Abstract
Background
Expanding access to HIV pre-exposure prophylaxis (PrEP) could help reduce rates of HIV infection in the United States. This study characterizes activities and barriers to PrEP implementation at local health departments (LHDs) in North Carolina (NC), which contains a large rural population.
Methods
In May 2016, a web-based survey was distributed to health directors of all county and district health departments in NC to assess PrEP-related activities, perceived barriers to PrEP implementation, and desired PrEP-related resources.
Results
Of 85 LHDs in NC, 56 (66%) responded to the survey. Of these, 2 (4%) reported PrEP prescribing and 7 (13%) externally referred for PrEP services. Among the 54 departments not prescribing PrEP, the most frequently cited reasons were cost concerns (n=25, 46%), lack of formal prescribing protocols (n=21, 39%), and belief that PrEP would be better managed at primary care or specialty clinics (n=19, 35%). Among the 47 departments not prescribing or referring clients for PrEP, the most frequently cited reasons for lack of PrEP referral were absence of local PrEP providers (n=29, 62%), lack of PrEP knowledge among staff (n=13, 28%), and perceived lack of PrEP candidates (n=12, 26%). The most frequently requested PrEP-related resources included training to help identify PrEP candidates (n=39, 70%) and training on PrEP prescribing and management (n=38, 68%).
Conclusions
PrEP prescribing and referral among LHDs in NC remains extremely limited. Increased PrEP-related training and support for LHD-based providers could enhance PrEP access, especially in rural and underserved areas.
Keywords: PrEP, HIV, local health departments
INTRODUCTION
Pre-exposure prophylaxis (PrEP) for human immunodeficiency virus (HIV) using a daily oral combination of emtricitabine (FTC) and tenofovir disoproxil fumarate (TDF) is now accepted as a safe and highly efficacious HIV prevention method.1–5 Based on early clinical trials demonstrating 44 to 75% reductions in HIV incidence with use of FTC/TDF1,2,4, the United States (US) Food and Drug Administration (FDA) approved FTC/TDF for PrEP in 2012.6 The US Public Health Service has since issued PrEP clinical practice guidelines7, and PrEP has been incorporated into the US National HIV/AIDS Strategy.8
An estimated 1.2 million US adults have indications for PrEP according to US Public Health Service guidelines, including 25% of adult MSM, 18% of adult intravenous drug users, and 0.4% of heterosexually active adults.9 Although national rates of PrEP initiation have increased annually since 2012, fewer than 80,000 US individuals have started FTC/TDF for PrEP as of 2015.10 Modelling data suggest that expanding the number of at-risk persons taking PrEP could have a major impact on HIV incidence; Jenness et al. estimated that PrEP use by 40% of at-risk MSM in the US could prevent 33% of new HIV infections over the next decade.11
Unfortunately, the task of achieving and maintaining population-level PrEP coverage in the US has been challenging, especially among underserved populations. Provision of PrEP-related care by sexually transmitted diseases (STD) clinics in local health departments (LHDs) represents a potential strategy to increase PrEP accessibility among health uninsured and publically insured populations.12,13 These settings may also be successful at engaging MSM, racial and ethnic minorities, and individuals without regular access to primary care.14,15 Early PrEP demonstration projects exploring the feasibility of PrEP implementation in public health clinics have reported high levels of interest and adherence to PrEP among participants from these settings.16,17
North Carolina (NC) has one of the highest rates of HIV diagnoses among US states, with 15.9 newly diagnosed infections among adults and adolescents per 100,000 population in 2015.18 The rate of HIV diagnoses has remained unchanged since approval of FTC/TDF for PrEP in 2012, suggesting a need for new strategies to enhance PrEP use across the state.19 To this end, the roles of NC LHDs in PrEP provision have not been comprehensively characterized. In this study, we conducted a survey of county and district health departments throughout NC to assess PrEP-related activities and examine barriers to PrEP implementation in this setting.
METHODS
Study setting
NC is divided into 100 counties which are served by a total of 85 LHDs operating at the county or multi-county (i.e. district) level. All LHDs in the state are required by NC law to offer core STD services to county or district residents. NC has the second largest rural population of any US state, with 3.2 million people residing in rural areas in 2010.20
Web-based survey of LHDs
In May 2016, a web-based survey was developed and distributed via email listserv to all 85 LHDs in NC. The survey was sent from the NC Communicable Disease Branch to LHD health directors. Health directors were requested to personally complete the survey but were not explicitly restricted from forwarding it to a designee. Completed surveys were collected using an online survey platform (SurveyMonkey, San Mateo, CA) over approximately three weeks. No compensation was provided for participation.
