Abstract
The present study aimed to analyze the impacts of a low back rehabilitation program accompanied with neck, shoulder and upper back exercises on pain, disability, and physical characteristics of patients with chronic low back pain. Twenty sedentary male patients with chronic low back pain participated in the study on a voluntary basis. The patients were randomly allocated into two groups: a conventional low back exercise group (CE) and a supported exercise group (SE; CE plus upper back, neck, and shoulder exercises). The Modified Oswestry Disability Questionnaire (MODQ) was used to evaluate the disability status and the Visual Analog Scale (VAS) was used to identify the pain states of the patients. In addition, neck, lumbar and shoulder isokinetic and isometric strengths of the patients were evaluated. The CE group performed lumbar stretching, mobilization and stabilization exercises in addition to low-back and abdominal isometric and concentric strengthening exercises. The SE group performed static stretching and isotonic exercises for the neck, upper-back, and shoulder muscles, in addition to the exercises performed in CE group. The exercises were implemented 3 days a week for 6 weeks in both groups. Following the 6-week exercise periods in both groups, statistically significant (p < 0.01) improvements were observed in the patients’ levels of pain and the scores of MODQ reflecting an easing of disability. With respect to the levels of pain and disability, the improvements observed in the SE group was significantly (p < 0.01) greater than the improvement observed in the CE group. Based on the findings of this study, we can conclude that a low back exercise program used in combination with neck, shoulder and upper back exercises reduces the level of pain and disability in patients with chronic low back pain more prominently than conventional low back exercises.
Key points.
The exercises applied to the upper part of the spinal muscular kinetic chain contribute to the relief of pain and disability in patients with chronic low back pain.
Neck, upper back, and shoulder exercises may enhance to the rehabilitation of patients with chronic low back pain.
Key words: Chronic back pain, back and neck exercises, pain, disability
Introduction
Low back pain, which affects individuals of all ages and socio-economic levels, is a crucial public health issue owing to the loss of labor and the ever-increasing health care costs associated with its presentation (Majid and Truumees, 2008). It has been estimated that the direct cost burden of low back pain leading to loss of labor, indirect additional costs, and loss of productivity is approximately $86 billion in United States (Ivanova et al., 2011).
Since a certain etiological risk factor cannot be identified, non-specific mechanical low back pain is the most common issue in 90% of the affected patients (Henschken et al., 2009). In treating chronic low back pain, analgesics, physical agents, nerve blockade, and acupuncture are the preferred options. However, the efficiency of these treatment agents still remains unclear (Artus et al., 2010; Huntoon and Burgher, 2008).
Exercise is one of the most frequently used treatment option, either alone or combined with other methods. It is recognized with a high level of evidence as being effective in treating patients with chronic low back pain (Airaksinen et al., 2006; Mannion et al., 2001). Various randomized controlled studies have revealed that low back exercises reduce the level of pain and improve the functional state of patients with chronic low back pain (Airaksinen et al., 2006; Petersen et al., 2002). Several type of exercises, such as aerobic exercises, dynamic and isometric flexion or extension exercises, stretching, stabilization, and balance and coordination exercises, are used to achieve these outcomes (Lizier et al., 2012; van Middelkoop et al., 2011). However, the identification of exercises that are more effective and the best exercise intensity, frequency, and duration to use in patients with chronic low back pain remains conflicting in the literature (Henchoz and Kai-Lik So, 2000).
Many researchers stated that one of the hallmark characteristics of non-specific chronic low back pain is the weakness of the spinal musclar chain (Ito et al., 1996; McKeon et al., 2006). Furthermore, Alaranta et al. (1995) reported that individuals with a poor back extensor muscle strength, have three times greater low back pain scores than those with normal muscle strength. Henchoz and and Kai-Lik So (2000) stated that strength and resistance training aimed at improving the spinal muscles, particularly body extensor muscles, is effective in protecting individuals from low back pain. According to De Ridder et al. (2013), these results reveal the importance of strength and endurance condition of the back muscles, and the criticality of the balance among low back, upper back and hip extensor muscles.
The relationship between the weakness of the hip extensor group, which is the lower part of the spinal muscular kinetic chain, and low back pain in patients with chronic low back pain is emphasized in a number of studies (Ferguson et al., 2004; Pirouzi et al., 2006; Plamondon et al., 2004). As a result, exercises aimed at the hip extensor group are still being implemented in rehabilitation protocols for non-specific chronic low back pain (Burns et al., 2011; Lemaire et al., 2013). In addition to the lower part of the spinal muscle chain in studying the upper part of this chain, Sunget al. (2009) and Sung (2013) stated that the average electromyography (EMG) frequency of the thoracic part of the erector spinae muscles of patients with chronic low back pain is significantly lower with respect to the lumbar part than that of healthy individuals with no chronic low back pain. They also emphasized that the insufficiency observed in the thoracic part of the erector spinae should be taken into account in rehabilitation strategies geared towards patients with low back pain.
As part of the routine exercises implemented in patients with chronic back pain, no detailed exercise is implemented for the upper part of the spinal muscle chain, such as the rhomboid, trapezius, or cervical part. Considering the spinal muscular kinetic chain in the light of EMG study results, strengthening exercises implemented in the upper part of the chain can be considered to contribute positively to the kinetic chain, which is similar to the impact of strengthening exercises implemented in the lower part of the kinetic chain. In our literature review, no study has investigated the combination of neck, shoulder and upper back exercises in patients with chronic low back pain and the impact of this treatment on pain and disability to date.
In the light of the information provided above, the present study intends to analyze the impacts of a low back rehabilitation program accompanied by neck, shoulder and upper back exercises on pain and disability in patients with chronic low back pain.
