Abstract
Background
It was reported that egg white protein (EWP) reduced body fat in rats. We developed a lactic-fermented egg white (LE) that facilitates the consumption of egg whites by fermenting them with lactobacillus, and were able to study their intake in humans. In this double-blind, placebo-controlled design, we evaluated the effect of LE on visceral fat area (VFA).
Methods
Participants included 37 adult males and females aged ≥40 years (VFA at navel ≥100 cm2). They were divided into two groups: the control group and the LE group. The control and LE groups consumed drinks containing whey and LE, respectively, for 12 weeks (providing 8 g protein/day). VFA was measured at baseline and at week 12 of intake. Abdominal girth was measured at baseline and at weeks 6 and 12.
Results
LE intake decreased VFA significantly compared with baseline (−8.89 cm2, p < 0.05), and VFA was significantly lower than that in the control group (+1.71 cm2, p < 0.05). The LE group showed significant improvement in the ratio of visceral to subcutaneous fat area compared with baseline and the control group (p < 0.05).
Conclusions
The results demonstrated that LE reduces VFA and improves the ratio of visceral to subcutaneous fat area. As other measurement items were not influenced, we concluded that LE improves visceral fat obesity.
Trial registration
This clinical trial was retrospectively registered with the University hospital Medical Information Network (UMIN) Center, (UMIN000026949; registered on 11/04/2017; http://www.umin.ac.jp/).
Keywords: Egg white, Visceral fat, Obesity, Japanese, Protein
Background
Visceral fat obesity causes complications such as dyslipidaemia, abnormal glucose tolerance, and hypertension. Along with serum LDL-cholesterol concentration, it is a risk factor for arteriosclerotic disease [1]. In Japan, approximately 50% men and 20% women ≥40 years have metabolic syndrome or pre-metabolic syndrome, which is becoming more serious [2].
Hen eggs contain almost all essential nutrients (except vitamin C and dietary fiber), and are known to be of high nutritive value [3]. Attention has been drawn to the cholesterol contained in eggs, and nutritional education for dyslipidaemia recommends avoiding egg consumption. Although the cholesterol in eggs is found in the yolk, some reports have indicated that consumption of egg yolk does not increase blood cholesterol levels [4–6] or mortality due to coronary heart disease [7]. Therefore, we considered whether the constituent that improves lipid metabolism is contained in eggs, specifically egg white protein (EWP). EWP is high in protein and low in fat and has been reported to reduce serum total and LDL cholesterol levels [8–10].
EWP is said to lower blood cholesterol by inhibiting cholesterol absorption in the small intestines. However, in doing so, triglyceride absorption is also inhibited [11]. Therefore, EWP not only reduces serum LDL cholesterol level but is also believed to prevent arteriosclerotic disease by reducing visceral fat.
In an experiment on rats, Matsuoka et al. reported that egg white proteins could reduce body and abdominal fat [12]. However, it is unclear whether the reduction was effective in human.
The consumption of egg white itself poses a problem in terms of taste and physical properties. We therefore developed a lactic-fermented egg white (LE) that facilitates the consumption of egg whites by fermenting them with lactobacillus, and were able to study their intake in humans [13, 14]. In a previous study, it was reported that the EWPs ovalbumin and ovotransferrin could inhibit lipid absorption [11]. It has been reported that beta-conglycinin, a soy protein, reduced visceral fat at the speed of 5 g/day [15]. Ovalbumin and ovotransferrin are reported to contain 54% and 11% EWP, respectively [16]. If we suppose that ovalbumin and ovotransferrin have the same visceral fat-reducing effect as beta-conglycinin at a daily intake of 5 g, a daily intake of 8 g of EWP would be required. We therefore conducted a double-blind, placebo-controlled study to evaluate the visceral fat-reducing effect of protein in Japanese adults with visceral fat obesity, via daily intake of LE for 12 weeks.
Methods
Test foods
The control drink and the drink containing LE were prepared by Co-op Foods Co., Ltd. (Tokyo, Japan). Flavors, sweeteners and water were added to the whey (Nippon-Shinyaku Co., Ltd., Kyoto, Japan) and LE [13] (Kewpie Egg Corporation, Tokyo, Japan) of each drink. Once homogeneously dispersed, the preparation was heat-sterilized. Measurement using the Kjeldahl method [17] indicated that both drinks contained 8 g of protein per 180 g serving. Ovalbumin content in LE was assessed by the sandwich ELISA procedure using anti-chicken ovalbumin polyclonal antibody, and horseradish peroxidase-labeled anti-chicken ovalbumin polyclonal antibody, respectively. A commercial kit, Egg (Ovalbumin) ELISA kit II (Morinaga Institute of Biological Science Inc., Yokohama, Japan) was used with absorbance detected at 450 nm by a multi-detection microplate reader (Powerscan® HT, DS Pharma Biomedical Co. Ltd., Osaka, Japan). Ovalbumin content of the LE drink was 4.17 g/180 g, as measured via sandwich ELISA. Based on a previous report that ovotransferrin accounts for 11% of total EWP [17], the content of ovotransferrin was calculated to be 0.88 g/180 g LE (Calculated value).
