Abstract
Despite an unmet need for hepatologists in the United States, every year transplant hepatology (TH) fellowship positions remain unfilled. To address this, we investigated factors that influence trainee decisions about pursuing a career in hepatology. We invited current gastroenterology (GI) and TH fellows from all Accreditation Council for Graduate Medical Education‐accredited programs for the academic year 2014‐2015 to participate in an online survey about factors influencing decisions to train in hepatology. The same paper‐based survey was distributed at a nationally recognized GI board review course. The survey was completed by 180 participants of which 91% were current GI or TH fellows and 24% were not aware of the pilot 3‐year combined GI and TH training program. A majority of respondents (57%) reported that a shorter time (3 versus 4 years) to become board certification eligible would influence their decisions to pursue TH. The most common reasons for not pursuing hepatology were less endoscopy time (67%), additional length of training (64%), and lack of financial compensation (44%). Personal satisfaction (66%), management of complex multisystem disease (60%), and long‐term relationships with patients (57%) were the most attractive factors. Sixty‐one percent of participants reported having a mentor, and 94% of those with mentors reported that their mentors influenced their career decisions. Conclusion: We have identified several factors that affect fellows' decision to pursue TH. Shorter training, increased financial compensation, and increased endoscopy time are potentially modifiable factors that may increase the number of trainees seeking careers in hepatology and help alleviate the deficit of hepatologists. (Hepatology Communications 2017;1:347–353)
Abbreviations
- AASLD
American Association for the Study of Liver Diseases
- ABIM
American Board of Internal Medicine
- ACGME
Accreditation Council for Graduate Medical Education
- AY
academic year
- GI
gastroenterology
- TH
transplant hepatology
Introduction
The burden of chronic liver disease in the United States has increased significantly over the past 20 years.1 Chronic liver disease with cirrhosis is the twelfth leading cause of death overall and the fifth leading cause of death for patients aged 45‐54 years. The prevalence of cirrhosis in the United States is approximately 0.27% of the population, accounting for 633,323 persons, with many cases remaining undiagnosed.2 Updated hepatitis C screening recommendations, an increasing immigrant population with chronic hepatitis B, and the worsening epidemic of obesity‐related liver disease promise to increase the need for specialized care of these patients.3, 4, 5 The continued success of liver transplantation for an increasing number of chronic liver diseases also requires physicians trained in the care of patients who require or who have had liver transplant.
There is a need to train more hepatologists.6, 7 In 2009, the American Association for the Study of Liver Diseases (AASLD) had approximately 3,500 dues‐paying members with 50% based in the United States; only half of those indicated that they or the majority of their practice focused on patients with liver disease.8 Of the surveyed liver transplant programs, 81% reported they were recruiting or would be recruiting additional hepatologists within the next 3 years, with many recruiting for two or more positions.9 A recent estimation in the United States indicated there are “a thousand or so hepatologists to serve our communities” or an average of one hepatologist per 330,000 individuals.10 The need to train additional hepatologists to meet rising demand is apparent.
Hepatology is in its infancy as a subspecialty of gastroenterology (GI) and internal medicine. The dedicated clinical practice of hepatology had its beginnings in the late 1990s, and this culminated in publication of curricular guidelines for training in transplant hepatology (TH) in 2002.11 In 2006, the American Board of Internal Medicine (ABIM) offered the first TH certifying examination. Presently, only ABIM‐certified gastroenterologists are eligible to train and certify in TH. Certification in TH commonly involves completion of a 3‐year internal medicine residency, a 3‐year GI fellowship, and a 1‐year TH fellowship. Many of the positions in the Accreditation Council for Graduate Medical Education (ACGME)‐accredited TH fellowship programs go unfilled each year.12 In recognition of the lengthy training process and to meet the growing demand for hepatologists, the ABIM and the AASLD Transplant Hepatology Pilot Steering Committee collaborated to create a 3‐year combined GI/TH Training Pilot Program in 2012.13 In academic year (AY) 2014‐2015, there were 10 such pilot programs in the United States; however, since its 2012 inception, the impact of implementing the 3‐year combined GI/TH Training Pilot Program in addressing this deficit is still unclear. An updated workforce study is needed to estimate the optimal workforce and to properly design training pathways.14
Many physicians start their careers with substantial financial debt. Because TH is not primarily a procedural specialty, many assume hepatologists generate less revenue than their GI colleagues. While it has been demonstrated that the level of medical student debt correlates with decisions against careers with lower earning potential, such as primary care specialties,15 the impact of debt on the career path of GI fellows is unexplored. Furthermore, the influence of mentorship in medical education has been shown across multiple medical specialties and levels of training16; however, no literature exists examining the role of mentor in the selection of GI subspecialty training. Our study aims to examine the potential influencing factors for or against a career in hepatology, including the impact of mentorship and educational debt, with reported career plans among GI fellows.
