Abstract
Introduction:
Dentin hypersensitivity (DH) is a sudden short sharp pain best explained by hydrodynamic theory. Several agents are available throughout the market that can treat DH either by blocking the nerves that helps in conducting pain or by blocking the open dentinal tubules. The aim of the present study was to compare the tubule occluding efficacy of four different desensitizing dentifrices under scanning electron microscope (SEM).
Materials and Methods:
Sixty-two dentin blocks measuring 5 mm × 5 mm × 3 mm were obtained from extracted human molar teeth and were randomly divided into five groups: Group 1 – no treatment (control, n = 2); Group 2 – Pepsodent Pro-sensitive relief and repair (n = 15); Group 3 – Sensodyne repair and protect (n = 15); Group 4 – Remin Pro (n = 15); Group 5 – Test toothpaste containing 15% nano-hydroxyapatite (n-HA) crystals (n = 15). The specimens were brushed for 2 min/day for 14 days and stored in artificial saliva. After final brushing, specimens were gold sputtered and viewed under SEM at ×2000 magnification. Results obtained were statistically analyzed using nonparametric Kruskal–Wallis test and least significant difference post hoc test.
Results:
All test groups showed significant increase in dentin tubule occlusion as compared to control group. The highest percentage of tubules occluded was shown by Group 4 and Group 5 which was significantly different from other groups (P ≤ 0.05), and there was no significant difference in tubule occlusion among them.
Conclusion:
Newer desensitizing dentifrices containing 15% n-HA and Remin Pro can provide effective tubule occlusion and thereby reduce the pain and discomfort caused by DH.
Key words: Dentine hypersensitivity, desensitizing toothpaste, nano-hydroxyapatite, scanning electron microscopy, tubule occlusion
INTRODUCTION
In dentistry, there are various reasons that are capable of causing unbearable and agonizing pain and one such major cause of pain and discomfort is dentin hypersensitivity (DH). DH has been defined as a sharp, sudden, painful reaction when the teeth are exposed to hot, cold, chemical, mechanical, touch, or osmotic (sweet or salt) stimuli and cannot be attributed to any other form of dental pathology or defect.[1]
The occurrence rate of DH usually ranges from 4% to 74%.[2,3,4] Although the age of the patients suffering from DH varies from 20 to 70 years, the peak incidence usually occurs in individuals between 20 and 40 years of age.[5] It has been reported that there is a slightly higher occurrence of DH in females than males.[3]
The buccal cervical area of teeth suffers most commonly from DH.[6] Teeth that are most commonly affected in decreasing order are canines, premolars, incisors, and molars.[7]
DH generally develops in two phases: lesion localization and lesion initiation.[8] Etiological factors include faulty tooth brushing, poor oral hygiene, premature contacts, gingival recession due to periodontal therapy, and exogenous/endogenous nonbacterial acids,[8] dietary habits, and low pH mouth rinses.[9] The triggering factor may be a thermal origin, evaporative, tactile, and/or osmotic.[10]
A wide variety of products are available that can be used to relieve the pain and discomfort caused by DH. These products basically fall into two categories based on their mode of action. First one is nerve desensitizing agents which consist of potassium salts. Other available products act by plugging the open dentinal tubules. Toothpaste containing 15% nano-hydroxyapatite (n-HA) was found to be most effective in reduction of DH after a single application up to a period of 4 weeks.[11] In spite of the availability of wide variety of treatment procedures, there is no single method available that has proved to be potent in eliminating DH completely and providing patients with complete relief.
The objective of this study was to compare the effectiveness of dentinal tubule occlusion of four different dentifrices under scanning electron microscope (SEM). The null hypothesis generated was that the distribution of the percentage of tubules occluded is the same across all dentifrices.
MATERIALS AND METHODS
Sixty-two human molars extracted for periodontal reasons were collected. Any remaining soft tissue remnants and calculus were cleaned and were stored in 10% formalin at room temperature before further use. The teeth were sectioned using diamond disc to create dentin specimens measuring 5 mm × 5 mm × 3 mm. The prepared discs were then mounted on acrylic block.
The mounted dentin specimens were then randomly divided into five groups:
Group 1: No treatment (control, n = 2)
Group 2: Samples treated with Pepsodent Pro-sensitive relief and repair (n = 15)
Group 3: Samples treated with Sensodyne repair and protect (n = 15)
Group 4: Samples treated with Remin Pro (n = 15)
Group 5: Samples treated with 15% n-HA containing test toothpaste (n = 15).
The specimens from all groups were smoothened with 1200 grit silicon carbide polishing paper (Metatech Ind., Pune, Maharashtra, India) followed by removal of smear layer by immersing in 17% ethylenediaminetetraacetic acid (Neelkanth Healthcare Pvt., Ltd., Jodhpur, Rajasthan, India) for 2 min, thoroughly rinsed thereafter, and stored in artificial saliva (ICPA Health Products Ltd., Ankleshwar, Gujarat, India). For Group 2, 3, 4, and 5, the specimens were then placed onto a customized jig prepared for holding the power toothbrush and samples prepared to standardize the pressure during brushing of the specimens.
