Abstract
A growing body of research from the United States informed by intersectionality theory indicates that racial identity, gender, and income are often entwined with one another as determinants of health in unexpectedly complex ways. Research of this kind from Canada is scarce, however. Using data pooled from ten cycles (2001-2013) of the Canadian Community Health Survey, we regressed hypertension (HT) and diabetes (DM) on income in subsamples of Black women (n = 3,506), White women (n = 336,341), Black men (n = 2,806) and White men (n = 271,260). An increase of one decile in income was associated with lower odds of hypertension and diabetes among White men (ORHT = .98, 95% CI (.97, .99); ORDM = .93, 95% CI (.92, .94)) and White women (ORHT = .95, 95% CI (.95, .96); ORDM = .90, 95% CI (.89, .91)). In contrast, an increase of one decile in income was not associated with either health outcome among Black men (ORHT = .99, 95% CI (.92, 1.06); ORDM = .99, 95% CI (.91, 1.08)) and strongly associated with both outcomes among Black women (ORHT = .86, 95% CI (.80, .92); ORDM = .83, 95% CI (.75, .92)). Our findings highlight the complexity of the unequal distribution of hypertension and diabetes, which includes inordinately high risks of both outcomes for poor Black women and an absence of associations between income and both outcomes for Black men in Canada. These results suggest that an intersectionality framework can contribute to uncovering health inequalities in Canada.
Keywords: Canada, Black-White Health Inequalities, Hypertension, Diabetes, Intersectionality
Introduction
Hypertension and diabetes are among the leading causes of mortality and disability-adjusted life years globally.1 Hypertension and diabetes rates continue to rise in most Western countries, including Canada.2,3 Unfortunately, both of these chronic conditions are unequally distributed by socioeconomic status in Canada.4-7 Previous research also suggests that prevalence rates in hypertension and diabetes are higher among Black Canadians than White Canadians and that recent increases in these rates are particularly steep among Black Canadian women.8-14 Given the fundamental role of income in peoples’ capacity for preventing disease and promoting good health, investigating the potentially mediating role of income in Black-White inequalities in hypertension and diabetes has the potential to inform population health intervention strategies. However, while income is strongly associated with both hypertension and diabetes in Canada, it does not appear to explain Black-White differences in these outcomes.11,12,15
To better conceptualize how racial identity, gender, and income might operate together to produce health inequalities, some researchers have turned to intersectionality theory, which contends that structural processes aligned with racism, sexism, and classism produce: 1) unique experiences for the inhabitants of the complex social locations (eg, wealthy Black women or poor White women); and 2) “multiple jeopardies” for those who are disempowered at multiple locations generated by these axes of inequality.16,17 Consistent with this postulate, American researchers have found that racial inequalities in self-rated health are inordinately strong among wealthy women,18 education-based inequalities in self-rated health are particularly weak among Black women,19 and poor Black women experience especially high increases in body mass index as they age.20 In other words, racial identity, gender, and socioeconomic conditions appear to be entwined with one another in quite complex ways as determinants of health in the United States.
Unfortunately, research of this kind is scarce in Canada. One study found that, among immigrants in Ontario, income had a strong protective effect on diabetes among women but not among men.21 Another study examined the three-way interaction between racial identity, gender, and income in association with hypertension and reported strong inverse relationships between income and likelihood of hypertension for Black women and White women, an absence of a relationship between income and hypertension for White men, and a strong positive relationship between income and likelihood of hypertension for Black men.22
The goal of our study was to further investigate how racial identity, gender, and income intersect with one another in complex ways to generate health inequalities in Canada. Informed by intersectionality theory and the accumulating evidence on the unequal distribution of hypertension and diabetes in Canada, this study compares the nature and strength of income-based inequalities in hypertension and diabetes in samples of Black women, White women, Black men, and White men. To do so, we examine pooled data from all available cycles of the largest ongoing Canadian health-related survey, the Canadian Community Health Survey (CCHS).
