Abstract
Background:
Hepatitis C virus (HCV) is a major cause of liver disease and a potential cause of substantial morbidity and mortality. This study aims to provide a comprehensive evidence on HCV Infection in Iranian hemodialysis (HD) patients we conducted a systematic review.
Materials and Methods:
In this systematic review and meta-analysis, through a comprehensive search of literature until January of 2016, we estimated the pooled prevalence of hepatitis C infection in Iranian HD patients. Using Medical Subject Headings terms, Emtree, and related equal Persian key words for Iranian databases and also international databases of PubMed and NLM Gateway (for MEDLINE), and SCOPUS. Interest outcome of HCV infection prevalence was confirmed based on positive hepatitis B surface antigen of blood samples. Random effect meta-analysis was used to estimate pooled prevalence of HCV infection in Iranian HD patients, date and language, HD patients, in adult HD patients, Institute of Scientific Information, Iran-doc, irrespective of age, living in Iran. Searches run through main domestic databanks of Iran-Medex, renal transplantation, Scientific Information Database, the relevant literature-searched concentrating on HCV infection.
Results:
Through searching steps, 305 publications were found from them following the excluding duplicates and overlapping studies 54 studies relevant to HCV prevalence in Iranian HD zcxw patients, with number of 23921 participants, remained in our analyses. The overall results of test of heterogeneity demonstrate sever heterogeneity between reported prevalence (I2 = 96.62%, Chi-square = 1566, P < 0.001). Due to sever heterogeneity results of random effect meta-analysis showed that the estimated pooled prevalence was 11% (95% confidence interval [CI] =10%–13%). The pooled prevalence base on polymerase-chain reaction, recombinant immunoblot assay, and enzyme-Linked Immunosorbant Antibody method were 11% (95% CI = 6%–15%), 9% (95% CI = 5–13) and 12% (95% CI = 10–14), respectively. In line with previous studies, the present finding shows the significant variation in the rate of HCV in dialysis units among the regions in Iran.
Conclusion:
Present paper is the comprehensive updated systematic review on HCV prevalence in the Iranian HD patients. Our findings provide the reliable evidence for promotion of policies and interventional programs.
Keywords: Hemodialysis, hepatitis C virus, Iran, systematic review
INTRODUCTION
Hepatitis C virus (HCV) is a major cause of liver disease and a potential cause of substantial morbidity and mortality in the future[1] HCV infection remains highly prevalent in developed and developing countries. In spite of significant decrease in the incidence and prevalence of HCV among Iranian hemodialysis (HD) patients, it is still a great concern of health priorities Infection due to HCV is one of the leading causes of morbidity and mortality around the world. Available data show 54,000 annual deaths and 955,000 annual disability-adjusted life years (DALYs) globally due to acute HCV infection.[1]
HCV has an impact on the life expectancy of HD patients.[2] In Asia-pacific region, HCV infection led to 57.29, 59.92, and 66.45 DALYs (per 100,000 population) in 1990, 2000, and 2010, respectively. DALYs and death rates showed a little decline trend for HCV cirrhosis; however, DALYs and death rates increased for acute hepatitis and liver cancer due to patients with HCV.[3]
Compare to the developed countries, there is a wide variation in the prevalence estimates among developing countries, and generally, less data available to validate assumptions about the burden of disease. This requires a comprehensive review of data reviewing that are among the world's most populous nations.[1,4]
A systematic review of national studies between 2001 and 2008 reported a 0.16% seroprevalence of HCV infection. In this investigation, the prevalence of HCV in high-risk groups such as HD patients was as high as 30%–90%.[5,6] Considering these results, a study on seroprevalence in Iran showed a high prevalence of 14.4% in 1999 and 4.5% in 2006 of HCV among patients undergoing HD.[7,8]
The previous systematic review study has conducted on the prevalence of hepatitis C in HD patients in 2010. In this investigation based on eighteen studies from 12 provinces (consisting 49.02% of the Iranian total population) and with the recombinant immunoblot assay (RIBA) method, the HCV infection prevalence in Iranian HD patients estimated as 7.61% (95% confidence interval [CI]: 6.06–9.16%).[9] Due to the increased trends in recent investigations and priority of this problem, there is a progressive need to evidence supporting related policies and programs all over the word. Another new attempt focus on determine HCV infection prevalence in the Middle-East countries and the overall prevalence of the region. Based on 56 studies were selected reporting the prevalence of HCV infection among HD patients from ten countries of the region; the overall HCV infection prevalence among HD patients in the estimated as 25.3%. In this evaluation, Egypt and Syria had the highest and Iran and Lebanon had the lowest rates of infection.[10]
Considering the limitations of each of the previous studies and benefitting from a well-developed protocol for comprehensive data gathering, we conducted a systematic review and meta-analysis to put all evidence on prevalence of Hepatitis C infection in Iranian HD patients.
MATERIALS AND METHODS
In this systematic review and meta-analysis, through a comprehensive search of published and gray literature until January of 2016, we estimated the pooled prevalence of hepatitis C infection in Iranian HD patients.
Eligibility criteria
Irrespective of date of study and language of documents, we included all related cross-sectional studies. If there were more than one document that was extracted from one source of data, more complete reported was considered. We also excluded article with duplicate citations.
Search strategy
Using Medical Subject Headings terms, Emtree, and related equal Persian key words for Iranian databases, irrespective of age, date and language, the relevant literature searched concentrating on HCV infection, HD patients, renal transplantation, in adult HD patients, living in Iran. Searches run through main domestic databanks of Iran-Medex, Scientific Information Database, Iran-doc, and also international databases of PubMed and NLM Gateway (for MEDLINE), Institute of Scientific Information, and SCOPUS. Interest outcome of HCV infection prevalence was confirmed based on positive hepatitis B surface antigen of blood samples.
Moreover the electronic sources, we found 36 national, regional, and international Iranian medical science-related congresses from related gray literature. We also searched the research projects of 15 out of 42 Iranian universities of medical sciences from their websites. The references and citations of relevant articles were also assessed.
Other resources
Related gray literature and detected reference lists of relevant primary studies and related key journals were searched for additional sources of information.
