Abstract
Background
Real world data have an important role to play in the evaluation of epidemiology and burden of disease; and in assisting health-care decision-makers, especially related to coverage and payment decisions. However, there is currently no overview of the existing longitudinal real world data sources in Parkinson’s disease (PD) in the USA. Such an assessment can be very helpful, to support a future effort to harmonize real world data collection and use the available resources in an optimal way.
Methods
The objective of this comprehensive literature review is to systematically identify and describe the longitudinal, real world data sources in PD in the USA, and to provide a summary of their measurements (categorized into 8 main dimensions: motor and neurological functions, cognition, psychiatry, activities of daily living, sleep, quality of life, autonomic symptoms and other). The literature search was performed using MEDLINE, EMBASE and internet key word search.
Results
Of the 53 data sources identified between May and August 2016, 16 were still ongoing. Current medications (81%) and comorbidities (79%) were frequently collected, in comparison to medical imaging (36%), genetic information (30%), caregiver burden (11%) and healthcare costs (2%). Many different measurements (n = 108) were performed and an interesting variability among used measurements was revealed.
Conclusions
Many longitudinal real world data sources on PD exist. Different types of measurements have been performed over time. To allow comparison and pooling of these multiple data sources, it will be essential to harmonize practices in terms of types of measurements.
Keywords: Parkinson disease, Rating scales, Longitudinal, Cohort studies, Real-world
Background
Parkinson’s disease (PD) is a progressive neurodegenerative disease affecting approximately 630,000 people in the USA and for which no disease-modifying therapy is currently available. With the ever growing ageing population, this number is projected to almost double to 1.1 million by 2030 [1].
The Food and Drug Administration (FDA) defines “real world data” as “all data collected from sources outside of traditional clinical trials” and “real world evidence” as “all evidence derived from aggregation and analysis of real world data” [2]. Such real world evidence reflecting disease progression, treatments and outcomes under conditions of routine clinical practice is a very important resource. It can take a pivotal role to improve the understanding of the underlying disease process [3], optimize currently available therapies and develop new treatment strategies [2, 4].
Although the burden of PD and the interest of real world data are well-known [5, 6], there has not been a literature review to present the overview of longitudinal, real world studies conducted in the USA on PD patients.
There is a need for a comprehensive review to create an integrated view and assist investigators and clinicians to optimize the measurements that best match with their objectives and the already existing data sources [4, 7]. Such an assessment can be very helpful, to support a future effort to harmonize real world data collection and use the available resources in an optimal way.
The objective of this comprehensive literature review is to systematically identify and describe the longitudinal, real world data sources in PD, and to provide a summary of the key characteristics and the measurements assessed in real world studies, as a part of an effort to mobilize a harmonization process, similar to the one that already takes place in Europe.
Methods
Search strategy and literature sources
The search was performed on ProQuest. It was based in MEDLINE on Pubmed, in EMBASE and internet key word search between May and August 2016. Related MeSH, EMTREE and key terms were combined. Articles from peer-reviewed journals, conference abstracts and reviews were screened (AT). The search equation terms are detailed in Appendix 1.
Study screening and selection
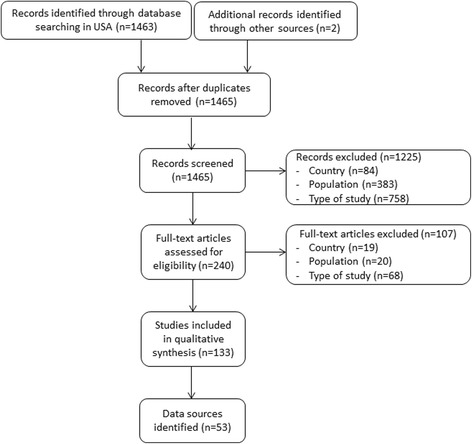
We included all studies including patients with a diagnosis of PD based on real world data. We restricted inclusion to only longitudinal, observational cohort studies and registries. The setting was restricted to the USA and the timing of publication in the last 10 years (2006-2016). Cohorts or registries without any publication in the last 10 years were considered as outdated. Exclusion criteria were based on population characteristics: Other diagnosis (e.g. Wolff-Parkinson-White disease or only Parkinsonian syndromes), autopsy data, and studies not focused on patients (e.g. focused on physicians). Moreover, studies without American patients or non-longitudinal studies, such as case-control, were also excluded. Only one main exclusion criterion was reported in the flow chart per excluded study (Fig. 1). No limits were applied for language.
Fig. 1.