Methods
Data
The CCHS is a repeated cross-sectional survey that collects information related to health status, health care utilization, and health determinants for the Canadian population.23 Statistics Canada conducted the CCHS in 2001, 2003, and 2005 and annually from 2007. The target populations for these surveys are all persons aged >12 years residing in Canada, excluding individuals living on Indian Reserves and Crown Lands, institutional residents, fulltime members of the Canadian Armed Forces, and residents of some remote regions. One person was chosen randomly from each household to complete the survey. Response rates for the surveys ranged from a high of 84.7% in 2001 to a low of 67.0% in 2011. This study was approved by the Behavioural Research Ethics Board at the University of British Columbia, Canada.
Measures
The two main dependent variables were self-reported hypertension and diabetes. Respondents were asked: “Have you ever been diagnosed with high blood pressure?” (Y/N) and “Do you have diabetes?” (Y/N).
Independent variables were racial identity (Black / White), gender (female / male), and income. Black-White racial identity was obtained using similar questions over time (in 2001-2010: “People living in Canada come from many different cultural and racial backgrounds. Are you…”; in 2011-2013: “You may belong to one or more racial or cultural groups on the following list. Are you…”) with 12 options including “Black” and “White.” Income was obtained by asking “What is your best estimate of the total income received by all household members, from all sources, before taxes and deductions, in the past 12 months?” We used a derived variable of income produced by Statistics Canada to represent household income adjusted for household size in decile (1-10) form. Missing data on income were imputed by Statistics Canada for cycles 2005 and onwards.23
To further examine what might explain health inequalities at the intersections of racial identity, gender and income, we explored the mediating role of three common behavioral risk factors associated with hypertension and diabetes, namely overweight/obesity, smoking, and physical activity. We used derived variables produced by Statistics Canada for body mass index (BMI: <25 normal, 25-29.9, overweight, obese, >30), current smoking status (current smoker, former smoker, non-smoker), and frequency of leisure-related physical activity (inactive, somewhat active, very active).23
Control variables are survey year (2001-2013) and the sociodemographic variables: age (continuous); age squared (continuous); immigration status (born in Canada, immigrated 0-19 years ago, immigrated >20 years ago); marital status (married or common-law, never married, divorced, separated or widowed), and education (high school not completed, high school completed, some post-secondary education, post-secondary education completed.
Our preliminary sensitivity analyses indicated that a linear trend for the income decile variable was appropriate as logarithmic and squared terms did not produce a better model fit.
Statistical Analyses
We pooled data from ten cycles of the CCHS (2001, 2003, 2005, 2007, 2008, 2009, 2010, 2011, 2012, and 2013). We only included participants who were aged ≥25 years in order to obtain stable measures of education and income.
We engaged in a three-stage analytical process. First, we modeled three-way interaction terms between racial identity, gender, and income in hierarchically well-ordered logistic regression models executed on hypertension and diabetes in the full sample, controlling for survey year, age, age squared, immigration status, marital status, and education.24 To help interpret these interaction terms, we regressed hypertension and diabetes on income in each of four subgroups (Black women, Black men, White women, White men), controlling for the same sociodemographic variables, and produced predicted probabilities of hypertension and diabetes by income decile from these logistic regression models. Finally, we attempted to explain the income-related health inequalities that emerged in the second stage by additionally controlling for BMI, smoking status, and physical activity in our regression models.
Except for income (10.2%), all variables had a low amount of missing variables (mean = 1.1%; maximum = 4.3%). We therefore applied a listwise deletion approach to missing data. To account for the complex sampling design, we applied the master weight and 500 bootstrap replicate weights provided by Statistics Canada to our models, a strategy recommended by Statistics Canada to produce more accurate point estimates and standard errors, respectively. Predicted probabilities and their CIs were computed using the margins (atmeans) command in Stata. All statistical analyses were performed in Stata 13.25
Results
Characteristics of the Sample
The final sample comprised 3,502 Black women, 336,341 White women, 2,806 Black men, and 271,260 White men. Table 1 presents the unweighted distributions of study variables by race and gender. Participants were aged 54 years average (SD = 17). The proportions of all participants who reported being diagnosed with hypertension and diabetes were 24.7% and 8.1%, respectively. The mean income decile was 3.80 among Black women, 5.20 among White women, 4.50 among Black men, and 5.97 among White men. Differences in overweight/obesity (ie, lower proportion of obesity among Black men) are consistent with other prevalence studies in Canada.26
Table 1. Characteristics of the pooled sample, 2001-2013; unweighted data.