Quality assessment and data extraction
This systematic review included all relevant cross-sectional and analytical studies which have conducted in native Iranian HD patients. The quality of studied assessed based on critical appraisal skills programme tools. There was not any restriction in terms of age and gender of the participants or jobs or type of background diseases which need to be treated by HD.
The data were extracted by a checklist which was recording; citation, publication year, study year, place of study, type of study, population, total sample size, mean age, type of measure, results of measures, and other information. All process of search and data extraction was followed independently by two research experts (Kappa statistic for agreement for quality assessment; 0.92) and probable discrepancy between them resolved based on third expert opinion.
Statistical analysis
The results presented as prevalence and 95% CI. The CI was estimated using the exact or Clopper-Pearson method.[11] The Chi-square-based Q-test using I square statistics used to assess the heterogeneity of between studies reported prevalence. The I2 statistic value ≤30%, 30%–70%, and ≥ 70% was considered as mild, moderate, and sever heterogeneity, respectively.[12] The result of Q-test was regarded to be statistically significant at P < 0.1.
The meta-analysis used to assess the pooled prevalence of hepatitis C infection in Iranian HD patients. Due to severe heterogeneity among studies regarding reported values, pooled prevalence was estimated using random-effect meta-analysis model (using the DerSimonian and Laird method). Forest plot also was used to present result of meta-analysis for the prevalence of HCV in Iranian HD patients schematically. Subgroup meta-analysis was performed to estimate the prevalence of HCV infection according to type of kit. The analyses were conducted using STATA Corp. 2011 (Stata Statistical Software, Release 11, StataCorp LP, Package, College Station, TX, USA) using “Metaprop” command.[13]
Ethical considerations
Protocol of study was approved by the ethical committee of Alborz University of Medical Sciences. All of included studies in our review would be cited in all reports and all publications of our study. Whenever we needed more information about a certain study, for obtaining required information, we contacted the corresponding author.
RESULTS
We refined data for the prevalence of HCV infection in Iranian HD patients. Through searching steps 305 publications were found from them 243 papers were found from international data bases, and other were from Iranian data banks. Following the excluding duplicates and overlapping studies, 189 of these publications were not related to aim of the present study base on reading the titles and abstracts. Finally, after further assessments, 54 studies relevant to HCV prevalence in Iranian HD patients remained in our list [Figure 1].[4,7,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]