The survey comprised 20 multiple-choice or open-ended questions about respondent and LHD characteristics, PrEP-related activities, and PrEP-related resources. Demographic characteristics were collected by asking respondents to report their affiliated county or district, gender, age group, years of experience in public health, whether they personally provided patient care through their affiliated LHD, and whether they had heard of PrEP.
Respondents were asked to describe the perceived optimal role of LHDs in PrEP implementation in NC, whether each LHD had received PrEP-related inquiries, and to describe the current state of PrEP-related activities at each LHD. Those affiliated with LHDs engaged in PrEP-related activities were asked to characterize PrEP referral or provision at their department and describe barriers to PrEP referral or provision. Those affiliated with LHDs not engaged in PrEP-related activities were asked to identify reasons for not providing these services.
Respondents were also asked to identify desired PrEP-related resources at each LHD. Response choices included various training materials for department staff, protocols, a directive from the NC Department of Health and Human Services, on-call assistance, support for patient assistance programs, and education materials for health providers and/or the community.
Data analysis
When more than one survey was submitted per LHD (8/85; 9%), only the more complete submission was included in our analysis. Because county-level HIV incidence estimates were not available to this study, early (primary, secondary, and early latent) syphilis diagnosis rates were used to approximate STD incidence. County- or district-level HIV and early syphilis diagnosis rates per 100,000 population were calculated based on 2015 STD surveillance data from the NC Department of Health and Human Services and July 2015 population estimates from the National Center for Health Statistics.19,21 Survey and county- or district-level HIV data were analyzed in R (Vienna, Austria) using RStudio (Boston, MA, USA). Bivariate analysis was performed using Wilcoxon rank sum test; two-sided p-value was used.
Ethics statement
This study was conducted as part of an IRB research-exempt protocol (Duke Pro00067331). No personal health information was collected in the survey.
RESULTS
Respondent characteristics
Fifty-six (66%) of 85 LHDs responded to the survey. All have on-site STD clinics. Of survey respondents, 47 (84%) were female and 21 (38%) provided clinical care to LHD clients. Twenty-four (43%) were 45 years of age or younger. Nine (16%) reported fewer than 5 years of public health experience, 9 (16%) reported 6–10 years, 12 (21%) reported 11–15 years, 4 (7%) reported 16–20 years, and 22 (39%) reported greater than 20 years. Awareness of PrEP was reported among 49 (88%) of total respondents and among all respondents providing clinical care at their department.
Among the participating LHDs’ jurisdictions, the median (range) jurisdiction-wide rate of new HIV diagnoses in 2015 was 9 (0 – 34) diagnoses per 100,000 population, and the median (range) rate of persons living with diagnosed HIV was 215 (65 – 628) persons per 100,000 population.
PrEP-related activities
Nine (16%) LHDs reported receiving PrEP-related inquiries from healthcare providers in the community, and 20 (36%) reported receiving inquiries from the general public. Six (11%) respondents were unsure whether their affiliated departments had received PrEP-related inquiries.
Nine (16%) LHDs were engaged in PrEP-related activities, defined as either PrEP prescribing at health department clinics or referral of clients to PrEP prescribers in the community, at the time of survey (Figure 1). LHD engagement in PrEP-related activities was associated with higher rates of HIV diagnoses (p=0.04) and higher rates of persons living with diagnosed HIV (p=0.004) within the jurisdiction of the LHD, but there was no association between LHD engagement and early syphilis diagnosis rates (p=0.1). Of the nine LHDs engaged in PrEP-related activities, two reported on-site PrEP prescribing. Both of these LHDs prescribed PrEP to health-insured and uninsured clients, and neither identified any barriers to prescribing. The other seven LHDs referred clients externally to PrEP prescribers in the community. Of these, four referred clients to community health centers, three to academic medical centers, one to private practices, and one to various local providers without a formal process. Five (71%) of these LHDs reported no barriers to PrEP referral. Among the two identifying referral barriers, lack of a formal protocol (n=1) and cost of PrEP (n=1) were identified as the greatest obstacles.