Participants and test methods
Recruitment was done per the following process: Japanese subjects with body mass index (BMI) (≥25), aged more than 40 years (male) or postmenopausal female, who were not undergoing treatment for hyperlipidemia or diabetes, who had no subjective symptoms of gout and who were capable of filling out the required forms, such as self-diagnosis forms, and of visiting a designated institution as scheduled. The exclusion criteria were as follows: taking drugs that could potentially affect the test results (e.g., anti-hyperlipidemic agents, anti-diabetic agents, oral corticosteroid formulations, and antihypertensive agents); regular consumption of foods for specified health uses that could potentially affect test results; excessive alcohol consumption; suspected allergic reactions (particularly to egg and milk); participation in other clinical studies; a history of serious liver damage, kidney damage, or myocardial infarction; a history of, or current, hepatitis; and serious anemia. In this study, 80 adults were screened and 48 individuals with visceral fat area (VFA) (≥100 cm2) were included as test subjects.
The study followed a double-blind, parallel-arm design. Participants were divided into two groups: a control group and LE group. The control group was given a drink containing whey (8 g of protein), and the LE group was given a drink containing LE (8 g of protein) every day at breakfast for 12 continuous weeks.
At 0 and 12 weeks of intake, computed tomographic (CT) scanning of the abdomen (Aquilion™, Toshiba Medical Systems Corporation, Tochigi, Japan) was performed, and VFA was measured at the navel (Fat Scan, East Japan Institute of Technology Co., Ltd., Ibaraki, Japan). CT scans were conducted at the Nakajima Clinic (Tokyo, Japan). At weeks 0, 6, and 12, bodyweight, blood pressure, and abdominal girth, respectively, were measured after fasting overnight. Blood was sampled from a forearm vein, and blood tests were performed at baseline, and weeks 6 and 12 of intake.
Blood tests
Peripheral blood test was performed using flow cytometry. Serum analysis included the following items: total cholesterol (enzyme method); HDL cholesterol (direct method); triglyceride (enzyme method); free fatty acid (FFA; enzyme method); phospholipid (enzyme method); glucose (hexokinase UV test); HbA1c (latex coagulating method); RLP cholesterol (immunoadsorption); insulin (CLEIA method); AST (JSCC transferable method); ALT (JSCC transferable method); gamma-GTP (JSCC transferable method); blood urea nitrogen (BUN; urease LED UV method); creatinine (enzyme method); and uric acid (enzyme method). LDL cholesterol concentration was calculated using the Friedewald formula [18]. Blood tests were performed by SRL Corporation (Tokyo, Japan).
Dietary intake
The nutritional value of the content of meals recorded by participants over a three-day period was calculated using Excel Eiyoukun Food Frequency Questionnaire version 5 (Kenpakusha, Tokyo, Japan). The 2010 Standard Table of Food Composition in Japan database was used in this nutrition-calculation software.
Statistical analysis
Test results are shown as mean ± standard error. Comparisons with baseline values were performed using paired t-tests for VFA and Dunnett’s test for all other items. Comparisons with the control group were performed using the student’s t-test. A significance level of less than 5% was considered substantial. Statistical analyses were performed using SPSS version 20 (SPSS Inc., Tokyo, Japan). Change in VFA is indicated by ∆ cm2.
Results
Adherence and participant attributes
During the study period, two participants withdrew from the study; one individual in the control group could not get accustomed to the taste of the test food and one individual in the LE group experienced melena. The latter’s condition was assumed to be due to the participant’s tendency toward constipation and the melena was thus determined to not be causally related to the test food (Fig. 1).
Fig. 1.
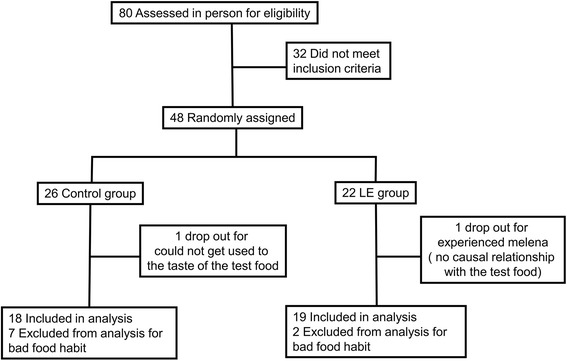
Participant flow through a randomized trial
From the control group, seven participants were excluded: two of whom did not fast prior to blood sampling; four who did not complete the food diary sufficiently to track actual food intake; and one who was inconsistent in the timing of test food consumption. From the LE group, two participants were excluded: one who did not fast prior to blood sampling and one who completed the food diary insufficiently (Fig.1). From the above, we analyzed 18 individuals in the control group and 19 in the LE group. There were no significant differences observed at baseline between the two groups in terms of age, height, or BMI (p > 0.05, Table 1).
Table 1.
Background of subjects
| Control | LE | |||||
|---|---|---|---|---|---|---|
| Age (y) | 55.2 | ± | 1.5 | 56.6 | ± | 1.2 |
| Height (cm) | 166 | ± | 3 | 167 | ± | 2 |
| Body weight (kg) | 76.1 | ± | 2.5 | 78.4 | ± | 2.2 |
| BMI | 27.5 | ± | 0.7 | 28.0 | ± | 0.7 |
| Systolic blood presure (mmHg) | 131 | ± | 5 | 135 | ± | 4 |
| Diastolic blood pressure (mmHg) | 80.1 | ± | 3.1 | 87.1 | ± | 2.5 |
Mean ± SE of 18 (control) and 19 (LE)
Control Control group, LE Lactic fermented egg white group
Dietary intake
There was no significant change in the amount of food consumed during the study period in either group (Table 2).
Table 2.