Figure 1.
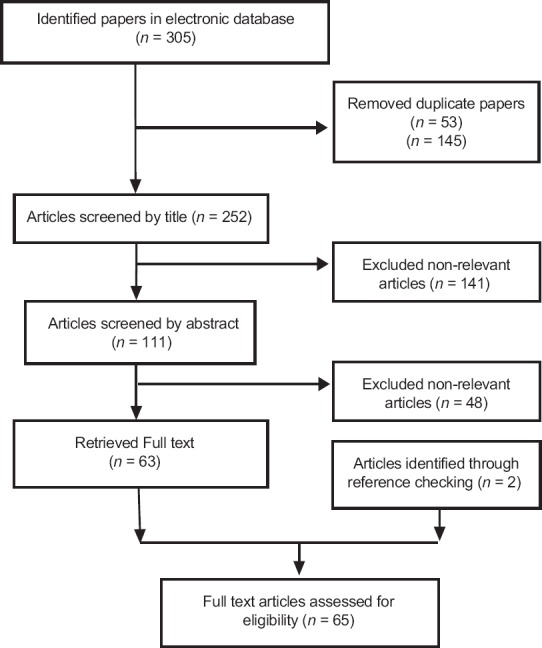
Papers search and review flowchart for selection of primary study
All of searched documents were in English or Persian language. Considering the geographic distribution, five studies were at national level, and rest of them were at provincial or district level. One study's level was not clear. Retrieving articles were assigned to studies conducted between 1990 and 2015. Eleven papers did not mention their study years. The maximum and minimum mean age of patients was 62.1614 years old, respectively. Considering the systematic review results, 35 of the studies were reported based on Enzyme-Linked Immunosorbent Antibody (ELISA) as an HCV infection-detecting method. Rest of studies considered other methods such as polymerase chain reaction (PCR) (8 studies), RIBA (6 studies) [Table 1].
Table 1.
The results of including papers hepatitis C virus infection in the hemodialysis patients of Iran
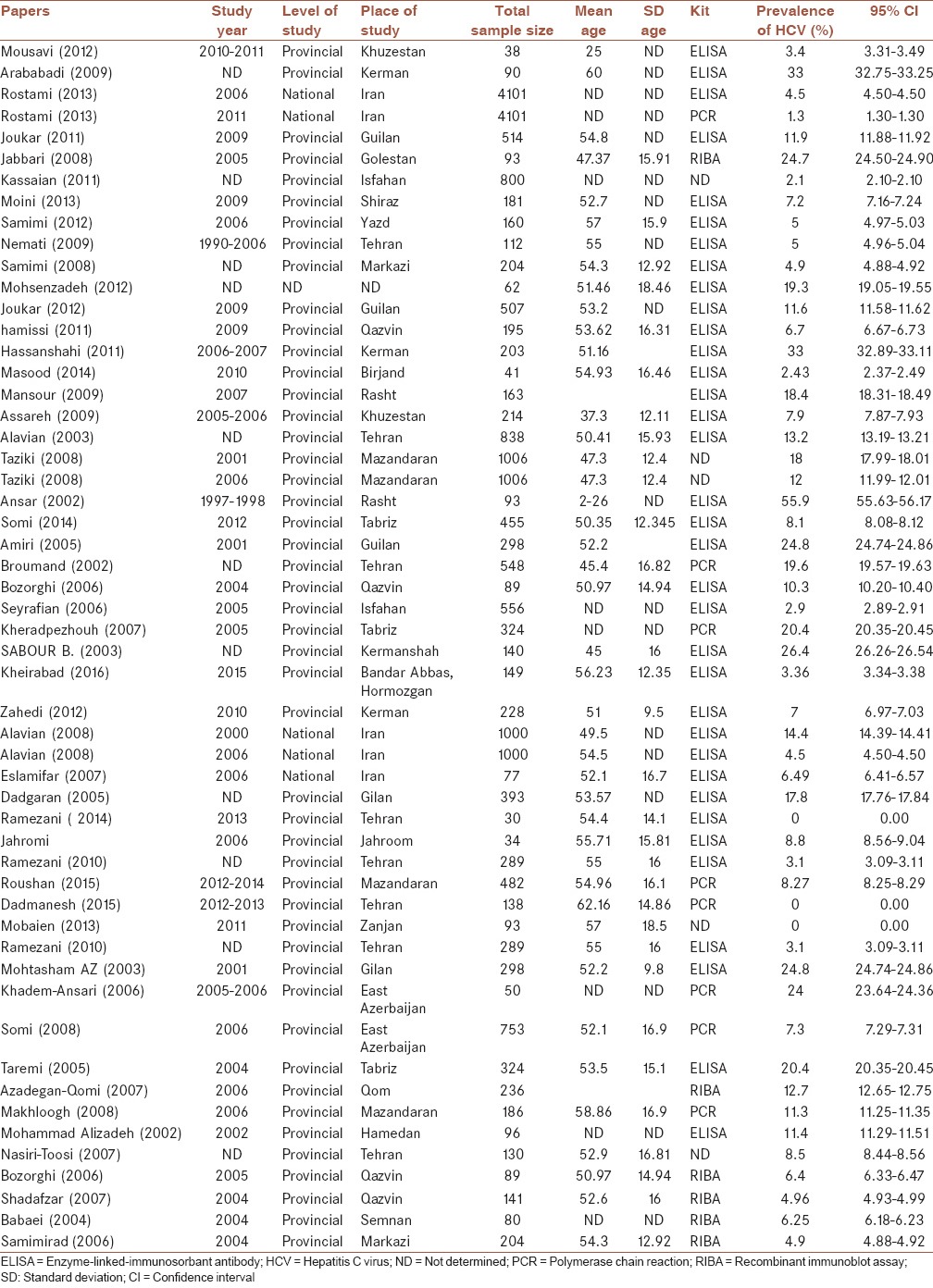
The prevalence rate varied from 0% in Tehran and Zanjan to 55.90% in Kerman. The national prevalence of HCV was reported between 1.30% up to 14.40 [Table 1].
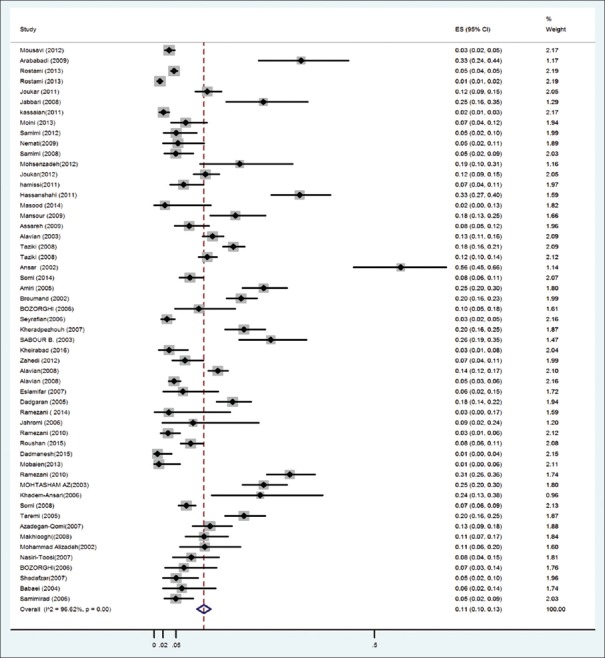
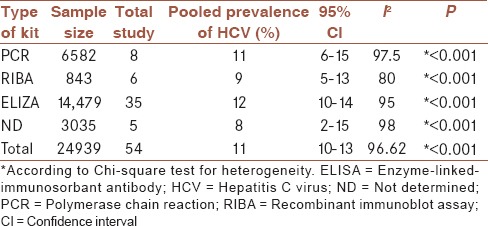
Reported percentages were heterogeneous. The overall results of test of heterogeneity demonstrate sever heterogeneity between reported prevalence (I2 = 96.62%, Chi-square = 1566, P < 0.001) [Figure 2]. Due to sever heterogeneity based on random effect meta-analysis, the estimated pooled prevalence reported as 11% (95% CI = 10%–13%) [Table 2]. Results of subgroup meta-analysis show that the pooled prevalence of HCV infection according to PCR, RIBA, ELIZA kit was 11%(95% CI = 6–15), 9% (95% CI = 5–13), and 12% (95% CI = 10–14), respectively. In addition, the estimated pooled prevalence, based on not determined kit, estimated as 8% (95% CI = 2%–15%).
Figure 2.
Prevalence of hepatitis C virus infection in Iranian hemodialysis patients
Table 2.
Prevalence of hepatitis C virus infection among hemodialysis patients according to type of kit
DISCUSSION
Patients involved with end-stage renal diseases need to be dialyzed through blood or peritoneal ways, that especially poses them to meet blood–borne infectious like hepatitis B and C.[47,62] In line with previous studies present finding show the significant variation in the rate of HCV in dialysis units among the regions in Iran. An overall results of test of heterogeneity demonstrate sever heterogeneity between reported prevalence (I2 = 96.62%, Chi-square = 1566, P < 0.001). Due to sever heterogeneity results of random effect meta-analysis showed that the estimated pooled prevalence was 11% (95% CI = 10%–13%). The pooled prevalence base on PCR, RIBA, and ELIZA were 11% (95% CI = 6%–15%, CI = 5–13, CI = 10–14) and it was 8% (95% CI = 2%–15%) base on not determined kit studies.
