Abstract
Aim
To examine the characteristics of community health workers (CHWs) involved in diabetes prevention programmes (DPPs) and their contributions to expected outcomes.
Methods
Electronic databases including PubMed-MEDLINE, EBSCOHost, and SCOPUS/EMBASE were searched for studies published between January 2000 and March 2016. All studies that used CHWs to implement DPP in ≥18-year-old participants without diabetes but at high risk for developing the condition, irrespective of the study design, setting or outcomes measured, were included. Results were synthesized narratively.
Results
Forty papers of 30 studies were identified. Studies were mainly community-based and conducted in minority populations in USA. Sample sizes ranged from 20 participants in a single community to 2369 participants in 46 communities. Although CHWs were generally from the local community, their qualifications, work experience and training received differed across studies. Overall the training was culturally sensitive and/or appropriate, covering topics such as the importance of good nutrition and the benefits of increased physical activity, communication and leadership. CHWs delivered a variety of interventions and also screened or recruited participants. The shared culture and language between CHWs and participants likely contributed to better programme implementation and successful outcomes.
Conclusions
The complexity of DPPs and the diverse CHW roles preclude attributing specific outcomes to CHW involvement. Nevertheless, documenting potential CHW roles and the relevant training required may optimise CHW contributions and facilitate their involvement in DPPs in the future.
Introduction
The rapid worldwide increase in type 2 diabetes (henceforth referred to as diabetes) has led to the development of a variety of different delivery models to prevent the development of this condition. To this end, a number of large randomised controlled trials (RCT) have demonstrated that lifestyle interventions reduce the incidence of diabetes between 29% and 58% in high-risk populations, and this can be maintained for well over 10 years [1]. However, these programmes when conducted under research conditions are usually resource intensive and thus, not practical or feasible to conduct in primary healthcare (PHC) or community-based settings. Particularly costly is employing professional healthcare workers to implement such interventions, it is not the best use of this resource, especially in developing regions with shortages of skilled healthcare workers.
The global need for efficient and cost-effective use of healthcare resources, particularly in low-income countries has led to the introduction of lay health workers or non-professional community health workers (CHWs) to fulfil a variety of tasks and roles such as patient care, education, support for care delivery, care coordination and social support, especially in remote areas or among minority groups [2, 3]. CHWs have become involved with supporting and filling a variety of capacities in healthcare programmes [4], including in relation to diabetes prevention programmes (DPPs). CHW-led support services to improve health outcomes range from small community-based initiatives to large national programmes. CHWs can be an important link between the community and healthcare, an intervention programme or service delivery by providing context-specific support [2, 5], which can lead to better long-term outcomes for the participants. Such individuals usually have commonality with the community they serve in terms of ethnicity, language, socioeconomic status and life experiences [6]. Rosenthal et al. [7] refers to CHWs as an umbrella term which includes “outreach workers, promotores (as) de salud, community health representatives, and patient navigators”. In a systematic review and meta-analysis of 28 United States (US)-based DPPs, Ali and colleagues [8] described the successes of CHW implemented DPPs. Most significantly, they reported that CHW-delivered interventions were associated with a similar change in weight at follow-up compared with health professional implemented programs [8].
To improve the delivery and outcomes of DPPs that CHW’s are involved with, it is important to identify the key characteristics of CHWs as well as the required training and level of support that are required. However, there is a shortage of such comprehensive assessments in the literature. Therefore, this systematic review aims to examine CHW implemented DPPs and describe the key characteristics that contributed to positive outcomes.
Methods
Data sources
We developed a systematic review protocol using guidelines described by the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) [9], which was registered on the PROSPERO Register (CRD42016043237). The electronic databases searches were done on MEDLINE via PubMed Central, EBSCOHost, and SCOPUS/EMBASE. Free text as well as Medical Subject Headings (MESH) were used, including community health workers, lay health workers, non-professional health workers, Promotores de Salud, community health aids, peer advisors, community health advisors, village aids, community aids, lay counsellors, health promotores, community health promotores, village health volunteers, lay health educators diabetes, diabetes mellitus, type 2 diabetes, and prevention. Boolean operators, such as AND/OR/NOT were used to string terms together. Searches were limited to publications in English. For example in PubMed Central the search strategy was the following:
("community health workers"[MeSH Terms] OR ("community"[All Fields] AND "health"[All Fields] AND "workers"[All Fields]) OR "community health workers"[All Fields]) AND ("diabetes mellitus"[MeSH Terms] OR ("diabetes"[All Fields] AND "mellitus"[All Fields]) OR "diabetes mellitus"[All Fields] OR "diabetes"[All Fields] OR "diabetes insipidus"[MeSH Terms] OR ("diabetes"[All Fields] AND "insipidus"[All Fields]) OR "diabetes insipidus"[All Fields]) AND ("prevention and control"[Subheading] OR ("prevention"[All Fields] AND "control"[All Fields]) OR "prevention and control"[All Fields] OR "prevention"[All Fields])
Additional methods to identify studies included manually searching journals and conference proceedings, checking reference lists, and identifying unpublished data. One author and an independent assessor (JH, LM) independently identified potentially relevant studies by reviewing titles and abstracts retrieved from the aforementioned databases. The full texts of studies identified as potentially relevant were retrieved and screened in duplicate for inclusion. Consensus was achieved through discussion and, when needed, consultation with a senior author (APK).
Definition of community health workers
For the purpose of this review, a CHW is any lay or non-professional health worker involved with the delivery of a diabetes prevention programme, either as a volunteer or for a stipend. This accords with Norris’s description of a CHW as an individual without formal healthcare training but trained to deliver context-specific healthcare to a community with whom s/he has a relationship [2].
Study inclusion criteria
All studies that used CHWs to implement DPP in ≥18-year-old participants without diabetes but at high risk for developing the condition, irrespective of the study design, setting or outcomes measured, were included. Studies that examined outcomes only among the CHWs, e.g. reports of CHW training interventions were also included because the aim of this systematic review is to establish the key characteristics of CHWs who contribute to successful DPP.
Eligible studies included those published in peer-reviewed journals from January 2000 until March 2016. Studies were excluded if they: 1) focused on diabetes management, 2) did not make use of CHWs, 3) comprised interventions of less than three months’ duration, or 4) were narrative reviews, opinion pieces, letters to the editor or any other form of publication without primary data.
Data extraction and synthesis
Two data extraction tables summarise the data from the included studies. Table 1 shows the study-specific details such as the authors’ names, demographic data, methodology and outcomes. Table 2 describes the CHW-specific characteristics including gender, age, education level, the training and support they received, and their role in the intervention. JH entered the summary data in the tables and LM then checked these. Given that the studies included in this systematic review were not sufficiently similar for a meta-analysis, data were synthesised narratively. We compiled thematic summaries relevant to the review objective and research questions stated in the systematic review protocol (unpublished).
Table 1. Study characteristics.
| Author; Year published | Country/Region; Setting | Study design, intervention and comparator | Participant characteristics | Outcomes measure | Effect of intervention | Length of intervention |
|---|---|---|---|---|---|---|
| 1. West et al., 2011 [10] 2. Krukowski et al., 2013 [11] 3. Krukowski et al., 2013 [12] |
Arkansas—USA; Senior centres | Design: Cluster RCT [lifestyle weight loss vs. cognitive training programme] | N = 228 Gender: 84% Female Age range: 60+ Race/ethnicity: 92% white |
Primary: Weight loss of ≥5% Secondary: Examination of costs Tertiary: Evidence to train lay health educators (LHE) to implement weight loss interventions |
Physiological outcome: 3.7 kg weight loss at 4 months Cost/economic outcome: a LHE-delivered DPP translation is effective in achieving weight loss at low cost at senior centres Implications for training LHE: Methods used produced favourable long-term retention of LHE’s and good adherence to intervention protocol |
-12 weekly group sessions -60 minutes each |
| 4. Perez et al., 2015 [13] | Philadelphia (US); clinical and community settings |
Design: RCT–parallel group design [standard care vs. metformin/ DDP lifestyle intervention to normal care] - 3-arm RCT | N = 92 Gender: 100% Female Age range: 45.1±12.5 Mean age: ≥20 years Race/ethnicity: Latina |
Primary: 12-month weight difference between groups Secondary: cardio metabolic markers |
Only baseline characteristics available | 24 sessions over 12 months, 12 weekly core sessions followed by ten maintenance sessions [90-minute sessions] |
| 5. Katula et al., 2010 [14] 6. Blackwell et al., 2011 [15] 7. Katula et al., 2011 [16] 8. Katula et al., 2013 [17] 9. Lawlor et al., 2013 [18] [HELP-PD] |
Forsythe County, North Carolina (US); Community-based |
Design: RCT -DPP lifestyle weight loss vs. enhanced usual care |
N = 301 overweight & obese volunteers/ Pre-diabetics Gender: 57.5% female Age: ≥ 21 years Mean Age: years: 57.9 ±9.5 Race/ethnicity: mostly white (73.8%) |
Primary: change in fasting glucose Secondary: change in CVD risk factors, health-related quality of life & social cognitive variables Tertiary: cost effectiveness |