Participants and Methods
SURVEY INSTRUMENTS
The survey is a 35‐item questionnaire (Supporting Appendix S1) designed to examine (1) respondent demographics, (2) training‐program characteristics, (3) factors influencing trainee decisions about pursuing hepatology as a career, and (4) involvement of mentors in making career decisions. This instrument was designed and assessed by pilot testing performed by gastroenterologists from our respective institutions and members of the AASLD Transplant Hepatology Pilot Program Committee.
PARTICIPANTS
All GI/TH fellows in ACGME‐accredited fellowships in the United States for AY 2014‐2015 were invited to participate in the study. Non‐GI physicians, pediatric gastroenterologists, and those from training institutions outside the United States were excluded.
SURVEY DISTRIBUTION
GI program directors and trainees were e‐mailed an introduction letter describing the study and an HTML link to the survey website. GI and TH program directors were also asked to assist in recruitment for survey participation. Reminder e‐mails were sent at 2 and 4 weeks after the initial e‐mail to encourage completion. The same survey was distributed at a nationally recognized GI board review course in paper form to increase study participation. The survey was designed and administered through SurveyMonkey, a secure web‐based application. All data were anonymous such that respondents could not be traced back to specific programs. We encouraged participation through an optional drawing for an iPad. Those respondents who opted in provided contact information.
DATA MANAGEMENT AND STATISTICAL ANALYSIS
Responses were de‐identified and recorded in a computer database for analysis. Descriptive statistics were computed for all factors with values expressed as means, standard deviations, and percentages. Data were collated and analyzed using statistical software package R v3.2.3 (Auckland, New Zealand). Fisher's exact test and the chi‐squared test were used for statistical analysis between group comparisons of categorical data. We defined statistical significance as a P value of less than 0.05. Georgetown University Institutional Review Board approved this study.
Results
DEMOGRAPHICS
A total of 180 participants from ACGME‐accredited GI Fellowship Programs across the United States completed the survey. Twenty‐five respondents (13.8%) were either in or planning on entering a TH fellowship. Most respondents were male (64%) and in a committed relationship (77%). Ninety‐one percent of the participants were current GI or TH fellows, and 9% had completed a fellowship (Table 1). The majority of respondents (81%) reported training in a university‐affiliated fellowship program. Fifty‐eight percent practiced in a liver transplant center, with 32% of respondents working in a hospital with an ACGME‐accredited TH fellowship. Twenty‐four percent of respondents were not aware of the 3‐year combined GI and TH pilot training program, and only 19% reported that their fellowship participated in a 3‐year combined GI/TH pilot training program. No financial debt was reported by 44% of respondents, while 5% reported they had over $350,000 dollars of debt (Table 2).
Table 1.
CHARACTERISTICS OF RESPONDERS
| % of Responses | |
|---|---|
| Responder's Characteristics | (n = 180) |
| Gender | |
| Men | 64 |
| Women | 36 |
| Relationship status | |
| Single | 77 |
| In a relationship | 17 |
| Children (under age 18 years) | |
| Yes | 43 |
| No | 56 |
| Level of training | |
| 1st year | 27 |
| 2nd year | 27 |
| 3rd year | 30 |
| 4th year | 7 |
| Completed | 9 |
| U.S. fellowship location | |
| New England | 8 |
| Mid‐Atlantic | 19 |
| East North Central | 16 |
| West North Central | 5 |
| Mountain | 5 |
| Pacific | 13 |
| South Atlantic | 20 |
| East South Central | 1 |
| West South Central | 11 |
| Type of fellowship program | |
| University | 81 |
| Community | 17 |
| Size of fellowship (number of GI fellows) | |
| 1‐3 | 9 |
| 4‐7 | 24 |
| 8‐11 | 26 |
| >12 | 36 |
Table 2.