Dietary intake of subjects
| Intake Period (Weeks) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 | 12 | ||||||||
| Energy (kcal) | Control | 1956 | ± | 109 | 2073 | ± | 163 | 1976 | ± | 112 |
| LE | 2163 | ± | 175 | 1978 | ± | 93 | 2012 | ± | 77 | |
| Protein (g) | Control | 71.9 | ± | 5.3 | 75.1 | ± | 5.2 | 73.4 | ± | 5.0 |
| LE | 80.1 | ± | 6.9 | 73.0 | ± | 3.3 | 74.2 | ± | 3.3 | |
| Lipids (g) | Control | 64.9 | ± | 4.9 | 68.6 | ± | 7.2 | 68.0 | ± | 4.6 |
| LE | 68.7 | ± | 8.5 | 61.0 | ± | 4.2 | 66.8 | ± | 5.2 | |
| Carbohydrate (g) | Control | 251 | ± | 15 | 266 | ± | 21 | 250 | ± | 15 |
| LE | 276 | ± | 20 | 244 | ± | 13 | 251 | ± | 11 | |
| Cholesterol (mg) | Control | 388 | ± | 47 | 396 | ± | 42 | 391 | ± | 37 |
| LE | 330 | ± | 33 | 335 | ± | 27 | 351 | ± | 36 | |
| Dietary fiber (g) | Control | 11.5 | ± | 0.9 | 12.4 | ± | 1.1 | 11.8 | ± | 0.9 |
| LE | 13.6 | ± | 1.3 | 12.1 | ± | 1.3 | 12.7 | ± | 0.8 | |
Mean ± SE of 18 (control) and 19 (LE)
Control Control group, LE Lactic fermented egg white group
Physical condition
The abdominal girth of the control group was significantly lower at 12 weeks than at baseline. No significant difference was observed for any other items between the control and LE groups, nor compared to baseline (Table 3).
Table 3.
Results of body composition at the navel level
| Intake Periods (Weeks) | |||||||
|---|---|---|---|---|---|---|---|
| 0 | 12 | ||||||
| Body weight (kg) | Control | 76.1 | ± | 2.5 | 76.0 | ± | 2.5 |
| LE | 78.4 | ± | 2.2 | 78.5 | ± | 2.2 | |
| BMI | Control | 27.5 | ± | 0.7 | 27.4 | ± | 0.7 |
| LE | 28.0 | ± | 0.7 | 28.1 | ± | 0.7 | |
| Waist (cm) | Control | 100 | ± | 2 | 99.8 | ± | 2.0a |
| LE | 99.3 | ± | 1.9 | 98.4 | ± | 2.2 | |
| Total fat area (cm2) | Control | 391 | ± | 22 | 391 | ± | 27 |
| LE | 386 | ± | 27 | 390 | ± | 28 | |
| Subcutaneous fat area (cm2) | Control | 249 | ± | 20 | 246 | ± | 24 |
| LE | 240 | ± | 24 | 254 | ± | 23a | |
| Visceral fat area (cm2) | Control | 143 | ± | 7 | 144 | ± | 8 |
| LE | 145 | ± | 9 | 136 | ± | 9a | |
| Visceral/Subcutaneous | Control | 0.766 | ± | 0.078 | 0.597 | ± | 0.052 |
| LE | 0.656 | ± | 0.048 | 0.546 | ± | 0.041* | |
Mean ± SE of 18 (control) and 19 (LE)
ap < 0.05 vs. 0 weeks by paired t-test
Control Control group, LE Lactic fermented egg white group
Fat area at the navel
There was no significant difference in the total fat area in the LE group compared to baseline or the control group (Table 3). Although no significant difference was observed between the two groups in terms of VFA and subcutaneous fat area, the LE group showed significantly less VFA, and a significant increase in subcutaneous fat area compared to baseline (p < 0.05). The control group showed no significant difference compared to baseline (Table 3).
Calculation of the visceral to subcutaneous fat ratio indicated a significantly lower ratio in the LE group compared to baseline. There was no significant difference in the control group compared to baseline or between the two groups (Table 3).
Calculation of the change in VFA revealed a significant reduction in the LE group compared to both baseline and the control group. With regards to the change in visceral to subcutaneous fat ratio at the navel (∆), the value was significantly reduced by the intake of LE compared to the control group and baseline ratio (Fig. 2 and Fig. 3).
Fig. 2.
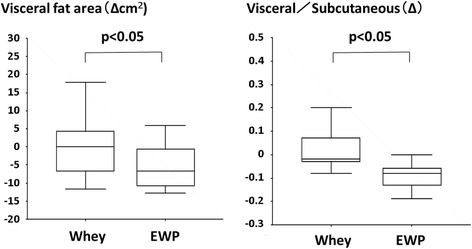
Change in visceral fat area and ratio of visceral to subcutaneous fat area of the subjects fed LE or whey for 12 weeks. Δ: 12 weeks–0 weeks. Mean ± SE of 18 (control) and 19 (LE), *: p < 0.05 vs. 0 weeks by paired t-test
Fig. 3.
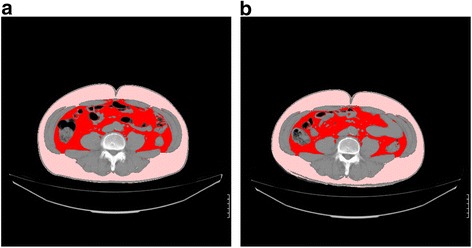
A photographic example of the change in visceral fat area (VFA) of the subjects fed LE for 12 weeks. Red: Visceral fat, Pink: Subcutaneous fat. a: Pre-intake (VFA = 119 cm2), b: Post-intake (VFA = 102 cm2)
Serum biochemical analysis
There was no significant variation observed in serum total cholesterol, LDL cholesterol, RLP cholesterol, triglycerides, phospholipids, insulin, or blood glucose levels. While the LE group exhibited significantly lower FFA concentrations compared to the control group in week 6 (p < 0.05), there was no significant difference observed in week 12. Moreover, while the LE group showed significantly lower HDL-cholesterol levels in week 6 compared to baseline (p < 0.05), there was no significant difference observed in week 12 (Table 4).