1 year results: Physiological outcomes: Intervention participants experienced significantly greater decreases in: -blood glucose (-4.3 vs. -0.4mg/dL; p <0.001) -insulin (-6.5 vs. 2.7 μU/mL; p <0.001) -homeostasis model assessment of insulin resistance (-1.9 vs. 0.8; p <0.001) -weight (-7.1 vs. -1.4 kg; p <0.001) -BMI (-2.1 vs. -0.3 kg/m2; p <0.001) -waist circumference (-5.9 vs. -0.8 cm; p <0.001) 2 year results: Physiological outcomes: -LWL participants significantly greater decreases in fasting glucose (-4.35 mg/Dl); insulin (-3.01 μU/ml); insulin resistance (-0.97); body weight (-4.19 kg); waist circumference (-3.23 cm); BMI (-1.40), with all p-values <0.01. Cost/economic outcome: Substantially lower medical costs. |
24 months [weekly sessions for 6 months, followed by monthly sessions (7–24 months] |
| 10. Islam et al., 2013 [19] | New York [Korean Community], Community setting |
Design: RCT | N = 48–25 in treatment group & 23 in control group Gender: 64% female Age: 18–75 years Mean Age: 59.7 years Race/ethnicity: Korean |
Primary: clinical measurements Secondary: health access |
No significant differences between treatment & control groups Changes in: Physiological Outcomes: -weight, -waist circumference,—systolic blood pressure, -physical activity Behavioural outcomes: -nutrition and diabetes knowledge as well as mental health |
6 month intervention period |
| 11. Horowitz et al., 2011 [20] [Project HEED] |
East Harlem, New York (US); Community-based | Design: RCT: Using a participatory approach, the partnership chose to focus on diabetes prevention, & co-developed all intervention, recruitment, research & evaluation strategies | N = 99 Gender: 85% female Age: ≤ 18 Race/ethnicity: 87% Latino |
Primary: effectively translating diabetes prevention Secondary: weight loss/impact local health |
Physiological Outcome: Achieved statistically significant weight loss |
8 sessions |
| 12. Duggan et al., 2014 [21] | Yakima Valley (rural area) (US); Educational sessions conducted in participants’ homes | Design: A parallel two-arm RCT | N = 228 Gender: 70.6% female Mean Age: 50.6 years Race/ethnicity: Hispanics |
Primary: HbA1c levels Secondary: Fruit & vegetable consumption Tertiary: Frequency and intensity of physical activity |
Physiological Outcome: -Intervention group showed significant improvement in HbA1c scores (-37.5%, p = 0.4) Behavioural Outcome: -a trend of greater increases in the frequency of moderate & vigorous physical activity in the intervention group |
5 weeks |
| 13. Koniak-Griffin et al., 2015 [22] | Southern California (US); Community settings | Design: A community prevention model was employed in planning & implementing this RCT | N = 223 Gender: Females Age: 35–64 years Mean age: 44.6 years Race/ethnicity: Latina |
Primary: Evaluate the effects of a lifestyle behaviour intervention by specially trained promotoras Secondary: Acceptability & feasibility of intervention |
Physiological Outcomes: -Statistically significant positive effect on waist circumference -Receiving higher intensity (dosage) of the intervention was modestly beneficial in terms of greater improvement in body mass index, weight, and waist circumference. Behavioural Outcomes: - Statistically significant positive effect on dietary habits, patterns of physical activity (daily steps), and knowledge about heart disease (e.g., risk factors, prevention measures). |
6 month lifestyle behaviour intervention |
| 14. Sathish et al., 2013 [23] | Rural Kerala, India; Community-based | Design: A cluster RCT of a peer-led lifestyle intervention | Inclusion criteria: Gender: Males & females on the electoral roll Age: 30–60 years Race/ethnicity: Malayan |
[EXPECTED] Outcomes: Behavioural outcomes -improved diet -increased physical activity -reduced tobacco use -reduced alcohol consumption Psychosocial outcomes -reduced stress -improved quality of life Clinical outcomes -reduced BP -reduced waist circumference -reduced body fat Biochemical outcomes -reduced incidence of diabetes -improved glycaemic control -improved lipid profile |
-11 peer-led small group sessions -2 education sessions led by experts |
|
| 15. Simmons et al., 2008 [24] |
Te Wai o Rona (New Zealand); Community-based |
Design: A cluster-RCT of intensive lifestyle change [pilot study cohort] |
N = 212 Vanguard: Gender: 34.4% male Mean age: 47 years Control: Mean age: 50 years Gender: 40.4% male Race/ethnicity: Maori |
Primary: 35% reduction in incident diabetes among Maori Secondary: cost effectiveness |
Physiological Outcome: -significant weight loss among all participants in pilot (-1.3 (SD 3.6) kg, p <0.001) Intervention Acceptability: -Participants & CHW found the messages, toolkit & delivery approach acceptable |
-not clear -mean of 189 days of intervention over study period |
| 16. DeJoy et al., 2013 [25] [FUEL Your Life] |
Union Pacific Railroad locomotive maintenance facility (US); Worksite |
Design: Intervention development Formative: stakeholder interviews, focus groups, and observation of work environment Pilot study method: single group design with data collection at three time points: baseline, 6 months, and 12 months |
N = 167 Gender:97% men Age: 20-69years Mean age: 47 years Race/ethnicity: 85% white |
Primary [pilot study]: Adaption/translation of DPP for the workplace Secondary: weight loss |
Physiological Outcome: -Modest but statistically significant weight reductions at both 6 (core intervention period) and 12 months (maintenance period) |
24 weeks |
| 17. Brace et al., 2015 [26] [FUEL Your Life] |
Union Pacific Railroad locomotive maintenance facilities (US); Worksite | Intervention Evaluation: The RE-AIM (Reach Effectiveness Adoption Implementation Maintenance) framework was used to examine the factors that influenced programme implementation using data from an environmental assessment, participant surveys, peer health coach surveys, peer health coach surveys, and occupational health nurse surveys | N = 479 employees enrolled Gender: 94% male Mean age: 46 years Race/ethnicity: 75% Caucasian [236 participants at post-test] |
Primary outcomes: -7% weight loss -150 minutes of physical activity Secondary: Process evaluation |
Physiological Outcome: Overall, the programme was effective for weight maintenance. |
Duration of FUEL Your Life |
| 18. Wilson et al., 2016 [27] [FUEL Your Life] |
Union Pacific Railroad locomotive maintenance facilities (US); Worksite |
Intervention implementation: RCT–five worksites |
N = 362 workers Gender: 94% male Mean age 46 Race/ethnicity: predominantly white (80.6% control, 71.60% treatment) |
Primary outcomes: -7% weight loss -150 minutes of physical activity |
Physiological Outcome: Participants in the intervention group maintained weight/BMI (-.1 pounds/-.1 BMI), whereas the control participants gained weight/BMI (+2.6 pounds/+.3 BMI), resulting in a statistically significant difference between groups. Fifty-five percent of intervention participants lost some weight, whereas only 35% of the control group lost weight |
12 months |
| 19. Ockene et al., 2012 [28] |
Lawrence, Massachusetts (US); Individual sessions at home & group sessions at senior centre (community site) |
Design: Lifestyle intervention care vs. Usual care | N = 312 Gender:74% female Age: 25–79 years Mean age: 52 years. Race/ethnicity: Hispanic/Latino |
Primary: weight loss & diabetes risk reduction | Physiological Outcomes: -Intervention group had a moderate but significant weight reduction (-2.5 vs. 0.63lb; p = .04) -clinically meaningful reduction in HBA1c (-0.10% vs. -0.04%; p = .009) -improved insulin resistance |
-Three individual and 13 group sessions over a 12-month period |
| 20. Staten et al., 2012 [29] [Pasos Adelante/ “Steps Forward”] |
Douglas Arizona (US-Mexico border); Community setting | Design: Quasi experimental pre-test, post-test study with follow-up | N = 305 (conclusion of programme 254, 3-month follow-up 221) Gender: 92% female Mean Age: 54.4 years Race/ethnicity: Hispanic |
Primary: Improvements in select physiological measures | Physiological Outcomes: Decreases in: - BMI (p = 0.04) -waist & hip circumference (p <0.001) -diastolic & systolic BP (p <0.001) -total cholesterol (p = 0.008) -glucose levels improved between conclusion & follow-up (p = 0.01) |
12 week sessions |
| 21. Islam et al., 2014 [30] [Project RICE] |
New York (US); Community-based |
Design: A quasi-experimental two-arm design pilot study |
N = 126 baseline (108 completed baseline & 6-month follow-up) Gender: 96% female (treatment grp.) Age: 18–75 years Mean age: 46.3 years (treatment grp.) Race/ethnicity: Sikh Asian Indian immigrants |
Primary: clinical variables (weight, BMI, waist, BP, glucose & cholesterol) Secondary: health behaviours |
Physiological Outcomes: Significant changes for treatment group in: -weight BMI -waist circumference -BP -glucose -physical activity -food behaviours -diabetes knowledge |
6-month intervention period |
| 22. Thompson et al., 2015 [31] | Rural Virginia (US); Housing complexes/camp | Design: Pilot study (quasi-experimental) | N = 66 [Migrant farmworkers] Gender: Males Age: 18–64 years Mean age: 33.67 years Race/ethnicity: Mexican |
Primary: Latino CHW can use non-invasive diabetes & CVD screening tools with similar accuracy as a registered nurse | -CHW perform similarly to registered nurses in the use of non-invasive DM and CVD tools -Risk screening |
One screening session. One follow-up call, if required |
| 23. Oba et al., 2011 [32] | Thailand; Community setting |
Design: Three-stage approach -situational analysis -model development -testing |
N- = 160 Gender: 91% female Age: > 35 years Mean age: 45.06 years Race/ethnicity: Thai [Pre-diabetics] |
Primary: to promote positive behaviour & lifestyle changes Secondary: to evaluate the effectiveness of the programme |
Physiological Outcomes: -BMI score lower (p = 0.001) -waist circumference lower (p = 0.01) -systolic BP lower (p = 0.01) Behavioural Outcome: -Mean score for physical activity increased (p≤0.01) |
+3 times a week for 3 months |
| 24. Balagopal et al., 2012 [33] | Gujarat (India); Community setting (rural villages) |
Design: A community-based participatory research method used to plan & tailor the intervention by engaging trained CHW as change agents to provide lifestyle education, serve as community advocates & collect data | N = 1638 Gender: 53% female Age: ≥ 18 years Mean age: 41.9 years Race/ethnicity: [rural] Indians |
Primary: to evaluate the effectiveness of a CBPR approach to diabetes prevention | Physiological Outcomes: –Reduced blood glucose levels by 5.7 & 14.9 mg/dL for individuals with prediabetes & diabetes respectively -lowered systolic & diastolic BP by 8mm Hg & 4mm Hg respectively in overall population -general & abdominal obesity also decreased by ≤1% Knowledge Improvement: -knowledge of diabetes & CVD improved by 50% in the high SES group & doubled in the low SES group |
6 months -lifestyle intervention = five one-on-one and five group based encounters |
| 25. O’Brien et al.,2015 [34] | Philadelphia (US); Community-based | Design: A pilot trial | N = 20 Gender: Females Age: ≥ 20 years Mean age: 44.5 years Race/ethnicity: Latina |