| Black | White | Missing | |||
| Women | Men | Women | Men | ||
| Variables | n (%) | n (%) | n (%) | n (%) | (%) |
| Total | 3,502 | 2,806 | 336,341 | 271,260 | |
| Hypertension | 839 (24.0) | 529 (18.9) | 87,605 (26.1) | 61,593 (22.8) | .2 |
| Diabetes | 303 (8.7) | 251 (8.9) | 24,936 (7.4) | 24,300 (9.0) | .1 |
| Income decile, mean (SD) | 3.80 (2.65) | 4.50 (2.77) | 5.20 (2.87) | 5.97 (2.83) | 10.2 |
| Age, mean (SD) | 45.9 (15.5) | 45.0 (14.1) | 49.3 (20.7) | 53.1 (16.2) | 0 |
| Immigration status | .2 | ||||
| Born in Canada | 680 (19.8) | 532 (19.2) | 300,014 (89.3) | 241,846 (89.3) | |
| Immigrated 0-19 years ago | 1,368 (39.9) | 1,185 (43.0) | 5,967 (1.8) | 4,997 (1.8) | |
| Immigrated ≥20 years ago | 1,382 (40.3) | 1,036 (37.6) | 29.877 (8.9) | 23.984 (8.9) | |
| Marital status | .2 | ||||
| Married or common-law | 1,436 (41.1) | 1,575 (56.3) | 189,286 (56.4) | 177,110 (65.4) | |
| Single / never married | 1,161 (33.2) | 807 (28.8) | 42,574 (12.7) | 49,743 (18.4) | |
| Divorced, separated or widowed | 897 (25.7) | 418 (14.9) | 103,895 (30.9) | 44,044 (16.3) | |
| Education | 1.1 | ||||
| High school not completed | 503 (14.5) | 379 (13.7) | 76,042 (22.9) | 61,342 (22.9) | |
| High school completed | 496 (14.3) | 445 (16.1) | 60,111 (18.0) | 43,064 (16.1) | |
| Some post-secondary education | 241 (7.0) | 186 (6.7) | 18,955 (5.7) | 15,490 (5.8) | |
| Post-secondary education completed | 2,221 (64.2) | 1,754 (63.5) | 178,004 (53.4) | 148,259 (55.3) | |
| BMI | 4.3 | ||||
| < 25 | 1,410 (44.3) | 1,151 (42.2) | 157,297 (50.0) | 93,139 (35.2) | |
| Overweight, 25-29.9 | 1,082 (34.0) | 1,166 (42.7) | 97,644 (30.8) | 115,196 (43.5) | |
| Obese, ≥30 | 690 (21.7) | 414 (15.2) | 61,794 (19.5) | 56,490 (21.3) | |
| Smoking status | .2 | ||||
| Current smoker | 321 (9.2) | 558 (19.9) | 70,332 (21.0) | 69,066 (25.5) | |
| Former smoker | 573 (16.4) | 840 (30.0) | 147,000 (43.8) | 141,244 (52.2) | |
| Never smoked | 2,602 (74.4) | 1,403 (50.1) | 118,353 (35.3) | 60,280 (22.3) | |
| Physical activity | 2.5 | ||||
| Not active | 589 (17.1) | 708 (25.7) | 69,646 (21.0) | 66,635 (25.6) | |
| Somewhat active | 715 (20.8) | 582 (21.1) | 84,429 (25.5) | 65,555 (25.2) | |
| Very active | 2,136 (62.1) | 1,468 (53.2) | 177,642 (53.6) | 128,441 (49.3) | |
Data are n (%) unless noted otherwise.
