Abstract
A 77-year-old male underwent open repair for a right indirect inguinal hernia and complained of right scrotal pain on the third postoperative day. Color Doppler imaging revealed decreased blood flow with heterogeneous hypoechogenicity in the right testis. A Tc-99m pertechnetate testicular scan showed diffuse hyperemia and increased uptake in the right scrotum. Additional SPECT/CT revealed a photon defect in the right testicle with increased uptake in the peri-testicular area. A subsequent operation revealed a large hematoma in the right spermatic cord and consequent right testicular infarction, and right orchiectomy was performed.
Keywords: SPECT/CT, Tc-99m pertechnetate, Testicular infarction, Testicular scan
The patient’s urologists decided on a diagnostic and therapeutic operation. During surgery, the right spermatic cord was seen to be compressed by a large hematoma with fluid and showed severe inflammatory changes. The right testicle and epididymis were a dark-brown to black color, suggesting hemorrhagic and necrotic changes. Right orchiectomy was done and histological examination revealed a necrotic testis. The blood vessels were congested and showed evidence of thrombus (Figs. 1 and 2).
Fig. 1.
A 77-year-old male underwent open repair for a right indirect inguinal hernia with prosthetic mesh. On the third postoperative day, the patient developed right scrotal swelling and pain. On physical examination, the right scrotum was enlarged and the right lower inguinal area was swollen with bluish discoloration. A testicular ultrasonography demonstrated both hydroceles. Color Doppler imaging revealed decreased blood flow with heterogeneous hypoechogenicity in the right testis (a). Normal blood flow was detected in the left testis (b). However, torsion knot was not found in the right spermatic cord
Fig. 2.
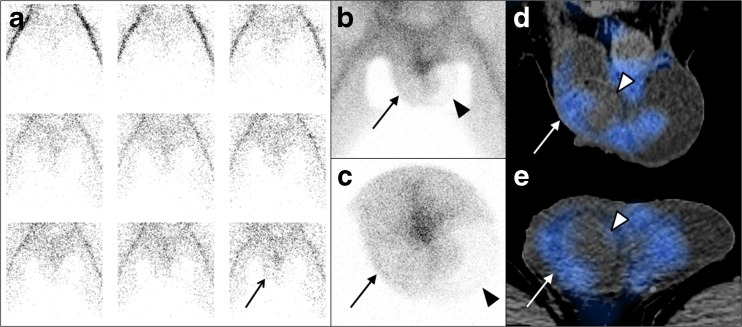
The patient was referred for a Tc-99m pertechnetate testicular scan. The flow phase showed mild and diffuse hyperemia in the right scrotum (a, arrow). A blood pool image at 5 min after injection (b) and a pinhole image at 10 min (c) also showed increased activity in right testis (arrows); this finding was not consistent with those of ultrasonography. Additional SPECT/CT was performed for differential diagnosis. Coronal and axial images of SPECT/CT showed a photon defect in the right testicle (arrow heads) with increased curvilinear tracer uptake in the peri-testicular area (white arrows) (d, e). These findings were consistent with right testicular infarction with peri-testicular hyperemia due to reactive changes such as inflammation
Global and segmental testicular infarctions are recognized consequences of torsion of the spermatic cord, incarcerated hernia, infection, trauma, vasculitis, sickle cell disease, hypercoagulable states, and inguinal hernia repair [1–4]. Although ultrasound is the imaging modality of choice for the evaluation of acute scrotal pain, testicular scintigraphy has proven to be reliable and accurate in reflecting acute testicular ischemia as well as chronic ischemia and infarction [5–7]. Tc-99m pertechnetate testicular SPECT/CT study generally would not be performed in emergency situations. However, SPECT/CT could provide more detailed information about the state of blood flow, as seen in this case. To the best of our knowledge, this is the first documented case of SPECT/CT findings in a patient with testicular infarction. This case highlights the usefulness of SPECT/CT to diagnose testicular infarction in a patient with uncertain findings on the testicular scans.
Acknowledgements
This paper was supported by Wonkwang University in 2016.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Saxon P, Badler RL, Desser TS, Tublin ME, Katz DS. Segmental testicular infarction: report of seven new cases and literature review. Emerg Radiol. 2012;19:217–23. doi: 10.1007/s10140-011-0999-7. [DOI] [PubMed] [Google Scholar]
- 2.Bilagi P, Sriprasad S, Clarke JL, Sellars ME, Muir GH, Sidhu PS. Clinical and ultrasound features of segmental testicular infarction: six-year experience from a single centre. Eur Radiol. 2007;17:2810–8. doi: 10.1007/s00330-007-0674-2. [DOI] [PubMed] [Google Scholar]
- 3.Kim W, Rosen MA, Langer JE, Banner MP, Siegelman ES, Ramchandani P. US MR imaging correlation in pathologic conditions of the scrotum. Radiographics. 2007;27:1239–53. doi: 10.1148/rg.275065172. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf G, Sellars ME, Kooiman GG, Diaz-Cano S, Sidhu PS. Global testicular infarction in the presence of epididymitis: clinical features, appearances on grayscale, color Doppler, and contrast-enhanced sonography, and histologic correlation. J Ultrasound Med. 2013;32:175–80. doi: 10.7863/jum.2013.32.1.175. [DOI] [PubMed] [Google Scholar]
- 5.Dunn EK, Zinn DL, Sarkar SD, Strashun AM. Oversized “bullseye” with central activity. a scintigraphic appearance of hemorrhagic testicular infarct following traumatic rupture of the testicle. Clin Nucl Med. 1993;18:786–8. doi: 10.1097/00003072-199309000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Nagle C, Clark K, Browning D, Howard R, Murphy J. Testicular ischemia and infarction following herniorrhaphy or varicocelectomy: evaluation by radionuclide imaging. Clin Nucl Med. 1989;14:243–8. doi: 10.1097/00003072-198904000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Vieras F. Evolution of acute epididymitis to testicular infarction. scintigraphic demonstration. Clin Nucl Med. 1986;11:158–60. doi: 10.1097/00003072-198603000-00004. [DOI] [PubMed] [Google Scholar]