Primary: to evaluate weight changes & cardio metabolic markers (waist, BP, plasma glucose, insulin, HbA1c, lipids) Secondary: assess the feasibility & acceptability of intervention |
Physiological Outcomes: -Mean weight loss of 10.8 pounds at 12 months -significant pre-post reductions in waist circumference, diastolic BP, LDL cholesterol & insulin levels -modest reductions in A1c and fasting plasma |
12 months -24 session curriculum |
| 26. Benyshek et al., 2014 [35] [The Life in BALANCE pilot study] |
Nevada, Las Vegas (US); Community-based resource centre | Design: A pilot translational study modelling the DPP intensive lifestyle coaching intervention | N = 22 [only 12 at the final post-programme follow-up] Gender: 83% female Age: ≥ 21 years Mean age: 39.6 years Race/ethnicity: American Indians / Alaska Natives |
Primary: translation of DPP for urban American Indians / Alaska Natives Secondary/Clinical measures: weight, BMI, waist, BP, blood lipids, fasting blood glucose, HbA1c |
Physiological Outcomes: -Significant decreases in waist circumference & elevated HDL cholesterol -triglycerides manifested the highest percentage change without statistical significance |
16 weeks intensive life coaching intervention |
| 27. Philis-Tsimikas et al., 2014 [36] | San Diego County (US); Community clinic setting | Design: A single-group pre-post design was utilised | N = 84 Gender: Females Age: 18–45 years Race/ethnicity: Latina |
Primary: HbA1c Secondary: lipids & BP Tertiary: [Self-reported]: physical activity, diet, perceived health, fatalistic beliefs, diabetes-specific cultural beliefs |
Significant (p <0.05) improvements in: Physiological Outcomes: -lipids -BP Behavioural Outcomes: -physical activity -dietary fat intake Knowledge Improvements: -fatalistic & cultural diabetes beliefs |
-8-week intervention -monthly maintenance & support sessions offered to participants following completion of the primary intervention period |
| 28. Cherrington et al., 2015 [37] |
Birmingham, Alabama (US); Community setting | Design: Developed a theory-based, promotora-delivered intervention to promote weight loss among immigrants an emerging Latina community in Alabama | N = 22 Gender: Females Mean age: 36.5 years Race/ethnicity: Latina |
Primary: to develop & pilot test a theory-based, promotora-delivered, peer support weight loss intervention | Physiological Outcomes: -significant weight loss (mean 2.1 kg, SD 2.6, p <0.001) Behavioural Outcomes: -levels of moderate physical activity increased (p <0.05) -dietary practices improved (p <0.001) -depressive symptoms also improved (p <0.001) |
8-week intervention |
| 29. Ruggiero et al., 2011 [38] | Southwest Chicago (US); Community setting | Design: A nonrandomized prospective study using a single-group design | N = 69 Gender: 92.8% female Age: 18–65 years Mean age: 37.86 years Race/ethnicity: Hispanic |
Primary: Anthropometric measures & Secondary: paper & pencil measures were administered to examine programme outcome |
Physiological Outcomes: At 6 months: -20% of the sample achieved a 7% weight loss goal -29% achieved a 5% weight loss goal At 12 months: -16% achieved 7% weight loss goal -30% achieved 5% weight loss goal |
1 year programme |
| 30. Treadwell et al., 2010 [39] |
Lorain county, Ohio (US); Community-based | Design: The save our son’s study is a community-based, culturally responsive 7 gender-specific intervention aimed at reducing obesity & diabetes among a small sample of African American men | N = 42 Gender: Males Race/ethnicity: African American |
Primary: feasibility of implanting a group health education & intervention model Secondary: access to & utilisation of health care services & community supportive resources |
Physiological Outcomes: -decreased BP, weight, BMI Behavioural Outcomes: -increased levels of exercise & fitness activities Knowledge Improvements: -participants had greater knowledge about strategies for prevention & management of obesity & diabetes |
6-week intervention |
| 31. Cadzow et al., 2013 [40] 32. Cadzow et al., 2014 [41] |
Buffalo city (US); Community settings |
Design: The Neighborhood Health Talker project aimed to train & implement cultural health brokers primarily targeting communities of colour to improve diabetes knowledge & diabetes self-management skills [Pre-test/Post-test] |
N = 13 CHW Gender: 92% female [12 women, one man] Age: 35–65+ years Race/ethnicity: Black/African American +700 community members) N = 208 (survey participants) 61.8% female Mean age: 33.6 years |
Primary: evaluation results of a community-based diabetes education pilot project Secondary: Diabetes resource libraries established |
Knowledge Improvements: -The training was successful in increasing trainee knowledge and confidence about diabetes prevention and self-management. Behavioural Outcomes: -Participants not only developed proficiency in discussing diabetes, they also made important lifestyle changes that demonstrated their commitment to the cause and the project Intervention Outcomes: -50 community conversations Eight resource libraries |
-5 Community conversations -July-October 2009 |
| 33. Staten et al., 2005 [42] [Pasos Adelante/ “Steps Forward”] |
Yuma & Santa Cruz counties, Arizona (US); Community-based (Churches, schools, health fairs) |
Design: A 12-week programme facilitated by CHW |
N = 248 (216 completed) Mean age: 49.5 Gender: mostly female Race/ethnicity: Hispanics |
Primary: primary prevention of chronic disease | Behavioural Outcomes: -Significant increase in moderate to vigorous walking -shifts in nutritional patterns |
12-week programme |
| 34. Sosa et al., 2013 [43] |
San Antonio, Texas (US) | Design: Recruitment, training & evaluation of intervention fidelity of Promotoras de Salud for obesity and diabetes prevention | N = 5 promotoras Gender: Females Age: 38–54 years Mean age: 46.5 years Race/ethnicity: Mexican American] N = 36 participants |
Primary: describe training process Secondary: fidelity of study protocol implementation |
Knowledge Improvements: -Post knowledge test scores were high (M = 83.5; SD = 6.4) Intervention Acceptability: -study participants perceived promotoras to be supportive & helpful in assisting them to reach their goals |
14 sessions, 90 min. each |
| 35. Kousar et al., 2015 [44] | Melbourne (Aus.); homes of community members or CHVs | Design: Strengthening capacity of key community volunteers to support diabetes prevention and self-management | N = 17 Community health volunteers Gender: Females Age: 20–60 years Race/ethnicity: Australian immigrants, fluent in at least one non-English language N = 30 Community members Mean age: 44 years Race/ethnicity: Culturally and linguistically diverse |
Primary: effectiveness of diabetes prevention & management model | Knowledge Improvements: -Diabetes knowledge among CHVs increased - Diabetes knowledge among community members increased Intervention Outcome: -CHVs were able to collect anthropometric data & knowledge surveys with greater participation than outreach programmes |
Not clear |
| 36. Coppell et al., 2009 [45] | Ngati (New Zealand); Community-based | Design: Interrupted time-series prevalence surveys with a process evaluation | [2003] N = 286 Gender: 59% female [2006] N = 235 Gender: 59% female Two age groups: -25-49 years. -50+ years Race/ethnicity: Indigenous Ngati Porou (Maori) community |
Primary: reduce the prevalence of insulin resistance | Physiological Outcomes: -Insulin resistance prevalence decreased markedly from 35.5% to 25.4% (p = 0.003) |
Ongoing |
| 37. Schulz et al., 2005 [46] | Detroit, Michigan (US); Community-based | Design: A case study description & analysis of the Healthy Eating & Exercise to Reduce Diabetes project in the theoretical context of a conceptual model of social determinants of health | A community | Primary: reduce the risk/delay onset of diabetes | Intervention Outcome: Barriers and facilitators to applying a social determinants model identified |
2 years |
| 38. Cohen & Ingam 2005 [47] 39. Teufel-Shone, Drummond & Rawiel et al., 2005 [48] 40. Reinschmidt et al., 2010 [49] |
U.S.-Mexican border; Community-based |
Design: Community case studies Design: Comparative study |
Yuma & Santa Cruz communities Race/ethnicity: Predominantly Hispanic (89.1–95.2%) |
Primary: description & analysis of a community-based model for diabetes prevention & control Secondary: building capacity of the communities to work together to establish comprehensive, integrated & sustainable diabetes prevention & control programmes Tertiary: Success of academic-community partnership Primary: development and adaptation of a culturally appropriate family-based diabetes program Primary: demonstration of how interventions are adapted at the intersection of multiple cultural contexts Secondary: comparing and contrasting original adaptations–addressing the tension between fidelity and adaption Tertiary: demonstrating the centrality of adaption of negotiations to community-based participatory and capacity building approaches. |
Intervention Outcomes: -Building capacity of the communities to work together to create comprehensive, integrated, & sustainable diabetes prevention & control programmes -the overwhelming success of this academic-community partnership to integrate both research & community perspectives to address the devastating toll of diabetes academic Knowledge improvements: -significant increase in diabetes risk knowledge Behaviour Outcomes: -significant decreases in the frequency of intake in sugar sweetened beverages -trend in exercising five or more times a week for 30 minutes or more Significant increase in participants reporting familial support Study Conclusions: - while socio-cultural are not required because the programme is appropriate for a particular population, adaptions that compliments the goals, objectives and resources of local agencies are important -the complexity of experiences, expertise and strengths of the other contexts pertinent to programme adaption requires consideration by public health practitioners - intervention curricula need to be balanced between fidelity and adaption - curricula that is too scripted, ignores the strengths of promotores or other CHW which are at the centre of this balance -adapting programs to the complexity of context is critical to facilitating local ownership and sustainable program |
-NP -12 week programme (10 points of contact) |
| 41. Whittemore et al., 2013 [50] | U.S.; Public housing community centres |
Design: Mixed-method embedded design |
N = 67 Gender: 79% female Age: >21 years Mean age: 40 years Race/ethnicity: 79% non-white |
Primary: description of implementation process Secondary: barriers & facilitators to programme identified |
Intervention Outcomes: -Home-care nurses were able to implement a DPP programme in public housing communities -nurses & CHW were resourceful & positive about programme implementation -linking existing resources is one approach to disseminating DPPs |
-6 months |
Table 2. CHW-specific characteristics.