SD, standard deviation; BMI, body mass index
Inequalities in Hypertension and Diabetes: Intersections with Racial Identity, Gender, and Income
Table 2 and table 3 describe associations between income and the outcomes in the four subgroups before and after controlling for behavioral risk factors (Models 1 and 2, respectively). Point estimates represent the modified odds of being diagnosed with hypertension and diabetes given an increase of one decile in income. Comparisons of the odds ratios and the predicted probabilities’ 95% CI provide a conservative test of whether differences in estimates are statistically significant.
Table 2. Associations between income and self-reported hypertension.
| Black | White | |||||||
| Women | Men | Women | Men | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Model 1 | .86a | (.80, .92) | .99 | (.92, 1.06) | .95a | (.95, .96) | .98a | (.97, .99) |
| Model 2 | .87a | (.81, .95) | .97 | (.90, 1.04) | .97a | (.96, .98) | .98a | (.97, .99) |
a. Significant at α = .05.
Odds ratios should be interpreted as the modified odds of being diagnosed with hypertension for an increase of one decile in household income.
Model 1 controls for survey year, age, age squared, immigration status, marital status and education.
Model 2 additionally controls for body mass index, current smoking and physical activity.
Table 3. Associations between income and self-reported diabetes.
| Black | White | |||||||
| Women | Men | Women | Men | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Model 1 | .83a | (.75, .92) | .99 | (.91, 1.08) | .90a | (.89, .91) | .93a | (.92, .94) |
| Model 2 | .83a | (.74, .93) | .99 | (.90, 1.08) | .91a | (.90, .93) | .92a | (.91, .93) |
a. Significant at α = .05.
Odds ratios should be interpreted as the modified odds of being diagnosed with hypertension for an increase of one decile in household income.
Model 1 controls for survey year, age, age squared, immigration status, marital status and education.
Model 2 additionally controls for body mass index, current smoking and physical activity.
The three-way interaction term between racial identity, gender, and income on hypertension in the full sample was marginally significant (P = .056). Controlling for sociodemographic factors, a one-decile increase in income corresponded to slightly lower odds of being diagnosed with hypertension among White women (OR =.95, 95% CI .95; .96) and White men (OR = .98, 95% CI .97; .99). The results for Black Canadians were less straightforward. Controlling for socio-demographic factors, income was not significantly associated with hypertension among Black men (OR = .99, 95% CI .92; 1.06) but was strongly associated with hypertension among Black women (OR = .86, 95% CI .80; .92). Comparisons of odds ratios from Model 1 to Model 2 in Table 2 indicate that behavioral risk factors did little to explain these associations.
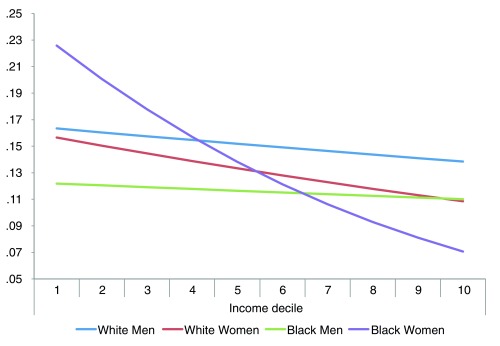
Figure 1 presents predicted probabilities of being diagnosed with hypertension by income decile with the other variables in Model 1 held at their mean values. The predicted probability of being diagnosed with hypertension in the lowest income decile was 22.6% (95% CI, 17.3, 27.8) for Black women, 15.7% (95% CI, 15.1, 16.2) for White women, 12.2% (95% CI, 7.2, 17.1) for Black men, and 16.3% (95% CI, 15.7, 17.0) for White men. Predicted probabilities in the highest income decile were 7.1% (95% CI, 4.0, 10.2) for Black women, 10.9% (95% CI, 10.5, 11.3) for White women, 11.0% (95% CI, 6.1, 15.9) for Black men, and 13.8% (95% CI, 13.3, 14.3) for White men. In other words, income was most strongly related to hypertension in the sample of Black women, with poor Black women being inordinately likely to report this chronic disease.