Figure 1.
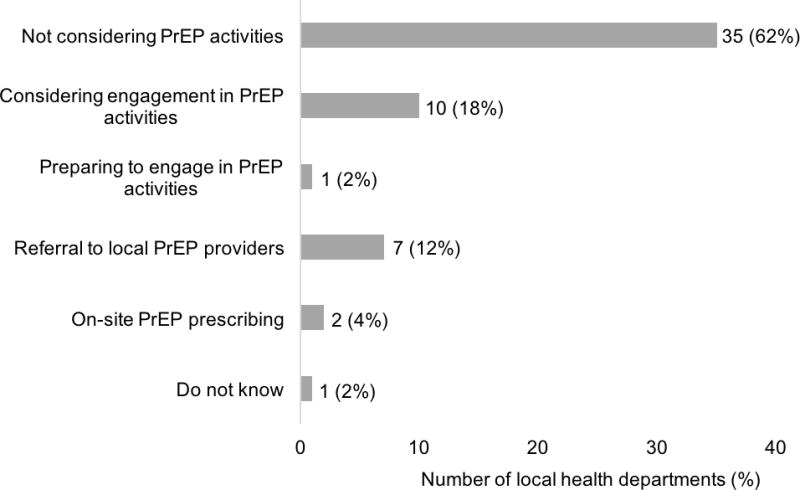
Status of HIV pre-exposure prophylaxis (PrEP)-related activities among local health departments in North Carolina, 2016 (n=56).
Among the 54 LHDs not prescribing PrEP at the time of survey, the most frequently cited reasons included concerns about the cost of PrEP (n=25, 46%), lack of a formal protocol for PrEP initiation and maintenance (n=21, 39%), and concerns that PrEP would be better prescribed in a primary care or specialty clinic (n=19, 35%) (Table 1). Among the 47 health departments not externally referring clients for PrEP at the time of survey, the most frequent reasons for lack of referral included lack of local PrEP providers (n=29, 62%), lack of PrEP awareness and knowledge among health department staff (n=13, 28%), and perceived lack of clients appropriate for PrEP (n=12, 26%) (Table 2).
Table 1.
Reasons for lack of PrEP prescribing programs among local health departments as reported by health directors or designees, North Carolina, 2016 (n=54).
| Reason | No. of respondents (%) |
|---|---|
| Concerns about the cost of PrEP | 25 (46) |
| Lack of a formal protocol to guide PrEP initiation and maintenance | 21 (39) |
| Concerns that PrEP would better be prescribed in a primary care or specialty clinic | 19 (35) |
| Lack of personnel to assist clients with navigating patient assistance programs for free or reduced-cost PrEP medication | 15 (28) |
| Lack of health department providers who are able to prescribe PrEP | 14 (26) |
| Lack of PrEP awareness and knowledge among health department staff | 10 (19) |
| Perceived lack of clients who are appropriate for PrEP | 10 (19) |
| Concerns that a PrEP prescribing program would divert resources from other services | 9 (17) |
| Uncertainty about which clients would be good candidates for PrEP | 6 (11) |
| Don’t know | 4 (7) |
| Lack of health department providers who are willing to prescribe PrEP | 4 (7) |
| Prefer not to respond | 3 (6) |
| Lack of support or interest from the local board of health or other local public health authority | 1 (2) |
| Lack of support or interest from health department staff | 0 (0) |
Multiple responses could be selected per respondent.
Table 2.
Reasons for lack of PrEP referral programs among local health departments as reported by health directors or designees, North Carolina, 2016 (n=47).
| Reason | No. of respondents (%) |
|---|---|
| Lack of local PrEP providers to which clients could be referred | 29 (62) |
| Lack of PrEP awareness and knowledge among health department staff | 13 (28) |
| Perceived lack of clients who are appropriate for PrEP | 12 (26) |
| Concerns about the cost of PrEP | 11 (23) |
| Uncertainty about which clients are good candidates for PrEP | 7 (15) |
| Don’t know | 3 (6) |
| Concerns that a PrEP referral program would divert resources from other services | 2 (4) |
| Prefer not to respond | 1 (2) |
| Lack of support or interest from the local board of health or other local public health authority | 0 (0) |
| Lack of support for or interest in PrEP from health department staff | 0 (0) |
Multiple responses could be selected per respondent.