Flowchart
Data extraction
In a first step, when a publication allowed the identification of a data source of interest, the detailed information available in the publication was extracted. Information on design and setting, funding, population selection, follow-up and measurements were recorded. This was supplemented and updated via information found with an internet search of the study website, registration sites such as clinicaltrials.gov and investigators / funders’ websites. The list of all information captured is available in Appendix 2.
In a second step, a classification of measurements was performed for the following dimensions: motor and neurological function, cognition, psychiatric symptoms, activities of daily living, sleep quality, quality of life, autonomic symptoms and other. The “other” dimension gathers some known PD symptoms such as olfaction [8] not included in the previous main dimensions and more general information such as caregivers’ burden measurements. Some dimensions were subdivided in sub dimensions due to their complexity and variety (e.g. Motor and neurological symptoms is sub divided into 4 sub dimensions: global, gait and balance, fine movement and other). This classification was based on the literature [4] with one adaptation: as very few sensory markers were identified, they were gathered in the “other” category.
Data analysis
Data source characteristics were described globally. To address the variability of sources, the description was also performed according to four main characteristics: the completion status (ongoing vs completed); the study population (Parkinson specific data sources vs “generic” data sources including both Parkinsonian patients and patients of other diagnostics); the categories of studies (investigate for motor symptoms, non-motor symptoms, biomarkers, genetics or mixed); and the country (US only vs international sources). Descriptive statistics were reported as absolute frequency and percentages.
Results
Of 1463 records screened, 84% were excluded based on title and abstract, and 7% after review of the full-text (Fig. 1). The most frequent exclusion criterion was that studies were not longitudinal. Only 133 (9%) were included in the qualitative analysis. Of these 133 studies, data from 53 different data sources were extracted [9–61]. Only one registry was included with 52 cohorts.
Longitudinal real world sources (Table 1)
Table 1.
Overview of data sources characteristics (n = 53)
| Characteristics | Included | Status | Country | Study population | ||||
|---|---|---|---|---|---|---|---|---|
| All (n = 53) | Ongoing (n = 16) | Completed (n = 37) | USA (n = 42) | International (n = 11) | Parkinson cohort (n = 25) |
“Generic” cohort (n = 28) |
||
| Size (number of Parkinsonian patients) | ||||||||
| 0-500 | 42 (79) | 11 (69) | 31 (84) | 37 (88) | 5 (45) | 22 (88) | 20 (71) | |
| 500-1000 | 7 (13) | 4 (25) | 3 (8) | 3 (7) | 4 (36) | 3 (12) | 4 (14) | |
| >1000 | 4 (8) | 1 (6) | 3 (8) | 2 (5) | 2 (18) | 0 (0) | 4 (14) | |
| Duration of follow-up (years) | ||||||||
| <2 | 6 (11) | 0 (0) | 6 (16) | 4 (10) | 2 (18) | 4 (16) | 2 (7) | |
| 2-5 | 20 (38) | 4 (25) | 16 (43) | 16 (38) | 4 (36) | 13 (52) | 7 (25) | |
| ≥5 | 27 (51) | 12 (75) | 15 (41) | 22 (52) | 5 (45) | 8 (32) | 19 (68) | |
| Dimensions assessed | ||||||||
| Motor and neurological | 46 (87) | 12 (75) | 34 (92) | 36 (86) | 10 (91) | 25 (100) | 21 (75) | |
| Cognition | 41 (77) | 13 (81) | 28 (76) | 36 (86) | 5 (45) | 17 (68) | 24 (86) | |
| Psychiatric symptoms | 38 (72) | 10 (63) | 28 (76) | 30 (71) | 8 (73) | 19 (76) | 17 (61) | |
| Activities of daily living | 22 (42) | 6 (38) | 16 (43) | 15 (36) | 7 (64) | 12 (48) | 10 (36) | |
| Sleep quality | 11 (21) | 4 (25) | 7 (19) | 5 (12) | 6 (55) | 2 (8) | 9 (32) | |
| Quality of life | 9 (17) | 4 (25) | 5 (14) | 5 (12) | 4 (36) | 6 (24) | 3 (11) | |
| Autonomic symptoms | 7 (13) | 4 (25) | 3 (8) | 3 (7) | 4 (36) | 0 (0) | 7 (25) | |
| Other | 20 (38) | 9 (56) | 11 (30) | 13 (31) | 7 (64) | 8 (32) | 12 (43) | |
| Other assessments | ||||||||
| Current medications | 43 (81) | 13 (81) | 30 (81) | 32 (76) | 11 (100) | 22 (88) | 21 (75) | |
| Comorbidities | 42 (79) | 14 (88) | 28 (76) | 31 (74) | 11 (100) | 20 (80) | 22 (79) | |
| Medical imaging | 19 (36) | 6 (40) | 13 (34) | 11 (26) | 8 (73) | 6 (24) | 13 (46) | |
| Genetics | 16 (30) | 6 (38) | 10 (27) | 10 (24) | 6 (55) | 3 (12) | 13 (46) | |
| Caregiver burden | 6 (11) | 4 (27) | 2 (5) | 5 (12) | 1 (9) | 4 (16) | 2 (7) | |
| Healthcare costs | 1 (2) | 1 (7) | 0 (0) | 0 (0) | 1 (9) | 1 (4) | 0 (0) | |
Data are shown as absolute frequency (percentage)
Forty-two sources (79%) were only in the USA. Three of the 11 international sources were only in North America while the other eight included patients in the USA and Europe, and two also included Asia. Most of the sources included less than 500 PD patients (79%) for more than 5 years (51%). Although most of the sources included information about current medications (81%) and comorbidities (79%); only few collected information on medical imaging (36%), genetics (30%), caregiver’ burden (11%) and healthcare costs (2%).