Figure 1. Predicted probabilities of being diagnosed with hypertension by income decile.
The three-way interaction term between racial identity, gender, and income on diabetes in the full sample was significant (P=.009). Controlling for sociodemographic factors, income was not significantly associated with diabetes (OR = .99, 95% CI (.91, 1.08) among Black men but was strongly associated with diabetes among Black women (OR = .83, 95% CI .75, .92). Relationships between income and diabetes were less strong for White women (OR = .90, 95% CI, .89, .91) and White men (OR = .93, 95% CI, .92, .94). Comparisons of odds ratios from Model 1 to Model 2 in Table 3 indicate that behavioral risk factors contributed little to explaining these associations.
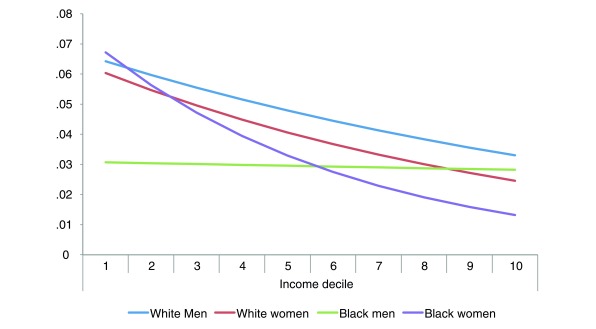
Figure 2 presents predicted probabilities of being diagnosed with diabetes by income decile, with the other variables in Model 1 held at their mean values. The predicted probability of being diagnosed with diabetes in the lowest income decile was 6.7% (95% CI, 3.8, 9.6) for Black women, 6.0% (95% CI, 5.7, 6.4) for White women, 3.1% (95% CI, 1.4, 4.7) for Black men, and 6.4% (95% CI, 6.0, 6.8) for White men. Predicted probabilities in the highest income decile were 1.3% (95% CI, .2, 2.4) for Black women, 2.5% (95% CI, 2.3, 2.6) for White women, 2.8% (95% CI, 1.1, 4.5) for Black men, and 3.3% (95% CI, 3.1, 3.5) for White men. In short, relationships between income and diabetes were moderately strong and in the expected directions for White women and men, strong and in the expected direction for Black women, and nonexistent for Black men.
Figure 2. Predicted probabilities of being diagnosed with diabetes by income decile.
Discussion
Intersectionality theory suggests that racial identity, gender, and income may be entwined with one another – and with indicators of health such as hypertension and diabetes – in unexpectedly complicated ways. To the degree this is true, examining the distinct effects of racial identity, gender, and income before or after controlling for one another can obscure the true nature of health inequalities in Canadian society. Our findings suggest that there are indeed no singular income effects on hypertension or diabetes: the particularities of the combinations of identities reported by Canadians shape their risks of hypertension and diabetes, and neither racial identity, gender, nor income can be isolated from one another in the patterning of them.
In regard to household income and likelihood of self-reported hypertension, we found a strong inverse relationship for Black women, a modest inverse relationship for White women, a weak inverse relationship for White men, and no relationship for Black men. The result for Black men in particular stands in contrast to an earlier study that reported a positive association between income and hypertension in this group.22 In regard to household income and likelihood of self-reported diabetes, we found a strong inverse relationship for Black women, fairly strong inverse relationships for White women and men, and no relationship for Black men.