| Authors | Demographics of CHW | CHW eligibility | Training [type] received | Length of training received | Support provided to CHW | Role of the CHW |
|---|---|---|---|---|---|---|
| 1. West et al., 2011 [10] 2. Krukowski et al., 2013 [11] 3. Krukowski et al., 2013 [12] |
Gender: 90% women Mean age: 61 years Mean education level: 70% reported some college or a college degree |
NP | Content: - All aspects of delivering the lifestyle programme - key elements of a behavioural weight-control approach - protocol fidelity Intervention goals -behavioural strategies -giving feedback on self-monitoring diaries -recruitment methods -techniques for conducting effective group sessions -individual session materials reviewed and rehearsed -responsible conduct of research -obtained human subjects protection certification Format: - face-to-face training -experiential learning exercises |
32 hours | A weekly technical support conference call | Lay health educators delivered 12 weekly sessions |
| 4. Perez et al., 2015 [13] | Gender: NP Mean age: NP Mean education level: NP |
-High school completion -Spanish language fluency -natural leadership skills -commitment to serving their community |
Content and Format: -18-hour training on Group Lifestyle Balance protocol -2-day training on diabetes prevention -post-intervention feedback sessions: 50h (2h per session) over a 2-month period |
±34 hours | Ongoing supervision to CHW during implementation by the director of the promotora programme | One CHW leads or runs the session, the second provides logistical support, including weighing participants |
| 5. Katula et al., 2010 [14] 6. Blackwell et al., 2011 [15] 7. Katula et al., 2011 [16] 8. Katula et al., 2013 [17] 9. Lawlor et al., 2014 [18] [HELP-PD] |
Gender: 8 Females, 2 males Mean age: 57.2 years Mean education level: -8 reported some education - all (10) completed some form of diabetes self-management education |
-Recruited patients with Type 2 diabetes -experience in group leadership -well controlled HbA1c -history of healthy eating, physical activity & weight loss -evidence of potential for effective leadership (prior experience & strong interpersonal skills) |
Training style/approaches: -experiential learning -didactic instruction -peer monitoring -observation Content: -study protocol -intervention philosophy, goals & procedures -weight loss (energy balance) -physical activity basics -nutrition basics -group facilitation -cognitive-behavioural principles -participant monitoring & toolbox methods -data entry |
36-hour programme over the course of 6–9 weeks | -Trained & monitored by registered dieticians | -Conducted the lifestyle intervention group sessions -managed group participants -data entry of participant body weights obtained in each session |
| 10. Islam et al., 2013 [19] | Gender: NP Mean age: NP Mean education level: NP |
-Trained (at a medical school), bilingual Korean-American CHW |
Content and Format: -60-hour core competency-based training 30 hours of additional training on mental health; motivational interviewing & other related topics. |
-60 hours, over eight days in a three-week period -30-hour additional training Total = 90 hours |
No info | -Facilitated group sessions -follow-up phone calls |
| 11. Horowitz et al., 2011 [20] [Project HEED/HEAL] |
Gender: NP Mean age: NP Mean education level: NP |
NP | NP | NP | NP | Delivered classes [Trained to conduct eight, 90-minute classes (6 weekly, then two bi-weekly)] |
| 12. Duggan et al., 2014 [21] | Gender: NP Mean age: NP Mean education level: NP |
NP | Content: -diabetes education -working in the community Training Resources: -CDC’s CHW Evaluation Tool Kit -training by a local diabetes specialist |
100 hours | -twice-yearly refresher courses | -recruitment -conducted sessions |
| 13. Koniak-Griffin et al., 2015 [22] | Gender: NP Mean age: NP Mean education level: Promotoras had a high school diploma or equivalent |
-Four or more years’ employment as a community health worker -either resided in or had extensive work experience in the community where the study was implemented |
Content: -Orientation to the study -extensive training in the curriculum -protocol-defined content -behaviour change -human subjects’ protection -structured training activities, including 4 days focusing on delivery of modules in Su Corazón, Su Vida [Your Heart, Your Life] (conducted by a bilingual promotora trainer with extensive experience implementing the curriculum and educating promotoras) -research-specific skill sessions |
100 hours | -Regular staff meetings with opportunities to discuss experiences -observations of performance in classes and home visits to verify the accuracy of content and appropriateness of counselling in the Individual Teaching and Coaching sessions |
-delivered 6-month intervention |
| 14. Satish et al., 2013 [23] | Gender: NP Mean age: NP Mean education level: NP |
NP | Content: -Group facilitation -communication skills -how to set & monitor goals for lifestyle behaviours -goal setting & planning for a healthy lifestyle |
2 days | -Refresher training (2days) after session 5 -peer leaders contacted before & after each session to share their experiences -face-to-face meetings with groups of peer leaders at regular intervals -ongoing support & communication between the peer leaders & the K-DPP intervention team & among peer leaders |
-Deliver small group sessions -keep a record of each interaction with participants & intervention team |
| 15. Simmons et al., 2008 [24] |
Gender: NP Mean age: NP Mean education level: NP |
NP | Content and Format: -Trained to deliver intervention based on social cognitive theory Maori CHW training was provided in modular form covering: -basic anatomy & physiology -communication skills -motivational interviewing -broader health issues -the content & background to the 12 messages of lifestyle intervention Training resources: *A desk file (including safety & engagement principles & intervention approach) & a toolkit supporting the 12 messages were created from existing materials or developed de novo & distributed in a case to each Maori CHW (included a personal digital assistant (PDA) each Maori CHW was allocated a set of scales |
NP | NP | -Delivered the intervention |
| 16. DeJoy et al., 2013 [25] FUEL Your Life |
Gender: NP Mean age: NP Mean education level: NP |
-Peer coaches were identified by occupational nurses | Format: -Given talking points for each lesson to use in reinforcing the self-study programme -participated in a 1-hour training session with the research team Training Resource: -received a peer health coach manual |
1-hour training session | NP | -Peer health coaches -ongoing informal contact with participants -responsible for providing basic information, answering simple questions -providing encouragement & support |
| 17. Brace et al., 2015 [26] FUEL Your Life |
Gender: NP Mean age: NP Mean education level: NP |
-Peer health coaches were identified by occupational nurses with the intent of representing each department/shift | Format: -Had an individual meeting with research team to discuss responsibilities Training Resource: -Received a manual |
NP | NP | - Ongoing informal contact with participants -to use talking points to reinforce FYL lessons -provide social support |
| 18. Wilson et al., 2016 [27] FUEL Your Life |
Gender: NP Mean age: NP Mean education level: NP |
-Respected & trusted co-workers who were also participants in the programme | NP | 1-hour | Site coordinator [occupational nurse] served as a resource to health coaches | -Peer health coaches -providing basic information -answering simple questions -providing encouragement & support -referral to site coordinator & research team for complex issues |
| 19. Ockene et al., 2012 [28] | Gender: NP Mean age: NP Mean education level: NP |
-Spanish speaking - post high school education -some previous undergraduate education in nutrition -none were registered dietitians |
Content: -Extensive training in delivery of the intervention protocol -nutritional & exercise aspects of intervention -theoretical background -training in motivational counselling -group management skills Format: -led by a behavioural psychologist and a senior registered dietician |
NP | -Booster training sessions scheduled semi-annually | Delivered intervention/sessions |
| 20. Islam et al., 2014 [30] [Project RICE] |
Gender: NP Mean age: NP Mean education level: NP |
NP | Content and [some] Format] - The CHW supervisor participated in a two-part 105-hour core competency & curriculum based training [comprehensive skills training for CHW; disease prevention & management] -the CHW supervisor was trained on the delivery of the adapted curriculum -the CHW supervisor & study staff subsequently trained three additional study CHW on the study protocol, delivery & curriculum [Some] Content: -all study staff attended approximately 30 hours of additional training on mental health, motivational interviewing/basic action planning & other related issues |
Not clear | NP | Facilitated group sessions |
| 21. Thompson et al. 2015 [31] | Gender: NP Mean age: NP Mean education level: NP |
-previous training in obtaining blood pressure readings using an automatic cuff -one-time training session in diabetes and CVD -ability to speak and read Spanish -ability to attend one screening session -access to telephone |
Content: -one session on screening |
NP | NP | -risk screening -referral |
| 22. Oba et al., 2011 [32] | Gender: NP Mean age: NP Mean education level: NP |
-Recruited based on interest in developing a diabetes mellitus programme | NP | NP | NP | -Recruited people who were at risk for developing diabetes -ran programme -provided nutrition education -selected appropriate exercise types for fitness phase |
| 23. Balagopal et al., 2012 [33] | Gender: NP Mean age: NP Mean education level: 60% had a college degree |
-At least a high school diploma -an interest in health care & community -willingness to learn -leadership qualities -bilingual (English & Gujarati) -previous healthcare or community experience -a strong commitment to work in the community |
Content: -4 weeks of structured training on an existing diabetes prevention & management curriculum -skill-based knowledge using hands-on training on vital signs, dietary intake, anthropometrics & health screening -knowledge on diabetes & its risk factors & complications -ethics & confidentiality of dealing with human subjects & survey dissemination Format: -training provided by an expert & multidisciplinary team, i.e. a registered dietician, a certified health educator, a public health practitioner, an endocrinologist, a sanitation specialist, a general practitioner & an internal medicine specialist |
4 weeks | NP | -Change agents to provide health education -serve as community advocates -collect data for the study |
| 24. O’Brien et al., 2015 [34] | Gender: NP Mean age: NP Mean education level: High school education |
-Dedication to the community -natural leadership skills -worked with the investigative team for 8 years -conducted several group-based lifestyle interventions |
Format: -Training from local & national diabetes experts |
18 hours | -Supervision & feedback before implementing the study protocol -all sessions were attended by an author |
Delivered sessions |
| 25. Benyshek et al., 2014 [35] [The Life in BALANCE pilot study] |
Gender: NP Mean age: NP Mean education level: NP |
NP | Format: Centralised training that included: -required reading -instructional video tapes -observation of trained personnel -audio/videotaped practice sessions -resource core review |
NP | NP | Delivered core curriculum and conducted follow-up Native lifestyle coaches |
| 26. Philis-Tsimikas et al., 2014 [36] | Gender: NP Mean age: NP Mean education level: NP |
NP | Content: In-depth standardised training in the curriculum (Dulce Mothers) & group facilitation methods: -disease content -group management dynamics -motivational interviewing skills -Health Insurance Portability & Accountability Act (HIPPA) -and other health workplace regulations Format: -trained by a lead health educator with at least 5 years’ experience in leading peer-led interventions |
40 hours | Supported by a multi-disciplinary team | Teach/deliver sessions |
| 27. Cherrington et al., 2015 [37] | Gender: NP Mean age: NP Mean education level: NP |
-bilingual, bicultural -good personal communication skills -a driver’s license -a desire to work in the community |
Content: -topics related to each session -the principles of Motivational Interviewing Format: -role-playing & practice sessions |
NP | NP | -delivered group & individual sessions |
| 28. Ruggiero et al., 2011 [38] | Gender: NP Mean age: NP Mean education level: NP |
-delivered a 1-yr Vanguard group prior to this study | Content: -group leadership skills -diabetes self-care -behaviour change & psychosocial topics -physical activity -healthy eating |
NP | Ongoing supervision & support in delivering the programme | -served as a Healthy Life Coach |
| 29. Treadwell et al., 2010 [39] | Gender: NP Mean age: NP Mean education level: NP |
NP | Content: Trained to: -to recruit participants -implement the obesity & diabetes prevention intervention -facilitate exercise & healthy lifestyle activities -connect men with primary health care providers & other supportive community resources |
NP | NP | -to recruit participants -data collection -implement the obesity & diabetes prevention intervention -facilitate exercise & healthy lifestyle activities -connect men with primary healthcare providers & other supportive community resources |
| 30. Cadzow et al., 2013 [40] | Gender: 12 females, 1 male Mean age: >35–65 years Mean education level: -Two-thirds had a 4-yr college degree -one some training/coursework beyond degree -one high school diploma -one with some college training, but not completed a formal degree |
-recruited through block clubs, tenant council meetings, a community health centre & a woman’s church group -upon recruitment, prior to acceptance into training programme a Baseline survey including demographics & a list of other types of leadership activities in which they had participated |