A pea-sized amount of the assigned dentifrice was placed onto the dentin surface. The brush bristles were at 90° angulation to the specimen and remained in contact with the dentin surface. The brushing duration was for 2 min (measured by stopwatch) each day for 14 days. Separate toothbrush head was used for each group. After brushing, the specimens were washed and stored in artificial saliva.
Scanning electron microscope analysis
After the last brushing session, the samples were thoroughly washed in distilled water, dried, and sputter coated with a thin layer of gold in the sputter coating machine (Q150R ES, GS Quorum Technologies Limited, England) and photomicrographs were taken using SEM (Merlin Compact, Carl Zeiss) at ×2000 magnification and 5 kV.
Statistical analysis
Percentage of occluded tubules was obtained by dividing the total number of occluded tubules by total number of tubules in the photomicrograph [Figure 1]. This result was then multiplied by 100 to obtain the percentage of occluded tubules for each photomicrograph. Results were statistically analyzed using nonparametric Kruskal–Wallis test and least significant difference post hoc test in SPSS software version 21 (SPSS, Chicago, IL, USA). The level of statistical significance was set at 0.05.
Figure 1.
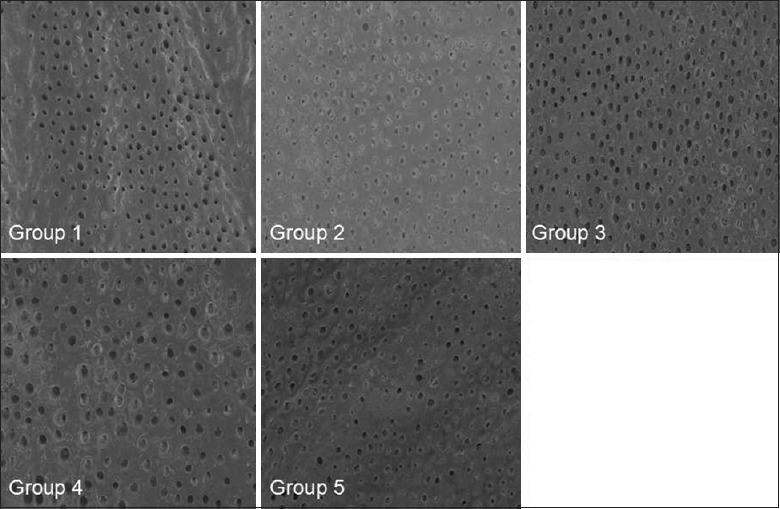
Scanning electron microscope photomicrograph (×2000) for all groups
RESULTS
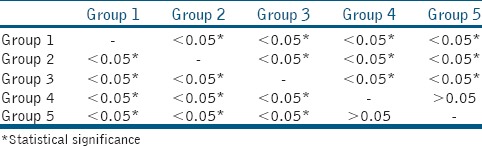
All test groups showed significantly more tubule occlusion as compared to control group as given in Table 1. Statistical analysis did not reveal any significant difference in the percentage of tubule occlusion by Remin Pro and 15% n-HA groups [Table 2].
Table 1.
Mean percentage of tubules occluded
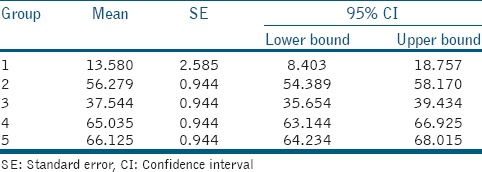
Table 2.
Intergroup comparison between desensitizing toothpastes and dentin tubule occlusion for all groups (P)
DISCUSSION
The present study investigated the efficacy of dentin tubule occlusion of four different dentifrices containing potassium salts, bioactive glass, combination of fluoride, hydroxyapaptite and xylitol and 15% n-HA crystals. Test toothpaste was prepared using the n-HA material (nanoXIM®, Fluidinova Technologies, Moreira de Maia, Portugal) into a nonaqueous dentifrice without fluoride containing 15% by weight of the n-HA. The product contains under 50 nm-sized nanoparticles and with a high specific surface area. NanoXIM•CarePaste is naturally preserved and complies with dentifrices and food-grade standards.[12]
Pepsodent Pro-sensitive relief and repair (Hindustan Unilever Limited, India) contains potassium citrate as an active ingredient along with hydroxyapatite, zinc citrate, and fluoride. Potassium ions released from toothpastes diffuse along the dentinal tubules to inactivate intradental nerves and act by blocking synapses between nerve cells, thereby reducing nerve excitation and the associated pain.[13,14] When applied in vivo to the exposed dentin of human, potassium ions produced a temporary block of impulse conduction in sensory nerve endings in the dentin or pulp.[15] This group showed significantly higher tubule occlusion when compared with Group 3.