Methods
Twenty male patients who visited the Sports Medicine Department outpatient clinic of Uludag University Medical Faculty with complaints of low back pain were involved in this study on a voluntary basis. The patients were categorized into two groups via draw lot (Oaks, 2012). The first group was identified as the conventional low back exercise (CE) group and the second group as the low back exercise supported by upper back, neck, and shoulder exercises (SE) group. Prior to the study, the volunteers were subjected to a detailed general physical examination, including examinations with respect to the cardiovascular and musculoskeletal systems. Patients with acute back pain, those with surgical history, and those requiring further examination and treatment based on the clinical examination findings were excluded from the current study. The patients were informed about the study in detail and asked to sign a voluntary informed consent form approved by the Uludag University Faculty of Medicine, Ethical Board of Medical Studies (Decision no: 2014-3/2).
The heights of the subjects were measured using an anthropometry kit (CPM anthropological instruments; Siber Hegner Maschinen AG, Zurich, Switzerland), which is capable of measuring to a sensitivity of 1 mm; their weight was measured using the Tanita BC-418 segmental body composition analysis instrument (Tanita Corporation of America, Inc., Arlington Heights, IL, USA), which is capable of measuring to a sensitivity of 100 g, while they were wearing only sports clothes. Additionally, the participants’ finger-to-ground distance (FGD) values were measured and recorded using an FGD measurement instrument capable of measuring to a sensitivity of 0.5 cm (TKK 1860; Takei Scientific Instruments Co., Ltd, Niigata City, Japan). The patients were also asked to fill out a Visual Analog Scale (VAS) form and Modified Oswestry Disability Questionnaire (MODQ)(Figure 1).
Figure 1.
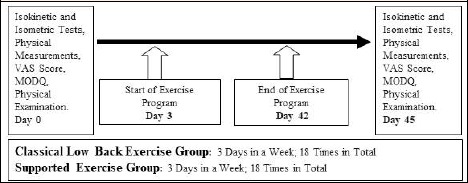
Study Plan. VAS: Visual Analog Scale, MODQ: Modified Oswestry Disability Questionnaire
Tests and testing procedure
The patients were asked to complete static stretching exercises for the neck, back, low back, hip, and pelvic muscles after a warm-up of 10 minutes on a cycle ergometer. Isokinetic strength measurements were performed with the Humac NORM isokinetic test and rehabilitation system (CSMI Computer Sports Medicine, Inc., Stoughton, MA, USA). After positioning the patients according to the angles and heights specified in the “Patient Setup” section of the Humac NORM program, gravity correction was performed for each measurement. Prior to the tests, the patients were directed to perform two trials in each angular speed to ensure maximum alignment with the test applications. The patients were verbally encouraged during the tests.
Lumbar Strength Test: Using an isokinetic dynamometer in the trunk extension-flexion modular component, the joint range of motion was adjusted to 10° extension and 80° flexion with reference to the anatomical zero position. The tests were implemented as follows: a) isometric strength of the back extensor and flexor muscles, three repetitions for each of directions at 60° flexion; and b) isokinetic concentric muscle strength of the back extensor and flexor muscles, three repetitions at 60°/s angular speed and 16 repetitions at 120°/s angular speed.
Shoulder Abduction and Shoulder Horizontal Abduction Strength Tests: Gravity corrections were performed at 80° abduction and 60° horizontal abduction by stabilizing the dynamometer lever (Camargo et al., 2010). After two sub-maximal attempts, isometric muscle strength tests were applied with three repetitions at 30° shoulder abduction, and isokinetic concentric strength tests were applied with three repetitions at 60°/s angular speed and 16 repetitions at 120°/s angular speed.
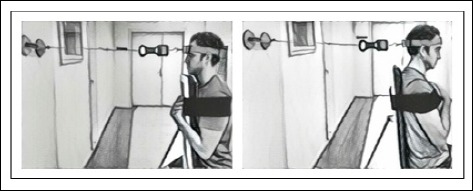
Isokinetic Neck Strength Test: The dynamometer height was determined as level 5, rotation degree as 40°, dynamometer chair back angle as 0°, rotation degree as 40°, front/back position as level 0, and monorail distance as level 23. Each participant assumed a face-down position, and the dynamometer shaft rotation axle was positioned such that it would pass through the middle of the line between the C7 spinous process and the sternal notch (Cagnie et al., 2007). The dynamometer was positioned such that the knee/hip adapter was positioned at the back of the head. The patients were stabilized using a stabilizing belt placed on the patients’ back (Figure 2).The position at which the patients were parallel to the ground was considered to be anatomic zero, and gravity correction was performed. The starting position was determined as 20° neck extension and the ending position as 30° neck flexion. Following two sub-maximal attempts, the isokinetic concentric muscle strengths of the flexor and extensor muscles were measured with three repetitions at 60°/s angular speed and 16 repetitions at 90°/s angular speed. The test was repeated with a week apart in 11 patients to evaluated the reliability and intraclass correlation coefficients (ICC, r) for the isokinetic concentric strength measurements in the cervical flexor and extensor muscles were found as r = 0.79-0.91.
Figure 2.

Isokinetic neck strength test.
Isometric Neck Strength Test: The Fladen digital hand scale with a measurement sensitivity of 10 g (Fladen Outdoor Digital Scale, 25 kg; Fladen Ab. Varberg, Sweden) was used in the isometric test measurement. A sit-up chair was positioned vertically at 90°. The patients were positioned with their heads, necks, and body in the neutral position and hip and knee at 90° flexion (Ylinen et al., 1999; Naish et al., 2013). The patients were stabilized using a stabilizing belt (Figure 3). With their heads in the neutral position, the patients were asked to apply isometric strength with maximal force for 5 seconds. Three measurements were completed with intervals of 20 seconds. The figures were read in kilograms, and the highest figure of the three measurements was obtained and recorded. The test was repeated with a week apart in 11 patients to evaluated the reliability and the ICCs were found (r = 0.92-0.95) within a high reliability range.
Figure 3.
Isometric neck strength test.