Table 4.
Serum biochemical analysis
| Intake Period (Weeks) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 | 12 | |||||||||
| Total Cholesterol | Control | 209 | ± | 6 | 210 | ± | 7 | 209 | ± | 8 | |
| (mg/dL) | LE | 215 | ± | 6 | 210 | ± | 6 | 217 | ± | 6 | |
| HDL-Cholesterol | Control | 55.8 | ± | 2.26 | 55.1 | ± | 2.60 | 54.8 | ± | 2.26 | |
| (mg/dL) | LE | 58.1 | ± | 2.85 | 52.4 | ± | 2.02a | 55.8 | ± | 2.51 | |
| LDL-Cholesterol | Control | 133 | ± | 4 | 131 | ± | 5 | 131 | ± | 6 | |
| (mg/dL) | LE | 132 | ± | 5 | 130 | ± | 6 | 135 | ± | 5 | |
| Triglyceride | Control | 127 | ± | 16 | 150 | ± | 25 | 123 | ± | 15 | |
| (mg/dL) | LE | 132 | ± | 18 | 150 | ± | 18 | 134 | ± | 12 | |
| NEFA | Control | 496 | ± | 31 | 553 | ± | 36 | 515 | ± | 34 | |
| (mEq/L) | LE | 481 | ± | 42 | 443 | ± | 37# | 543 | ± | 49 | |
| Phospholipid | Control | 218 | ± | 7 | 221 | ± | 8 | 215 | ± | 7 | |
| (mg/dL) | LE | 224 | ± | 6 | 221 | ± | 5 | 222 | ± | 5 | |
| Glucose | Control | 92.8 | ± | 2.0 | 91.7 | ± | 2.0 | 96.0 | ± | 3.0 | |
| (mg/dL) | LE | 92.7 | ± | 1.8 | 94.4 | ± | 2.1 | 93.6 | ± | 2.6 | |
| Insulin | Control | 6.65 | ± | 0.98 | 7.32 | ± | 0.95 | 6.93 | ± | 0.55 | |
| (mg/mL) | LE | 6.26 | ± | 0.74 | 8.35 | ± | 1.33 | 7.50 | ± | 0.82 | |
| HbA1c (NGSP) | Control | 5.53 | ± | 0.09 | 5.50 | ± | 0.08 | 5.51 | ± | 0.09 | |
| (%) | LE | 5.56 | ± | 0.08 | 5.54 | ± | 0.10 | 5.56 | ± | 0.10 | |
| RLP-Cholsterol | Control | 4.81 | ± | 0.66 | 6.25 | ± | 1.29 | 4.73 | ± | 0.49 | |
| (mg/dL) | LE | 5.58 | ± | 0.93 | 6.73 | ± | 1.21 | 5.34 | ± | 0.54 | |
Mean ± SE of 18 (control) and 19 (LE)
ap < 0.05 vs. 0 weeks by Dunnett test、#p < 0.05 vs. Control group by Student’s t-test
Control Control group, LE Lactic fermented egg white group
Hematological tests
The control group exhibited significantly high mean corpuscular volume (MCV) in week 6 compared to baseline, whereas mean corpuscular hemoglobin level (MCHC) in weeks 6 and 12 were significantly lower than baseline (p < 0.05). The LE group showed significantly higher MCV in week 6 compared to baseline (p < 0.05; Table 5). Throughout the entire study period, MCV and MCHC were significantly lower in the LE group compared to the control group (p < 0.05). All items’ values stayed within the normal range and no particular problems were observed (Table 5).
Table 5.
Results of hematological tests and hepatic and kidney function
| Intake Period (Weeks) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 | 12 | ||||||||
| WBC | Control | 5683 | ± | 334 | 6072 | ± | 382 | 5972 | ± | 327 |
| (/μL) | LE | 5779 | ± | 310 | 5758 | ± | 301 | 5579 | ± | 290 |
| RBC | Control | 473 | ± | 10 | 470 | ± | 9 | 476 | ± | 10 |
| (/μL) | LE | 488 | ± | 11 | 480 | ± | 10 | 491 | ± | 9 |
| Hb | Control | 14.7 | ± | 0.3 | 14.7 | ± | 0.3 | 14.6 | ± | 0.3 |
| (g/dL) | LE | 14.8 | ± | 0.3 | 14.7 | ± | 0.3 | 14.7 | ± | 0.3 |
| Ht | Control | 44.4 | ± | 0.9 | 44.9 | ± | 0.8 | 44.6 | ± | 0.8 |
| (%) | LE | 45.0 | ± | 0.9 | 44.8 | ± | 0.8 | 45.0 | ± | 0.7 |
| MCV | Control | 93.9 | ± | 0.6 | 95.7 | ± | 0.8a | 93.9 | ± | 0.7 |
| (fl) | LE | 92.3 | ± | 0.7 | 93.5 | ± | 0.8a | 91.8 | ± | 0.7# |
| MCH | Control | 31.1 | ± | 0.3 | 31.2 | ± | 0.3 | 30.8 | ± | 0.3 |
| (pg) | LE | 30.3 | ± | 0.3 | 30.6 | ± | 0.3a | 30.1 | ± | 0.3* |
| MCHC | Control | 33.0 | ± | 0.2 | 32.6 | ± | 0.2a | 32.8 | ± | 0.2 |
| (%) | LE | 32.8 | ± | 0.2 | 32.7 | ± | 0.2 | 32.7 | ± | 0.1 |
| Platelet | Control | 23.8 | ± | 1.4 | 23.0 | ± | 0.9 | 22.7 | ± | 0.9 |
| (/μL) | LE | 23.7 | ± | 1.3 | 22.5 | ± | 1.2 | 22.7 | ± | 1.2 |
| AST | Control | 21.9 | ± | 1.8 | 22.1 | ± | 2.0 | 24.4 | ± | 3.8 |
| (IU/L) | LE | 22.1 | ± | 1.3 | 24.7 | ± | 1.9 | 24.9 | ± | 2.3 |
| ALT | Control | 27.9 | ± | 4.2 | 27.2 | ± | 4.2 | 30.8 | ± | 7.1 |
| (IU/L) | LE | 25.0 | ± | 2.1 | 39.8 | ± | 3.2 | 28.0 | ± | 2.5 |
| γ-GTP | Control | 49.2 | ± | 12.2 | 48.0 | ± | 11.1 | 42.4 | ± | 9.1 |
| (IU/L) | LE | 42.7 | ± | 9.2 | 44.3 | ± | 8.9 | 40.6 | ± | 7.3 |
| BUN | Control | 14.6 | ± | 0.9 | 15.6 | ± | 0.7 | 14.5 | ± | 0.7 |
| (mg/dL) | LE | 13.8 | ± | 0.9 | 15.9 | ± | 0.8a | 15.2 | ± | 0.7 |
| Cr | Control | 0.737 | ± | 0.024 | 0.758 | ± | 0.025 | 0.736 | ± | 0.027 |
| (mg/dL) | LE | 0.839 | ± | 0.032# | 0.849 | ± | 0.030# | 0.853 | ± | 0.035# |
| UA | Control | 6.23 | ± | 0.28 | 6.56 | ± | 0.28 | 6.17 | ± | 0.30 |
| (mg/dL) | LE | 6.32 | ± | 0.24 | 6.49 | ± | 0.23 | 6.18 | ± | 0.24 |