Among the 53 sources, 16 (30%) are still ongoing. There has been an increased availability of genetic information (38% vs 27%) and caregivers’ burden data (27% vs 5%) in ongoing versus completed sources, respectively. Moreover, there has been a trend toward larger inclusions and longer durations: comparing ongoing versus completed sources, 31% vs 16% included more than 500 patients and 75% vs 41% have a duration of more than 5 years.
Likewise, US sources were smaller and shorter than international sources (88% vs 45% included less than 500 PD patients, and 52% vs 45% have a duration of more than 5 years). US sources reported more caregiver burden data than international sources (12% vs 9%) but less frequently the other assessments such as medical imaging (26% vs 73%) or genetic information (24% vs 55%).
Sources including only Parkinsonian patients were smaller (12% vs 28% included more than 500 patients) and shorter (32% vs 68% had a duration of more than 5 years) than the “generic” cohorts. Medical imaging (24% vs 46%) and genetics (12% vs 46%) were less assessed in Parkinson’s specific than in “generic” cohorts.
The 53 data sources have different objectives. Mainly the sources investigated as their primary objective: non-motor symptoms (32%), then biomarkers (21%), motor symptoms (15%) and genetics (4%). Fifteen sources (28%) investigated several of these points as first objective. The sources investigating the biomarkers as primary objective were large and recent with four sources still ongoing and four sources begun in the last 5 years. In contrast, the sources investigating the motor symptoms as primary objective were small, all with less than 500 patients and with very frequent assessment, on average twice a year.
Measurements in real world studies in PD
The name of each included data source with its main characteristics (Table 2) and its measurements (Table 3) are presented individually. A large number of measurements (n = 108) was identified through this literature review and each of the 53 sources had its own unique range of measurements (Table 4). Most of the measurements were cited only once or twice. The distribution of the number of measurements over the different dimensions was not equal with only 3 different to assess autonomic symptoms and 43 to assess cognition.
Table 2.
Overview of data sources characteristics listed in alphabetic order (n = 53)
| Nb | Study | Acronym | Individuals included | Follow-up duration (y) | Planned follow-up | Main inclusion criteria |
|---|---|---|---|---|---|---|
| 1 | A Longitudinal Observational Follow-up of the PRECEPT Study Cohorta | PostCEPT | 537 | 4 | Post-RCT; under dopaminergic therapy | |
| 2 | Abnormalities in metabolic network activity precede the onset of motor symptoms in Parkinson’s disease | 15 | 4 | Every 2 years | Hemi parkinsonism | |
| 3 | Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia | 46 | 5 | Annually | ||
| 4 | Arizona Study of Aging and Neurodegenerative Disease | AZSAND | 3000 | ongoing | ||
| 5 | Ashkenazi Jewish LRRK2 consortium cohort | LRRK2 | 2611 | 1.5 | Every 12-18 months | Ashkenazi Jewish |
| 6 | Baltimore Longitudinal Study of Aging | BLSA | 10,000? | ongoing | Every few years for life | Healthy |
| 7 | Boston university medical center - University of Alabama Birmingham - Washington University in Saint Louis School of medicine | 80 | 2 | >40 years | ||
| 8 | Central Control of Mobility in Aging | CCMA | 439 | ongoing | Annually | Elderly (>65 years); non demented |
| 9 | Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study | 50 | 4 | Annually | Levodopa treatment | |
| 10 | Charting the progression of disability in Parkinson disease | 171 | 2 | Every 6 months | >40 years; mild to moderate Parkinson’s disease | |
| 11 | Clinical course in Parkinson’s disease with elevated homocysteine | 97 | 2 | Every 2 years | 35-90 years without brain surgery or neurologic/psychiatric comorbidity | |