LEVEL OF DEBT
| Debt (U.S. Dollars) | Response, %(n = 180) |
|---|---|
| 0‐49,999 | 44.4 |
| 50,000‐99,999 | 5.6 |
| 100,000‐149,999 | 8.9 |
| 150,000‐199,999 | 7.2 |
| 200,000‐249,999 | 10.6 |
| 250,000‐299,000 | 11.1 |
| 300,000‐349,999 | 3.9 |
| 350,000‐399,999 | 3.3 |
| >400,000 | 1.7 |
| No response | 3.3 |
INTEREST IN A TH FELLOWSHIP
The majority of respondents (86%) were either undecided or not planning on training in hepatology. Of these, 21% reported having no interest in a TH fellowship. Fifty‐seven percent reported that board certification eligibility in 3 years rather than 4 years would encourage them to pursue a TH fellowship, and 52% reported that financial compensation equivalent to their GI colleagues would influence them to pursue TH. Of those who responded that neither of these factors would influence their decision, the majority (66%) reported no interest in hepatology or were pursuing another subspecialty.
ATTRACTORS AND DETERRENTS
Those planning on entering a hepatology fellowship were more likely to be attracted to the management of complex systems (92.0% versus 54.8%, P < 0.001), financial compensation (56.0% versus 33.5%, P = 0.044), and prestige (36.0% versus 18.7%, P = 0.065) when compared to those who were undecided or not planning on hepatology.
Two unique deterring factors for undecided respondents were concerns over financial debt and possible geographic relocation. Respondents with high educational debt (>$200,000) were more likely to list financial debt as a deterrent (56.4% versus 23.3%, P <0.001).
Respondents who were married or in a committed relationship were more likely to be deterred by an additional year of training (80.6% versus 61.2%, P = 0.04) or geographic relocation (54.8% versus 27.3%, P = 0.002). Respondents with children were more likely to list the additional year of training (72.7% versus 58.0%, P = 0.042) or influence of family (37.7% versus 25.0%, P = 0.070) as deterrents. Female respondents were more likely than males to list the influence of family (43.5% versus 23.5%, P = 0.009) as a deterrent. Those unsure or not planning on hepatology were more likely to list the patient population (e.g., patients with chronic liver disease from alcohol or illicit drug use who may make ongoing self‐destructive choices) as a deterring factor than those planning on hepatology (34% versus 4%, P = 0.005). Those at a community‐based medical center were more likely to list the additional year of training as a deterrent than those at a university center (83.3% versus 60.7%, P = 0.018) (Table 3; Figs. 1 and 2).
Table 3.
FACTORS INFLUENCING THE DECISION TO PURSUE HEPATOLOGY
| Response, % | |
|---|---|
| (n = 180) | |
| What would attract you to a career in hepatology? | |
| Personal satisfaction | 66 |
| Management of complex, multisystem diseases | 60 |
| Long‐term relationships with patients | 57 |
| Financial compensation | 37 |
| Prestige | 21 |
| Additional board certification | 16 |
| None of the above | 10 |
| Which of the following factors would deter you from a career in hepatology? | |
| Less endoscopy time | 67 |
| Additional length of training | 64 |
| Lack of financial compensation | 44 |
| Additional application process/board certification | 35 |
| Too much financial debt | 33 |
| Possible geographic location | 33 |
| Patient population | 32 |
| Influence of family | 31 |
| Pursuing other subspecialty training | 21 |
| No interest in hepatology | 18 |
| Management of complex multisystem diseases | 9 |
| None of the above | 5 |
| Lack of prestige | 3 |
| Long‐term relationships with patients | 1 |
Figure 1.