Content: -Refining Leadership Skills -Cultural Broker Skill Development & Cultural Diversity Awareness -Diabetes 101 -Health Literacy & the State of Ageing & Health in America -Methods of Cultural Health Brokering [the curriculum was approved for Continuing Professional Education credit at Buffalo State College] -conducting & evaluating community conversations |
4 weeks | NP | -held five community conversations, reaching 700 community members -established eight diabetes resource libraries |
| 31. Cadzow et al., 2014 [41] | Gender: 12 females, 1 male Mean age: -35->65 years Mean education level: at least a 4-yr degree |
-community members who were active in various area community organisations were recruited | Content: -addressed skills & methods in leadership -cultural health brokering -basic diabetes knowledge -health literacy |
20 hours of formal training, during one week | Met monthly with programme leaders & evaluators | Neighbourhood Health Talkers -led community conversations -established a resource library |
| 32. Staten et al., 2005 [42] [Pasos Adelante/ “Steps Forward”] |
Gender: 10 females, 1 male Mean age: NP Mean education level: NP |
-Recruitment of CHW/promotoras was left to the contracted agencies | Format: -Nine of the promotoras were involved in curriculum design & received ± 6hrs. of manual training -the two additional promotoras were trained individually by other promoters with technical assistance from programme personnel -in addition, many promotoras attended week long training at a CHW conference -also, the promotoras attended a variety training on diabetes |
6 hours [extra training not accounted for] |
Additional training was conducted when necessary throughout the programme | Facilitated programme -Led the sessions working in pairs -provided feedback on sessions |
| 33. Staten et al., 2012 [29] [Pasos Adelante/ “Steps Forward”] |
Gender: Female (3) Mean age: NP Mean education level: NP |
-Lived in community for 20–35 years -two of the three promotoras facilitated the Pasos Adelante 1-yr pilot programme in their community |
Content and Format: -Su Corazon, Su Vida curriculum at a national conference |
One week, half day training | Ongoing training included quarterly refresher training & local & national conferences | Facilitated sessions |
| 34. Sosa et al., 2013 [43] | Gender: NP Mean age: NP Mean education level: NP |
-Recruited from a CHW certification programme | Content: -to communicate with participants -to provide health education and support -basic nutrition and physical activity knowledge -nutrition counselling skills -nutrition education -behaviour change skills -physical activity skills -health knowledge on obesity, diabetes & CVD -healthy eating and physical activity impacts on health -ethical issues in health promotion -small group dynamics/management -presentation skills -protecting human subjects -helping participants use implementation tools -leading physical activity lessons -leading cooking demonstrations -ensuring food safety -implementing health and nutrition lessons |
-30 hours training -6 weeks participation in condensed version of implementation |
-weekly staff meetings to provide ongoing training & support | Delivered intervention/sessions |
| 35. Kousar et al., 2015 [44] | Gender: NP Mean age: NP Mean education level: NP |
-part of communities, i.e. hold language & cultural knowledge -have potential to make lifestyle changes -have existing qualifications/experience in the education, social welfare/health sectors from their country of origin, beyond the category of “lay” or “peer” |
Content: -diabetes complications -prevention & management -Day 1: Understanding of diabetes–types of diabetes; diabetes complications; prevention; the global diabetes epidemic; the role and skills of training & education necessary to become a socially active member of community; info on health professionals related to diabetes -Day 2: Understanding diet & nutrition–barriers to healthy eating; food labels; healthy food shopping; the healthy food pyramid -Day 3 –mental health & well-being in diabetes–how to collect anthropometric indicators of diabetes risk factors–administer diabetes knowledge assessments \7 dietary recall questionnaires -Day 4 –Report day–feedback evaluation by each CHV Format: -Interactive education & training workshops -presentations, guided activities & group discussions |
4 days | NA | NA |
| 36. Coppell et al., 2009 [45] | Gender: NP Mean age: NP Mean education level: NP |
NP | NP | NP | NP | -not clear -recruitment |
| 37.Schulz et al., 2005 [46] | Gender: NP Mean age: NP Mean education level: NP |
[existing skills] -experience as community organisers -personal trainers -youth leaders -caregivers |
Content: -detailed information about diabetes & the role of diet & physical activity -nutrition label reading -recipe modification -strategies for working with communities to address diabetes |
2 weeks | Support from project coordinator & members of steering committee | HEED advocates developed: -activities to promote healthy diets & physical activity -a weekly walking club for senior citizens -events focused on diabetes awareness & prevention -cooking demonstrations -monthly fruit & veg market |
| 38. Cohen & Ingam, 2005 [47] 39. Teufel-Shone, Drummond & Rawiel, 2005 [48] 40.Reinschmidt et al., 2010 [49] |
Gender: NP Mean age: NP Mean education level: NP |
-previous experience and training in community outreach services -they were uniquely familiar with the curriculum as they were involved in its development and adaption |
Content: introduction to the overall flow and curriculum format; and instruction in the use of educational materials Format: role play, practicing delivery and co-worker critique of delivery styles Resources: instructional manual provides an overview of the goals and format of the programme, a description of objectives, an outline of the activities and supplies needed for each contact point |
One day | -carrying out project components -involved in the development of family curriculum component -grassroots leadership Not part of their duties: -participated in food demonstrations -collecting signatures for a petition to create a community park in another area -implemented the programme Adaption 1: -conducted home visits -implemented educational classes Adaption 2: -recruitment and consenting -scheduling of measurement appointments -family curriculum implementation -reminder calls -attendance documentation -follow-up support |
|
| 41. Whittemore et al., 2013 [50] | Gender: NP Mean age: NP Mean education level: NP |
NP | NP | -4-hour training | Ongoing supervision by nurses and PI of study | -recruitment -class set up -follow-up |
*NA–Not applicable
*NP–Not Provided
Results
Overview of the searches
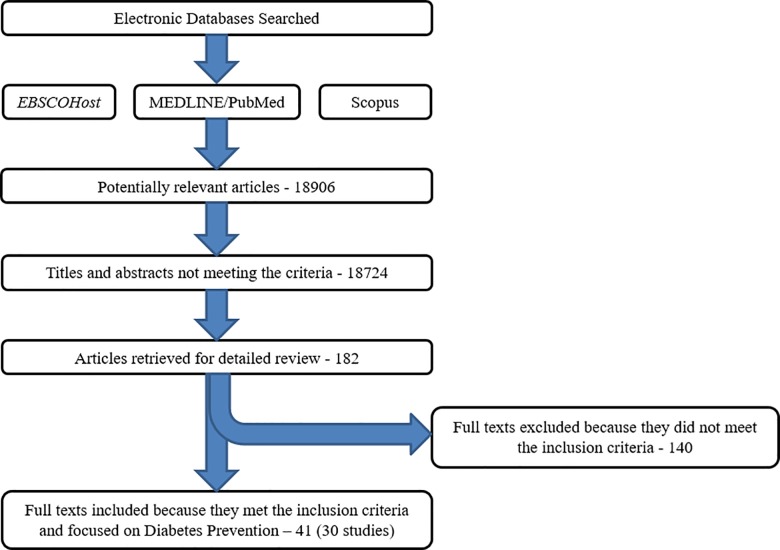
Database searches identified 18906 entries; after removing duplicates and screening titles and abstracts, 182 publications were selected for further full-text evaluation (Fig 1). Forty one papers fulfilled the inclusion criteria and form the basis of this review. These 41 papers reported on 30 studies with companion papers comprising protocol papers, pilot studies, cost analyses and process evaluation papers.
Fig 1. Flow diagram of retrieved studies.
Study designs and geographic locations
Most studies (24) were conducted in the US, while two studies each were conducted in India [23, 33] and New Zealand [24, 45], and one each in Thailand [32] and Australia [44]. None of the publications originated from Africa.
The 30 primary studies included 10 RCT [10, 13, 14, 19–24, 27], 14 quasi-experimental/comparative observational studies [25, 28–39], three studies with a one-group pre- test/post-test or post-test only design [41, 43, 44], two case studies [46, 47] and a study each with an interrupted time-series prevalence survey design [45], and a mixed method embedded design [50].
Study settings, participants and interventions
The sample sizes varied widely from 20 participants in a single community to 2369 participants in 46 communities. Intervention settings varied but were mainly community-based such as churches, homes and community centres. A study each was conducted at senior centres [10, 11] and worksites [25–27].
Studies were conducted mainly in minority populations such as Latinas/Hispanics [13, 20–22, 28, 29, 34, 36–38, 42, 43, 47] and African Americans in the US [39, 40], the Maori in New Zealand, and in people without “easy” access to healthcare services [24, 45]. Most studies (n = 22) included 18–79 year old men and women, with a female preponderance. Two studies included men only [31, 39], while six targeted women only [13, 22, 34, 36, 37, 43].
The diabetes prevention interventions and methods of delivery were culturally adapted to the target population. Most of the DPPs were lifestyle interventions; however, one study focused on diabetes education only [40, 41] and another on diabetes risk screening [31].
Profile of community health workers
CHWs were generally from the local study community and shared the same race/ethnic and language backgrounds as the participants. Two exceptions were a worksite-specific study which made use of peer coaches [25–27] and a senior centre study of whom some of the lay health educators or coaches were staff members [12]. Nevertheless, these CHWs were likely very familiar with the communities under study. Language was a specified criteria for studies conducted in Hispanic [13, 28, 31] and Korean- American [19] communities in the US, Aborigines in Australia [44], and in Gujarat, India [33].
Most of the publications included in the review did not provide detailed information on CHW characteristics. Gender, age and education level were reported in only eight [12, 17, 29, 40–44], six [12, 17, 40, 41, 43, 44] and seven [12, 17, 22, 33, 34, 40, 41] studies, respectively. CHWs were mostly women aged between 20 and 65 years, but usually older than 35 years. Education level varied from high school education to non-health related college degrees [12, 17, 22, 33, 34] with CHWs in Buffalo City, US even having post-graduate qualifications [40, 41].
The qualifications and work experience of CHWs varied widely across studies. Qualifications included: 1) completing only high-school [13, 22, 33, 34] or 2) a CHW-certification programme [43] 3) previous training on measuring automated blood pressure (BP) [31] 4) and 5) post-high school education and some undergraduate education in nutrition [28]. Instead of qualifications, other studies focused on work experience as a CHW [22], prior or current experience in working in various areas of health [51], experience as a community organiser, personal trainer or caregiver [41, 46, 48], or having worked with the investigative team previously [34], as well as being involved in developing and adapting programme curriculum [48]. A qualification or experience in the education, social welfare or health sectors was a pre-requisite in an Australian study [44].
A single study used CHWs with well-controlled diabetes and a history of healthy eating, regular physical activity, weight loss and group leadership experience [14, 18]. In contrast, a study in Thailand recruited CHWs who were simply interested in developing a DPP [32]. Many studies emphasised soft skills in the selection of their CHWs. These included possessing leadership qualities [13, 33, 34, 40, 41], good communication skills and the ability to listen [37], and a dedication to the community [13, 34, 37].
Community health worker training
The duration of the training varied considerably among studies, from a single one-hour session [25, 27] to 40 hours [36], and even 100 hours or more [21, 22, 30]. Overall, the training was culturally sensitive and/or appropriate (Table 2). Topics covered included the importance of good nutrition [32, 43, 44] and the benefits of increased physical activity [14, 38, 43, 46]. Communication [23, 24] and leadership [38, 40, 41] skills to run group sessions, and motivational interviewing to facilitate behaviour change [19, 24, 28, 30, 36, 37] were also emphasised. Most studies utilised interactive training and role-playing to impart skills during the training sessions. Four studies did not describe CHW training [32, 45, 47, 50]. One study put specific emphasis on intervention fidelity/following study protocol [12].
Post-training support ranged from daily supervision to monthly meetings. These included ongoing supervision, monitoring and support [13, 14, 23, 38], weekly technical conference calls [10], weekly staff meeting [43], and monthly meetings with programme leaders and evaluators [41].
Some studies also provided continuous or booster training. These included ongoing training with quarterly refresher training sessions as well as local and national conference attendances [29, 42], biannual booster training sessions [21, 28] and a two-day refresher training mid-way through the intervention programme [23].
Community health worker responsibilities
As summarised in Table 2, most CHWs in these studies delivered the intervention activities, i.e. led or facilitated the group sessions. These included developing and organising activities to promote healthy diets and physical activity such as a weekly senior citizen walking club, diabetes awareness and prevention events, cooking demonstrations, and a monthly fruit and vegetable market [10, 11, 13–24, 28–30, 32–39, 42, 43, 47, 51]. In Buffalo City (US), CHWs led community “living diabetes well” conversations and established “diabetes resource libraries”, which provided information on diabetes, healthy living, healthcare providers, and recipe cards and cookbooks [40, 41]. CHWs linked African-American men with primary healthcare providers and other supportive community resources [39], and in migrant farmworkers screened and referred those at high risk for diabetes and cardiovascular disease (CVD) [31].