Conventional and Supported Low Back Exercise Programs: The identified exercise programs were implemented by the same exercise specialist 3 days per week, for 6 weeks. For the isotonic exercises, the OMNI Resistance Exercise Scale (RES) (Robertson et al., 2003), which is used as an effort scale for resistance exercises to determine the initial weight and the weekly weight increases of users, was used. The initial weight was determined as the weight corresponding to level 8 according to the effort scale in OMNI-RES resistance exercises. Each week, the weight was increased to the highest amount the patient could tolerate.
The CE group performed the conventional stretching, isometric back exercises, mobilization, stabilization, and back and abdominal concentric strengthening exercises 3 days per week for a period of 6 weeks. In week 1, the patients performed stretching, isometric back, and mobilization exercises. Following 10 minutes of warm-up on a cycle ergometer, static stretching exercises for the back, hip, and pelvic muscles were applied (Figure 4a). Static stretching exercises were repeated twice at the pain limit and for 30 seconds. In week 2, stabilization, back, and abdominal concentric strengthening exercises (Figure 5a) were started, in addition to stretching, isometric back and mobilization exercises. The exercises were consecutively performed with 5-second intervals and 30-minute breaks between each set (Table 1).
Figure 4.
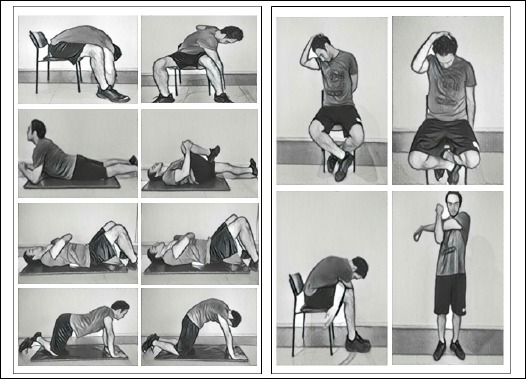
Stretching, mobilization, and isometric exercises.
Figure 5.

Lumbar stabilization exercises, (a) abdominal and lumbar concentric exercises, and (b) isotonic neck, shoulder, and back exercises.
Table 1.
Exercise program of the conventional (CE) and upper body supported (SE) groups
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | ||
|---|---|---|---|---|---|---|---|
| CE and SE | Stretching Exercises | 20 Seconds; 2 Repetitions |
20 Seconds; 2 Repetitions |
20 Seconds; 2 Repetitions |
20 Seconds; 2 Repetitions |
20 Seconds; 2 Repetitions |
20 Seconds; 2 Repetitions |
| Isometric Exercises | 2 Sets; 6 Repetitions |
2 Sets; 8 Repetitions |
2 Sets; 10 Repetitions |
2 Sets; 12 Repetitions |
2 Sets; 12 Repetitions |
2 Sets; 12 Repetitions |
|
| Dynamic Exercises | - | 2 Sets; 6 Repetitions |
2 Sets; 8 Repetitions |
2 Sets; 10 Repetitions |
2 Sets; 12 Repetitions |
2 Sets; 12 Repetitions |
|
| SE Group | Resistance Exercises | - | At level 8 according to OMNI-RES | Tolerable increase | Tolerable increase | Tolerable increase | Tolerable increase |
The SE group performed static stretching and isotonic exercises intended for the neck, back, and shoulder muscles, in addition to the exercises completed by the CE group. In week 1, back, neck, and shoulder stretching exercises and isometric back and mobilization exercises (Figures4a-b) were performed. In week 2, back stabilization, low back and abdominal concentric strengthening exercises (Figure 5a) and neck, back, and shoulder isotonic exercises (Figure 5b) were also started, in addition to the stretching, isometric back, and mobilization exercises (Table 1).
Statistical analysis
Statistical analysis was performed using the SPSS version 16.0 (SPSS, SPSS Inc, Chicago, IL, USA) software. The statistical significance level was set at p < 0.05.To evaluate the normality of the distribution of all data, the Shapiro-Wilk test was implemented. To compare the values in the groups before and after the exercises, the non-parametric Wilcoxon matched pair test was used. Additionally, for comparing statistical differences between the groups, the non-parametric Mann-Whitney U test was used. The ICC was calculated to assess the reliability of the neck isokinetic and isometric test measurements. The reliability was judged in accordance with the following established criteria: 0.90-0.99, high reliability; 0.80-0.89, good reliability; 0.70-0.79, moderate reliability; and <0.69, poor reliability.
Results
Physical characteristics of the patients
No statistically significant differences in the body mass index, body fat percentage, and pain duration were observed between the groups before the exercises (Table 2).
Table 2.
Participants’ physical characteristics and pain duration. Data are means (SEM).
| SE (n = 10) | CE (n = 10) | |
|---|---|---|
| Age (y) | 24.7 (.4) | 25 (.8) |
| Height(m) | 1.78 (.01) | 1.75 (.09) |
| Weight (kg) | 74.4 (3.2) | 70.6 (2.3) |
| BMI (kg·m-2) | 23.4 (1.0) | 22.9 (.6) |
| BFP | 11.8 (1.4) | 12.5 (1.7) |
| PD (month) | 31.8 (6.4) | 30.6 (5.4) |
SEM: Standard error means; SE: Supported exercise group; CE: Conventional exercise group; BMI: Body mass index; BFP: Body fat percentage; PD: Pain duration.
Isometric test results
The low back isometric flexion and extension peak torques, shoulder isometric abduction peak torque, and neck isometric flexion and extension strengths significantly (p < 0.01) increased in the SE group after the exercise intervention (Table 3). In the CE group, statistically significant (p < 0.01) increase was observed in the low back isometric extension peak torque following the exercise program. Right shoulder abductor, and neck isometric flexion and extension strength values in SE group were greater (p < 0.01) compared with the values of CE group following the interventions. Furthermore, a significantly (p < 0.001) higher improvement in the left shoulder abductor strength value was also observed in the SE group compared with the CE group after the exercise.
Table 3.