Latest studies depicted the HCV prevalence in the Iran HD unites to be in range of 7.61% to 12%, which was about 1 time greater than the prevalence of the present study. It may be due to sample of the studies number; in this study, 54 studies were selected reporting the prevalence of HCV infection in HD patients in Iran, in against the latest studies in 2010 and 2017, respectively, 18, 21 studies were reported from Iran.[9,10]
HCV infection has been known as a major problem in dialysis patients and its prevalence varies significantly among different regions of the world. In HD groups, many factors such as blood transfusion, impaired cellular immunity, frequent hospitalization, and underlying diseases, increase the risk of infection and its adverse health outcomes.[63,64]
In Iran, comparing to the general population, there are higher detected prevalence of HCV infection in HD patients that across the different provinces HCV prevalence show considerably variation from 5.5% to over 24%.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67]
This review shows that the pooled prevalence of HCV infection among HD patients was 11% (95% CI: 10% to 13%) in 24,939 persons who were studied from 1990 to 2015. Assessed estimation significantly is lower than those of Pakistan (23.7%), Jordan (32.5%), Kuwait (43.4%), and Saudi Arabia (50.5%), but higher than those of Australia (2.3%), United Kingdom (2.7%), Germany (3.9%), and Bahrain (7.4%).[2] According to a recent meta-analysis in Iran, the prevalence of HCV infection among this group of patients was reported to be 13.6%, 12.2%, and 7.6%, respectively, by ELISA, RIBA, and PCR.[68]
Regarding the estimation of HCV prevalence in HD patients, Perumalet, Reddy, Harmankaya, and Ocak through four-independent studies reach to results of 15%, 4.7%, and 5.9%, 12.7%, respectively.[69,70,71,72] In Asia-Pacific countries, the prevalence of HCV infection and HCV seroprevalences estimated between 0.7%–18.1% and 0.7%–18.1%, respectively.[73,74]
A systematic review of national studies between 2001 and 2008 reported a 0.16% seroprevalence of HCV infection. In this investigation, the prevalence of HCV in high-risk groups such as HD patients was as high as 30%–90%.[5,6] Considering these results, a study on seroprevalence in Iran showed a high prevalence of 14.4% in 1999 and 4.5% in 2006 of HCV among patients undergoing HD.[7,8]
Evidence confirmed that HCV-infected HD patients have 1.4 times more chance for dying than uninfected HD patients.[71] HCV infection was highly predictive of mortality in Japan (relative risk 1.37, 95% CI: 1.15–1.62, P = 0.003), Australia, and New Zealand (adjusted hazards ratio 1.29, 95% CI: 1.05–1.58).[73]
In the present study, the HCV prevalence according to the data of 21 provincials and 5 national studies was 12% (95% CI: 10%–14%) with ELISA; 9% (95% CI: 5%–13%) with the RIBA and 11% (95% CI: 6%–15%) with PCR method according to the national epidemiological survey of HCV from April 2001 to March 2008, HCV infection rate among the HD patients estimated 13.57% (95% CI: 9.86%–17.21%) with ELISA and 7.61% (95% CI: 6.06%–9.16%) with the RIBA/PCR method.[9]
This decline coincides with the worldwide decreasing trend and is attributed to the improved patient care and infection control practices, screening for blood products, and the strict adherence to universal hygiene precautions.[75] It seems that fulfillment of compulsory thorough blood donor screening in Iran since 1995 and decline of transfusion number led to decreasing occurrence of HCV and HBV infection in HD patients. In recent years, the hospital-transmitted infections have played an increasing role. In addition, duration of the HD period was an independent risk factor for the acquisition of HCV infection regardless of the number of blood transfusions, and a history of previous renal transplantation.[7,76] In addition, routinely screened HD patients for this infection, and adherence to standard infection control practices will remain the key strategies for preventing HCV transmission in HD units.[77]
Based on our study, most routine screening tests for HCV infection in HD units were second- and third-generation ELISA. However, the actual prevalence of HCV is difficult to assess because serological tests do not discriminate among acute, chronic, or resolved infection. This systematic review assessed 8 studies which were used reverse transcriptase PCR (RT-PCR) for HCV RNA. This test is designed based on reverse transcription of viral RNA; using this technique, the prevalence of HCV was lower than routine methods. As the results showed the HCV prevalence according to this data was 12% (95% CI: 10%–14%) with ELISA and 9% (95% CI: 5%–13%) with the RIBA and 11% (95% CI: 6%–15%) with PCR method. One explanation to these lower results is that antibody-positive participants did not have positive RT-PCR results because they had cleared HCV viremia. Other probability is that false-positive ELISA and RIBA results for HCV are frequent.[78] Thus, researchers were attempted to design more useful techniques to identify viral genomes, such as RT-PCR.[26]
Nearly from the year 2001, there has been a steady decline in this incidence in all region.[9] In our study, compared with other regions, South West and North of Iran had relatively higher HCV prevalence rate among HD patients, accounting for 55.9% and 33.3% in Rasht and Kermanshah. Meanwhile, the lowest epidemic rate was found in central and Northern west 0%, 2.1%, and 0% in Tehran, Zanjan, and Isfahan. Notably, previous studies also reported the highest HCV infection prevalence 24.8% (19.9–29.7) in Gilan.[9,32,34] High prevalence of HCV infection has been shown among HD patients in some provinces of Iran such as Kermanshah (26.4%), Golestan (24.7%), and West Azarbaijan (24%).[9] In contrast, result of Joukar's study showed lower rate of HCV prevalence (11.9%) in HD patients in Guilan province. However, some provinces such as Zanjan, Isfahan, Birjand, hormozgan, Khuzestan, Markazi, Ghazvin and Yazd reported an anti-HCV infection prevalence rate equal and lower than 5%, in particular, low rate of anti-HCV infection was reported in the center and the south of Iran. This may be due to the method of evaluating HCV infection (ELISA and not determined, respectively), which can be interpreted as a falsely high HCV infection prevalence.[17] Reports on the prevalence of HCV infection in special populations in Iran are as high as 11%–25% for patients on HD[79] Taziki et al. reported 12% for HCV prevalence rate, and also showed HCV prevalence rate in HD patients has reduced during the past decade in the Mazandaran province in northern Iran.[31] It is noteworthy that the key to reducing the incidence of viral hepatitis in HD patients is to control contagion and reduce the frequency of blood transfusion and cross-infection.[80] Differences in HCV infection prevalence might be due to local risk factors in different Iranian regions.[21] Some factors such as using some other prevention modalities and having less contact with neighbors of country, hepatitis care plans, usage rate of dialysis beds, dialysis durations, and HCV detecting tests may be responsible for these rates.
In our study, data were restricted to the north, east, south and central provinces of Iran. We do not have any studies from provinces that are located in the West of Iran. Of course these data is more comprehensive than previous studies.[9] Therefore we need to follow studies about HCV prevalence in HD patients which are related to these parts of Iran for more precise and accurate estimation.