Three of the included studies, however, used occupational [27], homecare [50] and rural health nurses [45], instead of CHWs, to deliver the interventions. CHWs only recruited [45] and maintained regular contact with participants providing ongoing support and information [27], and set-up meeting venues and coordinated walking groups [50] in these studies.
CHWs also recruited programme participants in four of the studies where they led the interventions [21, 32, 39, 49] and provided follow-up support between the intervention programme/sessions in three studies [30, 35, 49]. Other CHW tasks included data collection [39] and entry [14, 17], and recording attendance [18, 49] and interactions between participants and project staff [23].
Diabetes prevention programme outcomes
Outcomes of the DPPs are reported in Table 1. Most studies (20) included a measure of adiposity such as weight or waist circumference with weight loss ranging from more than 7% of body weight [38] to modest weight loss of 1.1kg [28]. Unexpectedly, a study reported a significant difference between groups because of weight maintenance in the intervention group, but weight gain in the control group [27].
Eleven studies reported on biochemical outcomes. Blood glucose and insulin levels were measured in 10 studies; it was the primary outcome in six of these studies [14, 18, 22, 28–30, 33–35, 37, 39, 45]. Six studies reported significant improvements in glucose levels between intervention and control groups or post- and pre-intervention periods [16, 18, 28–30, 33]. For example, greater reductions were found in the intervention vs. the usual care groups (-4.3 mg/dL vs. -0.4 mg/dL) [16]), in individuals with impaired fasting glycaemia vs. normoglycaemia (-6.02 mg/dL vs. -1.3 mg/dL) [33], and at the study conclusion vs. during follow-up (-4.529mg/dL vs. 0.686 mg/dL) [29]. Statistically significant reductions in insulin (6.5 uU/ml vs. 2.7uU/ml) and insulin resistance (HOMA-IR) (1.9 vs. 0.8) in the intervention compared to the usual care groups were reported in only a single study [16]. Glycated haemoglobin (HbA1c) was measured in four studies [21, 28, 34, 36] with improvements noted in two studies on Hispanic communities [21]. One study reported a proportionate HbA1c reduction of 37.5% vs. 0.44% in the intervention compared with the delayed intervention group [21], while the other described an absolute reduction of 0.10% vs. 0.04% in the intervention compared to the usual care group in [28].
BP was measured in 13 studies [19, 22, 28–36, 39, 45] with improvements noted in eight. Four studies reported significant improvement in both systolic BP (SBP) and diastolic BP (DBP) with reductions of 3.2 mmHg to 13 mmHg for SBP and 2.3 mmHg to 5.1 mmHg for DBP [29, 30, 33, 36]. A single study each reported a 23% decrease in overall BP level [39], a 2.61 mmHg drop in SBP [32] and a 6.2 mmHg reduction in DBP [34].
Lipid levels were measured in nine studies [22, 28–30, 34–37, 45] with improvements found in five studies. Three studies each reported significant improvements in total cholesterol [29, 36, 37] and low-density lipoprotein cholesterol levels [34, 36, 37].
Nine studies reported on behavioural changes pertaining to greater physical activity levels with different variables assessed [19, 21, 22, 30, 36, 37, 39, 42, 48]. Significant improvements in physical activity were measured as 1) increases in physical activity between baseline and six months [30], and in particular vigorous activity [37], 2) increases in moderate and vigorous walking levels [42], 3) greater aerobic exercise, flexibility and strength [36], 4) increased fitness levels [39], and 5) better social interaction and greater confidence in performing physical activities [19].
Of the nine studies that assessed various food and dietary behaviours, six reported significant improvements. These dietary variables included general food behaviour [22, 42], consumption of sweetened beverages [48], and fruit and vegetable [30]; dietary fat intake [36], and caloric intake and proportion derived from protein sources [37].
Eight studies assessed knowledge on diabetes and/or CVD with all reporting significant improvements [19, 22, 30, 39, 41, 43, 44, 48]. Improved mental health outcomes were noted in two studies; the Personal Health Questionnaire (PHQ-2) and the Generalized Anxiety Disorder Scale (GAD-2) were used in a US Korean community [19] and the Patient Health Questionnaire (PHQ-8) in a US Hispanic population [37]. A single study that examined fatalistic and cultural diabetes beliefs, measured by the Power Fatalism Inventory, showed significant reductions in fatalistic beliefs about diabetes manageability and endorsement of culturally driven diabetes beliefs [36]. Although two studies collected data on quality of life outcomes, neither study reported these findings [14, 23].
Cost analyses of diabetes prevention programmes
Two studies, both from the US, conducted cost analyses for their DPPs [11, 18]. In the study conducted in senior centres, total estimated cost for the CHW delivered lifestyle intervention was $2731 per senior centre or $165 per participant or $45 per kilogram weight lost [11]. These costs were almost half those of a health professional delivered DPP which cost $300 per participant or $88 per kilogram lost [52]. Direct medical costs per participant in the HELP-PD lifestyle intervention programme conducted over two years were $850 compared to $2361 for the first two years in the original DPP conducted in the US [18].
The effect of community health workers on programme outcome
Studies did not specifically compare the use of CHWs vs. health professionals on programme outcomes, except for Thompson et al. [31] who found that CHWs perform as well as registered nurses in the use of non-invasive risk screening tools. Therefore, it is difficult to quantify the specific advantages of using CHWs to implement DPPs. However, DPPs that targeted vulnerable/underserved communities highlighted the importance of CHWs in contributing to their acceptability and appropriateness (Table 3) [21, 22, 24, 30, 35]. Additionally, studies have also emphasised the importance of community participation per se as a major contributor to programme effectiveness [32, 33, 38, 46–49]. The shared culture and language between CHWs and participants likely contributed to better programme implementation and outcomes [19, 21, 30, 36, 44]. In essence, using CHWs in DPPs that target culturally and linguistically diverse groups seem to be a credible strategy [44].
Table 3. Direct CHW effect/contribution as recognised by study authors.
| Study | CHW impact |
|---|---|
| West et al., 2011 [10] | “Lay health workers offers a promising vehicle for translation of evidenced-based obesity treatment in underserved areas” |
| Krukowski et al., 2013 [11] Krukowski et al., 2013 [12] |
“A LHE [lay health educator] DPP translation in senior centers is effective in achieving weight loss at low cost and offers promise for the dissemination of this evidenced-based intervention” “Training LHE’s to disseminate evidenced-based interventions holds great promise for improving public health and access to effective care, particularly in medically underserved areas” |
| Katula et al., 2013 [17] | “A DPP administered through an existing community-based system and delivered by CHWs is effective at inducing significant long-term reductions in metabolic indicators and adiposity” |
| Islam et al., 2013 [19] | “…CHWs can facilitate support by serving as a bridge to the health care system and proving culturally- and linguistically- tailored health education”. …many participants felt connected to, and appreciative of the CHWs’ efforts, suggesting that CHWs serve a unique role in health promotion effort” |
| Duggan et al., 2014 [21] | “Bilingual CHWs removed linguistic barriers” |
| Koniak-Griffin et al., 2014 [22] | “Findings of this RCT support the feasibility and positive outcomes of implementing a promotora-facilitated Life Behaviour intervention in the community with overweight/obese Latinas” |
| Simmons et al., 2008 [24] | “Intensively treated participants would have had one or more unrecorded MCHW [Maori CHW] encounters and these may have had a significant effect” “The MCHW intervention was seen as key to the downstream intervention activities” |
| Staten et al., 2005 [42] | “The Pasos Adelante Program has demonstrated that an educational curriculum in conjunction with the support of promotoras can motivate people to healthy lifestyle behaviors” |
| Islam et al., 2014 [30] | “Participants reported positive feedback about the program and about the CHWs, particularly regarding the cultural congruence of CHWs and the strong connectedness of the intervention with community resources and cultural and religious norms and values” |
| Oba et al., 2011 [32] | “The research found that the health volunteers in each community were important for conducting the health promotion activities in their own villages” |
| Balagopal et al., 2012 [33] | “…that CHWs can provide advice on lifestyle modification and improve awareness of diabetes and CVD similar to allied health professionals in earlier studies… The CHWs were able to successfully empower the women to speak up at their meetings and instil them with confidence in their decision making abilities as related to their health and well-being. Using CHWs strengthened the links among project personnel, the community and existing community networks” |
| Philis-Tsimikas et al., 2014 [36] | “Participants appreciated the convenient community location, social support received from other participants and the promotoras” |
| Cherrington et al., 2015 [37] | “…peer delivered interventions may be particularly well-suited to the needs of immigrant women in newly emerging Latino communities” |
| Ruggiero et al., 2011 [38] | “For this project, the training, quality, professionalism and commitment of the CHWs that worked with program participants had an instrumental impact on high rates of retention and engagement of participants with project activities” |
| Sosa et al., 2013 [43] | “…evaluation results showed that promotoras were capable to deliver and retain participants in a lifestyle intervention program” |
| Kousar et al., 2015 [44] | “Here we confirm that CHV [community health volunteers] represent an effective tool for health promotion within culturally and linguistically diverse communities and have the capacity to incorporate evidence-based collection as part of their health education” |
| Cadzow et al., 2013 [40] | “Participants not only developed proficiency in discussing this important issue with their neighbors and peers, they also made important lifestyle changes that demonstrated their commitment to the cause and project” “The Neighborhood Health Talkers’ commitment to the program and embeddedness in their own communities resulted in an unpredicted reach to community residence” |
| Thompson et al., 2014 [31] | “This quasi-experimental study supports the hypothesis that Latino CHWs can use non-invasive diabetes and CVD screening tools with similar accuracy as a registered nurse” |
| Coppell et al., 2009 [45] | “A key factor underpinning the program was early involvement of CHWs, community members and local organizations and the use of local resources and talents so that the program would become embedded into everyday community life and sustainable in the long term. |
| Cohen & Ingram, 2005 [47] | “The curriculum for the family component, for example, was developed collaboratively between academics and promotoras who had never worked together in the past” |
| Whittemore et al., 2014 [50] | “…better understanding of the role of the CHW in the delivery of health programs is needed” |
Discussion
The current review provides evidence from 33 studies of the increasing involvement of CHWs in implementing DPPs. The majority of the studies, however, were undertaken in high income countries, particularly the US. Only three studies were conducted in developing countries, where the incorporation of CHWs in resource-limited settings is likely to have a greater impact.
Most studies targeted the underserved minority such as African-American and Hispanic communities in the US, Aborigines in Australia and the Maori people in New Zealand [24]. The same was true of developing regions where rural communities were the focus in India [23, 33] and Thailand [32]. DPPs that target minority and other vulnerable groups are likely suited to use CHWs who share a common culture, belief system (tradition), and language with the programme participants. This accords with The Centers for Disease Control and Prevention’s Policy Brief (2015) which produce strong evidence for the use of trained lay people i.e. CHWs as a best practice for reducing CVD risk and improving outcomes in high-risk minority populations [53]. Unfortunately, the existing evidence is unclear, inconsistent and insufficient to inform the scaling up of DPPs in diverse settings using CHWs. The complexity of the programmes precluded attributing any specific benefit to the use of CHWs. Similar to these findings, Shah and colleagues noted that despite the large body of literature on CHWs and diabetes care, the wide range of CHW roles and differing outcomes made it difficult to draw conclusions on their overall effectiveness [5].