NovaMin (bioactive glass) is an inorganic amorphous calcium sodium phosphosilicate (CSPS) material containing 45% SiO2, 24.5% Na2O, 24.5% CaO, and 6% P2O5.[16] Sensodyne repair and protect (Glaxo SmithKline, India) is NovaMin (5%) containing desensitizing dentifrices. CSPS in NovaMin has a strong attraction to collagen[17] as well as physically occludes dentin tubules. Initial reactivity of the NovaMin particles is associated with the development of a surface negative charge which facilitates binding to side groups on Type I collagen fibers.[18] NovaMin can quickly occlude dentin tubules to form a protective layer on the dentin surface.[19] One possible limitation is that the apatite formation and blocking of the dentine tubules may take several weeks.[20] In this study also, this group showed the least percentage of tubule occlusion among all the test groups.
Remin Pro (VOCO GmbH, Germany) is a water-based desensitizing paste. In our study, mean percentage of tubule occlusion in this group was 65.04%. Superior quantity of dentinal tubule occlusion can be attributed to its contents, i.e., sodium fluoride (1450 ppm), hydroxyapatite, and xylitol, thus making it effective against demineralization and erosion. On the tooth surface, fluoride is converted to fluorapatite when it comes in contact with saliva. Once the fluorapatite layer is formed, the tooth surface becomes more resistant to acid attacks. The hydroxyapatite contained in Remin Pro fills superficial enamel lesions and the tiniest irregularities that arise from erosion. Cariostatic properties of xylitol prevent it from being converted into harmful lactic acid by cariogenic bacteria thus allowing the mouth to naturally remineralize damaged teeth with less interruption.[21]
n-HA-based toothpastes were first introduced in Japan in 1980s[11] and are used in oral care formulations for effective occlusion of dentinal tubules.[22] Unlike micro-sized hydroxyapatite, the n-HA can be easily integrated into the dental tubules thus enhancing their occlusion and reducing DH. n-HA also facilitates its binding to the dentin apatite and tooth enamel due to higher surface area, biological activity, and chemical reactivity.[12]
In this study, the test toothpaste group containing 15% n-HA showed the highest percentage of dentin tubule occlusion (66.13%). This is probably due to the ability of n-HA particles to self-assemble to form enamel-like structures in aqueous solution. Since the chemical composition is similar to the main structure of enamel, it forms a protective new layer over tooth enamel having a thickness of 1–2 μm covering the open pores of tubules[23] and effectively reduces DH even after single application.[11] Results of this study are comparable to earlier studies which showed that the toothpastes containing n-HA crystals occluded 75% more dental tubules than the regular toothpaste.[12]
CONCLUSION
Within the limitations of the current study, it can be concluded that:
All the experimental dentifrices used showed significantly higher percentage of dentinal tubule occlusion when compared to the control group
Among the dentifrices, Remin Pro and test toothpaste containing 15% n-HA proved to be the most effective with a mean tubule occlusion of 65.04% and 66.13%, respectively, followed by Pepsodent Pro-sensitive relief and repair (56.28%) and Sensodyne repair and protect (37.54%)
The findings of the present study encourage the application n-HA dentifrices as an effective desensitizing agent due to its low cost, ease of use, and home application.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Mr. Paulo Quadros, Head of Product and Business Development, Fluidinova, SA, Portugal, for providing us the 15% n-HA paste.