Among all respondents, the most frequently perceived optimal roles of LHDs in PrEP implementation included referral of clients to external PrEP providers (n=40, 71%), PrEP education and outreach to clients and community members (n=39, 70%), PrEP education and outreach to local healthcare providers (n=28, 50%), and on-site prescribing of PrEP (n=18, 32%).
Desired resources for PrEP implementation
When asked what PrEP-related resources would be most helpful for each LHD, the most frequently requested resources included training on identification of potential PrEP candidates (n=39, 70%), training on PrEP prescribing and management (n=38, 68%), and PrEP education and outreach materials for clients and community members (n=37, 66%) (Table 3). Among 42 respondents expressing a preference for potential PrEP training formats, the most frequently preferred options were web-based (n=22, 52%) or in-person (n=15, 36%) training events, with a minority of respondents preferring peer networks or forums (n=3, 7%) or visits to health departments with existing PrEP-prescribing programs (n=2, 5%).
Table 3.
Desired PrEP-related resources among local health departments as reported by health directors or designees, North Carolina, 2016 (n=56).
| Resource | No. of respondents (%) |
|---|---|
| Training on how to identify clients who might benefit from PrEP | 39 (70) |
| Training on PrEP prescribing and management | 38 (68) |
| PrEP education and outreach materials for clients and communities | 37 (66) |
| Protocols for PrEP referral from a local health department clinic to a healthcare provider in the community | 36 (64) |
| Protocols for PrEP initiation and management in a local health department clinic setting | 36 (64) |
| PrEP education and outreach materials for healthcare providers | 35 (63) |
| Support to help clients navigate patient assistance programs for free or reduced-cost PrEP medication | 34 (61) |
| Directive from the state department of Health and Human Services regarding PrEP engagement in local health departments | 29 (52) |
| Availability of on-call assistance (e.g., “hotline”) to answer questions about PrEP prescribing and management | 26 (46) |
Multiple responses could be selected per respondent.
DISCUSSION
Large-scale PrEP implementation in the US could substantially reduce the HIV burden among at-risk groups.11 The need to expand PrEP services is especially apparent in the Southern US, which has disproportionately high rates of new HIV diagnoses and worse outcomes among persons living with HIV compared to other US regions.18,22 Creating access to PrEP services in rural areas remains a challenge, with the Southern states bearing the highest percentage of individuals with HIV living outside of urban areas of any US geographic region.18 Integration of PrEP-related services into publicly funded STD prevention and treatment programs, such as those delivered by LHDs, has been reported as a potential strategy to augment the accessibility of PrEP among medically underserved and rural populations.23–25
Our study reveals that implementation of PrEP services among LHDs in NC remains extremely limited. Only 16% of LHDs were engaged in PrEP activities at the time of this survey, while 62% of LHDs were not considering future engagement in PrEP activities. These results suggest that additional resources and funding would be necessary to build the infrastructure for PrEP services in the local public health sector. Importantly, greater than one-third of respondents in this study reported that the lack of a formal clinical guidance protocol was a barrier to PrEP prescribing, and training materials were among the most frequently requested PrEP-related resources. While comprehensive PrEP clinical guidelines are available7, the documentation is lengthy, and other studies have suggested that clinical personnel may not be aware these guidelines.26 Furthermore, there remains an unmet need to develop and disseminate guidance that is tailored to the unique structure, resources, and challenges of a LHD clinic. In this time- and resource-constrained setting, use of point-of-care risk assessment tools to identify individuals at increased risk of HIV acquisition could be a practical and accessible strategy to screen for potential PrEP candidates.27,28 Roll-out of such tools would need to be coupled with skills-based training on identification of candidates for PrEP, drug prescribing and safety monitoring, counseling on medication adherence and behavioral risk reduction, and navigation of medication assistance programs.29 Academic detailing programs, involving on-site education of clinic providers and staff, have been used to improve clinic readiness for PrEP services in other settings and could be further explored as a method to deliver PrEP-related training to LHDs.30
Not surprisingly, cost concerns were the most frequently cited barrier to PrEP provision in this study. LHDs are often in a unique position to engage harder-to-reach low-income and uninsured populations at risk for HIV acquisition, but there remains a question of how to account for the costs of PrEP service delivery among these clients without diverting resources from other LHD activities.13,15,25,31 Recurrent medical costs associated with PrEP provision include clinic visits; screening tests for HIV, hepatitis B, and other STDs; periodic laboratory tests including serum creatinine levels; and patient counseling and aid with medication assistance programs.32,33 Although some of the laboratory costs associated with PrEP initiation and follow-up are already supported by STD clinic budgets, the public funding of these clinics throughout the US has recently faced the threat of budgetary reductions.34,35 Notably, at the time of this study NC has not expanded Medicaid under the Afforable Care Act. In order to implement and sustain PrEP programs in LHDs, public health providers will need assistance to leverage existing funding mechanisms (e.g. private health insurance, Medicaid, and medication assistance programs) as well as develop novel strategies for resource allocation.