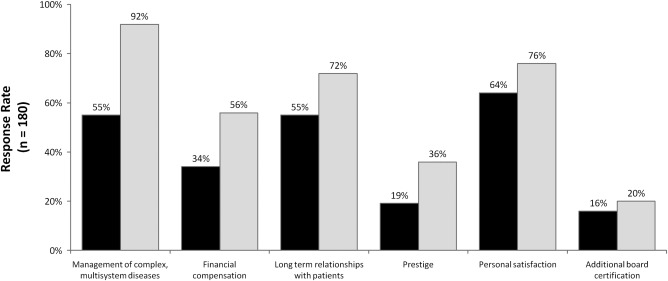
Reported attracting factors among trainees in/planning on entering a TH fellowship compared to those who are not and those who are unsure about pursing TH (180 respondents).
Figure 2.
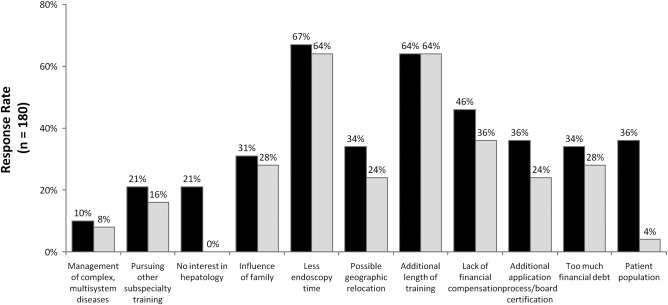
Reported deterring factors among trainees in/planning on entering a TH fellowship compared to those who are not and those who are unsure about pursing TH (180 respondents).
MENTORSHIP
Seventy‐three out of 78 (94%) respondents with mentors reported that their mentors influenced their career decisions, while only 5 responded that their mentor had no influence (Table 4). Twenty‐two percent of mentors were hepatologists. The 25 respondents planning on a career in hepatology were more likely to have a mentor than those not planning on a career in hepatology (88.0% versus 56.8%, P = 0.003); 19 of these reported their mentor practices hepatology. Those with a mentor were more likely to practice at a center with a TH training program (60.0% versus 27.7%, P = 0.002).
Table 4.
MENTOR
| n | Percent (%) | |
|---|---|---|
| Mentor | 110 | 61 |
| No mentor | 70 | 39 |
| Mentor subspecialty | ||
| Hepatology | 40 | 22 |
| Inflammatory bowel disease | 20 | 11 |
| Advanced endoscopy | 20 | 11 |
| General or other | 18 | 10 |
| No answer | 82 | 46 |
Discussion
It is widely assumed GI fellows avoid pursuing hepatology careers due to an increase in length of training and financial disincentive. Unfilled TH programs and declining numbers of transplant hepatologists taking the ABIM TH certification exam suggest the shortage is due in part to the length of time it takes to become a hepatologist.17 Our study is the first to examine these factors. Awareness of these factors may aid in changing how TH programs recruit GI fellows and internal medicine residents.
Our data demonstrate that the additional application process, length of training, and possible geographic relocation are factors frequently cited as deterrents to pursuing training in hepatology. This was especially true among women and those with families. Those working or training at a community‐based center were more likely to list the additional year of training as a deterrent than those at a university center, suggesting university trainees are more comfortable with or more likely to see the value of additional training than those at a community‐based center. We believe increasing awareness about the combined GI/TH pilot program, particularly among community‐based centers, may help mitigate several of these concerns. Unfortunately, nearly a quarter of respondents were not aware of the GI/TH pilot fellowship, suggesting that increasing awareness of the pilot program is an important factor in recruiting applicants to the TH fellowship.
Less endoscopy time was a frequently cited deterrent to a TH fellowship both among those who are and are not planning a hepatology career. Most GI fellows, regardless of a future desire to specialize in hepatology, are attracted to endoscopy and seek to maintain endoscopy as part of their future practice. With this in mind, TH fellowships may consider emphasizing and creating opportunities for endoscopic procedures when recruiting GI fellows.