REFERENCES
- 1.Holland GR, Narhi MN, Addy M, Gangarosa L, Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J Clin Periodontol. 1997;24:808–13. doi: 10.1111/j.1600-051x.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 2.Rees JS, Jin LJ, Lam S, Kudanowska I, Vowles R. The prevalence of dentine hypersensitivity in a hospital clinic population in Hong Kong. J Dent. 2003;31:453–61. doi: 10.1016/s0300-5712(03)00092-7. [DOI] [PubMed] [Google Scholar]
- 3.Fischer C, Fischer RG, Wennberg A. Prevalence and distribution of cervical dentine hypersensitivity in a population in Rio de Janeiro, Brazil. J Dent. 1992;20:272–6. doi: 10.1016/0300-5712(92)90043-c. [DOI] [PubMed] [Google Scholar]
- 4.Taani DQ, Awartani F. Prevalence and distribution of dentin hypersensitivity and plaque in a dental hospital population. Quintessence Int. 2001;32:372–6. [PubMed] [Google Scholar]
- 5.Flynn J, Galloway R, Orchardson R. The incidence of 'hypersensitive' teeth in the West of Scotland. J Dent. 1985;13:230–6. doi: 10.1016/0300-5712(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 6.Addy M, Mostafa P, Newcombe RG. Dentine hypersensitivity: The distribution of recession, sensitivity and plaque. J Dent. 1987;15:242–8. doi: 10.1016/0300-5712(87)90045-5. [DOI] [PubMed] [Google Scholar]
- 7.Orchardson R, Collins WJ. Clinical features of hypersensitive teeth. Br Dent J. 1987;162:253–6. doi: 10.1038/sj.bdj.4806096. [DOI] [PubMed] [Google Scholar]
- 8.Orchardson R, Gillam DG. Managing dentin hypersensitivity. J Am Dent Assoc. 2006;137:990–8. doi: 10.14219/jada.archive.2006.0321. [DOI] [PubMed] [Google Scholar]
- 9.Bartold PM. Dentinal hypersensitivity: A review. Aust Dent J. 2006;51:212–8. [PubMed] [Google Scholar]
- 10.Kleinberg I, Kaufman HW, Wolff M. Measurement of tooth hypersensitivity and oral factors involved in its development. Arch Oral Biol. 1994;39(Suppl):63S–71S. doi: 10.1016/0003-9969(94)90190-2. [DOI] [PubMed] [Google Scholar]
- 11.Jena A, Shashirekha G. Comparison of efficacy of three different desensitizing agents for in-office relief of dentin hypersensitivity: A 4 weeks clinical study. J Conserv Dent. 2015;18:389–93. doi: 10.4103/0972-0707.164052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.nanoxim CarePaste Reduces Dental Hypersensitivity and Promotes Enamel Remineralization. [Last accessed on 2017 Jan 05]. Available from: http://www.news-medical.net/whitepaper/20140508/nanoXIMe280a2 CarePaste-Reduces-Dental-Hypersensitivity-and-Promotes-Enamel-Remineralization.aspx .
- 13.Peacock JM, Orchardson R. Effects of potassium ions on action potential conduction in A- and C-fibers of rat spinal nerves. J Dent Res. 1995;74:634–41. doi: 10.1177/00220345950740020301. [DOI] [PubMed] [Google Scholar]
- 14.Markowitz K, Bilotto G, Kim S. Decreasing intradental nerve activity in the cat with potassium and divalent cations. Arch Oral Biol. 1991;36:1–7. doi: 10.1016/0003-9969(91)90047-x. [DOI] [PubMed] [Google Scholar]
- 15.Ajcharanukul O, Kraivaphan P, Wanachantararak S, Vongsavan N, Matthews B. Effects of potassium ions on dentine sensitivity in man. Arch Oral Biol. 2007;52:632–9. doi: 10.1016/j.archoralbio.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Kobayashi M, Saito H, Mase T, Sasaki T, Wang W, Tanaka Y, et al. Polarization of hybridized calcium phosphoaluminosilicates with 45S5-type bioglasses. Biomed Mater. 2010;5:25001. doi: 10.1088/1748-6041/5/2/025001. [DOI] [PubMed] [Google Scholar]
- 17.Oréfice R, Hench L, Brennan A. Evaluation of the interactions between collagen and the surface of a bioactive glass during in vitro test. J Biomed Mater Res A. 2009;90:114–20. doi: 10.1002/jbm.a.32080. [DOI] [PubMed] [Google Scholar]
- 18.Layer TM. Development of a fluoridated, daily-use toothpaste containing novaMin technology for the treatment of dentin hypersensitivity. J Clin Dent. 2011;22:59–61. [PubMed] [Google Scholar]
- 19.Litkowski LJ, Hack GD, Sheaffer HB, Greenspan DC. Occlusion of dentin tubules by 45S5 bioglass®. Bioceramics. 1997;10:411–4. [Google Scholar]
- 20.Kumar A, Singh S, Thumar G, Mengji A. Bioactive glass nanoparticles (NovaMin®) for applications in dentistry. J Dent Med Sci. 2015;14:30–5. [Google Scholar]
- 21.Blaes J. Tooth Protection, Freedom, Whitening, and Better Gums. Dental Economics. PennWell Corporation. 2011. [Last accessed on 2017 Jan 25]. Available from: http://www.dentaleconomics.com/articles/print/volume-101/issue-11/practice/tooth-protection-freedom-whitening-and-better-gumshtml .
- 22.Kunam D, Manimaran S, Sampath V, Sekar M. Evaluation of dentinal tubule occlusion and depth of penetration of nano-hydroxyapatite derived from chicken eggshell powder with and without addition of sodium fluoride: An in vitro study. J Conserv Dent. 2016;19:239–44. doi: 10.4103/0972-0707.181940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amin M, Mehta R, Duseja S, Desai K. Evaluation of the efficacy of commercially available nano-hydroxyapatite paste as a desensitizing agent. Adv Hum Biol. 2015;5:34–8. [Google Scholar]