Our results suggest that poor Black women in Canada experience a multiplicative jeopardy of hypertension that is higher than expected given the distinct jeopardies of being poor, being Black, and being women. These results are troubling in light of the economic inequalities that continue to negatively affect Black Canadians.26,27 In our models, BMI, smoking status, and physical activity failed to explicate the multiplicative jeopardy of hypertension experienced by poor Black Canadian women. Similar to American trends, it could be that poor Black women are more likely than poor White Canadians and poor Black men to be single parents, have long commutes to work, work at menial jobs, or lack access to quality health care.28,29 For instance, in the province of Nova Scotia, many Black Canadians live in rural settings with a limited health service infrastructure providing access to preventive measures that mitigate the development of health conditions such as hypertension.30-32 Enang notes that a high proportion of Black women in that province are not able to avail themselves of preventive health tests such as Pap smears, breast exams, and routine physical examinations; this may be especially true for poor Black women.33 These women may also encounter expectations to be strong role models for their families and others in the face of everyday racism and/or may have fewer resources to maintain resiliency in the face of racism.30,31
In regard to the absence of relationships between income and both health outcomes for Black Canadian men, similar results have been noted in the United States with regard to diabetes and hypertension among African Americans and Black Americans of Caribbean origin.6,34-37 Robbins and colleagues examined 1,800 Black American participants in the US National Health and Nutrition Examination Survey (NHANES III) and found no significant association between income and diabetes among African American men and a strong association between income and diabetes among African American women. They suggested that different experiences of obesity, stress, and depression could contribute to explaining these gender differences.34,35 In Canada, evidence suggests that Black women and men face a similar burden of discrimination in everyday life and the workplace.37 However, it might be the case that wealthy Black men work in more predominately White environments, which puts them at higher risk of experiencing unique kinds of health-damaging discrimination. That being said, the lack of a meaningful association between income and hypertension among Black men and White men suggests that this may be a male phenomenon more generally. Further research into the relative viability of these plausible explanations for our findings is clearly needed.
Limitations and Conclusion
We conclude by noting three key limitations. First, we acknowledge that the heuristic value of intersectionality theory in understanding the complex configurations producing social inequalities in health reaches far beyond the three dimensions of inequality (racial identity, gender, and income) studied here. Factors such as disability, sexuality, education, immigration status, and region of residence may also intersect with racial identity, gender, and/or income to predict health. Second, although self-reported hypertension and diabetes are often treated as valid surrogates of biometric measures, people with lower income and education more frequently underreport them, which can lead to an underestimate of the true strength of associations.38,39 This is especially problematic for our study if the underreporting of hypertension and diabetes among people of low socioeconomic standing is itself further patterned by racial identity and gender. This potential source of error might perhaps explain the lack of significant associations found among Black men in our study. Finally, the cross-sectional nature of our analysis means that we cannot rule out reverse causation (ie, that chronic illness influences income) or unobserved confounding in regard to the associations reported in this study.
We welcome future attempts to more conclusively establish the differential causal effects of income on hypertension and diabetes among the different groups formed by the intersection of race and gender.
References
- 1. Forouzanfar MH, Afshin A, Alexander LT, et al. ; GBD 2015 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659-1724. 10.1016/S0140-6736(16)31679-8 10.1016/S0140-6736(16)31679-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995-2005: a population-based study. Lancet. 2007;369(9563):750-756. 10.1016/S0140-6736(07)60361-4 10.1016/S0140-6736(07)60361-4 [DOI] [PubMed] [Google Scholar]
- 3. Padwal RS, Bienek A, McAlister FA, Campbell NR; Outcomes Research Task Force of the Canadian Hypertension Education Program . Epidemiology of Hypertension in Canada: an Update. Can J Cardiol. 2016;32(5):687-694. 10.1016/j.cjca.2015.07.734 [DOI] [PubMed] [Google Scholar]
- 4. Bird Y, Lemstra M, Rogers M, Moraros J. The relationship between socioeconomic status/income and prevalence of diabetes and associated conditions: A cross-sectional population-based study in Saskatchewan, Canada. Int J Equity Health. 2015;14(1):93. 10.1186/s12939-015-0237-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown K, Nevitte A, Szeto B, Nandi A. Growing social inequality in the prevalence of type 2 diabetes in Canada, 2004-2012. Can J Public Health. 2015;106(3):e132-e139. 10.17269/cjph.106.4769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walsemann KM, Goosby BJ, Farr D. Life course SES and cardiovascular risk: heterogeneity across race/ethnicity and gender. Soc Sci Med. 2016;152:147-155. 10.1016/j.socscimed.2016.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804-818. 10.1093/ije/dyr029 10.1093/ije/dyr029 [DOI] [PubMed] [Google Scholar]
- 8. Leenen FHH, Dumais J, McInnis NH, et al. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ. 2008;178(11):1441-1449. 10.1503/cmaj.071340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liu R, So L, Mohan S, Khan N, King K, Quan H. Cardiovascular risk factors in ethnic populations within Canada: results from national cross-sectional surveys. Open Med. 2010;4(3):e143-e153. [PMC free article] [PubMed] [Google Scholar]
- 10. Gasevic D, Ross ES, Lear SA. Ethnic Differences in Cardiovascular Disease Risk Factors: A Systematic Review of North American Evidence. Can J Cardiol. 2015;31(9):1169-1179. 10.1016/j.cjca.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 11. Veenstra G, Patterson AC. Black-White Health Inequalities in Canada. J Immigr Minor Health. 2016;18(1):51-57. 10.1007/s10903-014-0140-6 [DOI] [PubMed] [Google Scholar]
- 12. Veenstra G, Patterson AC. Health differences between native-born Black and White Canadians: Revisiting Lebrun and LaVeist (2011, 2013). Can Ethn Stud. 2015;47(3):163-176. 10.1353/ces.2015.0027 [DOI] [Google Scholar]
- 13. Chiu M, Austin PC, Manuel DG, Tu JV. Comparison of cardiovascular risk profiles among ethnic groups using population health surveys between 1996 and 2007. CMAJ. 2010;182(8):E301-E310. 10.1503/cmaj.091676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chiu M, Maclagan LC, Tu JV, Shah BR. Temporal trends in cardiovascular disease risk factors among white, South Asian, Chinese and black groups in Ontario, Canada, 2001 to 2012: a population-based study. BMJ Open. 2015;5(8):e007232. 10.1136/bmjopen-2014-007232 10.1136/bmjopen-2014-007232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Veenstra G. Racialized identity and health in Canada: results from a nationally representative survey. Soc Sci Med. 2009;69(4):538- 542. https://doi.org/ 10.1016/j.socscimed 2009.06.009. PMID:19560246. [DOI] [PubMed]
- 16. Hankivsky O. Women’s health, men’s health, and gender and health: implications of intersectionality. Soc Sci Med. 2012;74(11):1712- 1720. https://doi.org/ 10.1016/j.socscimed 2011.11.029. PMID:22361090. [DOI] [PubMed]
- 17. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10-17. https://doi.org/ 10.1016/j socscimed.2014.03.022. PMID:24704889. [DOI] [PubMed]
- 18. Brown TH, Richardson LJ, Hargrove TW, Thomas CS. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: the intersecting consequences of race, gender, SES, and age. J Health Soc Behav. 2016;57(2):200-222. 10.1177/0022146516645165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cummings JL, Brayboy Jackson P. Race, gender, and SES disparities in self-assessed health, 1974-2004. Res Aging. 2008;30(2):137-167. 10.1177/0164027507311835 [DOI] [Google Scholar]
- 20. Ailshire JA, House JS. The unequal burden of weight gain: an intersectional approach to understanding social disparities in BMI trajectories from 1986 to 2001/2002. Soc Forces. 2011;90(2):397-423. 10.1093/sf/sor001 10.1093/sf/sor001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Creatore MI, Moineddin R, Booth G, et al. Age- and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ. 2010;182(8):781-789. 10.1503/cmaj.091551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Veenstra G. Race, gender, class, sexuality (RGCS) and hypertension. Soc Sci Med. 2013;89:16-24. https://doi.org/ 10.1016/j. socscimed.2013.04.014. PMID:23726211. [DOI] [PubMed]
- 23. Canadian Community Health Survey (CCHS) Statistics Canada. Last accessed March 1, 2017 from http://www.statcan.gc.ca/imdb-bmdi/3226-eng.htm.
- 24. Jaccard J. Interaction Effects in Logistic Rregression. Thousand Oaks, CA: Sage. QASS #135; 2001. https://doi. org/ 10.4135/9781412984515. [DOI] [Google Scholar]
- 25. StataCorp Stata: Release 13. Statistical Software. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 26. Tremblay MS, Pérez CE, Ardern CI, Bryan SN, Katzmarzyk PT. Obesity, overweight and ethnicity. Health Rep. 2005;16(4):23-34. [PubMed] [Google Scholar]
- 27. Livingstone AM, Weinfeld M. Black families and socio-economic inequality in Canada. Can Ethn Stud. 2015;47(3):1-23. 10.1353/ces.2015.0026 [DOI] [Google Scholar]
- 28. National Council of Welfare (NCW) A Snapshot of Racialized Poverty in Canada. National Council of Welfare. 2012. Last accessed November 1 from http://www.esdc.gc.ca/eng/communities/reports/poverty_profile/snapshot.pdf.
- 29. Bureau of Labor Statistics (BLS), U.S. Department of Labor, The Economics Daily Occupational employment by race and ethnicity, 2011. Bureau of Labor Statistics (BLS), 2016. Last accessed March 1, 2017 from http://www.bls.gov/opub/ted/2012/ted_20121026.htm.
- 30. Kids Count Children in Single-Parent Families by Race. Kids Count. 2012. Last accessed November 1, 2016 from http://datacenter.kidscount.org/data/tables/107-children-insingle-parent-families-by#detailed/1/any/false/869,36,868,867,133/ 10,11,9,12,1,185,13/432,431.
- 31. Etowa J, Keddy B, Egbeyemi J, Eghan F. Depression: the ‘invisible grey fog’ influencing the midlife health of African Canadian women. Int J Ment Health Nurs. 2007;16(3):203-213. 10.1111/j.1447-0349.2007.00469.x 10.1111/j.1447-0349.2007.00469.x [DOI] [PubMed] [Google Scholar]
- 32. Etowa J, Wiens J, Bernard WT, Clow B. Determinants of Black women’s health in rural and remote communities. Can J Nurs Res. 2007;39(3):56-76. [PubMed] [Google Scholar]
- 33. Enang J. Black women’s health: A synthesis of health research relevant to Black Nova Scotians. Maritime Centre of Excellence for Women’s Health. 2001. Last accessed November 1, 2016 from https://www.dal.ca/content/dam/dalhousie/pdf/ace-womenhealth/ACEWH_health_research_relevant_to_black_nova_scotian_women.pdf.
- 34. Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and type 2 diabetes in African American and non-Hispanic white women and men: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2001;91(1):76-83. 10.2105/AJPH.91.1.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Robbins JM, Vaccarino V, Zhang H, Kasl SV. Excess type 2 diabetes in African-American women and men aged 40-74 and socioeconomic status: evidence from the Third National Health and Nutrition Examination Survey. J Epidemiol Community Health. 2000;54(11):839-845. 10.1136/jech.54.11.839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bidulescu A, Francis DK, Ferguson TS, et al. ; U.S. Caribbean Alliance for Health Disparities Research Group (USCAHDR) . Disparities in hypertension among black Caribbean populations: a scoping review by the U.S. Caribbean Alliance for Health Disparities Research Group (USCAHDR). Int J Equity Health. 2015;14(1):125. 10.1186/s12939-015-0229-0 10.1186/s12939-015-0229-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chui T, Maheux H. Women in Canada: A gender-based statistical report--Visible minority women. Component of Statistics Canada Catalogue no. 89-503-X. 2016. Last accessed March 1, 2017 from http://www.statcan.gc.ca/pub/89-503-x/2010001/article/11527-eng.pdf.
- 38. Tenkorang EY, Sedziafa P, Sano Y, Kuuire V, Banchani E. Validity of Self-Report Data in Hypertension Research: Findings From The Study on Global Ageing and Adult Health. J Clin Hypertens (Greenwich). 2015;17(12):977-984. 10.1111/jch.12616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yuan X, Liu T, Wu L, Zou ZY, Li C. Validity of self-reported diabetes among middle-aged and older Chinese adults: the China Health and Retirement Longitudinal Study. BMJ Open. 2015;5(4):e006633. 10.1136/bmjopen-2014-006633 [DOI] [PMC free article] [PubMed] [Google Scholar]