In light of the barriers, the perceived optimal role of LHDs in PrEP implementation varied among survey respondents. Overall, preference was shown for referral of LHD clients to external PrEP providers as opposed to on-site prescription at LHD clinics. Direct PrEP provision at LHD clinics would promote access for medically underserved populations at risk for HIV acquisition, as well as allow opportunities to integrate PrEP into comprehensive STD services.23 However, these clinics tend to be optimized for drop-in or episodic care rather than longitudinal follow-up of patients. By referring patients directly to local PrEP-prescribing clinics or initiating patients on PrEP on-site but referring externally for follow-up care, LHDs could avoid this shortcoming while fulfilling critical roles in the PrEP cascade, including screening for HIV and other STDs, identification of PrEP candidates, and linkage to PrEP care.36 A caveat, however, is that PrEP referral relies on a sufficiency of local, financially accessible PrEP-prescribing clinics. Among LHDs without the necessary infrastructure or personnel to deliver PrEP services, establishment of telemedicine services through collaborating LHDs or other institutions represents another potential strategy to expand PrEP access among rural populations. Ultimately, the optimal role of public health departments in PrEP delivery may depend on the local milieu, including local HIV prevalence, characteristics of the local population at risk for HIV acquisition, and the geographic and financial accessibility of local PrEP-prescribing clinics.
Our study comes with limitations. First, approximately one-third of LHDs did not respond to our survey. Additionally, health directors were chosen as survey respondents due to their ability to assess their respective LHDs’ readiness for PrEP implementation and their role in programmatic decision making; however, fewer than half of respondents directly provided clinical care to LHD clients. A dedicated survey of public health clinicians may provide further insight into the perceived need for, interest in, and anticipated challenges to PrEP referral or provision among clients. Finally, as this study only reports on health departments in NC, our results cannot be generalized to other states. However, a prior survey of a national sample of LHDs by Smith et al. reported similarly low overall rates of PrEP implementation, with higher rates of PrEP services among LHDs in the Western states.37 Next steps include further evaluation of PrEP capacity among LHDs in other states to assess barriers to implementation on a wider scale.
While few LHDs in NC are currently engaged in PrEP prescribing or referral services, preparations for or consideration of PrEP activities were reported by several survey respondents. These findings, as well as the high level of interest in PrEP-related training resources, educational materials, and protocols among respondents suggests a potential for future expansion of PrEP services among LHDs across the state. Of note, significant efforts to build PrEP capacity already been undertaken through the NC AIDS Training and Education Center, and additional LHDs in NC have recently received PrEP training and are working to implement PrEP programs in their area.38 Addressing the challenges of PrEP implementation in the public health sector, including training, administrative, and funding needs, will be critical to meet the needs of underserved populations at risk for HIV infection.
Acknowledgments
This publication resulted in part from research supported by the Duke University Center for AIDS Research (CFAR), an NIH funded program (P30AI064518). CBH is supported by the National Institute of Mental Health (NIMH; K23MH099941) and the UNC CFAR (P30AI50410). The views expressed are not necessarily those of the NIH or NIMH. We acknowledge Aaron Fleischauer, Jacquelyn Clymore, Evelyn Foust, and Erika Samoff from the NC Division of Public Health; Gregory Samsa from Duke University; Gretchen Weiss from National Association of City and County Health Officials; and the NC Association of Local Health Directors for their contribution to this work.
Source of Funding: MM is supported by the Duke CFAR (P30AI064518). CBH is supported by the National Institute of Mental Health (NIMH; K23MH099941) and the UNC CFAR (P30AI50410). ACS receives FOCUS grant funding from Gilead Inc. ACS and HS receive royalties from UpToDate.
Footnotes
Conflicts of Interest: This publication resulted in part from research supported by the Duke University Center for AIDS Research (CFAR), an NIH funded program (P30AI064518).
References
- 1.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grohskopf LA, Chillag KL, Gvetadze R, et al. Randomized trial of clinical safety of daily oral tenofovir disoproxil fumarate among HIV-uninfected men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2013;64(1):79–86. doi: 10.1097/QAI.0b013e31828ece33. [DOI] [PubMed] [Google Scholar]
- 4.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–434. doi: 10.1056/NEJMoa1110711. [DOI] [PubMed] [Google Scholar]
- 5.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–2090. doi: 10.1016/S0140-6736(13)61127-7. [DOI] [PubMed] [Google Scholar]
- 6.Food and Drug Administration. FDA approves first medication to reduce HIV risk. 2012 https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm311821.htmAccessed June 4, 2017.
- 7.US Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV Infection in the United States – 2014 clinical practice guideline. Atlanta, GA: US Department of Health and Human Services; 2014. [Google Scholar]
- 8.White House Office of National AIDS Policy. National HIV/AIDS strategy for the United States: updated to 2020. Washington, DC: White House Office of National AIDS Policy; 2015. [Google Scholar]
- 9.Smith DK, Van Handel M, Wolitski RJ, et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition–United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(46):1291–1295. doi: 10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- 10.Mera R, McCallister S, Palmer B, Mayer G, Magnuson D, Rawlings MK. FTC/TDF (Truvada) for HIV pre-exposure prophlyaxis (PrEP) utilization in the United States: 2012–2015. Paper presented at: 21st International AIDS Conference 2016; Durban, South Africa. [Google Scholar]
- 11.Jenness SM, Goodreau SM, Rosenberg E, et al. Impact of the Centers for Disease Control’s HIV preexposure prophylaxis guidelines for men who have sex with men in the United States. J Infect Dis. 2016;214(12):1800–1807. doi: 10.1093/infdis/jiw223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearson WS, Cramer R, Tao G, Leichliter JS, Gift TL, Hoover KW. Willingness to use health insurance at a sexually transmitted disease clinic: a survey of patients at 21 US clinics. Am J Public Health. 2016;106(8):1511–1513. doi: 10.2105/AJPH.2016.303263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stephens SC, Cohen SE, Philip SS, Bernstein KT. Insurance among patients seeking care at a municipal sexually transmitted disease clinic: implications for health care reform in the United States. Sex Transm Dis. 2014;41(4):227–232. doi: 10.1097/OLQ.0000000000000109. [DOI] [PubMed] [Google Scholar]
- 14.Seth P, Wang G, Sizemore E, Hogben M. HIV testing and HIV service delivery to populations at high risk attending sexually transmitted disease clinics in the United States, 2011–2013. Am J Public Health. 2015;105(11):2374–2381. doi: 10.2105/AJPH.2015.302778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehtani NJ, Schumacher CM, Johnsen LE, et al. Continued importance of sexually transmitted disease clinics in the era of the Affordable Care Act. Am J Prev Med. 2016;51(3):364–367. doi: 10.1016/j.amepre.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu AY, Cohen SE, Vittinghoff E, et al. Preexposure Prophylaxis for HIV Infection Integrated With Municipal- and Community-Based Sexual Health Services. JAMA Intern Med. 2016;176(1):75–84. doi: 10.1001/jamainternmed.2015.4683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen SE, Vittinghoff E, Bacon O, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP demonstration project. J Acquir Immune Defic Syndr. 2015;68(4):439–448. doi: 10.1097/QAI.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2015. Atlanta, GA: US Department of Health and Human Services; 2016. [Google Scholar]
- 19.North Carolina HIV/STD Surveillance Unit. 2015 North Carolina HIV/STD Surveillance Report. Raleigh, NC: North Carolina Department of Health and Human Services; 2016. [Google Scholar]
- 20.US Census Bureau. Census urban and rural classification and urban area criteria. 2010 https://www.census.gov/geo/reference/ua/urban-rural-2010.htmlAccessed June 4, 2017.