| 12 | Clinical Research in Neurology (CRIN) - Emory center | CRIN | 3581 | 15 | ||
| 13 | Comparative utility of the BESTest; mini-BESTest; and brief-BESTest for predicting falls in individuals with Parkinson disease: a cohort study | BESTest | 80 | 1 | Every 6 months | Without neuropsychiatric comorbidities |
| 14 | Comparison of the Agonist Pramipexole With Levodopa on Motor Complications of Parkinson’s Diseasea | CALM-PD follow-up | 301 | 2 | Annually | Post-RCT; under dopaminergic therapy; diagnostic < 7 years |
| 15 | Contursi kindred | CONTURSI | 210 | ? | ||
| 16 | Deprenyl and Tocopherol Antioxidative Therapy of Parkinsonisma | DATATOP | 403 | 6 | Every 3 months | Early phase; postRCT; 30-79 years |
| 17 | Depression in Parkinson’s disease | 685 | 3.9 | Annually | ||
| 18 | Dopamine agonist withdrawal syndrome in Parkinson diseasea | DAWS | 93 | 0.25 | Annually | Non demented |
| 19 | Einstein Aging Study (Bronx Aging Study) | EAS | 791 | ongoing | Every 12 to 18 months | Elderly (>70 years) |
| 20 | Emergence and evolution of social self-management of Parkinson’s disease | 120 | 3 | Every 6 months | Non demented | |
| 21 | Hallucinations and sleep disorders in PD: ten-year prospective longitudinal study | 89 | 10 | 0; 6 months; 18 months; 4 years; 6 years; 10 years | 24-h caregiver; without neuroleptic treatment; without some comorbidities | |
| 22 | Harvard Alumni Health Study | 500,002 | 77 | 1962; 1966; 1972; 1988; 1993 | Harvard students | |
| 23 | Health Professionals Follow-up Study | HPFS | 51,529 | ongoing | Biannually | Men; healthy; 40-75 years |
| 24 | Honolulu Asia Aging Study | HAAS | 3741 | 15 | 3 times between 1994 and 2001 | Elderly Japanese-American men |
| 25 | Longitudinal study of normal cognition in Parkinson disease | 141 | 6 | Biannual for 4 years and annual after | Normal cognition at baseline | |
| 26 | Long-term outcomes of bilateral subthalamic nucleus stimulation in patients with advanced Parkinson’s diseasea | 33 | 2 | 0 –3 –6 –12 –18 – 24 months | Advanced phase with deep brain stimulation | |
| 27 | Loss of ability to work and ability to live independently in Parkinson’s disease | 495 | 10 | |||
| 28 | Major life events and development of major depression in Parkinson’s disease patients | PEG study | 221 | 4 | Annually | New onset (within 3 years) |
| 29 | Mayo Clinic cohort study of Personality and Aging (including Rochester Epidemiology project) | 7216 | 29.2 | Historically for life | 20-69 years | |
| 30 | Mayo clinic study of aging (Olmsted county resident) - Rochester Epidemiology project indexing system | MCSA | 2739 | ongoing | ||
| 31 | Molecular Epidemiology of Parkinson’s Disease | MEPD | 1600 | ongoing | >40 years | |
| 32 | Mood and motor trajectories in Parkinson’s disease: multivariate latent growth curve modeling | 186 | 1.5 | 6 months; 18 months | ||
| 33 | Mood and Subthalamic Nucleus Deep Brain Stimulationa | MOST | 91 | 1 | Deep brain stimulation eligible; not demented | |
| 34 | Morris K Udall Parkinson’s Disease Research Center of Excellence cohort - Veteran affair | Udall | 314 | ongoing | Elderly (>60 years) | |
| 35 | National Parkinson Foundation Quality Improvement Initiative | NPF-QII | 10,000 | on going | ||
| 36 | NeuroGenetics Research Consortium | NGRC | 3072 | >10 | ||
| 37 | Nurses’ Health Study | NHS | 280,000 | ongoing | Every 2 years | Women; healthy; 19-51 years |
| 38 | Oxford Parkinson’s Disease Centre | OPDC | 1500 | 1.5 | 18 months | |
| 39 | Parkinson’s Associated Risk Study | PARS | 10,000 | ongoing | Elderly (>60 years) | |
| 40 | Parkinson’s Disease Biomarkers Program | PDBP | 1436 | ongoing | Evidence of response to dopaminergic medication | |
| 41 | Parkinson’s Disease Research Education and Clinical Center - Parkinson’s Genetic Research Study | PADRECCS - PaGeR | 1880 | ongoing | ||
