Lipman RS, Covi L, Shapiro AK. The Hopkins Symptom Checklist (HSCL): factors derived from the HSCL-90. J Affect Disord. 1979;1:9–24. doi: 10.1016/0165-0327(79)90021-1. [DOI] [PubMed] [Google Scholar]
- Marttunen MJ, Aro HM, Henrikson MM, Lonqvist JK. Mental disorders in adolescent suicide. DSM III-R Axes I and II diagnoses in suicide among 13 to 19 year olds in Finland. Arch Gen Psychiatry. 1991;48:834–839. doi: 10.1001/archpsyc.1991.01810330058009. [DOI] [PubMed] [Google Scholar]
- Marttunen MJ, Henriksson MM, Isometsä ET, Heikkinen ME, Aro HM, Lönnqvist JK. Completed suicide among adolescents with no diagnosable psychiatric disorder. Adolescence. 1998;33(131):669–81. [PubMed] [Google Scholar]
- Meijer R. Diagnosing item score patterns on a test using item response theory-based person-fit statistics. Psychol Methods. 2003;8:72–87. doi: 10.1037/1082-989x.8.1.72. [DOI] [PubMed] [Google Scholar]
- Meijer R, Egberink I, Emons W, Sijtsma K. Detection and Validation of Unscalable Item Score Patterns Using Item Response Theory: An Illustration with Harter’s Self-Perception Profile for Children. Journal of Personality assessment. 2008;90:227–238. doi: 10.1080/00223890701884921. [DOI] [PubMed] [Google Scholar]
- Meijer R, Sijtsma K. Methodology review: Evaluating person fit. Appl Psychol Meas. 2001;25:107–135. [Google Scholar]
- Molenaar IW, Giuhtubj H. The many null distributions of person fit indices. Psychometrika. 1990;55:75–106. [Google Scholar]
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- O’Donnell I, Farmer R, Catalan J. Explaining suicide: the views of survivors of serious suicide attempts. Brit J Psychiatry. 1996;168:780–6. doi: 10.1192/bjp.168.6.780. [DOI] [PubMed] [Google Scholar]
- Portzky G, Audenaert K, van Heeringen K. Psychosocial and psychiatric factors associated with adolescent suicide: A case-control psychological autopsy study. J Adolesc. 2008 Nov 20; doi: 10.1016/j.adolescence.2008.10.007. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Portzky G, Audenaert K, van Heeringen K. Adjustment disorder and the course of the suicidal process in adolescents. J Affect Disord. 2005;87(2–3):265–70. doi: 10.1016/j.jad.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Portzky G, Audenaert K, van Heeringen K. Suicide among adolescents. A psychological autopsy study of psychiatric, psychosocial and personality-related risk factors. Soc Psychiatry Psychiatr Epidemiol. 2005;40(11):922–30. doi: 10.1007/s00127-005-0977-x. [DOI] [PubMed] [Google Scholar]
- Rasch G. Probabilistic models for some intelligence and attainment tests. Copenhagen: Danmarks Paedogogiske Institut; 1960. (Republished Chicago: The University of Chicago Press: 1980) [Google Scholar]
- Reise SP, Flannery WP. Assessing person-fit on measures of typical performance. Appl Psychol Meas. 1996;9:9–26. [Google Scholar]
- Reise SP, Waller NG. Traitedness and the assessment of response pattern scalability. J Personality Soc Psychol. 1993;65:143–151. [Google Scholar]
- Riley B, Dennis ML, Conrad KJ. The Use of Content Balancing Procedures to Estimate Multiple Clinical Domains in Computerized Adaptive Testing; Relative Precision, Efficiency and Detection of Atypical Responding: Technical Report. Chestnut Health Systems; Bloomington, IL: 2007. [Google Scholar]
- Schmitt N, Chan D, Sacco JM, McFarland LA, Jennings D. Correlates of person fit and effect of person fit on test validity. Appl Psychol Meas. 1999;23:41–53. [Google Scholar]
- Shafii M, Carrigan S, Whittinghill JR, Derrick A. Psychological autopsy of completed suicide in children and adolescents. Am J Psychiatry. 1985;142(9):1061–4. doi: 10.1176/ajp.142.9.1061. [DOI] [PubMed] [Google Scholar]
- Shafii M, Steltz-Lenarsky J, Derrick AM, Beckner C, Whittinghill JR. Comorbidity of mental disorders in the post-mortem diagnosis of completed suicide in children and adolescents. J Affect Disord. 1988;15(3):227–33. doi: 10.1016/0165-0327(88)90020-1. [DOI] [PubMed] [Google Scholar]
- Simon TR, Swann AC, Powell KE, Pottter LB, Kresnow M, O’Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(Supplement):49–59. doi: 10.1521/suli.32.1.5.49.24212. [DOI] [PubMed] [Google Scholar]
- Smith RM. A comparison of Rasch person analysis and robust estimators. Educ Psychol Meas. 1985;45:433–444. [Google Scholar]
- Smith RM. Person fit in the Rasch model. Rasch Meas Trans. 1986:359–372. [Google Scholar]
- Smith RM, Schumacher RE, Bush MJ. Using item mean squares to evaluate fit to the Rasch model. J Outcome Meas. 1998;2:66–78. [PubMed] [Google Scholar]
- Stevens S, Murphy B, McKnight K. Traumatic stress and gender differences in relationship to substance abuse, mental health, physical health, and HIV risk behavior in a sample of adolescents enrolled in drug treatment. Child Maltreatment. 2003;8:46–57. doi: 10.1177/1077559502239611. [DOI] [PubMed] [Google Scholar]
- Strauss MA. Conflict Tactic Scale. In: Strauss MA, Gelles RJ, editors. Physical violence in American families: Risk factors and adaptations to violence in 8, 145 families. Durham, NH: University of New Hampshire; 1990. [Google Scholar]
- Tellegen A. The analysis of consistency in personality assessment. J Personality. 1988;56:621–663. [Google Scholar]
- U.S. Public Health Service. The surgeon general’s call to action to prevent suicide. Washington, D.C: 1999. [Google Scholar]
- Vandivort DS, Locke BZ. Suicide ideation: its relation to depression, suicide and suicide attempt. Suicide Life Threat Behav. 1979;9:205–218. doi: 10.1111/j.1943-278x.1979.tb00439.x. [DOI] [PubMed] [Google Scholar]
- Williams C, Davidson J, Montgomery I. Impulsive suicidal behavior. J Clin Psychol. 1980;36:90–94. doi: 10.1002/1097-4679(198001)36:1<90::aid-jclp2270360104>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Wilson M. Constructing measures: An item response modeling approach. Mahwah, NJ: Erlbaum Associates; 2005. [Google Scholar]
- Wright BD, Masters GN. Rating scale analysis. Chicago, IL: MESA Press; 1982. [Google Scholar]
- Wright BD, Stone MH. Best test design. Chicago: University of Chicago, MESA Press; 1979. [Google Scholar]
- Zickar MJ, Drasgow F. Detecting faking on a personality instrument using appropriateness measurement. Appl Psychol Meas. 1996;20:71–88. [Google Scholar]
- Zickar MJ, Robie C. Modeling faking good on personality items: An item-level analysis. J Appl Psychol. 1999;84:551–563. [Google Scholar]