Mean ± SE of 18 (control) and 19 (LE)
ap < 0.05 vs. 0 weeks by Dunnett test、#p < 0.05 vs. Control by Student’s t-test
Control Control group, LE Lactic fermented egg white group
Liver and kidney functions indices
While the LE group exhibited significantly higher BUN levels in week 6 compared to baseline (p < 0.05), BUN was within the normal range, with no significant difference observed in week 12. The LE group showed significantly lower creatinine levels than the control group at baseline and in week 12 (p < 0.05). However, there was no significant variation observed throughout the intake period, and because changes were within the normal range, this was not considered to pose any problem. For all other items, no influence of the test foods was observed (Table 5).
Discussion
Results of this study indicated that when 8 g of LE (i.e., EWP) was consumed daily for 12 weeks, VFA was significantly reduced compared to baseline and the control group. Therefore, we concluded that LE has a visceral fat-reduction effect. It has been previously reported that the visceral fat-reduction food constituents include catechine [19] and polyphenol [20]. The degree by which these constituents reduced visceral fat of the food consumed for 12 weeks was −10.3 cm2 for catechine and −7.9 cm2 for polyphenol, compared to a reduction of 8.89 cm2 by LE in this study. This finding suggests that LE has the same effect as food constituents that are generally considered to reduce visceral fat. It has been reported that protein-derived constituents also reduce visceral fat, and therefore, in this study we evaluated the effect of a daily intake of 8 g of lactic acid-fermented albumin as protein, based on a report on beta-conglycinin in soybeans [13, 14]. However, this study did not examine whether less than 8 g of EWP would exhibit a visceral fat-reduction effect and this requires further study. Furthermore, it has been reported that lactoferrin (LF), found in milk protein, has a visceral fat-reduction effect [21]. It has been found that a daily intake of 300 mg of LF significantly reduced VFA compared to baseline and the control group. In this study, the control group was given whey, which contains LF. It was expected that a daily intake of 8 g of whey would correspond to a daily intake of 450 mg of LF and was therefore expected to have a visceral fat-reduction effect. However, whey did not reduce visceral fat in the control group. A possible explanation is that whey contains many nutrients other than LF, which may have competed. It has previously been reported that a daily intake of 28 g of whey had no effect on visceral fat [22]. It was reported that it needs to be subjected to enteric coating to exert its visceral fat–reducing effects because LF itself is vulnerable to heating and is easily degraded by gastric acid [21]. This should explain why the whey sample used in the present study failed to reduce visceral fat.
Furthermore, in this study the ratio of visceral to subcutaneous fat was significantly reduced after consumption of LE compared to baseline ratio and the control group. The visceral to subcutaneous fat ratio is an indicator of visceral fat obesity, with a ratio > 0.4 indicating visceral fat obesity [23]. In our study, LE not only reduced VFA but also considerably reduced the visceral to subcutaneous fat ratio; therefore, we concluded that the symptoms of visceral fat obesity had reduced.
Although it is unclear why LE intake reduces visceral fat, it has been reported that EWP, the main constituent of LE, has an inhibitory effect on the absorption of triglycerides [11]. EWP inhibited the absorption of fat, thereby functioning to reduce lipid content within bile acid micelles. The components involved in this process are ovalbumin and ovotransferrin, both of which reduce lipid content within bile acid micelles to an equivalent extent. No other components have been shown to affect this process [11]. As such, we inferred that these two components might also have come into play in this experiment. Especially, the underlying cause of this has been reported to involve lipase inhibitory activity in ovalbumin [24], the main constituent of EWP, as well as the inhibitory effect of lipid micelles [11]. Furthermore, ovalbumin has been found to form FFAs and gels [25, 26]. Therefore, it is believed that EWP can inhibit the absorption of lipids by way of its physicochemical properties.
EWP has an amino acid score of 100, with a higher rate of net protein utilization than soy and milk proteins [27]. In a previous examination of the effect of EWP on carcass protein contents in rat compared to casein, we reported that EWP showed significantly higher levels than casein [12]. As the main constituent of muscle is protein, it is believed that the increase in carcass protein contents in rats were due to increased muscle mass. In general, however, a muscle does not increase without exercise; thus, further studies should be conducted to determine whether a muscle increases because of the high net protein utilization and increased body protein. The fact that muscle burns fat in the event of increased muscle may be one explanation for the observed reduction in visceral fat.
It is generally believed that active food constituents that reduce visceral fat are often those whose structures do not change through absorption or metabolic process (e.g., polyphenol), the effects of which are easily evaluated in vivo. In contrast, proteins become effective after being broken down into peptides and amino acids in the digestive tract. With regards to the details of the active constituents contained in EWP, we believe that the visceral fat-reduction mechanism should first be clarified and then confirmed via in vitro evaluation.
In this study, participants consumed either LE or whey drink at breakfast. Suzuki et al. reported that pre-exercise intake of EWP increases muscle and muscular strength [28]. It has been reported that consuming hen’s eggs at breakfast induced satiety and reduced participants’ body fat [29]. However, in this study, while participants’ energy intake hardly changed and the lactic acid drink did not affect their satiety, we confirmed that visceral fat was reduced. On the contrary, protein intake following muscle strength training is recommended to increase muscles [30]. Therefore, we believe that consuming LE after dinner or before sleeping might reduce visceral fat more effectively. Furthermore, if the visceral fat-reduction mechanism of EWP lies in the inhibition of lipid absorption [11], it may be preferable to consume LE at dinnertime, the meal with the highest energy intake. Moreover, previous research has reported that the circadian rhythm gene BMAL1, which is involved in lipid accumulation [31], is abundantly secreted at night. Therefore, we believe that the consumption of LE at dinnertime could more effectively inhibit the accumulation of lipids. Per these factors, while the present study indicated that LE intake at breakfast reduces VFA, the timing at which it effectively reduces visceral fat was not clarified and should be examined in future studies.
In the present study, the blood biomarkers exhibited no significant differences between week 0, week 6, and week 12. Although the present study involved subjects with slightly high levels of visceral fat weight, the other parameters such as blood lipids were within the normal range. This might have resulted in no significant changes being observed in the blood biomarkers. In previous studies, subjects with slightly high levels of serum cholesterol showed significant decreases in serum total cholesterol and LDL-cholesterol concentrations at week 4 and week 8 during 8 weeks of LE consumption as compared with prior to consumption [8]. This suggests the possibility that marked improvements may be achieved if subjects with borderline or abnormal blood biomarker values are involved.
Concern has been raised that EWP intake could cause allergies and biotin deficiency. In this study, individuals with food allergies were excluded during recruitment. It has been demonstrated that avidin found in raw egg whites binds to biotin, thereby reducing its absorption [32]. While the participants of this study were asked to consume 8 g of EWP per day for 12 consecutive weeks, there was no sign of clinical symptoms. A study in which participants consumed 200 g of dried egg white (approximately 160 g of EWP) daily reported signs of biotin deficiency after week 7 [33, 34]. The consumption period was 12 weeks; however, the amount of EWP intake was 8 g, which was 1/20th of the amount of EWP that caused biotin deficiency in the previous study, and may explain the observed lack of biotin deficiency. Furthermore, when egg white is in its raw state or heated, it has been reported that electrophoretic avidine bands disappear upon activation of pepsin [34]. During the digestive process, as pepsin is usually activated, we believe that a daily intake of 8 g of LE for 12 weeks should not cause biotin deficiency. Finally, we measured markers of liver and kidney function. No abnormal increases or decreases in numeric values were observed, suggesting that EWP can be consumed safely.
Metabolic syndrome, triggered by obesity, leads to hypertension, abnormal glucose tolerance, and is ultimately considered a cause of arteriosclerotic diseases. If we pursue this study further and clarify the visceral fat-reduction effect of EWP, we believe that it could improve the quality of life of patients with obesity. Furthermore, if the practical application of LE, which facilitates the egg white intake, becomes available, we believe that it would provide a good source of protein while reducing visceral fat and might be utilized to promote the health among the Japanese.
Conclusions
The results demonstrated that LE reduces VFA and improves the ratio of visceral to subcutaneous fat area. As other measurement items were not influenced, we concluded that LE improves visceral fat obesity.
Acknowledgments
This study was supported completely by a grant received from Kewpie Corporation, Japan. We thank Prof. Michihiro Sugano (Kyushu University, and Prefectural University of Kumamoto) for providing technical advice about this trial. The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
Experimental work in Nutrition Clinic, Kagawa Nutrition University was supported by Kewpie Corporation (Tokyo, Japan).
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Abbreviations
- BMI
Body Mass Index
- CT
Computed tomographic
- EWP
Egg white protein
- LE
Lactic-fermented egg white
- VFA
Visceral fat area
Authors’ contributions
RM, KK, MU, WW, YM, MK, AT, and KU conceived the study concept and design. AT, as the principal investigator, was responsible for study logistics, data acquisition and RM and KK for manuscript preparation. KK, MU, and WW were responsible for conducting the trial, data collection, and performing laboratory analysis. RM and AT carried out the statistical analysis. YM, MK, and KU supervised the study design and commented on the manuscript. All authors contributed to the intellectual content of the manuscript. All authors read and approved the final amnuscript.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki, and with the approval of the Ethics Committee of Kagawa Education Institute of Nutrition (authorization no. 243; 13th March, 2013). Participants received a thorough explanation of the study protocol and those who provided consent were included. The study was conducted at the Nutritional Clinic of Kagawa Education Institute of Nutrition.
Consent for publication
Not applicable.
Competing interests
KK, AT, KU declare no conflict of interest. RM, MU, WW, Y.M. and M.K. are employees of Kewpie Corporation. There are no other patents, products in development or marketed products to declare.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ryosuke Matsuoka, Email: ryosuke_matsuoka@kewpie.co.jp.
Keiko Kamachi, Email: kamachi@eiyo.ac.jp.
Mika Usuda, Email: mika_usuda@kewpie.co.jp.
Wei Wang, Email: yui_ou@kewpie.co.jp.
Yasunobu Masuda, Email: yasunobu_masuda@kewpie.co.jp.
Masaaki Kunou, Email: masaaki_kunou@kewpie.co.jp.
Akira Tanaka, Email: atanaka@eiyo.ac.jp.
Kazunori Utsunomiya, Email: kazu-utsunomiya@jikei.ac.jp.
References
- 1.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications, part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 2.Kato Y, Hamasaki T, Sato S, Ando Y. Relationship between the attitudes towards improving eating habits and prevalence of metabolic syndrome. Data from the 2005 National Health and nutrition survey and the comprehensive survey of living conditions. Nihon Koshu Eisei Zasshi. 2014;61:385–395. [PubMed] [Google Scholar]
- 3.Ruxto C. Recommendation for the use of egg in the diet. Nurs Stand. 2010;24:47–55. doi: 10.7748/ns.24.37.47.s53. [DOI] [Google Scholar]
- 4.Kats DL, Evans MA, Namaz H, Hjike VY, Chan W, Comerford BP, Hoxley ML. Egg consumption and endothelial function: a randomized controlled crossover trial. Int J Cardiol. 2010;99:65–70. doi: 10.1016/j.ijcard.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 5.Njike V, Faridi Z, Dutta S, Gonzalez-Simon AL, Kalz DL. Dietary egg consumption in hyperlipidemic adults-effects on endothelial function and cardiovascular risk. Nutr J. 2010;9:28. doi: 10.1186/1475-2891-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakamura Y, Iso H, Kita Y, Ueshima H, Okada K, Konishi M, Inoue M, Tsugane S. Egg consumption serum total cholesterol concentrations and coronary heart disease incidence: Japanese public health center-based prospective study. Br J Nutr. 2006;96:921–928. doi: 10.1017/BJN20061937. [DOI] [PubMed] [Google Scholar]
- 7.McNamara DJ. Dietary cholesterol and atherosclerosis. Biochem Biophys Acta. 2000;1529:310–320. doi: 10.1016/s1388-1981(00)00156-6. [DOI] [PubMed] [Google Scholar]
- 8.Asato L, Wang MF, Chan YC, Yeh SH, Chung HM, Chung SY, Chida S, Uezato T, Suzuki I, Yamagata N, Kokubu T, Yamamoto S. Effect of egg white on serum cholesterol concentration in young women. J Nutr Sci Vitaminol. 1996;42:87–96. doi: 10.3177/jnsv.42.87. [DOI] [PubMed] [Google Scholar]
- 9.Matsuoka R, Kimura M, Muto A, Masuda Y, Sato M, Imaizumi K. Mechanism for the cholesterol-lowering action of egg white protein in rats. Biosci Biotechnol Biochem. 2008;72:1506–1512. doi: 10.1271/bbb.80016. [DOI] [PubMed] [Google Scholar]
- 10.Matsuoka R, Takahashi Y, Kimura M, Masuda Y, Kunou M. Heating has no effect on the net protein utilisation from egg whites in rats. Sci World J. 2017:6817196. [DOI] [PMC free article] [PubMed]
- 11.Matsuoka R, Shirouchi B, Kawamura S, Baba S, Shiratake S, Nagata K, Imaizumi K, Sato M. Dietary egg white protein inhibits lymphatic lipid transport in thoracic lymph duct-cannulated rats. J Agr Food Chem. 2014;62:10694–10700. doi: 10.1021/jf502741b. [DOI] [PubMed] [Google Scholar]
- 12.Matsuoka R, Shirouchi B, Umegatani M, Fukuda M, Muto A, Masuda Y, Kunou M, Sato M. Dietary egg-white protein increased body protein mass and reduces body fat mass through an acceleration of hepatic β-oxidation in rats. Br J Nutr. 2017;118:423–430. doi: 10.1017/S0007114517002306. [DOI] [PubMed] [Google Scholar]
- 13.Arimitsu K, Takashi K, Matsuoka R, Narita K, Idei A. The good function of lactic fermented egg white “Lacty Egg.”. Jpn J Food Engineering. 2015;16:79–82. [Google Scholar]
- 14.Matsuoka R, Usuda M, Masuda Y, Kunou M, Utsunomiya K. Lactic-fermented egg white reduced serum cholesterol concentrations in mildly Hypercholesterolemic Japanese men: a double-blind, parallel-arm design. Lipids Health Dis. 2017;16:101. doi: 10.1186/s12944-017-0499-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kohno M, Hirotsuka M, Kito M, Matsuzawa Y. Decreases in serum triglycerol and visceral fat mediated by dietary soybean beta-conglycinin. J Atheroscler Thromb. 2006;13:247–255. doi: 10.5551/jat.13.247. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura R, Takeyama M, Nakamura K, Umemura O. Constituent proteins of globulin fraction obtained from egg white. Agric Biol Chem. 1980;44:2357–2362. [Google Scholar]
