Abstract
Objective
Measure associations between adolescent baseball players’ perceptions of smokeless tobacco (ST) use by professional baseball players and those adolescents’ actual ST use and susceptibility.
Methods
Male baseball players (N=360) at 25 rural California high schools completed tobacco behavior surveys and reported how likely they believed it was their favorite major league baseball player used ST. We compared ST use and, among ST never-users, willingness and expectations to use ST, according to perceived favorite player’s use.
Results
Adolescents responding that their favorite player definitely or probably used ST were significantly more likely to use ST themselves. High school ST never-users who perceived that their favorite player definitely used ST were 2.5 to 3-times more likely to be susceptible to ST initiation than participants responding that their favorite player definitely did not use ST.
Conclusions
Adolescents’ ST behaviors and intentions were correlated with their perceptions of professional baseball players’ ST use.
Keywords: Adolescents, Rural Community Health, Athletics, Baseball, Smokeless Tobacco, Health Perceptions
INTRODUCTION
In the United States, conventional smokeless tobacco (ST) includes oral moist snuff and chewing tobacco: products associated with oral and pancreatic cancer and other adverse oral conditions, including periodontal diseases, dental caries, tooth loss, and mucosal lesions(1). Despite declining youth smoking, the prevalence of ST use among U.S. adolescents has persisted at nearly the same level for over a decade(2), and in 2015, equaled that of cigarettes among male high school students(2). Dental professionals are likely to encounter young ST users in practice and play a role in preventing youth tobacco use through individual patient counseling and by supporting policies and other measures that aim to reduce youth initiation.
Living in rural areas, being male, and participation in certain sports are associated with ST use(3). Baseball, particularly, has a history of tobacco industry sponsorship and high prevalence of ST use among players, from amateur to professional levels(4). Young fans may perceive ST use by professional athletes during widely broadcast games as an implicit tobacco endorsement, potentially normalizing ST use and encouraging initiation(4,5).
The present study aimed to assess the perception among a sample of high school baseball players regarding the likelihood that their favorite Major League Baseball (MLB) player used ST and to evaluate the association of that perception with the high school players’ current ST use and, among ST never-users, susceptibility to ST initiation. We hypothesized greater ST use and ST susceptibility among adolescents who perceived it more likely that their favorite MLB player used ST.
METHODS
This cross-sectional study analyzed baseline data from a cohort of male baseball players at rural high schools who were asked about their perceptions and experiences with tobacco products, including ST. The cohort study incorporated the dual-process model(6), hypothesizing that adolescent decision-making includes both reasoned action and social influences, such as perceived acceptability. Rolling school enrollment began in 2014. Schools initially approached for participation had collaborated with investigators previously and were located in rural California communities (county population density <1000 persons/square-mile; municipality <50,000 residents). Recruitment expanded to schools in the same baseball leagues or recommended by coaches or administrators at participating schools. Fifty-three schools met with the study team, and 36 (68%) enrolled. Schools declining to participate tended to be larger (median enrollment: 1000 vs. 700; p=0.70) and to serve a lower percentage of students eligible for free or reduced price school lunch (50% vs. 55%; p=0.31), but these differences were not statistically significant. Students provided signed parental consent and participant assent (age 14–17) or self-consent (age 18). Of approximately 1060 student baseball players, 762 (72%) returned consent forms, of which 594 (78%) indicated positive consent and completed the survey. Questions about professional baseball players were added during 2015. Therefore, eligible for the present study were 377 male baseball athletes at 25 schools who completed the added baseline items during the 2015 or 2016 baseball seasons, representing 13 California counties (median municipality size: 12,000 residents).
Electronic surveys, completed in classrooms before or after baseball practice, included the free-response item, “Who is your favorite current Major League Baseball (MLB) player?” and on the next screen, “Do you think that player uses smokeless tobacco (dip or chew)?” (responses: definitely yes, probably yes, probably not, definitely not). Seventeen participants who did not name a MLB player were excluded from analysis. Adolescents who reported having never tried ST (n=250) were asked whether they would use ST if “one of your best friends offered” and whether they think they “will be using dip or chew a year from now” with the same Likert-type response options. Failure to strongly reject these items with an answer of “definitely not” was considered susceptible to ST use: a categorization predictive of subsequent tobacco initiation(7).
We compared ST susceptibility prevalence according to perceived MLB player ST use (chi-squared test) and used generalized estimating equations (exchangeable working correlation structure) to calculate prevalence ratios and robust 95% confidence intervals (CI) adjusted for grade in school, race/ethnicity, parental education, and intra-school clustering. Sample size planning was based on the full cohort; for the 360 individuals in this sub-study, there would be 86% power (2-tailed test; alpha=0.05) to detect 1.5-times the prevalence of ST ever-use among those reporting that their favorite MLB player definitely or probably used ST (44% of the sample) versus those reporting that their favorite MLB player definitely or probably did not use ST (assuming 25% ever-use in this group).
The University of California San Francisco Institutional Review Board approved all study procedures. For participation, schools received $150 to $300, and individuals received $10 credit with an online retailer.
RESULTS
Of 360 adolescents who named one current MLB player, responses to whether that player used ST were: definitely yes (8%), probably yes (36%), probably not (41%), and definitely not (15%). Responses covered 82 MLB players from 27 teams. Mean participant age was 15.8 years (SD: 1.2), 47% identified as Hispanic/Latino, 41% identified as Non-Hispanic White, and 57% reported having at least one parent with a college degree. Overall, 31% had tried ST at least once, and 13% had used ST in the past month. Older age and identifying as Non-Hispanic White were positively associated with ST use. Participants who responded that their favorite MLB player definitely or probably used ST were significantly more likely to have ever tried ST themselves (38% vs. 25%; p=0.007) and to have used ST in the past month (18% vs. 8%; p=0.003).
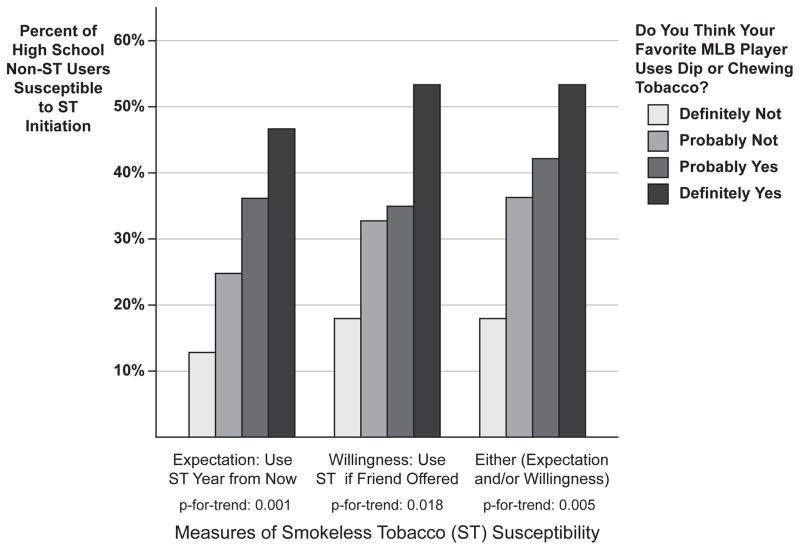
There was a gradated, positive association between ST susceptibility and perceived ST use by favorite MLB players (Figure). Adolescent ST never-users who perceived that their favorite player definitely used ST were more likely to express willingness to try ST, have positive expectations about future ST use, and were more likely to be susceptible to ST initiation by either measure compared to participants who reported that their favorite player definitely did not use ST (Figure). This association was robust to statistical adjustment for socio-demographic variables (Table) and persisted among never-users of any tobacco (prevalence ratio for ST susceptibility by either measure among tobacco never-users: 3.7; 95% CI: 1.0, 13.3; p=0.045).
Figure.
Susceptibility to smokeless tobacco (ST) initiation among ST never-using high school male baseball players, according to perceived ST use by their favorite professional baseball player
Among rural high school baseball players (n=250) who had never tried smokeless tobacco (ST), the percent of respondents susceptible to ST initiation was increasingly higher among adolescents who perceived it more likely that their favorite Major League Baseball (MLB) player used ST.
Table.
High school baseball players’ smokeless tobacco behavior and susceptibility, according to perceived ST use by their favorite professional baseball player
| All participants (n = 360) ST behavior |
ST never-users (n = 250) ST susceptibility |
||||||
|---|---|---|---|---|---|---|---|
| Do you think your favorite MLB player users dip or chewing tobacco? | n | Lifetime ST use | Past-month ST use | n | Expectation PR (95% CI) | Willingness PR (95% CI) | Expectation and/or willingness PR (95% CI) |
|
|
|
|
|||||
| Definitely No | 53 | 26% | 9% | 39 | reference | reference | reference |
| Probably No | 149 | 24% | 7% | 113 | 1.7 (0.8, 3.4) | 1.6 (0.8, 3.2) | 1.8 (1.0, 3.3) |
| Probably Yes | 131 | 37% | 19% | 83 | 2.5 (1.1, 5.5) | 1.8 (0.9, 3.6) | 2.0 (1.1, 3.8) |
| Definitely Yes | 27 | 44% | 15% | 15 | 3.3 (1.3, 8.2) | 2.5 (1.0, 6.1) | 2.5 (1.0, 5.8) |
Prevalence ratios adjusted for grade in school, race/ethnicity, parental education, and intra-school clustering using generalized estimating equations.
Abbreviations: ST = smokeless tobacco (oral snuff and chewing tobacco); MLB = Major League Baseball; PR = prevalence ratio; CI = confidence interval
DISCUSSION
In this population, perceived smokeless tobacco use by admired MLB players was strongly associated with high school baseball players’ current ST use and with susceptibility to ST initiation among ST never-users. This finding is consistent with studies reporting that emulation of respected male figures, including athletes and during sports participation, contributes to normalizing ST and encouraging initiation(8). Tobacco related-norms and acceptability are fodder for effective anti-tobacco counseling from oral health professionals. Meanwhile, the potential influence of high-profile figures on youth tobacco use provides reason for further limits on tobacco in professional sports.
Some study limitations merit attention. Importantly, associations were cross-sectional: it is possible that adolescents’ prior tobacco experiences may have influenced how they perceived major leaguers, projecting their own tobacco behavior when observing MLB players. However, associations persisted when restricted to tobacco never-users, and the susceptibility measures used in this study have predicted future tobacco use elsewhere(7). It is also possible that adolescents’ perceptions were discordant with MLB players’ actual ST use. Nonetheless, perceptions may match reality in driving behavior, as youth who perceive greater ST use and acceptance by others are at heightened risk for ST initiation themselves(9). Finally, while this investigation tested a novel questionnaire item in a target population at high-risk of ST use, schools were enrolled via convenience sampling: external validity may not extend to non-athletes or other geographic regions. We speculate that this sample could underestimate ST use among rural males: inclusion of junior varsity and freshman teams yielded a relatively young sample, and coaches and administrators most willing to participate might have also promoted tobacco control measures at their schools.
Hoping to deter youth tobacco experimentation, several U.S. cities recently enacted ordinances to ban tobacco in MLB stadiums, but enforcement is challenging. MLB itself began prohibiting players from carrying ST products on their uniforms in 2012 but did not bar on-field use, which remains prominent during game telecasts. In 2017, new MLB players, but not those who entered the league before 2017, will be banned from using ST in games(10). These actions are promising steps, but limited reach might curb their impact on the widespread perception that baseball and tobacco chewing are culturally intertwined, let alone on potential health consequences of ST use for current players. Future monitoring is needed to track potential changes in adolescents’ perceptions and actual ST use among professional athletes following these new restrictions.
In this study, rural adolescent baseball players who reported that their favorite major league baseball player used smokeless tobacco were themselves more likely to use smokeless tobacco or be susceptible to use. Smokeless tobacco use by professional athletes remains a plausible contributor to youth initiation in this population. Recent steps by individual cities and MLB to limit tobacco on the playing field take aim at this risk factor. Dental practitioners and public health professionals could contribute by supporting consistent tobacco control measures that challenge the perceived acceptability of tobacco in sports and prevent young fans from beginning this potentially deadly behavior.
Acknowledgments
We acknowledge the contributions of Joanna Hill, Janelle Urata, Victoria Campbell, Archnaa Rajasekaran, and Dr. Margaret Walsh, all of the University of California San Francisco, in study design, administration, and data collection. The U.S. National Institutes of Health National Cancer Institute and Food and Drug Administration Center for Tobacco Products (grant number P50CA180890) and the NIH National Center for Advancing Translational Sciences (grant number KL2TR000143) supported this work. The funding organizations had no role in study design, data collection, analysis, interpretation, or publication. Content does not necessarily reflect the official views of the funding organizations.
References
- 1.National Cancer Institute and Centers for Disease Control and Prevention. Smokeless tobacco and public health: a global perspective. Bethesda, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Institutes of Health, National Cancer Institute; [Accessed 2016 October 27]. NIH Publication No. 14-7983. http://cancercontrol.cancer.gov/brp/tcrb/global-perspective/SmokelessTobaccoAndPublicHealth.pdf. Published 2014. [Google Scholar]
- 2.Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, et al. Youth risk behavior surveillance - United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 3.Gansky SA, Ellison JA, Kavanagh C, Isong U, Walsh MM. Patterns and correlates of spit tobacco use among high school males in rural California. J Public Health Dent. 2009;69(2):116–24. doi: 10.1111/j.1752-7325.2008.00109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connolly GN, Orleans CT, Blum A. Snuffing tobacco out of sport. Am J Public Health. 1992;82(3):351–3. doi: 10.2105/ajph.82.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones RB. Use of smokeless tobacco in the 1986 World Series. N Engl J Med. 1987;316(15):952. doi: 10.1056/nejm198704093161521. [DOI] [PubMed] [Google Scholar]
- 6.Gibbons FX, Houlihan AE, Gerrard M. Reason and reaction: the utility of a dual-focus, dual-processing perspective on promotion and prevention of adolescent health risk behaviour. Br J Health Psychol. 2009;14(Pt 2):231–48. doi: 10.1348/135910708X376640. [DOI] [PubMed] [Google Scholar]
- 7.Choi WS, Gilpin EA, Farkas AJ, Pierce JP. Determining the probability of future smoking among adolescents. Addiction. 2001;96(2):313–23. doi: 10.1046/j.1360-0443.2001.96231315.x. [DOI] [PubMed] [Google Scholar]
- 8.Helme DW, Cohen EL, Parrish AJ. Health, masculinity and smokeless tobacco use among college-aged men. Health Commun. 2012;27(5):467–77. doi: 10.1080/10410236.2011.610257. [DOI] [PubMed] [Google Scholar]
- 9.Elder JP, Molgaard CA, Gresham L. Predictors of chewing tobacco and cigarette use in a multiethnic public school population. Adolescence. 1988;23(91):689–702. [PubMed] [Google Scholar]
- 10.Lacques G. Can Major League Baseball really rid itself of smokeless tobacco? [Accessed 2016 Dec 9];USA Today. 2016 Dec 1; http://www.usatoday.com/story/sports/mlb/2016/12/01/baseball-smokeless-tobacco-cba-mlb/94721720/