The outcomes of interest in the included studies were mostly intermediate, such as changes in behaviour or body weight, with no study reporting diabetes incidence. Nevertheless, CHWs are regarded as adding value to programmes by fulfilling a gap/an unmet need [54]. CHW-led interventions are optimally suited to programmes where there is greater community involvement, as shown by a number of studies in this review, which used community-based participatory research approaches [19, 20, 22, 30, 32, 33, 35, 37, 38, 46–48].
The profile, scope of roles played, and training received by CHWs varied substantially across programmes. Most DPPs provided information on the training/curriculum to varying degrees [32, 45, 47, 50]. The duration of training varied significantly with shorter training sessions generally scheduled in programmes with fewer CHW responsibilities. While a systematic review reported that the performance of CHWs might improve with regular supervision and continuous training, an optimal model was not suggested [55]. Additionally, CHWs would benefit from clearly defined roles and clear processes for communication [55]. Guidelines that describe the potential roles of CHWs, the appropriate training required for each task/role and the type of programmes that would benefit from CHW involvement may be useful. While such guidelines may need to be adapted for different populations, they may encourage greater utilisation of CHWs in in appropriate healthcare programmes, including DPPs, and lead to better outcomes.
The frequency and duration of the DPP interventions varied, with higher versus lower intensity programmes having the greater impact. For example, CHWs in the HELP-PD programme delivered the intervention sessions, which comprised weekly group sessions for six months, and a monthly session for the following 18 months [16]. This study achieved significant improvements in blood glucose and insulin levels, insulin resistance, weight and BMI with the effects sustained over a two-year period [15–17]. Identifying the ideal programme intensity and duration may be useful/of value for optimal outcomes; however, this may possibly vary depending on the outcomes targeted. In addition, longer-term studies are required to ascertain the need to provide intermittent support beyond the 2-year period, which was the maximum duration of the studies included in this review.
The high concentration of studies from developed countries, especially the US, limits the generalisability of our findings. However, most populations studied were underserved or minority communities, which may be of relevance to developing region settings. The inclusion of only published studies in English language in this review may have missed lessons being learnt from potential ongoing CHW-led DPPs, particularly from developing regions, or studies published in other languages. Additional information was not obtained from the study authors to provide greater insight on CHW education, training, experience and supervision and attrition rates. Therefore, the potential for publication bias is evident in this review.
Conclusions
In view of the labour-intensive nature of community-based healthcare programmes, particularly DPPs, and the high cost of professional healthcare staff, pragmatic cost-effective solutions are required for optimal outcomes. The utilisation of adequately trained CHWs with ongoing supervision to perform clearly defined tasks is likely to be most beneficial, as noted in a World Health Organization report on the state of evidence of CHW programmes, “…they must be carefully selected, appropriately trained and–very important–adequately and continuously supported” [3]. In addition to the aforementioned, the success of CHW-led programmes lies in the commonalities such as language, culture and tradition shared between the CHWs and participants. These commonalities facilitate communication and dialogue, which is crucial, and may play a key role in the success of such programmes. However, considering the complexity of DPPs and the diverse roles played by CHWs, it is difficult to disentangle the specific contribution of CHWs to these programmes. Nevertheless, developing guidelines for potential CHW roles and determining the appropriate level of training required may help identify the optimal CHW contribution to DPPs, which is currently lacking in the literature. Furthermore, this may perhaps encourage the wider uptake of CHW-led DPPs and lead to the development of better programmes.
Supporting information
(DOCX)
Acknowledgments
The authors are pleased to acknowledge Ms Lorraine Moses (LM) for her contribution to this review [checking the summary tables against the articles]. The electronic search was made possible by the South African Medical Research Council’s Online Library [databases].
Data Availability
All relevant data are within the paper.
Funding Statement
Study funded by the South African Medical Research Council, and the South African National Research Foundation, under the Thuthuka Funding Instrument (Reference: TTK160517165315). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Aziz Z, Absetz P, Oldroyd J, Pronk NP, Oldenburg B. A systematic review of real-world diabetes prevention programs: learnings from the last 15 years. Implementation science: IS. 2015;10:172 Epub 2015/12/17. doi: 10.1186/s13012-015-0354-6 ; PubMed Central PMCID: PMCPmc4681022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabetic medicine: a journal of the British Diabetic Association. 2006;23(5):544–56. Epub 2006/05/10. doi: 10.1111/j.1464-5491.2006.01845.x . [DOI] [PubMed] [Google Scholar]
- 3.Lehmann U, Sanders D. Community health workers: What do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. Geneva: World Health Organization Evidence and Information for Policy DoHRfH; 2007. [Google Scholar]
- 4.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public health nursing (Boston, Mass). 2002;19(1):11–20. Epub 2002/02/14. . [DOI] [PubMed] [Google Scholar]
- 5.Shah M, Kaselitz E, Heisler M. The Role of Community Health Workers in Diabetes: Update on Current Literature. Current diabetes reports. 2013;13(2):163–71. doi: 10.1007/s11892-012-0359-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aponte J. Diabetes Training for Community Health Workers. Journal of community medicine & health education. 2015;5(6):378 doi: 10.4172/2161-0711.1000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenthal EL, Brownstein JN, Rush CH, Hirsch GR, Willaert AM, Scott JR, et al. Community health workers: part of the solution. Health affairs (Project Hope). 2010;29(7):1338–42. Epub 2010/07/08. doi: 10.1377/hlthaff.2010.0081 . [DOI] [PubMed] [Google Scholar]
- 8.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health affairs (Project Hope). 2012;31(1):67–75. Epub 2012/01/11. doi: 10.1377/hlthaff.2011.1009 . [DOI] [PubMed] [Google Scholar]
- 9.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed). 2015;349:g7647 Epub 2015/01/04. doi: 10.1136/bmj.g7647 . [DOI] [PubMed] [Google Scholar]
- 10.West DS, Bursac Z, Cornell CE, Felix HC, Fausett JK, Krukowski RA, et al. Lay health educators translate a weight-loss intervention in senior centers: a randomized controlled trial. American journal of preventive medicine. 2011;41(4):385–91. Epub 2011/10/04. doi: 10.1016/j.amepre.2011.06.041 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krukowski RA, Pope RA, Love S, Lensing S, Felix HC, Prewitt TE, et al. Examination of costs for a lay health educator-delivered translation of the Diabetes Prevention Program in senior centers. Preventive medicine. 2013;57(4):400–2. Epub 2013/07/09. doi: 10.1016/j.ypmed.2013.06.027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krukowski RA, Lensing S, Love S, Prewitt TE, Adams B, Cornell CE, et al. Training of Lay Health Educators to Implement an Evidence-based Behavioral Weight Loss Intervention in Rural Senior Centers. The Gerontologist. 2013;53(1):162–71. doi: 10.1093/geront/gns094 [DOI] [PubMed] [Google Scholar]
- 13.Perez A, Alos VA, Scanlan A, Maia CM, Davey A, Whitaker RC, et al. The rationale, design, and baseline characteristics of PREVENT-DM: A community-based comparative effectiveness trial of lifestyle intervention and metformin among Latinas with prediabetes. Contemporary clinical trials. 2015;45(Pt B):320–7. Epub 2015/11/26. doi: 10.1016/j.cct.2015.10.011 ; PubMed Central PMCID: PMCPmc4674352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katula JA, Vitolins MZ, Rosenberger EL, Blackwell C, Espeland MA, Lawlor MS, et al. Healthy Living Partnerships to Prevent Diabetes (HELP PD): design and methods. Contemporary clinical trials. 2010;31(1):71–81. Epub 2009/09/18. doi: 10.1016/j.cct.2009.09.002 ; PubMed Central PMCID: PMCPmc2818212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blackwell CS, Foster KA, Isom S, Katula JA, Vitolins MZ, Rosenberger EL, et al. Healthy Living Partnerships to Prevent Diabetes: recruitment and baseline characteristics. Contemporary clinical trials. 2011;32(1):40–9. Epub 2010/10/27. doi: 10.1016/j.cct.2010.10.006 ; PubMed Central PMCID: PMCPmc3005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katula JA, Vitolins MZ, Rosenberger EL, Blackwell CS, Morgan TM, Lawlor MS, et al. One-year results of a community-based translation of the Diabetes Prevention Program: Healthy-Living Partnerships to Prevent Diabetes (HELP PD) Project. Diabetes care. 2011;34(7):1451–7. Epub 2011/05/20. doi: 10.2337/dc10-2115 ; PubMed Central PMCID: PMCPmc3120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katula JA, Vitolins MZ, Morgan TM, Lawlor MS, Blackwell CS, Isom SP, et al. The Healthy Living Partnerships to Prevent Diabetes study: 2-year outcomes of a randomized controlled trial. American journal of preventive medicine. 2013;44(4 Suppl 4):S324–32. Epub 2013/03/27. doi: 10.1016/j.amepre.2012.12.015 ; PubMed Central PMCID: PMCPmc3731757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lawlor MS, Blackwell CS, Isom SP, Katula JA, Vitolins MZ, Morgan TM, et al. Cost of a group translation of the Diabetes Prevention Program: Healthy Living Partnerships to Prevent Diabetes. American journal of preventive medicine. 2013;44(4 Suppl 4):S381–9. Epub 2013/03/27. doi: 10.1016/j.amepre.2012.12.016 ; PubMed Central PMCID: PMCPmc3839056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Islam NS, Zanowiak JM, Wyatt LC, Chun K, Lee L, Kwon SC, et al. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. Journal of community health. 2013;38(6):1030–41. Epub 2013/07/03. doi: 10.1007/s10900-013-9711-z ; PubMed Central PMCID: PMCPmc3964609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horowitz CR, Eckhardt S, Talavera S, Goytia C, Lorig K. Effectively translating diabetes prevention: a successful model in a historically underserved community. Translational behavioral medicine. 2011;1(3):443–52. Epub 2011/12/23. doi: 10.1007/s13142-011-0067-6 ; PubMed Central PMCID: PMCPmc3242468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duggan C, Carosso E, Mariscal N, Islas I, Ibarra G, Holte S, et al. Diabetes prevention in Hispanics: report from a randomized controlled trial. Preventing chronic disease. 2014;11:E28 Epub 2014/03/01. doi: 10.5888/pcd11.130119 ; PubMed Central PMCID: PMCPmc3938962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koniak-Griffin D, Brecht ML, Takayanagi S, Villegas J, Melendrez M, Balcazar H. A community health worker-led lifestyle behavior intervention for Latina (Hispanic) women: feasibility and outcomes of a randomized controlled trial. International journal of nursing studies. 2015;52(1):75–87. Epub 2014/10/14. doi: 10.1016/j.ijnurstu.2014.09.005 ; PubMed Central PMCID: PMCPmc4277872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sathish T, Williams ED, Pasricha N, Absetz P, Lorgelly P, Wolfe R, et al. Cluster randomised controlled trial of a peer-led lifestyle intervention program: study protocol for the Kerala diabetes prevention program. BMC public health. 2013;13:1035 Epub 2013/11/05. doi: 10.1186/1471-2458-13-1035 ; PubMed Central PMCID: PMCPmc3937241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simmons D, Rush E, Crook N. Development and piloting of a community health worker-based intervention for the prevention of diabetes among New Zealand Maori in Te Wai o Rona: Diabetes Prevention Strategy. Public health nutrition. 2008;11(12):1318–25. Epub 2008/06/13. doi: 10.1017/S1368980008002711 [DOI] [PubMed] [Google Scholar]