Lumbar, shoulder, and neck isometric test results. Data are means (SEM).
| CE (n = 10) | SE (n = 10) | ||
|---|---|---|---|
| 60° Isometric Lumbar Flexion PT (Nm) | BE | 170(14) | 161(11) |
| AE | 173(11) | 194(12)** | |
| 60° Isometric Lumbar Extension PT (Nm) | BE | 286(19) | 316(25) |
| AE | 351(21)** | 416(25)** | |
| 30° Isometric Right Shoulder Abduction PT (Nm) | BE | 52.9 (3.8) | 58.3 (3.7) |
| AE | 52.9 (2.1) | 71.5 (3.7)**˒†† | |
| 30° Isometric Left Shoulder Abduction PT (Nm) | BE | 50.4 (3.1) | 55.3 (3.4) |
| AE | 50.8 (2.1) | 68.5 (3.1)**˒††† | |
| Isometric Neck Flexion (kg) | BE | 14.4 (1.0) | 14.7 (.9) |
| AE | 15.6 (1.1) | 19.4 (.6)**˒†† | |
| Isometric Neck Extension (kg) | BE | 19.5 (.9) | 19.6 (.7) |
| AE | 20.3 (.9) | 24.7 (.5)**˒†† | |
SEM: Standard error means; SE: Supported exercise group; CE: Conventiona exercise group; BE: Before exercise; AE: After exercise; PT: Peak torque
** p < 0.01: statistical significance level within groups before and after exercise
†† p < 0.01
††† p < 0.001: statistical significance level between groups.
Isokinetic test results
The low back extensor peak torques and total works at 60°/s and 120°/s angular speeds, flexor peak torque and flexor total work at 60°/s angular speed were significantly (p < 0.01) increase in the SE group. A statistically significant (p < 0.05) increase in the flexor peak torque at 120°/s angular speed was also observed in the SE group after the exercise. The low back flexor total work values in the SE group were significantly (p < 0.05) greater compared with those observed in the CE group after the exercise.
Except for the left shoulder abductor strength values at 120°/s angular speed, all shoulder abductor and horizontal abductor peak torques and total works significantly (p < 0.01) increased in the SE group after exercise (Table 4). Those changes in the SE group were also significantly (p < 0.001) greater compared with those observed in the CE group.
Table 4.
Lumbar, shoulder, and neck isokinetic test results. Data are means (SEM).
| CE (n = 10) | SE (n = 10) | ||||||
|---|---|---|---|---|---|---|---|
| 60°PT(Nm) | 120°PT(Nm) | TW (J) | 60°PT(Nm) | 120°PT(Nm) | TW (J) | ||
| Isokinetic Lumbar Flexion (Nm) | BE | 154(7) | 131 (7.6) | 1982(108) | 143 (8.4) | 121 (8.8) | 1643(138) |
| AE | 156 (7.9) | 128 (7.1) | 2094(122) | 179 (9.7)** | 149 (9.9)* | 2279(189)**˒† | |
| Isokinetic Lumbar Extension (Nm) | BE | 257 (20.3) | 216.6 (17.6) | 3201(283) | 256 (24.5) | 215 (21.2) | 3120(336) |
| AE | 314 (18.9)** | 265 (15.6)** | 4094(324)** | 334 (23.6)** | 272 (22.9)** | 4120(371)** | |
| Right Shoulder Abduction PT (Nm) | BE | 47.2 (2.4) | 48.3(2) | 658(81) | 47.6 (2.3) | 49.4 (2.4) | 671(91) |
| AE | 43.8 (1.1) | 45.8 (1.9) | 619(67) | 70 (4.4)**˒††† | 66.2 (2.4)**˒††† | 1153(93)**˒††† | |
| Left Shoulder Abduction PT (Nm) | BE | 42.2 (2.5) | 48.9 (1.4) | 437(41) | 46.5 (2.2) | 51 (1.6) | 578(44) |
| AE | 41.4 (1.7) | 48.4(2) | 448(48) | 63(3.8)**˒††† | 58.2(3)† | 1068(72)**˒††† | |
| Right Shoulder Horizontal Abduction PT (Nm) | BE | 51 (2.3) | 45.3 (2.7) | 663(57) | 53.8 (3.4) | 45.7 (2.5) | 561(54) |
| AE | 50.5 (2.9) | 43.4(2) | 606(50) | 75(5)**˒†† | 66.9(3.1)**˒††† | 839(67)**˒† | |
| Left Shoulder Horizontal Abduction PT (Nm) | BE | 49.2 (3.1) | 45.3(3) | 667(55) | 51.6 (3.4) | 47.1 (2.6) | 647(61) |
| AE | 49.1 (3.2) | 46.9 (2.7) | 674(60) | 71(3.6)**˒††† | 68.7(4)**˒††† | 905(71)**˒† | |
| 60°PT(Nm) | 90°PT(Nm) | TW(J) | 60°PT(Nm) | 90°PT(Nm) | TW(J) | ||
| Neck Flexion(Nm) | BE | 31.5 (2.1) | 15.5 (1.2) | 272 (16.9) | 30.9 (1.6) | 17.6 (1.0) | 287(8.6) |
| AE | 32.7 (2.3) | 18.1 (1.4) | 291 (16.3) | 40.2 (1.3)**˒†† | 23.6 (1.4)*˒†† | 344 (11.5)**˒† | |
| Neck Extension (Nm) | BE | 43.9 (2.6) | 25 (1.4) | 378 (27.3) | 41.1 (2.6) | 26.7 (1.7) | 355 (23.7) |
| AE | 45.9 (2.8) | 28.6 (2.4) | 408.1 (22.8) | 60.3 (2.9)**˒†† | 38.9 (1.9)**˒†† | 493 (22.2)**˒† | |
SEM: Standard error means; SE: Supported exercise group; CE: Conventional exercise group; BE: Before exercise; AE: After exercise; 60°: 60°/s velocity; 90°: 90°/s angular velocity; 120°: 120°/s angular velocity; TW: Total Work; PT: Peak torque; n: Number of patients
* p < 0.05
** p < 0.01; statistical significance level with in groups before and after exercise
† p< 0.05
††p < 0.01
††† p < 0.001: statistical significance level between groups.
The isokinetic neck flexor values at 90°/s angular speed significantly improved (p < 0.05) in the SE group after the exercise as well as all the other neck isokinetic concentric strength and total work values (p < 0.01) (Table 4). A statistically significant (p < 0.01) increase was determined in both the flexor and extensor values at 60°/s and 90°/s angular speeds in the SE group compared with the CE group. Similarly, a statistically significant (p < 0.05) increase in the flexor and extensor total work values were observed after the exercise in the SE group compared with those observed in the CE group.
Clinical findings
Statistically significant (p < 0.01) improvements in the fingertip-to-floor distance and VAS scores were noted in both groups after the exercise. Further, the decreased post-exercise VAS score in the SE group was statistically significant (p < 0.01) compared with that observed in the CE group (Figure 6).
Figure 6.
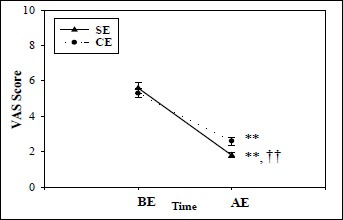
Change in the VAS scores. VAS: Visual Analog Scale; SE: Supported exercise group; CE: Classical exercise group; BE: Before exercise; AE: After exercise; ** p < 0.01: statistical significance level within groups before and after exercise; †† p < 0.01: statistical significance level between groups.
Similarly, decrease in the percent change of the MODQ score determined in the SE group after the exercise was a statistically significant (p < 0.001) compared with that determined in the CE group (Figure 7).
Figure 7.

Percent change in the MODQ scores. MODQ: Modified Oswestry Disability Questionnaire; SE: Supported exercise group; CE: Conventional exercise group; BE: Before exercise; AE: After exercise; **p<0.01: statistical significance level within groups before and after exercise; ††p<0.001: statistical significance level between groups.
Discussion
Weakness in the spinal muscular kinetic chain is related to low back pain. The exercises for different parts of spinal kinetic chain such as low back and hip extensors are frequently used in non-specific chronic low back pain rehabilitation programs (Lemaire et al., 2013; Pirouzi et al., 2006). De Ridder et al. (2013) stated that an adequate balance among the low back, thorax, and hip extensors is critical for the well-being of the back muscle chain, and emphasized that the hip extension strength being in the lower part of the kinetic chain is important for lumbar health.
Previous studies (Sung et al., 2009; 2013) showed that patients with the chronic low back pain have lower average EMG frequencies in the thoracic part of the erector spinae muscles compared with the lumbar part. Therefore the authors have suggested that the thoracic part of the erector spinae should be taken into account in rehabilitation strategies. However, we could not find any study in the current literature that investigated the impact of combined neck and back exercises on pain and disability in patients with chronic low back pain.
It is very well known that the lumbar muscle strength weakness results in an early fatigability in the patients with chronic back pain (Coorevits et al., 2008; Dixit et al., 2007; Ito et al., 1996). Miltner et al. (2001) investigated the effects of exercises on the lumbar extensors in patients with chronic low back pain and reported that the exercises are affective on pain, range of motion, spinal condition and back extensors’ strength with significant improvements. Our findings of 23-25% improvements in the lumbar strength in the CE group are similar to the findings of other studies (Bronfort et al., 2011; Calmels et al., 2004; Durmus et al., 2014; Moon et al., 2013; Rissanen, et al., 1995). In the SE group, which performed upper body exercises in addition to the conventional home exercise program, an average increase of 34% in lumbar isometric extension strength and 29% to 32% in lumbar isokinetic extension peak torque strength were observed. The strength increase in the extensor muscles in the SE group was non-significantly greater than the CE group. Therefore, it can be concluded that the upper body supported exercises used in the study are contribute to the low back extensor strength.
Tarnanen et al. (2008) examined the impact of isometric contraction of the shoulder on the lumbar muscle activities. They observed that the surface EMG activities of the longissimus and multifidus muscles during a maximal isometric lumbar extension together with shoulder isometric horizontal abduction were greater by 69% to 84% compared with the maximal isometric lumbar extension alone. Tarnanen et al. (2008) also evaluated muscle EMG activities during a maximal isometric trunk flexion with a bilateral isometric shoulder extension compared with only the trunk flexion, they found that the EMG activities of the rectus abdominis and obliquus externus abdominis muscles increased by 102% to 114% when shoulder extension added to the motion. Thus, they interpreted their findings as an increase in shoulder strength could be enhanced in the lumbar stability as a result of kinetic chain relationships. In another EMG study, Callaghan et al. (1998) stated that when the hands and knees are in the swimming position, the combination of hip extension with cross-arm flexion increases the activation of the upper part of the erector spinae muscle by 30% when compared with only hip extension. The results of these two studies strengthen the starting point of the present study that exercising the upper extremity may improve low back extensor muscle strength and lumbar balance. In speculation, the possible reason of greater increase of back strength in the SE group observed in this study compared with CE group may be explained by the concept of greater activations in the extensor muscles enabled by the activity of upper extremity exercises as stated by Tarnanen et al. (2008) and Callaghan et al. (1998). Considering the spinal muscular kinetic chain in general and, the findings of present and the prior EMG studies, strength/resistance exercises implemented in the upper part of the chain may positively affect the kinetic chain, which is similar to the impact of strengthening exercises applied to the lower part of the kinetic chain. Heo et al. (2015) also demonstrated that lumbar stabilization exercises in combination with thorax mobilization have a greater impact on lumbar part stabilization, pain relief, and patients’ functionality. However, it needs further studies to make accurate conclusion.
Sung et al. (2009) and Sung (2013) analyzed the resistance of the upper part of the chain via EMG studies, applied the isometric fatigue test, and evaluated the degree of fatigue in the thoracic and lumbar erector spinae muscles using surface EMG. They observed that, in patients with chronic low back pain, the average EMG frequency of the thoracic part of the erector spinae muscle is significantly low in comparison with that observed in healthy individuals. They also reported that, because of the insufficiency observed in the thoracic part of the eroctor spinae, the thoracic part of extensor muscles should be taken into account in rehabilitation strategies for patients with low back pain. In accordance with this, several studies (Henchoz and Kai-Lik So, 2000; Sung, 2013) emphasize the need of exercises focused on the extensor muscle group, particularly the thoracic part, in the rehabilitation of patients with chronic low back pain.
It is a very well-known that exercise is an effective method in treating the symptom of pain, which is the most frequent complaint of patients with chronic low back pain (Durmus et al., 2014; Hayden et al., 2005). In several studies (Ahmed et al., 2014; França et al., 2012; Koumantakis at al., 2005), the authors reported a decrease between 1.4 and 5.9 in VAS scores of lumbar pain by applying the conventional exercise programs. The possible reasons for the differences in terms of VAS scores noted the studies should be related to the age and sex distributions of the patients involved in the studies, and the differences in exercise period and intensity used in the studies. In the present study, average decline in the VAS scores were 2.7 and 3.8 in the CE and SE groups, respectively. A greater improvement in VAS score observed in SE group compared with CE group should be related to the upper body exercises used in SE group. Therefore, it can be concluded that the exercises applied to the upper part of the kinetic chain contribute to the relief of pain in patients with chronic low back pain.
It is emphasized that the functional limitation scores of patients, consisting of the severity of pain and treatment success as subjectively determined by patients, are the most important factor in determining chronic low back pain (Maul et al., 2005). Several exercise protocols (Ahmed et al., 2014; França et al., 2012; Moon et al., 2013; Sertpoyraz et al., 2009), which include conventional home exercises, low back school programs, stretching exercises, and dynamic and concentric isokinetic exercises, decrease MODQ scores. However, the impact of exercise models on MODQ scores show differences. Moon et al. (2013) found a decline of 6.1 in the MODQ score for their lumbar stabilization exercise group after 8 weeks of exercise program while they found a decline of 3.6 in the score for their dynamic exercise group. In another study on patients with low back pain, Ahmed et al. (2014) reported a decrease of 22.4 in the MODQ score of the group that performed lumbar mobilization and stabilization exercises and 25.2 in the group that performed only stabilization exercises after 6 weeks. França et al. (2012), who compared stabilization exercises with stretching exercises in 30 patients with chronic low back pain, reported a decrease of 15.2 in the MODQ score of the group that performed stabilization exercises and 9.5 in the group that performed stretching exercises. Discrepancies among the results of the studies should be related to the differences in age and sex distributions, exercise periods and intensities, and initial MODQ scores of the patients involved in the studies. In the present study, the post-exercise MODQ scores decreased by an average of 14.4 in the CE group and by 17.4 in the SE group. In the current literature, we were unable to find a study that investigated the impact of CE exercise programs supported by neck and shoulder exercises on disability in patients with chronic low back pain. However, the results of EMG studies (De Ridder et al., 2013; Sung et al., 2009; Sung, 2013) focused on the muscle weakness of the thoracic part in patients with chronic low back pain bring to mind that in patients undergoing CE exercise programs combined with neck, upper back, and shoulder exercises, the MODQ scores may positively contribute to their recovery from chronic low back pain. The lack of EMG measurements and the absence of long-term monitoring data regarding how long the strength changes continue following the exercise programs, as well as long-term findings on pain and functional state of patients limit our conclusions.
Conclusions
Based on the findings of the present study, it can be argued that the level of pain and disability decrease more significantly in the patients with chronic low back pain who performed back exercises supported with neck, upper back and shoulder exercises compared with the patients who performed only conventional low back exercises. In home exercise programs for patients with chronic low back pain, we believe that it would be more appropriate to include neck, upper back, and shoulder exercises in the program. However, to clarify this issue further in patients with chronic low back pain, long-term studies that would present data on kinetic chain interaction via EMG studies and include findings from neck, back, and shoulder exercises are needed.
Acknowledgements
The authors would like to express their appreciation for the support of the Department of the Scientific Research Projects of Uludag University (Project Number= HDP(T)-2014/4). The experiments comply with the current laws of the country in which they were performed. The authors have no conflict of interest to declare.
Biographies

Erdem ATALAY
Employment
Consultant, Department of Sports Medicine, Eskisehir Yunus Emre State Hospital, Eskisehir, Turkey
Degree
MD
Research interests
Sports injuries and rehabilitation, low back pain, isokinetic and exercise
E-mail: dreatalay@hotmail.com

Bedrettin AKOVA
Employment
Professor, Department of Sports Medicine, Medical Faculty of Uludag Univeristy, Bursa, Turkey
Degree
MD
Research interests
Sport injuries, eccentric exercise, athletic heart
E-mail: bakova@uludag.edu.tr

Hakan GÜR
Employment
Professor, Department of Sports Medicine, Medical Faculty of Uludag Univeristy, Bursa, Turkey
Degree
MD, PhD
Research interests
Sports rehabilitation, ageing, exercise and muscle.
E-mail: hakan@uludag.edu.tr

Ufuk ŞEKİR
Employment
Professor, Department of Sports Medicine, Medical Faculty of Uludag Univeristy, Bursa, Turkey
Degree
MD
Research interests
Sports injuries and rehabilitation, proprioception, surface EMG evaluation, chronic diseases and exercise, musculoskeletal ultrasound
E-mail: ufuksek@uludag.edu.tr
References
- Ahmed R., Shakil-ur-Rehman S., Sibtain F. (2014) Comparison between specific lumber mobilization and core-stability exercises with core-stability exercises alone in mechanical low back pain. Pakistan Journal of Medical Sciences 30(1), 157-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Airaksinen O., Brox C., Cedraschi J., Hildebrandt J., Klaber-Moffett F., Kovacs AF., Mannion S., Reis S., Staal J. B., Ursin H., Zanoli G. (2006) European guidelines for the management of chronic non-specific low back pain. European Spine Journal 15(2), 192-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaranta H., Luoto S., Heliövaara M., Hurri H. (1995) Static back endurance and the risk of low-back pain. Clinical Biomechanics 10(6), 323-324. [DOI] [PubMed] [Google Scholar]
- Artus M., van der Windt D.A., Jordan K.P. (2010) Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology 49(12), 2346-2356. [DOI] [PubMed] [Google Scholar]
- Bronfort G., Maiers M.J., Evans R.L., Schulz C.A., Bracha Y., Svendsen K.H., Grimm R.H., Jr, Owens E.F., Jr, Garvey T.A., Transfeldt E.E. (2011) Supervised exercise, spinal manipulation, and home exercise for chronic low back pain: a randomized clinical trial. The Spine Journal 11(7), 585-598. [DOI] [PubMed] [Google Scholar]
- Burns S.A., Mintken P.E., Austin G.P., Cleland J. (2011) Short-term response of hip mobilizations and exercise in individuals with chronic low back pain: a case series. The Journalo of Manual and Manipulative Therapy 19(2), 100-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagnie B., Cools A., De Loose V., Cambier D., Danneels L. (2007) Differences in isometric neck muscle strength between healthy controls and women with chronic neck pain: the use of a reliable measurement. Archives of Physical Medicine and Rehabilitation 88(11), 1441-1445. [DOI] [PubMed] [Google Scholar]
- Callaghan J.P., Gunning J.L., McGill S.M. (1998) The relationship between lumbar spine load and muscle activity during extensor exercises. Physical Therapy 78(1), 8-18. [DOI] [PubMed] [Google Scholar]
- Calmels P., Jacob J.F., Fayolle-Minon I., Charles C., Bouchet J.P., Rimaud D., Thomas T. (2004) Use of isokinetic techniques vs standard physiotherapy in patients with chronic low back pain. Preliminary results. Annales de Réadaptation et de Médecine Physique 47(1), 20-27. [DOI] [PubMed] [Google Scholar]
- Camargo P.R., Avila M.A., Asso N.A., Salvini T.F. (2010) Muscle performance during isokinetic concentric and eccentric abduction in subjects with subacromial impingement syndrome. European Journal of Applied Physiology 109(3), 389-395. [DOI] [PubMed] [Google Scholar]
- Coorevits P., Danneels L., Cambier D., Ramon H., Vanderstraeten G. (2008) Assessment of the validity of the Biering-Sørensen test for measuring back muscle fatigue based on EMG median frequency characteristics of back and hip muscles. Journal of Electromyography and Kinesiology 18(6), 997-1005. [DOI] [PubMed] [Google Scholar]
- De Ridder E.M., Van Oosterwijck J.O., Vleeming A., Vanderstraeten G.G., Danneels L.A. (2013) Posterior muscle chain activity during various extension exercises: an observational study. Biomed Central Musculoskeletal Disorders 9(14), 204-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixit R.K., Imboden J., Hellmann D., Stone J. (2007) Approach to the patient with low back pain. Current diagnosis and treatment in Rheumatology Ed: Imboden J., 2th edition North America: McGraw-Hill; 100-110. [Google Scholar]
- Durmus D., Unal M., Kuru O. (2014) How effective a modified exercise program on its own or with back school in chronic low back pain? A randomized-controlled clinical trial. Journal of Back and Musculoskeletal Rehabilitation 27(4), 553-561. [DOI] [PubMed] [Google Scholar]
- Ferguson S.A., Marras WS., Burr D.L., Davis K.G., Gupta P. (2004) Differences in motor recruitment and resulting kinematics between low back pain patients and asymptomatic participants during lifting exertions. Clinical Biomechanics 19(10), 992-999. [DOI] [PubMed] [Google Scholar]
- França F.R., Burke T.N., Caffaro R.R., Ramos L.A., Marques A.P. (2012) Effects of muscular stretchıng and segmental stabılızatıon on functıonal dısabılıty and paın in patıents wıth chronıc low back paın: arandomızed, controlled trıal. Journal of Manipulative and Physiological Therapeutics 35(4), 279-285. [DOI] [PubMed] [Google Scholar]
- Hayden J.A., van Tulder M.W., Malmivaara A.V., Koes B.W. (2005) Meta-analysis: exercise therapy for nonspecific low back pain. Annals of Internal Medicine 142(9), 765-775. [DOI] [PubMed] [Google Scholar]
- Henchoz Y., Kai-Lik So A. (2000) Exercise and nonspecific low back pain: a literature review. Joint Bone Spine 75(5), 533-539. [DOI] [PubMed] [Google Scholar]
- Henschken N., Maher C.G., Refshauge K.M., Herbert R.D., Cumming R.G., Bleasel J. (2009) Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis and Rheumatism 60(10), 3072-3080. [DOI] [PubMed] [Google Scholar]
- Heo M.Y., Kim K., Hur B.Y., Nam C.W. (2015) The effect of lumbar stabilization exercises and thoracic mobilization and exercises on chronic low back pain patients. Journal of Physical Therapy Science 27(12), 3843-3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huntoon M.A., Burgher A.H. (2008) Back to the future: the end of the steroid century? Pain Physician 11(6), 713-716. [PubMed] [Google Scholar]
- Ito T., Shirado O., Suzuki H., Takahashi M., Kaneda K., Strax T.E. (1996) Lumbar trunk muscle endurance testing: an inexpensive alternative to a machine for evaluation. Archives of Physical Medicine and Rehabilitation 77(1), 75-79. [DOI] [PubMed] [Google Scholar]
- Ivanova J.I., Birnbaum H.G., Schiller M., Kantor E., Johnstone B.M., Swindle R.W. (2011) Real-world practice patterns, health-care utilization, and costs in patients with low back pain: the long road to guideline-concordant care. The Spine Journal 11(7), 622-632. [DOI] [PubMed] [Google Scholar]
- Koumantakis G.A., Watson P.J., Oldham J.A. (2005) Controlled trial of patients with recurrent low back exercise versus general exercise only: randomized trunk muscle stabilization training plus general. Physical Therapy 85(3), 209-225. [PubMed] [Google Scholar]
- Lemaire A., Ripamonti M., Ritz M., Rahmani A. (2013) Relationships between hip muscles and trunk flexor and extensor muscles in chronic low back pain patients: a preliminary study. Computer Methods in Biomechanics and Biomedical Engineering 16, 161-163. [DOI] [PubMed] [Google Scholar]
- Lizier D.T., Perez M.V., Sakata R.K. (2012) Exercises for treatment of nonspecific low back pain. Revista Brasileira de Anestesiologia 62(6), 838-846. [DOI] [PubMed] [Google Scholar]
- Majid K., Truumees E. (2008) Epidemiology and natural history of low back pain. Seminars in Spine Surgery 20(2), 87-92. [Google Scholar]
- Mannion AF., Muntener M., Taimela S., Dvorak J. (2001) Comparison of three active therapies for chronic low back pain: results of a randomized clinical trial with one-year follow-up. Rheumatology 40(7), 772-778. [DOI] [PubMed] [Google Scholar]
- Maul I., Läubli T., Oliveri M., Krueger H. (2005) Long-term effects of supervised physical training in secondary prevention of low back pain. European Spine Journal 14(6), 599-611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeon M.D., Albert W.J., Neary J.P. (2006) Assessment of neuromuscular and haemodynamic activity in individuals with and without chronic low back pain. Dynamic Medicine 31(5), 116-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miltner O., Wirtz D.C., Siebert C.H. (2001) Strengthening lumbar extensors herapy of chronic back pain an overview and meta-analysis. Zeitschrift für Orthopädie und ihre Grenzgebiete 139(4), 287-293. [DOI] [PubMed] [Google Scholar]
- Moon H.J., Choi K.H., Kim D.H., Kim H.J., Cho Y.K., Lee K.H., Kim J.H., Choi Y.J. (2013) Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Annals of Rehabilitation Medicine 37(1), 110-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naish R., Burnett A., Burrows S., Andrews W., Appleby B. (2013) Can a specific neck strengthening program decrease cervical spine injuries in a men’s professional rugby union team? A retrospective analysis. Journal of Sports Science and Medicine 12(3), 542-550. [PMC free article] [PubMed] [Google Scholar]
- Oaks T. (2012) Choosing the type of probability sampling. Sampling Essentials: Practical Guidelines for Making Sampling Choices. Ed: Daniel J.N. 1th edition United States of America: Sage Publications; 125-174. [Google Scholar]
- Petersen T., Kryger P., Ekdahl C., Olsen S., Jacobsen S. (2002) The effect of McKenzie therapy as compared with that of intensive strengthening training for the 90 treatment of patients with subacute or chronic low back pain: A randomized controlled trial. Spine 27(16), 1702-1709. [DOI] [PubMed] [Google Scholar]
- Pirouzi S., Hides J., Richardson C., Darnell R., Toppenberg R. (2006) Low back pain patients demonstrate increased hip extensor muscle activity during standardized submaximal rotation efforts. Spine 31(26), 999-1005. [DOI] [PubMed] [Google Scholar]
- Plamondon A., Trimble K., Larivière C., Desjardins P. (2004) Back muscle fatigue during intermittent prone back extension exercise. Scandinavian Journal of Medicine and Science in Sports 14(4), 221-230. [DOI] [PubMed] [Google Scholar]
- Rissanen A., Kalimo H., Alaranta H. (1995) Effect of intensive training on the isokinetic strength and structure of lumbar muscles in patients with chronic low back pain. Spine 20(3), 333-340. [DOI] [PubMed] [Google Scholar]
- Robertson R.J., Goss F.L., Rutkowski J., Lenz B., Dixon C., Timmer J., Frazee K., Dube J., Andreacci J. (2003) Concurrent validation of the OMNI perceived exertion scale for resistance exercise. Medicine and Science in Sports and Exercise 35(2), 333-341. [DOI] [PubMed] [Google Scholar]
- Sertpoyraz F., Eyigor S., Karapolat H., Çapacı K., Kirazlı Y. (2009) Comparison of isokinetic exercise versus standard exercise training in patients with chronic low back pain: a randomized controlled study. Clinical Rehabilitation 23(3), 238-247. [DOI] [PubMed] [Google Scholar]
- Sung P.S. (2013) Disability and back muscle fatigability changes following two therapeutic exercise interventions in participants with recurrent low back pain. Medical Science Monitör 14(19), 40-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung P.S., Lammers A.R., Danial P. (2009) Different parts of erector spinae muscle fatigability in subjects with and without low back pain. The Spine Journal 9(2), 115-120. [DOI] [PubMed] [Google Scholar]
- Tarnanen S.P., Ylinen J.J., Siekkinen K.M., Mälkiä E.A., Kautiainen H.J., Häkkinen A.H. (2008) Effect of isometric upper-extremity exercises on the activation of core stabilizing muscles. Archives of Physical Medicine and Rehabilitation 89(3), 513-521. [DOI] [PubMed] [Google Scholar]
- van Middelkoop M., Rubinstein S.M., Kuijpers T., Verhagen A.P., Ostelo R., Koes B.W., van Tulder M.W. (2011) A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European Spine Journal 20(1), 19-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ylinen J.J., Rezasoltani A., Julin M.V., Virtapohja H.A., Mälkiä E.A. (1999) Reproducibility of isometric strength: measurement of neck muscles. Clinical Biomechanics 14(3), 217-219. [DOI] [PubMed] [Google Scholar]