In present study 55.9% of HCV infected HD patients were in the of 2–26 years age group. Most of the related studies have not reported any statistical difference of prevalence of HCV infected in different age groups. Fattahi et al. showed that higher prevalence of HCV-positive was seen in age ≤12 years old.[81] The interesting finding of Bhaumik and Debnath study confirmed that compare to general population, in HD patients, HCV infection occur at much early age.[82] In contrast, Alaviyan demonstrated that most of the HBV/HCV infected patients (67%) were in the age group of 31–50 years.[70]
HCV infection can be transmitted by infected hands of the medical staff, HD machines, other medical equipment's, or objects circulating between patients, for example swabs, plaster rolls, disinfection fluid bottles, dish trays, etc. Dental or surgical intervention, salivary inoculation, family members infected with HCV, cocaine abuse, HIV infection, and lower socioeconomic position also each correlate with an increased risk of this infection.[6] To enforce isolation strategies and assigning individual nurses for these patients and surveillance of universal precaution in dialysis units may play an important role in decreasing the spread of this infection further in coming years.[7]
This is a comprehensive systematic review on prevalence of Hepatitis C infection in the Iranian HD patients that included all available data of eligible studies. Our findings have some limitations. The first one is our study is restricted to the north, east, south, and central provinces of Iran. We do not have any studies from provinces that are located in the west of Iran. Therefore, we need to follow studies about HCV prevalence in HD patients which are related to these parts of Iran for more precise and accurate estimation. The second one is the heterogeneity of searched results that limits the generalization of our findings.
CONCLUSIONS
This is the comprehensive updated systematic review on HCV prevalence in the Iranian HD patients. Our findings could be useful to the promotion of prevention policies and interventional programs. Standardized isolation strategies and assigning individual nurses for these patients and surveillance of universal precaution in dialysis units may play an important role in decreasing the spread of this infection.
Financial support and sponsorship
This project was funding by Alborz University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are thankful of Bahonar Hospital Clinical Research Development Unit for their assistance.
REFERENCES
- 1.Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5:558–67. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- 2.Taherkhani R, Farshadpour F. Epidemiology of hepatitis C virus in Iran. World J Gastroenterol. 2015;21:10790–810. doi: 10.3748/wjg.v21.i38.10790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The 22nd conference of the Asian Pacific association for the study of the liver: APASL 2012-Taipei, Taiwan-16-19 February. Hepatol Int. 2012;6:67–309. doi: 10.1007/s12072-011-9333-4. [DOI] [PubMed] [Google Scholar]
- 4.Moini M, Ziyaeyan M, Aghaei S, Sagheb MM, Taghavi SA, Moeini M, et al. Hepatitis C virus (HCV) infection rate among seronegative hemodialysis patients screened by two methods; HCV core antigen and polymerase chain reaction. Hepat Mon. 2013;13:e9147. doi: 10.5812/hepatmon.9147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alavian SM, Ahmadzad-Asl M, Lankarani KB, Shahbabaie MA, Bahrami Ahmadi A, Kabir A. Hepatitis C infection in the general population of Iran: A systematic review. Hepat Mon. 2009;9:211–23. [Google Scholar]
- 6.Tillmann HL, Manns MP. Mode of hepatitis C virus infection, epidemiology, and chronicity rate in the general population and risk groups. Dig Dis Sci. 1996;41:27S–40S. doi: 10.1007/BF02087874. [DOI] [PubMed] [Google Scholar]
- 7.Alavian SM, Bagheri-Lankarani K, Mahdavi-Mazdeh M, Nourozi S. Hepatitis B and C in dialysis units in Iran: Changing the epidemiology. Hemodial Int. 2008;12:378–82. doi: 10.1111/j.1542-4758.2008.00284.x. [DOI] [PubMed] [Google Scholar]
- 8.Liang TJ. Current progress in development of hepatitis C virus vaccines. Nat Med. 2013;19:869–78. doi: 10.1038/nm.3183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alavian SM, Kabir A, Ahmadi AB, Lankarani KB, Shahbabaie MA, Ahmadzad-Asl M, et al. Hepatitis C infection in hemodialysis patients in Iran: A systematic review. Hemodial Int. 2010;14:253–62. doi: 10.1111/j.1542-4758.2010.00437.x. [DOI] [PubMed] [Google Scholar]
- 10.Ashkani-Esfahani S, Alavian SM, Salehi-Marzijarani M. Prevalence of hepatitis C virus infection among hemodialysis patients in the middle-east: A systematic review and meta-analysis. World J Gastroenterol. 2017;23:151–66. doi: 10.3748/wjg.v23.i1.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–13. [Google Scholar]
- 12.Fletcher J. What is heterogeneity and is it important? BMJ. 2007;334:94–6. doi: 10.1136/bmj.39057.406644.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nyaga VN, Arbyn M, Aerts M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mousavi SS, Hajiani E, Hayati F, Hashemi SJ, Shayesteh A, Behbehani SM, et al. Epidemiology of hepatitis C virus infection in ESRD patients in Khuzestan Province, Iran. Shiraz E Med J. 2012;13:135–40. [Google Scholar]