- 17.Kimberly AE, Roberts MGA. Method for the direct determination of organic nitrogen by the Kjeldahl process. Public Health Pap Rep. 1905;31:109–122. [PMC free article] [PubMed] [Google Scholar]
- 18.Friedewald WT, Levy RI, Frederickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 19.Nagao T, Hase T, Tokimitsu IA. Green tea extract high in cathechins reduces body fat and cardiovascular risks in humans. Obesity. 2007;15:1473–1483. doi: 10.1038/oby.2007.176. [DOI] [PubMed] [Google Scholar]
- 20.Akazome Y, Kametani N, Kanda T, Shimasaki H, Kobayashi S. Evaluation of safety of excessive intake and efficacy of long-term intake of beverages containing apple polyphenols. J Oleo Sci. 2010;59:321–338. doi: 10.5650/jos.59.321. [DOI] [PubMed] [Google Scholar]
- 21.Ono T, Murakoshi M, Suzuki N, Iida N, Ohdera M, Iigo M, Yoshida T, Sugiyama K, Nishino H. Potent anti-obesity effect of enreric-coated lactoferrin: decrease in visceral fat accumulation in Japanese men and women with abdominal obesity after 8-week administration of enteric coated lactofferin tablets. Br J Nutr. 2010;104:1688–1695. doi: 10.1017/S0007114510002734. [DOI] [PubMed] [Google Scholar]
- 22.Beer DJ, Stoke KS, Paul DR, Harris GK, Rumpler WV, Clevidence BA. Whey protein but not soy protein supplementation alters body weight and composition in free-living overweight and obese adults. J Nutr. 2011;141:1489–1494. doi: 10.3945/jn.111.139840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kadowaki T, Sekikawa A, Murata K, Maegawa H, Takamiya T, Okamura T, El-Saed A, Miyamatsu N, Edmundowicz D, Kita Y, et al. Japanese men have larger areas of visceral adipose tissue than Caucasian men in the same levels of waist circumference in a population-based study. IntJ Obesity. 2006;30:1163–1165. doi: 10.1038/sj.ijo.0803248. [DOI] [PubMed] [Google Scholar]
- 24.Gargouri Y, Julien R, Sugihara A, Verger R, Sarda L. Inhibition of pancreatic and microbial lipases by proteins. Biochim Biophys Acta. 1984;795:326–331. doi: 10.1016/0005-2760(84)90082-1. [DOI] [PubMed] [Google Scholar]
- 25.Uno-Ohta N, Toryu H, Higasa T, Maeda H, Okada M, Ohta H. Gelation properties of ovalbumin as affected by fatty acid salts. J Food Sci. 1996;61:906–910. doi: 10.1111/j.1365-2621.1996.tb10899.x. [DOI] [Google Scholar]
- 26.Handa A, Gebbadios A, Hanna MA, Weller CL, Kuroda N. Physical and molecular properties of egg-white lipid films. Food Chem Toxicol. 1999;64:860–864. [Google Scholar]
- 27.Sheffner AL, Eckfeldt GA, Spector H. The pepsin-digest-residue (PDR) amino acid index of net protein utilization. J Nutr. 1956;60:105–120. doi: 10.1093/jn/60.1.105. [DOI] [PubMed] [Google Scholar]
- 28.Kato Y, Sawada A, Numao S, Suzuki M. Chronic effect of light resistance exercise after ingestion of a high protein snack on increase of skeletal muscle mass and strength in young adults. J Nutr Sci Vitaminol. 2011;57:233–238. doi: 10.3177/jnsv.57.233. [DOI] [PubMed] [Google Scholar]
- 29.Fallaize R, Wilson L, Gray J, Morgan LM, Griffin BA. Variation in the effects of three different breakfast meals on subjective satiety and subsequent intake of energy at lunch and evening meal. Eur J Nutr. 2013;52:1353–1359. doi: 10.1007/s00394-012-0444-z. [DOI] [PubMed] [Google Scholar]
- 30.Wilkinson SB, Tarnopolsky MA, Macdonald MJ, Macdonald JR, Armstrong D, Phillips SM. Consumption of fluid skim milk promotes greater muscle protein accretion after resistance exercise than does consumption of an isonitrogenous and isoenergetic soy-protein beverage. Am J Clin Nutr. 2007;85:1031–1340. doi: 10.1093/ajcn/85.4.1031. [DOI] [PubMed] [Google Scholar]
- 31.Shimba S. The roles of clock genes in obesity. Nihon Rinsho. 2013;71:244–248. [PubMed] [Google Scholar]
- 32.Said AM. Cell and molecular aspect of human intestinal biotin absorption. J Nutr. 2008;139:158–162. doi: 10.3945/jn.108.092023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baugh CM, Malone JH. Human biotin deficiency, a case history of biotin deficiency induced by raw egg consumption in a cirriphotic patient. Am J Clin Nutr. 1968;21:173–182. doi: 10.1093/ajcn/21.2.173. [DOI] [PubMed] [Google Scholar]
- 34.Sakai K, Ushiyama Y, Manabe S. Peptic and pancreatic digestibility of raw and heat-coagulated hen’s egg white proteins. Jpn J Pediatr Allergy Clin Immunol. 1999;13:36–42. doi: 10.3388/jspaci.13.36. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.