- 21.National Center for Health Statistics. Vintage 2015 bridged-race postcensal population estimates. 2015 https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm.
- 22.Reif S, Pence BW, Hall I, Hu X, Whetten K, Wilson E. HIV diagnoses, prevalence and outcomes in nine southern states. J Community Health. 2015;40(4):642–651. doi: 10.1007/s10900-014-9979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcus JL, Volk JE, Pinder J, et al. Successful implementation of HIV preexposure prophylaxis: lessons learned from three clinical settings. Curr HIV/AIDS Rep. 2016;13(2):116–124. doi: 10.1007/s11904-016-0308-x. [DOI] [PubMed] [Google Scholar]
- 24.Cohen RA, Martinez ME, Zammitti EP. Health insurance coverage: early release of estimates from the National Health Interview Survey, 2015. National Center for Health Statistics; 2016. [Google Scholar]
- 25.Gift TL, Haderxhanaj LT, Torrone EA, Behl AS, Romaguera RA, Leichliter JS. Estimating the size and cost of the STD prevention services safety net. Public Health Rep. 2015;130(6):602–609. doi: 10.1177/003335491513000608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krakower DS, Oldenburg CE, Mitty JA, et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: results from a survey of healthcare providers in New England. PLoS One. 2015;10(7):e0132398. doi: 10.1371/journal.pone.0132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith DK, Pan Y, Rose CE, et al. A brief screening tool to assess the risk of contracting HIV infection among active injection drug users. J Addict Med. 2015;9(3):226–232. doi: 10.1097/ADM.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith DK, Pals SL, Herbst JH, Shinde S, Carey JW. Development of a clinical screening index predictive of incident HIV infection among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2012;60(4):421–427. doi: 10.1097/QAI.0b013e318256b2f6. [DOI] [PubMed] [Google Scholar]
- 29.Krakower DS, Mayer KH. The role of healthcare providers in the roll out of preexposure prophylaxis. Curr Opin HIV AIDS. 2016;11(1):41–48. doi: 10.1097/COH.0000000000000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Conniff J, Evensen A. Preexposure prophylaxis (PrEP) for HIV prevention: the primary care perspective. J Am Board Fam Med. 2016;29(1):143–151. doi: 10.3122/jabfm.2016.01.150223. [DOI] [PubMed] [Google Scholar]
- 31.Landry DJ, Forrest JD. Public health departments providing sexually transmitted disease services. Fam Plann Perspect. 1996;28(6):261–266. [PubMed] [Google Scholar]
- 32.Koppenhaver RT, Sorensen SW, Farnham PG, Sansom SL. The cost-effectiveness of pre-exposure prophylaxis in men who have sex with men in the United States: an epidemic model. J Acquir Immune Defic Syndr. 2011;58(2):e51–52. doi: 10.1097/QAI.0b013e31822b74fe. [DOI] [PubMed] [Google Scholar]
- 33.Calabrese SK, Magnus M, Mayer KH, et al. Putting PrEP into practice: lessons learned from early-adopting U.S. providers' firsthand experiences providing HIV pre-exposure prophylaxis and associated care. PLoS One. 2016;11(6):e0157324. doi: 10.1371/journal.pone.0157324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ye J, Leep C, Newman S. Reductions of budgets, staffing, and programs among local health departments: results from NACCHO’s economic surveillance surveys, 2009–2013. J Public Health Manag Pract. 2015;21(2):126–133. doi: 10.1097/PHH.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 35.Willard R, Shah GH, Leep C, Ku L. Impact of the 2008–2010 economic recession on local health departments. J Public Health Manag Pract. 2012;18(2):106–114. doi: 10.1097/PHH.0b013e3182461cf2. [DOI] [PubMed] [Google Scholar]
- 36.Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61(10):1590–1597. doi: 10.1093/cid/civ664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith D, Weiss G, Kitlas A, Newman S, Ye J. HIV Research for Prevention. Chicago, IL: 2016. PrEP implementation by local health departments in US cities and counties: findings from a 2015 assessment of local health departments. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.North Carolina AIDS Training and Education Center. https://www.med.unc.edu/ncaidstraining Accessed June 4, 2017.