- 15.Arababadi MK, Hassanshahi G, Yousefi H. HBV-DNA in hemodialysis patients infected by HCV. Saudi J Kidney Dis Transpl. 2009;20:398–401. [PubMed] [Google Scholar]
- 16.Rostami Z, Lessan Pezeshki M, Soleimani Najaf Abadi A, Einollahi B. Health related quality of life in iranian hemodialysis patients with viral hepatitis: Changing epidemiology. Hepat Mon. 2013;13:e9611. doi: 10.5812/hepatmon.9611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joukar F, Besharati S, Mirpour H, Mansour-Ghanaei F. Hepatitis C and hepatitis B seroprevalence and associated risk factors in hemodialysis patients in Guilan Province, North of Iran: HCV and HBV seroprevalence in hemodialysis patients. Hepat Mon. 2011;11:178–81. [PMC free article] [PubMed] [Google Scholar]
- 18.Jabbari A, Besharat S, Khodabakhshi B. Hepatitis C in hemodialysis centers of Golestan Province, Northeast of Iran (2005) Hepat Mon. 2008;8:61–5. [Google Scholar]
- 19.Kassaian N, Nokhodian Z, Babak A, Ataei B, Adibi P. Hepatitis C in patients with multi blood transfusion. J Isfahan Med Sch. 2011;28:1560–4. [Google Scholar]
- 20.Samimi-Rad K, Hosseini M, Mobeini G, Asgari F, Alavian SM, Tahaei ME, et al. Hepatitis C virus infection among multi-transfused patients and personnel in haemodialysis units in central Islamic Republic of Iran. East Mediterr Health J. 2012;18:227–35. doi: 10.26719/2012.18.3.227. [DOI] [PubMed] [Google Scholar]
- 21.Nemati E, Alavian SM, Taheri S, Moradi M, Pourfarziani V, Einollahi B, et al. Hepatitis C virus infection among patients on hemodialysis: A report from a single center in Iran. Saudi J Kidney Dis Transpl. 2009;20:147–53. [PubMed] [Google Scholar]
- 22.Samimi-Rad K, Hosseini M, Shahbaz B. Hepatitis C virus infection and HCV genotypes of hemodialysis patients. Iran J Public Health. 2008;37:146–52. [Google Scholar]
- 23.Mohsenzadeh M, Jafari M, Afkari R, Yaghobi R, Pirouzi A. Molecular evaluation of hepatitis G virus and hepatitis C virus in patients with chronic renal failure in Iran. Afr J Microbiol Res. 2012;6:6257–61. [Google Scholar]
- 24.Joukar F, Mansour-Ghanaei F, Besharati S, Khosh-Sorur M. Occult hepatitis B infection in a hemodialysis population in Guilan Province, Northern Iran. Hemodial Int. 2012;16:294–7. doi: 10.1111/j.1542-4758.2011.00645.x. [DOI] [PubMed] [Google Scholar]
- 25.Hamissi J, Mosalaei S, Yousef J, Ghoudosi A, Hamissi H. Occurrence of hepatitis B and C infection among hemodialyzed patients with chronic renal failure in Qazvin, Iran: A preliminary study. Health Med J. 2011;5:301–6. [Google Scholar]
- 26.Hassanshahi G, Arababadi MK, Assar S, Hakimi H, Karimabad MN, Abedinzadeh M, et al. Post-transfusion-transmitted hepatitis C virus infection: A study on thalassemia and hemodialysis patients in Southeastern Iran. Arch Virol. 2011;156:1111–5. doi: 10.1007/s00705-011-0950-y. [DOI] [PubMed] [Google Scholar]
- 27.Masood Z, Roghiye A, Hasan NM. Prevalence of HCV infection in hemodialysis patients of South Khorasan in comparison with HBV, HDV, HTLV I/II, And HIV infection. Bangladesh J Med Sci. 2014;13:36–9. [Google Scholar]
- 28.Mansour-Ghanaei F, Sadeghi A, Mashhour MY, Joukar F, Besharati S, Roshan ZA, et al. Prevalence of hepatitis B and C infection in hemodialysis patients of Rasht (Center of Guilan Province, Northern Part of Iran) Hepat Mon. 2009;9:45–9. [Google Scholar]
- 29.Assarehzadegan MA, Shakerinejad G, Noroozkohnejad R, Amini A, Rahim Rezaee SA. Prevalence of hepatitis C and B infection and HC V genotypes among hemodialysis patients in Khuzestan Province, Southwest Iran. Saudi J Kidney Dis Transpl. 2009;20:681–4. [PubMed] [Google Scholar]
- 30.Alavian SM, Einollahi B, Hajarizadeh B, Bakhtiari S, Nafar M, Ahrabi S, et al. Prevalence of hepatitis C virus infection and related risk factors among Iranian haemodialysis patients. Nephrology (Carlton) 2003;8:256–60. doi: 10.1046/j.1440-1797.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- 31.Taziki O, Espahbodi F. Prevalence of hepatitis C virus infection in hemodialysis patients. Saudi J Kidney Dis Transpl. 2008;19:475–8. [PubMed] [Google Scholar]
- 32.Ansar MM, Kooloobandi A. Prevalence of hepatitis C virus infection in thalassemia and haemodialysis patients in North Iran-Rasht. J Viral Hepat. 2002;9:390–2. doi: 10.1046/j.1365-2893.2002.00368.x. [DOI] [PubMed] [Google Scholar]
- 33.Somi MH, Etemadi J, Ghojazadeh M, Farhang S, Faramarzi M, Foroutan S, et al. Risk factors of HCV seroconversion in hemodialysis patients in Tabriz, Iran. Hepat Mon. 2014;14:e17417. doi: 10.5812/hepatmon.17417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amiri ZM, Shakib AJ, Toorchi M. Seroprevalence of hepatitis C and risk factors in haemodialysis patients in Guilan, Islamic Republic of Iran. East Mediterr Health J. 2005;11:372–6. [PubMed] [Google Scholar]
- 35.Broumand B, Shamshirsaz AA, Kamgar M, Hashemi R, Aiazi F, Bekheirnia M, et al. Prevalence of hepatitis C infection and its risk factors in hemodialysis patients in tehran: Preliminary report from “the effect of dialysis unit isolation on the incidence of hepatitis C in dialysis patients” project. Saudi J Kidney Dis Transpl. 2002;13:467–72. [PubMed] [Google Scholar]
- 36.Bozorghi S, Ramezany H, Vahid T, Mostajeri A, Karegharfard H, Rezayi M, et al. Assessment of prevalence and risk factors of hepatitis C virus infection in haemodialysis patients in Ghazvin. Sci J Blood Transfus Organ. 2006;2:331–337. [Google Scholar]