- 25.DeJoy DM, Padilla HM, Wilson MG, Vandenberg RJ, Davis MA. Worksite translation of the Diabetes Prevention Program: formative research and pilot study results from FUEL Your Life. Health promotion practice. 2013;14(4):506–13. Epub 2012/10/24. doi: 10.1177/1524839912461014 . [DOI] [PubMed] [Google Scholar]
- 26.Brace AM, Padilla HM, DeJoy DM, Wilson MG, Vandenberg RJ, Davis M. Applying RE-AIM to the evaluation of FUEL Your Life: a worksite translation of DPP. Health promotion practice. 2015;16(1):28–35. Epub 2014/06/20. doi: 10.1177/1524839914539329 . [DOI] [PubMed] [Google Scholar]
- 27.Wilson MG, DeJoy DM, Vandenberg R, Padilla H, Davis M. FUEL Your Life: A Translation of the Diabetes Prevention Program to Worksites. American journal of health promotion: AJHP. 2016;30(3):188–97. Epub 2015/01/24. doi: 10.4278/ajhp.130411-QUAN-169 . [DOI] [PubMed] [Google Scholar]
- 28.Ockene IS, Tellez TL, Rosal MC, Reed GW, Mordes J, Merriam PA, et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. American journal of public health. 2012;102(2):336–42. Epub 2012/03/07. doi: 10.2105/AJPH.2011.300357 ; PubMed Central PMCID: PMCPmc3483988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Staten LK, Cutshaw CA, Davidson C, Reinschmidt K, Stewart R, Roe DJ. Effectiveness of the Pasos Adelante chronic disease prevention and control program in a US-Mexico border community, 2005–2008. Preventing chronic disease. 2012;9:E08 Epub 2011/12/17. ; PubMed Central PMCID: PMCPmc3277389. [PMC free article] [PubMed] [Google Scholar]
- 30.Islam NS, Zanowiak JM, Wyatt LC, Kavathe R, Singh H, Kwon SC, et al. Diabetes prevention in the New York City Sikh Asian Indian community: a pilot study. International journal of environmental research and public health. 2014;11(5):5462–86. Epub 2014/05/24. doi: 10.3390/ijerph110505462 ; PubMed Central PMCID: PMCPmc4053907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thompson RH, Snyder AE, Burt DR, Greiner DS, Luna MA. Risk screening for cardiovascular disease and diabetes in Latino migrant farmworkers: a role for the community health worker. Journal of community health. 2015;40(1):131–7. Epub 2014/07/06. doi: 10.1007/s10900-014-9910-2 . [DOI] [PubMed] [Google Scholar]
- 32.Oba N, McCaffrey R, Choonhapran P, Chutug P, Rueangram S. Development of a community participation program for diabetes mellitus prevention in a primary care unit, Thailand. Nursing & health sciences. 2011;13(3):352–9. Epub 2011/08/05. doi: 10.1111/j.1442-2018.2011.00627.x [DOI] [PubMed] [Google Scholar]
- 33.Balagopal P, Kamalamma N, Patel TG, Misra R. A community-based participatory diabetes prevention and management intervention in rural India using community health workers. The Diabetes educator. 2012;38(6):822–34. Epub 2012/10/04. doi: 10.1177/0145721712459890 . [DOI] [PubMed] [Google Scholar]
- 34.O'Brien MJ, Perez A, Alos VA, Whitaker RC, Ciolino JD, Mohr DC, et al. The feasibility, acceptability, and preliminary effectiveness of a Promotora-Led Diabetes Prevention Program (PL-DPP) in Latinas: a pilot study. The Diabetes educator. 2015;41(4):485–94. Epub 2015/05/30. doi: 10.1177/0145721715586576 ; PubMed Central PMCID: PMCPmc4617318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benyshek DC, Chino M, Dodge-Francis C, Begay TO, Jin H, Giordano C. Prevention of type 2 diabetes in urban American Indian/Alaskan Native communities: The Life in BALANCE pilot study. Journal of diabetes mellitus. 2013;3(4):184–91. Epub 2014/03/19. doi: 10.4236/jdm.2013.34028 ; PubMed Central PMCID: PMCPmc3952556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Philis-Tsimikas A, Fortmann AL, Dharkar-Surber S, Euyoque JA, Ruiz M, Schultz J, et al. Dulce Mothers: an intervention to reduce diabetes and cardiovascular risk in Latinas after gestational diabetes. Translational behavioral medicine. 2014;4(1):18–25. Epub 2014/03/22. doi: 10.1007/s13142-014-0253-4 ; PubMed Central PMCID: PMCPmc3958598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cherrington AL, Willig AL, Agne AA, Fowler MC, Dutton GR, Scarinci IC. Development of a theory-based, peer support intervention to promote weight loss among Latina immigrants. BMC obesity. 2015;2:17 Epub 2015/07/29. doi: 10.1186/s40608-015-0047-3 ; PubMed Central PMCID: PMCPmc4511020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ruggiero L, Oros S, Choi YK. Community-based translation of the diabetes prevention program's lifestyle intervention in an underserved Latino population. The Diabetes educator. 2011;37(4):564–72. Epub 2011/06/22. doi: 10.1177/0145721711411107 . [DOI] [PubMed] [Google Scholar]
- 39.Treadwell H, Holden K, Hubbard R, Harper F, Wright F, Ferrer M, et al. Addressing obesity and diabetes among African American men: examination of a community-based model of prevention. Journal of the National Medical Association. 2010;102(9):794–802. Epub 2010/10/07. . [DOI] [PubMed] [Google Scholar]
- 40.Cadzow RB, Craig M, Rowe J, Kahn LS. Transforming community members into diabetes cultural health brokers: the Neighborhood Health Talker project. The Diabetes educator. 2013;39(1):100–8. Epub 2012/11/15. doi: 10.1177/0145721712465342 [DOI] [PubMed] [Google Scholar]
- 41.Cadzow RB, Vest BM, Craig M, Rowe JS, Kahn LS. "Living well with diabetes": evaluation of a pilot program to promote diabetes prevention and self-management in a medically underserved community. Diabetes spectrum: a publication of the American Diabetes Association. 2014;27(4):246–55. Epub 2015/02/04. doi: 10.2337/diaspect.27.4.246 ; PubMed Central PMCID: PMCPmc4231932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Staten LK, Scheu LL, Bronson D, Pena V, Elenes J. Pasos Adelante: the effectiveness of a community-based chronic disease prevention program. Preventing chronic disease. 2005;2(1):A18 Epub 2005/01/27. ; PubMed Central PMCID: PMCPmc1323321. [PMC free article] [PubMed] [Google Scholar]
- 43.Sosa ET, Biediger-Friedman L, Zenong Y. Lessons Learned from Training of Promotores de Salud for Obesity and Diabetes Prevention. Journal of Health Disparities Research & Practice. 2013;6(1):1–13. .25215265 [Google Scholar]
- 44.Kousar R, Apostolopoulos V, Stojanovska L, Mayhew M, Totikidis V, Skaria A, et al. An Effective Model for Prevention and Management of Type 2 Diabetes. Qualitative health research. 2016;26(5):603–12. Epub 2015/03/25. doi: 10.1177/1049732315578401 . [DOI] [PubMed] [Google Scholar]
- 45.Coppell KJ, Tipene-Leach DC, Pahau HL, Williams SM, Abel S, Iles M, et al. Two-year results from a community-wide diabetes prevention intervention in a high risk indigenous community: the Ngati and Healthy project. Diabetes research and clinical practice. 2009;85(2):220–7. Epub 2009/06/16. doi: 10.1016/j.diabres.2009.05.009 . [DOI] [PubMed] [Google Scholar]
- 46.Schulz AJ, Zenk S, Odoms-Young A, Hollis-Neely T, Nwankwo R, Lockett M, et al. Healthy eating and exercising to reduce diabetes: exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. American journal of public health. 2005;95(4):645–51. Epub 2005/03/31. doi: 10.2105/AJPH.2004.048256 ; PubMed Central PMCID: PMCPmc1449236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cohen SJ, Ingram M. Border health strategic initiative: overview and introduction to a community-based model for diabetes prevention and control. Preventing chronic disease. 2005;2(1):A05 Epub 2005/01/27. ; PubMed Central PMCID: PMCPmc1323308. [PMC free article] [PubMed] [Google Scholar]
- 48.Teufel-Shone NI, Drummond R, Rawiel U. Community Case Study: Developing and Adapting a Family-based Diabetes Program at the U.S.-Mexico Border. Preventing chronic disease. 2005. [PMC free article] [PubMed] [Google Scholar]
- 49.Reinschmidt KM, Teufel-Shone NI, Bradford G, Drummond RL, Torres E, Redondo F, et al. Taking a Broad Approach to Public Health Program Adaptation: Adapting a Family-Based Diabetes Education Program. The Journal of Primary Prevention. 2010;31(1):69–83. doi: 10.1007/s10935-010-0208-6 [DOI] [PubMed] [Google Scholar]
- 50.Whittemore R, Rosenberg A, Gilmore L, Withey M, Breault A. Implementation of a diabetes prevention program in public housing communities. Public health nursing (Boston, Mass). 2014;31(4):317–26. Epub 2013/11/21. doi: 10.1111/phn.12093 . [DOI] [PubMed] [Google Scholar]
- 51.Cene CW, Haymore LB, Ellis D, Whitaker S, Henderson S, Lin FC, et al. Implementation of the power to prevent diabetes prevention educational curriculum into rural African American communities: a feasibility study. The Diabetes educator. 2013;39(6):776–85. Epub 2013/10/17. doi: 10.1177/0145721713507114 ; PubMed Central PMCID: PMCPmc4429528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. American journal of preventive medicine. 2009;37(6):505–11. Epub 2009/12/01. doi: 10.1016/j.amepre.2009.07.020 . [DOI] [PubMed] [Google Scholar]
- 53.Promotion NCfCDPaH. Addressing Chronic Disease through throughCommunity Health Workers: A POLICY AND SYSTEMS-LEVEL APPROACHSecond. National Center for Chronic Disease Prevention and Health Promotion, Prevention DfHDaS; 2015 April 2015. Report No.
- 54.Schneider H, Hlophe H, van Rensburg D. Community health workers and the response to HIV/AIDS in South Africa: tensions and prospects. Health policy and planning. 2008;23(3):179–87. Epub 2008/04/05. doi: 10.1093/heapol/czn006 . [DOI] [PubMed] [Google Scholar]
- 55.Kok MC, Dieleman M, Taegtmeyer M, Broerse JE, Kane SS, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health policy and planning. 2015;30(9):1207–27. Epub 2014/12/17. doi: 10.1093/heapol/czu126 ; PubMed Central PMCID: PMCPmc4597042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper.