Abstract
The early post-operative course after hip arthroscopy for femoroacetabular impingement syndrome has not been thoroughly characterized or correlated to factors that may influence recovery. The aim of this study was to report on early pain, function and attitudes towards rehabilitation and to determine predictors of early recovery after hip arthroscopy. Sixty-two patients reported pre-operative pain, iHOT-12 (hip functional score), psychological status and other baseline characteristics. Pain, iHOT-12, hip flexion and several other outcomes were measured through 6 weeks post-operative. Baseline characteristics were correlated with outcomes using univariate and multivariable models. Pain relief started on post-operative day 1 and consistently improved throughout the 6 weeks of follow-up. The average patient’s pain was reduced from a pre-operative level of 5/10 to 2/10 by 6 weeks post-operative. Similarly, iHOT-12 improved from 33/100 to 57/100 whereas hip flexion increased by 9° by 6 weeks post-operative. At 2 weeks post-operative, pre-operative anti-inflammatory usage was associated with greater improvement in pain and swelling; pre-operative opioid usage with poorer patient-reported helpfulness of and adherence to rehabilitation; and higher ASA (American Society of Anesthesiologists) score and lower procedure time with improvement of the pre-operative pain complaint. At 6 weeks, greater depression was associated with lower post-operative pain reduction but greater pre-operative pain complaint improvement. Continuous passive motion usage was associated with increased hip flexion. Pain improved from pre-operative by Day 1 after hip arthroscopy, and early functional improvements were seen by 6 weeks post-operative. Pre-operative anti-inflammatory and opioid usage, depression, race, ASA score, procedure time and continuous passive motion usage were significantly associated with study outcomes.
INTRODUCTION
Femoroacetabular impingement syndrome (FAI) syndrome, affecting the young to middle-aged adult population, is described as an anatomical deformity that causes repeated collisions between the femoral neck and acetabular rim, resulting in symptoms of pain and decreased function along with increased risk of arthritis [1, 2]. Hip arthroscopy is a common minimally invasive treatment for FAI [3]. Surgery to remove the bony obstruction and correct concomitant labral damage has been demonstrated to reduce pain and improve function, even in 5-year or longer follow-up [4].
Younger age and lack of pre-existing arthritis have been associated with improved long-term hip arthroscopy survivorship [5]. Clinicians have also published post-surgical hip arthroscopy rehabilitation protocols intended to guide early post-operative treatment [6–9]. However, many of these protocols lack early outcome data, and, conversely, outcomes studies often lack detailed information relating pre-operative factors, operative and post-operative treatments and early outcomes [10, 11].
Although longer-term pain and functional outcomes are generally encouraging to patients and providers considering hip arthroscopy in treatment of FAI, the immediate post-operative course has not been thoroughly studied or linked to possible predictors of early recovery. However, this part of the treatment process is important to patients and influences overall satisfaction. This information could be useful for providers to accurately inform patients of the expected recovery experience and identify patients that are not progressing as expected. Our hypotheses in this manuscript were that (i) substantial improvement occurs early and is sustained and (ii) discrete patient and treatment factors impact early improvement.
MATERIALS AND METHODS
Study design
This IRB-approved study (IRB# 00066195) is a single-center, two-investigator, prospective, observational study. Results of two highly experienced hip preservations specialists at a tertiary-care academic medical center were combined to analyze early outcomes and factors associated with improved recovery. The study was designed and reported in a manner consistent with the STROBE statement intended to strengthen the reporting of observational studies [12].
Participants
Investigators recruited patients undergoing hip arthroscopy for FAI syndrome from November 2015 to July 2016. Surgical and post-operative protocols were standardized with the exceptions shown in the Supplementary Appendix. All candidates were ages 18 or older without significant hip osteoarthritis who had failed conservative measures such as corticosteroid injection and/or physical therapy.
Treatment
Operations were performed at one of two surgical suites at our university. Surgical treatment was based on intra-operative findings and primarily included labral repair, acetabular rim trimming, and/or femoral osteochondroplasty using a traction table. Patients routinely received an intra-articular or port-site injection of corticosteroid and local anesthetic at the conclusion of the procedure and stayed in the observation unit for less than 24 h. Medications administered in the observation unit were ordered at the discretion of the orthopedic and anesthesia staff on duty while discharge order sets were utilized. Order sets were created to encourage standard discharge medication prescribing. Further operative and post-operative details are provided in the Supplementary Appendix.
Principal investigators differed in the home post-operative rehabilitation strategy that they routinely prescribed patients [continuous passive motion (CPM), bracing and compressive ice versus active ROM and ice packs]. Patients prescribed CPM used standard devices (Kinetec Spectra, Jackson, WI, USA) and were instructed to use the device for 4–6 h per day for the first 3 weeks following surgery. Patients prescribed active ROM exercises were provided with a post-operative sheet of exercises that progressively escalated in intensity (see Supplementary Appendix). Finally, all patients were encouraged to begin formal outpatient physical therapy within 1 week of surgery, and hip flexion was restricted to 90° until 4 weeks post-operative.
Variables
Pre-operative measures included age, gender, opioid and anti-inflammatory usage over the 2 weeks prior to surgery, hip ROM as measured by hip flexion, body mass index (BMI), American Society of Anesthesiologists (ASA) score, race, intra-operative nerve block, procedure time and prior ipsilateral hip surgery. Additionally, the international Hip Outcome Tool [13] (iHOT-12, a validated hip function outcome measure) and pain on the 10-cm visual analog scale (VAS) [14] were measured. Patients were asked to report their average pain over the last 2 weeks in order to reduce the impact of day-to-day pain variations. Because of the recognized role of psychiatric influences in persistent pain after surgery [15], the Pain Catastrophizing Scale [16] (PCS, validated tool that measures exaggerated response to pain) and abbreviated Patient Health Questionnaire-8 [17] (PHQ-8, validated tool that assesses depression severity) were used as an assessment of pre-operative psychologic status. The authors of the PCS note that a total score of 30 represents a clinically relevant level of catastrophizing while PHQ scores of 5, 10, 15 and 20 represent mild, moderate, moderately severe and severe depression.
Patients reported daily pain measurements up to the 2-week visit on a study-provided diary. At the 2-week post-operative visit, pain and hip flexion were re-measured. Patients rated their adherence to the rehabilitation instructions and the helpfulness of rehabilitation on separate VAS scales. To assess patients’ perception of swelling resolution, patients were asked to report whether or not their post-operative swelling had resolved. This subjective, patient-reported outcome was chosen due to potential challenges with obtaining an accurate, objective measurement of post-operative swelling resolution and the importance of assessing patients’ experience of post-operative swelling. In order to assess whether or not patients’ specific pre-operative pain complaint with regard to their hip had been improved by the operation, patients were asked whether or not their pre-operative pain complaint was improved. This outcome was intended to ensure that post-operative pain reductions were not simply related to an expected time-dependent relief of post-operative pain. At the 6-week post-operative visit, VAS pain, iHOT-12, hip flexion, pre-operative pain complaint improvement and swelling resolution were re-assessed. Patients who could not return for one of their visits were instructed to complete the assessment form on their own at the appropriate time and to return the form to the investigators. Hip flexion in these cases was obtained from the patient’s local physical therapist with permission from the patient. Supplementary Table S1 describes further form completion characteristics.
Measurements
In determining the clinical importance of orthopedic treatments to reduce pain, Katz et al. [18] have advocated for defining minimal clinically important differences (MCIDs). Intervention success or failure is then based on differences in proportions between groups of these pre-defined MCID thresholds. This binary analytic strategy simultaneously reduces the effect of outliers and focuses analysis towards pre-determined clinically relevant outcomes.
In the absence of published work citing the MCID for pain relief in patients undergoing hip arthroscopy, the authors incorporated MCID pain reduction thresholds derived from values in mild to moderate hip osteoarthritis [18, 19]: change in VAS pain score of 10% from pre-operative to 2- and 6 weeks post-operative. This normalized scoring system was used to minimize potential floor effects and scale treatment expectations to the degree of pre-operative pain. This threshold identified patients who had at least mild pain reduction as might be expected in the early post-operative period and excluded patients whose pain worsened. Raw changes in pain over time are also shown. Although the MCID for iHOT-33 has been estimated as a 6.1-point change, there was no reported MCID for iHOT-12 [20]. Therefore, the MCID for the iHOT-33 was scaled to the iHOT-12 (value = 2.2 out of 12). Raw changes in function over time are also shown.
Study size
After surgeons standardized their operative and post-operative protocols, rehabilitation strategy was the only remaining major peri-operative treatment difference. The study was powered to detect differential outcomes by this potential confounder. Patient records from the CPM group (n = 10) and the active ROM group (n = 11) were reviewed to determine pre-operative and 2-week pain scores. 90% of patients in the CPM group met the MCID pain reduction threshold compared with 55% of patients in the active ROM group. Based on these results, ≥30 patients in each arm would be needed to detect a statistically significant difference in the primary study outcome, MCID normalized pain reduction, at an alpha of 0.05 and a beta of 0.8 using a standard sample size calculator for comparing two independent proportions (www.stat.ubc.ca/∼rollin/stats/ssize/b2).
Statistical analysis
Summary measures of outcomes such as proportions, means, Kaplan–Meier curves, standard deviation and standard error were calculated. Univariate analysis using t-tests, chi-square analysis and Pearson correlation was performed using JMP Pro version 13.0.0 (Statistical Analysis Software, Cary, NC, USA) to assess the impact of each covariate on each of the outcomes. Multivariable models were constructed for outcomes where more than one covariate demonstrated significant univariate association (P < 0.05). The threshold for multivariable significance was set at P < 0.05. No adjustment was made for multiple comparisons in order to increase sensitivity to possible risks and benefits of each factor.
Missing data
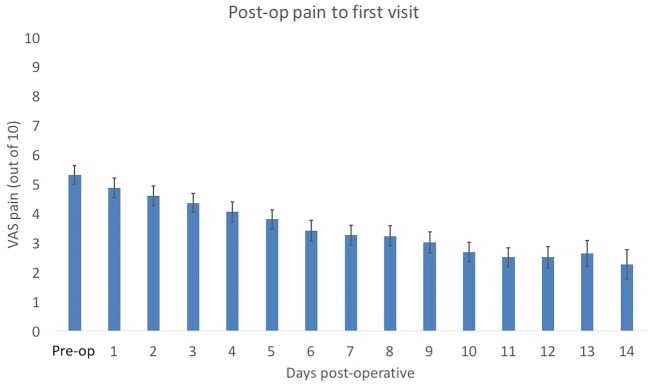
Because of the importance of assessing the impact of pre-operative factors and primary post-operative outcomes on a single cohort, 15 patients were excluded due to incomplete pre-operative data or missing primary post-operative study outcomes. A study enrollment diagram is shown in Fig. 1. A complete case analysis was carried out for all outcomes. At the most, three patients with complete pre-operative data were missing secondary outcome data and were excluded in the analysis for that outcome. Supplementary Table S2 shows a complete listing of this information.
Fig. 1.
Study enrollment flow diagram.
RESULTS
Out of 130 patients eligible for the study, 62 patients were included in the final analysis (Fig. 1). Fifty-three patients either declined participation or were unable to be included because of logistical constraints (standard CPM device unavailable or unable to consent prior to surgery). None of the 77 patients entering the study were lost to follow-up. Fifteen patients who did not complete their pre-operative form or the primary 2- or 6-week outcomes were excluded from the analysis.
The average patient enrolled in this study was a slightly overweight, mid-30’s female complaining of 5 out of 10 pain with a hip functional score less than 33/100, and depression rating consistent with mild depression (Table I). In the 2 weeks prior to surgery, 1/4 of patients reported opioid usage and 1/2 of patients reported anti-inflammatory usage. Average procedure time was approximately 2 h and 1/3 of patients received a nerve block prior to surgery. Several patients had had prior ipsilateral hip surgery or required additional operative interventions.
Table I.
Baseline patient and operative characteristics of the study population
| Baseline characteristic | Average (SD) or proportion (%) |
|---|---|
| Age | 37.4 (11.4) |
| Female gender | 48/62 (77%) |
| Caucasian race | 54/62 (87%) |
| BMI | 27.4 (5.8) |
| ASA | 1.8 (0.5) |
| Pre-operative opioid | 15/62 (24%) |
| Pre-operative anti-inflammatory | 31/62 (50%) |
| PHQ score (out of 24) | 5.4 (5.1) |
| PCS score (out of 52) | 15.8 (14.6) |
| Pre-operative pain (out of 10) | 5.2 (2.3) |
| iHOT-12 (out of 100) | 32.5 (18.8) |
| Procedure time (hours) | 2.1 (0.5) |
| Nerve block | 21/62 (33%) |
| Prior ipsilateral hip surgery | 4/62 (6%) |
| Additional intervention other than acetabular rim trimming, labral repair or femoral osteochondroplasty | 5/62 (8%) |
All patients underwent acetabular rim trimming and labral repair and almost all underwent femoral osteochondroplasty (Table II). Two patients underwent adjunctive procedures not directly related to FAI syndrome treatment (trochanteric bursectomy or hamstring repair). One surgeon’s patients used CPM, compressive icing devices and a night-time brace as part of rehabilitation compared with active ROM exercises and ice packs prescribed by the other surgeon.
Table II.
Surgical and post-operative interventions
| Baseline characteristic | Study patients |
|---|---|
| Acetabular rim trimming | 62/62 (100%) |
| Labral repair | 62/62 (100%) |
| Femoral osteochondroplasty | 58/62 (94%) |
| Acetabular microfracture | 3/62 (5%) |
| Hamstring repair | 1/62 (2%) |
| Trochanteric bursectomy | 1/62 (2%) |
| CPM (compared with active range of motion exercises)a | 31/62 (50%) |
| Compressive ice (compared with icing)a | 31/62 (50%) |
| Night-time bracea | 31/62 (50%) |
Surgeon-dependent factors.
By 2 weeks post-operative, many patients had shown considerable improvement (Table III). More than 80% of patients met the MCID for pain reduction, had swelling resolution and reported improvement of the specific pre-operative pain complaint that had influenced their decision to undergo surgery. However, hip flexion did not substantially improve by 2 weeks post-operative. The helpfulness of the home rehabilitation was rated at 76% while patients reported adhering to the rehabilitation guidelines 82% of the time.
Table III.
Outcomes at 2 weeks post-operative
| Study outcome | Average (SD) or proportion (%) |
|---|---|
| Pain MCID met | 50/62 (80.6%) |
| Pain change (out of 10) | −2.4 (2.5), n = 62 |
| Hip flexion change (°) | −0.8 (12.1), n = 59 |
| Swelling resolved | 52/61 (85.2%) |
| Pre-operative pain complaint improved | 53/61 (86.8%) |
| Rehab helpfulness (out of 100) | 76.2 (27.5), n = 59 |
| Rehab adherence (out of 100) | 82.3 (25.2), n = 60 |
N is displayed for each outcome.
By 6 weeks post-operative, more patients met the MCID pain threshold, reported swelling resolution and indicated that their specific pre-operative pain complaint had improved (Table IV). Further, even at this relatively early time point, slightly more than 50% of patients achieved the MCID for hip function with an average gain of 25 points out of 100. While hip flexion had been stagnant at 2 weeks post-operative, hip flexion increased approximately 9° by 6 weeks post-operative compared with pre-operative values.
Table IV.
Outcomes at 6 weeks post-operative
| Study outcome | Average (SD) or proportion (%) |
|---|---|
| Pain MCID met | 52/62 (83.8%) |
| Pain change (out of 10) | −3.1 (2.6), n = 62 |
| Hip function MCID met | 33/62 (53.2%) |
| Hip function change (out of 100) | 24.1 (21.9), n = 62 |
| Hip flexion change (°) | 9.1 (14.7), n = 60 |
| Swelling resolved | 55/62 (88.7%) |
| Pre-operative pain complaint improved | 53/61 (86.8%) |
Several patients did not complete specific study outcomes. N is displayed for each outcome.
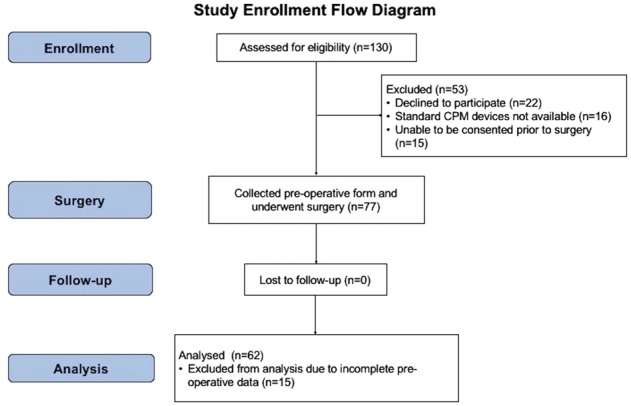
More than 50% of patients achieved at least a 10% reduction of their pre-operative pain by post-operative day 2 (Fig. 2). Further, 98% of patients had met this threshold at least once in the 2 weeks after surgery.
Fig. 2.
Kaplan–Meier curve displaying the time to patients achieving their first day with a pain level below their MCID threshold in the first 14 days post-operative. Greater than 50% of patients achieved this threshold between post-operative day 1 and 2.
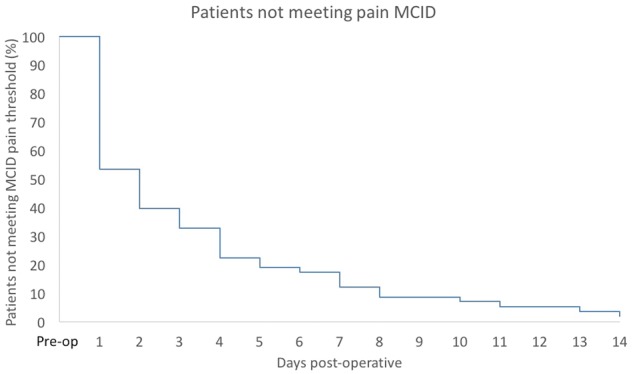
Pain decreased from pre-operative levels starting on post-operative day 1 and continued to consistently improve over the first 2 weeks after surgery as recorded by patient pain diaries (Fig. 3). In-office pain measurement showed the same trend from pre-operative to 2 weeks and then 6 weeks post-operative (Fig. 4). Similarly, hip function improved substantially (approximately 25 points out of 100) between pre-operative and 6 weeks post-operative (Fig. 5). Hip flexion remained stable from pre-operative to 2 weeks post-operative, likely related at least in part to the restriction of hip flexion to 90° in the first 4 weeks after surgery. However, it increased by approximately 9° by 6 weeks post-operative (Fig. 6).
Fig. 3.
Daily pain from pre-operative to the first post-operative visit, which was usually scheduled at approximately 10 days to 2 weeks post-operative of the 58 patients who completed the pain diary.
Fig. 4.
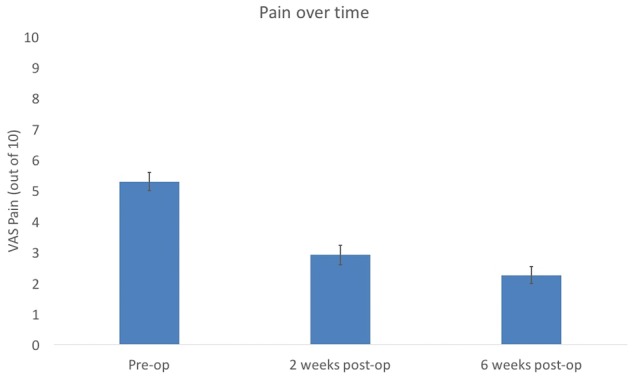
Average pre-operative to 6-week post-operative VAS pain rating for all patients in the analysis (n = 62). Standard error is also shown.
Fig. 5.
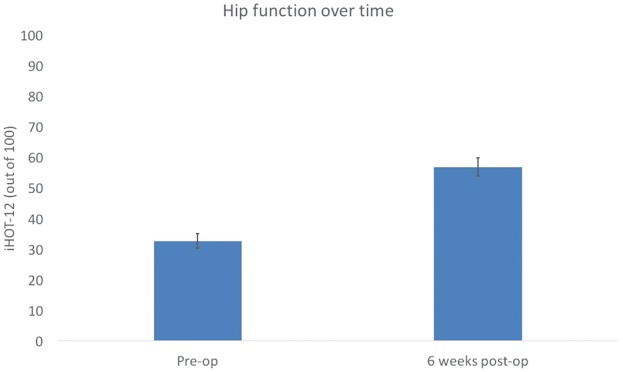
Average pre-operative to 6-week post-operative iHOT-12 scores along with error bars.
Fig. 6.
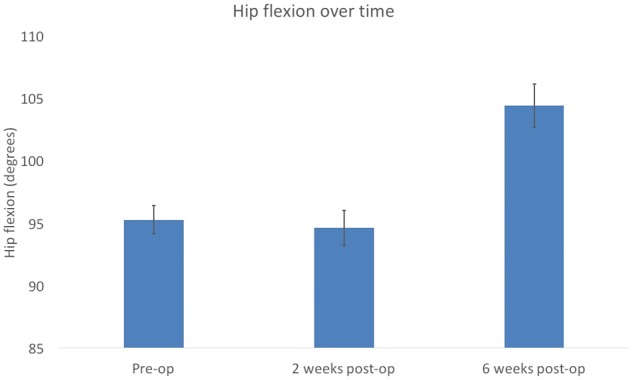
Average pre-operative, 2-week post-operative and 6-week post-operative hip flexion along with standard error.
As shown in Supplementary Table S4, the following associations were determined in multivariable analysis: higher pre-operative pain with greater pain reduction; higher ASA score and lower procedure time with greater likelihood of pre-operative p pain complaint improvement; and lack of pre-operative opioid usage with greater rehabilitation adherence. Factors that were associated with outcomes in univariate analysis but that did not remain associated with outcomes in multivariable models included the following: pre-operative anti-inflammatory usage with greater pain reduction and Caucasian race with greater rehabilitation adherence. In models where only one factor was associated with the outcome, the following correlations were observed: pre-operative anti-inflammatory usage with greater likelihood of meeting the MCID pain reduction threshold and swelling resolution and lack of pre-operative opioid usage with greater perceived rehabilitation helpfulness.
Supplementary Table S5 demonstrates associations between patient, operative and rehabilitative factors and outcomes at 6 weeks. In multivariable analysis, the following associations were determined: higher pre-operative pain with greater pain reduction. Factors that achieved significance in univariate but not multivariable analysis included the following: lower pre-operative hip function with higher pain reduction; higher pre-operative pain and lower pre-operative hip function with greater hip function increase; and lower depression rating, higher pre-operative hip function and lower pain catastrophizing with greater swelling resolution. In models where only one factor achieved significance, the following associations were determined: lower depression rating with higher likelihood of meeting the MCID pain reduction, CPM usage with greater hip flexion, higher depression rating with higher likelihood of pre-operative pain complaint improvement. In a separate, complete-case analysis (60 of 62 patients completed this 2-week outcome), lower patient-reported adherence was associated with lower likelihood of meeting the 6-week pain MCID threshold in univariate analysis. However, 2-week pain and 6-week iHOT-12 MCID’s were not significantly associated. Supplementary Table S6 shows detailed CPM usage data for the patients whose devices were equipped with usage monitors (n = 15) and demonstrates that patients followed usage guidelines (4–6 h/day) strictly only 25% of the days that they had the device.
Finally, in order to assess whether or not outcomes could have been substantially impacted by including the two patients that underwent adjunctive procedures at the time of their surgical treatment for FAI syndrome (hamstring repair or trochanteric bursectomy), study results were tabulated for the 60 patients that only had a combination of the following procedures performed: labral repair, acetabular rim trimming, femoral osteochondroplasty and acetabular microfracture. Results did not differ substantially between the slightly reduced cohort and the entire study cohort. However, it was noted that the two patients with hamstring repair or trochanteric bursectomy had lower pain relief, functional improvement, hip flexion improvement, early swelling resolution, early pre-operative pain complaint improvement, perception of rehabilitation helpfulness and rehabilitation adherence.
DISCUSSION
This study presents a high-volume hip preservation center’s typical early post-operative recovery after hip arthroscopy for femoroacetabular impingement syndrome. The first hypothesis of the study was that substantial improvement occurs early and is sustained. To that end, >50% of patients reported meeting the pre-defined pain MCID by 2 days post-operative with 98% of patients achieving that threshold by 2 weeks post-operative. Pain decreased consistently over the first 2 weeks and continued to improve through the 6-week visit. About 81% of patients experienced clinically significant pain improvements by 2 weeks and 84% by 6 weeks. Even at a relatively early time point of 6 weeks post-operative, hip function and flexion were increased, and most patients had reported swelling resolution and improvement of their pre-operative pain complaint. Patients reported 82% compliance with the rehabilitation protocol. Overall, clinically relevant improvements occurred rapidly after surgery in a broad range of outcomes and were sustained over the course of the study. This information could be very helpful to clinicians in setting appropriate patient expectations in the early recovery period.
The study’s second hypothesis was that discrete patient and treatment factors impact early improvement. As discussed below, a variety of patient and treatment factors modulated early improvement, including pre-operative medication usage. Meeting the MCID pain threshold was associated with pre-operative anti-inflammatory usage. Half of the patients in this series reported pre-operative anti-inflammatory usage. Post-operative anti-inflammatory usage after hip arthroscopy has been associated with lower heterotopic ossification [21, 22], which may reduce pain. Additionally, COX-2 inhibitors have been noted as effective pre-emptive analgesics in knee arthroscopy [23]. Pre-emptive anti-inflammatory analgesia could be differentiated from post-operative analgesic effect through determining post-operative anti-inflammatory adherence. The 1/4 of patients using pre-operative opioids reported lower adherence and satisfaction with their prescribed home rehabilitation regimen. Prior studies have demonstrated poor outcomes amongst patients with chronic opioid use [24].
Due to the increasingly recognized associations of psychological factors on outcomes [25], this study examined the role of depression and pain catastrophization on early recovery. Lower depression and pain catastrophization showed univariate association with several outcomes including greater pain reduction and swelling resolution by the 6-week post-operative visit. Although psychological distress has been associated with reduced pre-operative hip function [26], this is the first study to the authors’ knowledge to demonstrate post-operative associations with psychological factors on outcomes in treatment of FAI. Somewhat paradoxically, patients reporting that their pre-operative pain complaint had not improved at 6 weeks post-operative also reported lower depression scores. However, post-operative pain due to surgery and patients’ pre-operative pain complaint likely represent distinct entities experienced by patients that contribute individually to early recovery. Further, although the absolute difference in depression rating between the patients reporting pre-operative pain complaint improvement and patients not reporting pre-operative pain complaint improvement met statistical significance, the absolute difference in scores (4.2 points out of 24) and the number of patients reporting no improvement (8 out of 61) were relatively small.
Compared with patients using active ROM and icing as part of their home rehabilitation strategy, patients using CPM, brace and compressive cooling devices had greater increases in hip flexion by 6 weeks (14° versus 4.5°). This finding is in line with previous reports of the efficacy of CPM devices in both ACL reconstruction and total knee arthroplasty which demonstrate isolated improvements in ROM [27, 28]. However, a higher proportion of patients undergoing the active ROM and icing strategy reported pre-operative anti-inflammatory usage which was associated with improved early pain and swelling. Randomized, controlled data is necessary to determining clinical efficacy of specific treatments. The associations of pre-operative pain and function with changes in post-operative pain and function likely represent floor or ceiling effects and highlight the importance of evaluating MCID’s. Finally, although intra-operative corticosteroid injection could theoretically increase the potential risk of post-operative surgical site infection, the authors noted no surgical site infections within the study cohort and their patients have only rarely suffered this complication. Prospective, randomized trials of local injection of long-acting anesthetic agents in total knee replacements demonstrate improved pain control with the addition of low-dose dexamethasone [29]. The authors believe that corticosteroid injection assists in reducing post-operative pain. However, infection risk may depend on individual patient and surgeon characteristics. The decision to use a corticosteroid injection at the time of surgery should balance the desire for analgesia with a potential risk of infection.
While this prospective, observational study is strengthened by its collection of a broad array of relevant, detailed patient, operative and post-operative characteristics along with early post-operative outcomes, it is limited in its follow-up time. In particular, functional recovery is not complete at 6 weeks and care must be taken in drawing conclusions about functional recovery. Collection of longer-term outcomes is important to verify current study findings. Further, sample size was based on the potential impact of one of the factors (differential rehabilitation strategies) which was thought to potentially relate to outcomes after hip arthroscopy. Association of other binary factors with outcomes could be further evaluated with greater sample size.
In conclusion, this prospective, observational study of early recovery after hip arthroscopy for FAI syndrome provides evidence to guide patient and provider expectations. Clinically significant improvements in pain, function, and hip flexion were seen by the 6-week visit. Several factors were associated with improved study outcomes including pre-operative anti-inflammatory usage, lack of pre-operative opioid usage, CPM and decreased depression. Optimization of potentially modifiable factors could be evaluated prospectively to determine if pre-operative changes result in improved post-operative results.
SUPPLEMENTARY DATA
Supplementary data are available at Journal of Hip Preservation Surgery online.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to recognize Janice Baucom and Alan Moses for their contributions in the clinical management of patients in this study.
FUNDING
National Institutes of Health Clinical and Translational Sciences Awards (TL1TR001116). The funding source played no role in the investigation.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Beck M, Kalhor M, Leunig M, Ganz R.. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 2. Griffin DR, Dickenson EJ, O'Donnell J. et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016; 50: 1169–76. [DOI] [PubMed] [Google Scholar]
- 3. Ganz R, Parvizi J, Beck M. et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417:112–20. [DOI] [PubMed] [Google Scholar]
- 4. McCormick F, Nwachukwu BU, Alpaugh K, Martin SD.. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy 2012; 28: 1359–64. [DOI] [PubMed] [Google Scholar]
- 5. McCarthy JC, Jarrett BT, Ojeifo O. et al. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res 2011; 469: 362–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Edelstein J, Ranawat A, Enseki KR. et al. Post-operative guidelines following hip arthroscopy. Curr Rev Musculoskelet Med 2012; 5: 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Enseki KR, Martin R, Kelly BT.. Rehabilitation after arthroscopic decompression for femoroacetabular impingement. Clin Sports Med 2010; 29: 247–55. [DOI] [PubMed] [Google Scholar]
- 8. Voight ML, Robinson K, Gill L, Griffin K.. Postoperative rehabilitation guidelines for hip arthroscopy in an active population. Sports Health 2010; 2: 222–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wahoff M, Dischiavi S, Hodge J, Pharez JD.. Rehabilitation after labral repair and femoroacetabular decompression: criteria-based progression through the return to sport phase. Int J Sports Phys Ther 2014; 9: 813–26. [PMC free article] [PubMed] [Google Scholar]
- 10. Grzybowski JS, Malloy P, Stegemann C. et al. Rehabilitation following hip arthroscopy—a systematic review. Front Surg 2015; 2: 21.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cheatham SW, Enseki KR, Kolber MJ.. Postoperative rehabilitation after hip arthroscopy: a search for the evidence. J Sport Rehabil 2015; 24: 413–8. [DOI] [PubMed] [Google Scholar]
- 12. von Elm E, Altman DG, Egger M. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014; 12: 1495–9. [DOI] [PubMed] [Google Scholar]
- 13. Griffin DR, Parsons N, Mohtadi NG. et al. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy 2012; 28: 611–6. quiz 6–8. [DOI] [PubMed] [Google Scholar]
- 14. Hawker GA, Mian S, Kendzerska T, French M.. Measures of adult pain: visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken) 2011; 63(Suppl. 11): S240–52. [DOI] [PubMed] [Google Scholar]
- 15. Lewis GN, Rice DA, McNair PJ, Kluger M.. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015; 114: 551–61. [DOI] [PubMed] [Google Scholar]
- 16. Osman A, Barrios FX, Gutierrez PM. et al. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med 2000; 23: 351–65. [DOI] [PubMed] [Google Scholar]
- 17. Kroenke K, Spitzer RL, Williams JB.. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Katz NP, Paillard FC, Ekman E.. Determining the clinical importance of treatment benefits for interventions for painful orthopedic conditions. J Orthop Surg Res 2015; 10: 24.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stauffer ME, Taylor SD, Watson DJ. et al. Definition of nonresponse to analgesic treatment of arthritic pain: an analytical literature review of the smallest detectable difference, the minimal detectable change, and the minimal clinically important difference on the pain visual analog scale. Int J Inflam 2011; 2011: 231926.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mohtadi NG, Griffin DR, Pedersen ME. et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy 2012; 28: 595–605; quiz 606–10.e1. [DOI] [PubMed] [Google Scholar]
- 21. Beckmann JT, Wylie JD, Potter MQ. et al. Effect of naproxen prophylaxis on heterotopic ossification following hip arthroscopy: a double-blind randomized placebo-controlled trial. J Bone Joint Surg Am 2015; 97: 2032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dahners LE, Mullis BH.. Effects of nonsteroidal anti-inflammatory drugs on bone formation and soft-tissue healing. J Am Acad Orthop Surg 2004; 12: 139–43. [DOI] [PubMed] [Google Scholar]
- 23. Mardani-Kivi M, Karimi Mobarakeh M, Haghighi M. et al. Celecoxib as a pre-emptive analgesia after arthroscopic knee surgery; a triple-blinded randomized controlled trial. Arch Orthop Trauma Surg 2013; 133: 1561–6. [DOI] [PubMed] [Google Scholar]
- 24. Devin CJ, Lee DS, Armaghani SJ. et al. Approach to pain management in chronic opioid users undergoing orthopaedic surgery. J Am Acad Orthop Surg 2014; 22: 614–22. [DOI] [PubMed] [Google Scholar]
- 25. Ayers DC, Franklin PD, Ring DC.. The role of emotional health in functional outcomes after orthopaedic surgery: extending the biopsychosocial model to orthopaedics: AOA critical issues. J Bone Joint Surg Am 2013; 95: e165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Potter MQ, Wylie JD, Sun GS. et al. Psychologic distress reduces preoperative self-assessment scores in femoroacetabular impingement patients. Clin Orthop Relat Res 2014; 472: 1886–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rosen MA, Jackson DW, Atwell EA.. The efficacy of continuous passive motion in the rehabilitation of anterior cruciate ligament reconstructions. Am J Sports Med 1992; 20: 122–7. [DOI] [PubMed] [Google Scholar]
- 28. Harvey LA, Brosseau L, Herbert RD.. Continuous passive motion following total knee arthroplasty in people with arthritis. Cochrane Database Syst Rev 2014; 2: CD004260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ikeuchi M, Kamimoto Y, Izumi M. et al. Effects of dexamethasone on local infiltration analgesia in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 2014; 22: 1638–43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.