Our study suggests that the perception of a lower income for hepatologists may be less of a deterrent than assumed. A minority of respondents (44%) reported that lesser financial compensation when compared to their GI counterparts would dissuade them from pursuing additional hepatology training. Debt also did not have a significant impact on the decision to pursue hepatology except in those with a debt greater than $200,000; we attribute this to the financial burden of an extra year of training. We found that those planning on entering hepatology were significantly more likely to be attracted to the financial compensation of hepatology (56.0% versus 33.5%, P = 0.044) when compared to those who were undecided or not planning on hepatology. Perhaps those interested in hepatology receive better guidance on financial compensation available to hepatologists, and making this clearer may improve recruitment. These findings argue against the notion that earning potential and financial inequality are key deterrents for the majority of respondents.
The GI fellow's exposure to TH is often an inpatient experience. This frequently includes a high census of complex decompensated patients associated with a relatively high rate of morbidity and mortality. One study found that exposure to similarly ill patients on inpatient oncology rotations was associated with a decreased interest in pursuing this field among internal medicine residents.18 Few respondents planning on entering hepatology chose the patient population as a deterring factor, but those unsure about or not planning on entering hepatology were more likely to select the patient population as a deterring factor. Compared to 49% of those not planning on entering hepatology, 81% of those unsure about entering hepatology cite long‐term relationships with patients as an attracting factor. Exposing GI fellows to outpatient hepatology rotations where they have the opportunity to engage in longitudinal care, long‐term relationships, and interesting benign hepatology may improve the perception of hepatology as a practice.
Mentoring is known to facilitate career selection, advancement, publication productivity, and grant funding.16, 19, 20, 21 The challenges and increasing demands in academic medicine (aging population with more complex disease, highly competitive research, and less value on teaching in career assessment) have led to the reduction of the number and availability of mentors.8 In our study, most trainees already in or planning on a hepatology fellowship had a mentor. These data underscore the potential impact of mentorship by hepatologists in increasing interest in TH. TH training programs may consider expanding formal mentorship programs, initiating informal gatherings and journal clubs, and establishing awards for outstanding mentorship to foster a developmental climate. Interestingly, the presence of a mentor, regardless of specialty, correlated with a plan for a career in hepatology, suggesting that the career path of the mentor was not as crucial as the mentorship itself.
Our study has several limitations. The survey response rate can only be estimated because it is unclear whether all 441 GI fellows in the AY 2014‐2015 received a survey. Assuming every GI fellow received the survey, the response rate among e‐mail and board review attendee recipients was 180/441 (40.8%). The survey is a descriptive study, which allows us to analyze correlations but limits our understanding of causality. Despite a fair overall response rate, the results may have been biased because some respondents had completed a fellowship. Given that subjects were not supervised for their surveys, respondents may not have interpreted questions consistently. Factors preventing individuals from completing the survey included time constraints, incorrect e‐mail addresses, e‐mail forwarding to the “junk” folder, or lack of interest.
Modification of the deterring factors identified in this study may increase the number of trainees seeking a career in hepatology and help alleviate our deficit of hepatologists. Specifically, our data suggest aggressive measures to boost mentorship and continued support and advertisement of the TH 3‐year pilot program may have a positive impact on hepatologist recruitment. We affirm the need for a current workforce study to accurately assess the current deficit of hepatologists in the United States.
Supporting information
Additional Supporting Information may be found at onlinelibrary.wiley.com/doi/10.1002/hep4.1040/suppinfo.