- 37.Seyrafian S, Mobasherizadeh S, Javadi A, Akhzari M, Esfandiari J. Comparison and prevalence of hepatitis B and C infection and hepatitis B vaccination in hemodialysis patients and staffs in 13 hemodialysis centers in Isfahan (Iran) Nephrol Dial Transplant. 2006;15:12–21. [Google Scholar]
- 38.Kheradpezhouh M, Taremi M, Gachkar L, Aghabozorgi S, Khoshbaten M. Presence and significance of transfusion-transmitted virus infection in Iranian patients on maintenance hemodialysis. J Microbiol Immunol Infect. 2007;40:106–11. [PubMed] [Google Scholar]
- 39.Sabour B, Boroumand P, Mehrabi YE, Ghanbari M, Zarrinfam H. Prevalence and risk factors of hepatitis C infection in hemodialysis patients (Kermanshah, 1999-2000) Behbood Journal. 2003;7:60–6. [Google Scholar]
- 40.Kargar Kheirabad A, Bahri F, Kargar M, Ghasemzadeh I. Hepatitis C and G virus infection prevalence among hemodialysis patients and associated risk factors in the Hormozgan Province of Southern Iran. Hepat Mon. 2016;16:e40375. doi: 10.5812/hepatmon.40375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zahedi MJ, Darvish Moghaddam S, Alavian SM, Dalili M. Seroprevalence of hepatitis viruses B, C, D and HIV infection among hemodialysis patients in Kerman Province, South-East Iran. Hepat Mon. 2012;12:339–43. doi: 10.5812/hepatmon.5969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eslamifar A, Hamkar R, Ramezani A, Ahmadi F, Gachkar L, Jalilvand S, et al. Hepatitis G virus exposure in dialysis patients. Int Urol Nephrol. 2007;39:1257–63. doi: 10.1007/s11255-007-9267-x. [DOI] [PubMed] [Google Scholar]
- 43.Dadgaran S. Prevalence and risk factors of hepatitis C virus among hemodialysis patients. J Guilan Univ Med Sci. 2005;14:76–86. [Google Scholar]
- 44.Ramezani A, eslamifar A, Banifazl M, Keyvani H, Razaghi E, Ahmadi F, et al. Occult HCV infection in hemodialysis patients with elevated liver enzymes. Arak Med Univ J. 2014;16:120–7. [Google Scholar]
- 45.Sotoodeh Jahromi A, Nejatollahi F, Hossaini M. Prevalence of anti HCV antibody hemodialysis patients refering to hemmodialysis unit of Jahrom. Jahrom Univ Med Sci J. 2008;5:38–43. [Google Scholar]
- 46.Ramezani A, Banifazl M, Kalantar E, Ahmadi F, Razaghi E, Eslamifar A, et al. Hepatitis B prevalence of latent infection in hemodialysis patients. J Infect Dis. 2010;14:27–30. [Google Scholar]
- 47.Hasanjani Roushan MR, Farokhtabar S, Bayani M, Siadati S. Epidemiological aspects of hepatitis B and C and human immunodeficiency viruses among hemodialysis patients in Mazandaran Province, Iran. Nephrourol Mon. 2016;8:e37878. doi: 10.5812/numonthly.37878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dadmanesh M, Hosseinzadeh M, Keyvani H, Ghorban K, Rahimi M, Hosseinzadeh M, et al. Evaluation of prevalence and risk factors of hepatitis G virus infection among hemodialysis patients referred to Iranian Army Hospitals in Tehran during 2012-2013. Hepat Mon. 2015;15:e18322. doi: 10.5812/hepatmon.18322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mobaien AR, Mohammadi R, Sorouri R, Sadeghi K. Hepatitis E virus seroprevalence in haemodialysis patients in Zanjan Province, Islamic Republic of Iran. East Mediterr Health J. 2013;19:608–12. [PubMed] [Google Scholar]
- 50.Ramezani A, Banifazl M, Eslamifar A, Aghakhani A. Serological pattern of anti-HBc alone infers occult hepatitis B virus infection in high-risk individuals in Iran. J Infect Dev Ctries. 2010;4:658–61. doi: 10.3855/jidc.728. [DOI] [PubMed] [Google Scholar]
- 51.Mohammad Hassan KA, Mir-Davood O. Evaluation of diagnostic value of Elisa method (EIA) and PCR in diagnosis of hepatitis C virus in hemodialysis patients. Hepat Mon. 2006;6:19–23. [Google Scholar]
- 52.Somi MH, Keivani H, Ardalan MR, Farhang S, Pouri AA. Hepatitis C virus genotypes in patients with end-stage renal disease in East Azerbaijan, Iran. Saudi J Kidney Dis Transpl. 2008;19:461–5. [PubMed] [Google Scholar]
- 53.Taremi M, Khoshbaten M, Gachkar L, EhsaniArdakani M, Zali M. Hepatitis E virus infection in hemodialysis patients: A seroepidemiological survey in Iran. BMC Infect Dis. 2005;5:36. doi: 10.1186/1471-2334-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Azadegan-Ghomi H, Samak H, Forooghi S, Sahami M, Bitarafan M, editors. Tehran: The 3rd Iranian Congress of Virology; 2007. Prevalence of Hepatitis B, C, HIV in Patients Under Dialysis in Ghom 1383. [Google Scholar]
- 55.Makhloogh A, Mahdavi M, Haghshenas M, Ghasemian R, Jamshidi M. Hepatitis C prevalence in hemodialysis patients in Mazandaran, Iran: A survey by polymerase chain reaction and serological methods. Res J Biol Sci. 2008;3:265–8. [PubMed] [Google Scholar]
- 56.Mohamadalizadeh A, Ranjbar M, Seyf AS. The frequency of hepatitis in dialyse patients in Hamadan Ekbatan Hospital. Iran J Infect Dis Trop Med. 2002;7:27–34. [Google Scholar]
- 57.Toosi MN, Larti F, Rasteh M, Foroutan H, Salarieh N, Lessan-Pezeshki M, et al. Risk factors and seroprevalence of hepatitis B and C infections among hemodialysis patients in Tehran. Iran J Pathol. 2007;2:181–6. [Google Scholar]
- 58.Bozorghi SH, Ramezany YH, Vahid T, Mostajeri A, Karegharfard H, Rezayi M, et al. Assessment of prevalence and risk factors of hepatitis C virus infection in haemodialysis patients in Ghazvin. Sci J Iran Blood Transfus Organ. 2006;2:331–7. [Google Scholar]
- 59.Shad Afzar M. Qazvin: Qazvin University of Medical Sciences and Health Services; 2007. Prevalence and Incidence of Hepatitis C in Hemodialysis Patients in Bo-Ali Medical Center in Qazvin in 2003-2004. [Google Scholar]
- 60.Babaei M. Tehran, Iran: 4th Iranian International Congress of Gastroenterology & Hepatology and 2nd Congress of From Bed to Bench in Gastroenterology & Liver Disease; 2004. Comparison of Prevalence of Hepatitis C Virus (HCV) Infection among Injection Drug Users (Idus) with Other High Risk Groups: A Case-Control Study of Blood Donors. [Google Scholar]
- 61.Samimirad K, Shahbaz B, Noroozi M, Mahmoodi M. Prevalence of hepatitis C virus antibody and related risk factors among hemodialysis patients in Markazi Province. J Arak Univ Med Sci. 2006;9:23–33. [Google Scholar]
- 62.New York: World Health Organizztion; 2015. World Health Organizztion. Hepatitis B Fact Sheet. [Google Scholar]
- 63.Kishi Y, Sugawara Y, Tamura S, Kaneko J, Matsui Y, Makuuchi M, et al. New-onset diabetes mellitus after living donor liver transplantation: Possible association with hepatitis C. Transplant Proc. 2006;38:2989–92. doi: 10.1016/j.transproceed.2006.08.112. [DOI] [PubMed] [Google Scholar]
- 64.Quiroga JA, Llorente S, Castillo I, Rodríguez-Iñigo E, Pardo M, Carreño V, et al. Cellular immune responses associated with occult hepatitis C virus infection of the liver. J Virol. 2006;80:10972–9. doi: 10.1128/JVI.00852-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nobakht-Haghighi AZ, Nouroozi A. Hepatitis C antibody and related risk factors in hemodialysis patients in Iran. J Am Soc Nephrol. 2001;12:233A. [Google Scholar]
- 66.Rais-Jalali G, Khajehdehi P. Anti-HCV seropositivity among haemodialysis patients of iranian origin. Nephrol Dial Transplant. 1999;14:2055–6. doi: 10.1093/ndt/14.8.2055. [DOI] [PubMed] [Google Scholar]
- 67.Rezvan HA, Farhadi M. A preliminary study on the prevalence of anti HCV amongst healthy blood donors in Iran. Vox Sang. 1994;67:100. [Google Scholar]
- 68.Taherkhani R, Farshadpour F. Epidemiology of hepatitis C virus in Iran. World J Gastroenterol. 2015;21:10790. doi: 10.3748/wjg.v21.i38.10790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Harmankaya O, Cetin B, Obek A, Seber E. Low prevalence of hepatitis C virus infection in hemodialysis units: Effect of isolation? Ren Fail. 2002;24:639–44. doi: 10.1081/jdi-120013968. [DOI] [PubMed] [Google Scholar]
- 70.Perumal AR, Nair S, Anitha P, Illangovan V, Kanungo R. Seroprevalence of hepatitis B and C in patients on hemodialysis and their antibody response to hepatitis B vaccination. J Curr Res Sci Med. 2016;2:20–3. [Google Scholar]
- 71.Reddy GA, Dakshinamurthy KV, Neelaprasad P, Gangadhar T, Lakshmi V. Prevalence of HBV and HCV dual infection in patients on haemodialysis. Indian J Med Microbiol. 2005;23:41–3. doi: 10.4103/0255-0857.13872. [DOI] [PubMed] [Google Scholar]
- 72.Ocak S, Duran N, Kaya H, Emir I. Seroprevalence of hepatitis C in patients with type 2 diabetes mellitus and non-diabetic on haemodialysis. Int J Clin Pract. 2006;60:670–4. doi: 10.1111/j.1368-5031.2006.00738.x. [DOI] [PubMed] [Google Scholar]
- 73.Johnson DW, Dent H, Yao Q, Tranaeus A, Huang CC, Han DS, et al. Frequencies of hepatitis B and C infections among haemodialysis and peritoneal dialysis patients in Asia-Pacific countries: Analysis of registry data. Nephrol Dial Transplant. 2009;24:1598–603. doi: 10.1093/ndt/gfn684. [DOI] [PubMed] [Google Scholar]
- 74.Alavian SM. A shield against a monster: Hepatitis C in hemodialysis patients. World J Gastroenterol. 2009;15:641–6. doi: 10.3748/wjg.15.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shoukri M, Al-Sebayel M, Abaalkhail F, Elbeshbeshy H, Abdelfatah M, Al-Hamoudi W, et al. Regional and temporal variations in the prevalence of HCV among hemodialysis patients in Saudi Arabia. Epidemiology. 2016;6:2. [Google Scholar]
- 76.Karkar A. Hepatitis C in dialysis units: The saudi experience. Hemodial Int. 2007;11:354–67. doi: 10.1111/j.1542-4758.2007.00192.x. [DOI] [PubMed] [Google Scholar]
- 77.Mbaeyi C, Thompson ND. Hepatitis C virus screening and management of seroconversions in hemodialysis facilities. Semin Dial. 2013;26:439–46. doi: 10.1111/sdi.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Khodabandehloo M, Roshani D, Sayehmiri K. Prevalence and trend of hepatitis C virus infection among blood donors in Iran: A systematic review and meta-analysis. J Res Med Sci. 2013;18:674–82. [PMC free article] [PubMed] [Google Scholar]
- 79.Merat S, Rezvan H, Nouraie M, Jafari E, Abolghasemi H, Radmard AR, et al. Seroprevalence of hepatitis C virus: The first population-based study from Iran. Int J Infect Dis. 2010;14(Suppl 3):e113–6. doi: 10.1016/j.ijid.2009.11.032. [DOI] [PubMed] [Google Scholar]
- 80.Sun J, Yu R, Zhu B, Wu J, Larsen S, Zhao W, et al. Hepatitis C infection and related factors in hemodialysis patients in China: Systematic review and meta-analysis. Ren Fail. 2009;31:610–20. doi: 10.1080/08860220903003446. [DOI] [PubMed] [Google Scholar]
- 81.Fattahi MR, Safarpour A, Sepehrimanesh M, Hosseini Asl SM, Mohamaddoust F. The prevalence of hepatitis C virus infection and its related risk factors among the rural population of Fars Province, Southern Iran. Hepat Mon. 2015;15:e24734. doi: 10.5812/hepatmon.24734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bhaumik P, Debnath K. Prevalence of hepatitis B and C among hemodialysis patients of Tripura, India. BMC Infect Dis. 2016;16:1359–8. [Google Scholar]