Supporting Information
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Wise M, Bialek S, Finelli L, Bell BP, Sorvillo F. Changing trends in hepatitis C‐related mortality in the United States, 1995‐2004. Hepatology 2008;47:1128‐1135. [DOI] [PubMed] [Google Scholar]
- 2. Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, et al. The epidemiology of cirrhosis in the United States: a population‐based study. J Clin Gastroenterol 2015;49:690‐696. [DOI] [PubMed] [Google Scholar]
- 3. Cartwright EJ, Rentsch C, Rimland D. Hepatitis C virus screening practices and seropositivity among US veterans born during 1945‐1965. BMC Res Notes 2014;7:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mitchell T, Armstrong GL, Hu DJ, Wasley A, Painter JA. The increasing burden of imported chronic hepatitis B‐‐United States, 1974‐2008: PLoS One 2011;6:e27717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008: Clin Gastroenterol Hepatol 2011;9:524‐530.e1;quiz e60. [DOI] [PubMed] [Google Scholar]
- 6. Bacon BR. Workforce issues in hepatology: what is needed? Hepatology 2008;47:1801‐1804. [DOI] [PubMed] [Google Scholar]
- 7. Rustgi VK, Davis GL, Herrine SK, McCullough AJ, Friedman SL, Gores GJ. Future trends in hepatology: challenges and opportunities. Hepatology 2008;48:655‐661. [DOI] [PubMed] [Google Scholar]
- 8. Luxon BA. Training for a career in hepatology: which path to take? Curr Gastroenterol Rep 2010;12:76‐81. [DOI] [PubMed] [Google Scholar]
- 9. Shiffman ML, Rockey DC. Role and support for hepatologists at liver transplant programs in the United States. Liver Transpl 2008;14:1092‐1099. [DOI] [PubMed] [Google Scholar]
- 10. HCV Research and News . Revamping a specialty: advanced/ transplant hepatology. Gastroenterology & Endoscopy News 2011;62:10 http://hepatitiscresearchandnewsupdates.blogspot.com/2011/11/revamping‐specialty‐advancedtransplant.html. Accessed March 20, 2017. [Google Scholar]
- 11. Rosen HR, Fontana RJ, Brown RS, Wiesner RH, Schiano TD, Bass NM, et al. Curricular guidelines for training in transplant hepatology. Liver Transpl 2002;8:85‐87. [DOI] [PubMed] [Google Scholar]
- 12. Friedman LS, Brandt LJ, Elta GH, Fitz JG, Gores GJ, Katz PO, et al. Report of the Multisociety Task Force on GI training. Hepatology 2009;50:1325‐1329. [DOI] [PubMed] [Google Scholar]
- 13. American Association for the Study of Liver Diseases . ABIM Pilot Program for stimulating competency‐based education reform in graduate medical education. https://www.aasld.org/events-professional-development/gitransplant-hepatology-pilot. Accessed March 20, 2017.
- 14. Russo MW, Koteish AA, Fuchs M, Reddy KG, Fix OK. Workforce in hepatology: Update and a critical need for more information. Hepatology 2017;65:336‐340. [DOI] [PubMed] [Google Scholar]
- 15. Grayson MS, Newton DA, Thompson LF. Payback time: the associations of debt and income with medical student career choice. Med Educ 2012;46:983‐991. [DOI] [PubMed] [Google Scholar]
- 16. Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA 2006;296:1103‐1115. [DOI] [PubMed] [Google Scholar]
- 17. Halegoua‐De Marzio DL, Herrine SK. Training directors have positive perceptions of a competency‐based gastroenterology and transplant hepatology fellowship program. Clin Gastroenterol Hepatol 2015;13:398‐401.e3. [DOI] [PubMed] [Google Scholar]
- 18. McFarland DC, Holland J, Holcombe RF. Inpatient hematology‐oncology rotation is associated with a decreased interest in pursuing an oncology career among internal medicine residents. J Oncol Pract 2015;11:289‐295. [DOI] [PubMed] [Google Scholar]
- 19. Sambunjak D. Understanding wider environmental influences on mentoring: towards an ecological model of mentoring in academic medicine. Acta Med Acad 2015;44:47‐57. [DOI] [PubMed] [Google Scholar]
- 20. Sambunjak D, Straus SE, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 2010;25:72‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ramanan RA, Taylor WC, Davis RB, Phillips RS. Mentoring matters. Mentoring and career preparation in internal medicine residency training. J Gen Intern Med 2006;21:340‐345. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional Supporting Information may be found at onlinelibrary.wiley.com/doi/10.1002/hep4.1040/suppinfo.
Supporting Information