| 42 | Parkinson’s disease: increased motor network activity in the absence of movement | NMRP | 12 | 4.4 | Every 2 years | Non demented; tremor-dominant clinical manifestations; without some comorbidities |
| 43 | Parkinson’s Progression bioMarkers Initiative | PPMI | 748 | ongoing | Every 3 months the first year then every 6 months | Untreated recently diagnosed |
| 44 | Prospective cohort study of impulse control disorders in Parkinson’s disease | ICD-PD | 164 | 4 | Non demented | |
| 45 | Rate of 6-18Ffluorodopa uptake decline in striatal subregions in Parkinson’s disease | 37 | 4 | Every 1 to 2 years | ||
| 46 | Religious Order Study | ROS | >1100 | >7 | Annually | Elderly; religious clergy |
| 47 | Rush Memory and Aging Project | RMAP | 1556 | 5 | Annually | Elderly without know dementia |
| 48 | Study of Osteoporotic Fractures (SOF) Research Group | SOF | 9704 | >6 | Tri-annually | Women; Elderly (>65 years) |
| 49 | The effect of age of onset of PD on risk of dementia | 440 | 4 | Annually | Elderly (>65 years) | |
| 50 | University of California Los Angeles Center for Genes and Environmental in Parkinson’s Disease | UCLA CGEP | 363 | 5 | Diagnostic >3 years | |
| 51 | University of Miami Brain Endowment Bank | UM/BEB | 150 | ongoing | Annually | Consent to donate brain |
| 52 | UPDRS activity of daily living score as a marker of Parkinson’s disease progression | 162 | 6 | Every 2 years | ||
| 53 | Washington Heights-Inwood Columbia Aging | WHICAP | 2776 | 3.7 | Annually | Elderly (>65 years) |
Post-RCT = Open label extension after a Randomized Controlled Trial
aTreatment directed data sources
Table 3.
Overview of data source measurements and of the number of evaluations or assessments applied (n = 53)
| Nb | Study | Motor and neurological | Cognition | Psychiatry | Activities of daily living | Sleep | Quality of life | Autonomic | Other |
|---|---|---|---|---|---|---|---|---|---|
| 1 | A Longitudinal Observational Follow-up of the PRECEPT Study Cohort | 3 | 4 | 3 | 1 | 0 | 0 | 0 | 0 |
| 2 | Abnormalities in metabolic network activity precede the onset of motor symptoms in Parkinson’s disease | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3 | Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia | 2 | 14 | 1 | 0 | 0 | 0 | 0 | 0 |
| 4 | Arizona Study of Aging and Neurodegenerative Disease | 4 | 12 | 3 | 0 | 1 | 0 | 1 | 1 |
| 5 | Ashkenazi Jewish LRRK2 consortium cohort | 3 | 2 | 2 | 2 | 1 | 0 | 1 | 1 |
| 6 | Baltimore Longitudinal Study of Aging | 0 | 2 | 3 | 0 | 0 | 0 | 0 | 0 |
| 7 | Boston university medical center - University of Alabama Birmingham - Washington University in Saint Louis School of medicine | 9 | 1 | 1 | 0 | 0 | 1 | 0 | 0 |
| 8 | Central Control of Mobility in Aging | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 9 | Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study | 1 | 6 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10 | Charting the progression of disability in parkinson disease | 9 | 1 | 1 | 0 | 0 | 1 | 0 | 0 |
| 11 | Clinical course in Parkinson’s disease with elevated homocysteine | 1 | 9 | 1 | 1 | 0 | 0 | 0 | 0 |
| 12 | Clinical Research in Neurology (CRIN) - Emory center | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 13 | Comparative utility of the BESTest; mini-BESTest; and brief-BESTest for predicting falls in individuals with Parkinson disease: a cohort study | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14 | Comparison of the Agonist Pramipexole With Levodopa on Motor Complications of Parkinson’s Disease | 3 | 1 | 2 | 2 | 1 | 3 | 0 | 0 |
| 15 | Contursi kindred | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| 16 | Deprenyl and Tocopherol Antioxidative Therapy of Parkinsonism | 2 | 5 | 0 | 0 | 0 | 0 | 0 | 0 |
| 17 | Depression in Parkinson’s disease | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 18 | Dopamine agonist withdrawal syndrome in parkinson disease | 2 | 1 | 4 | 1 | 0 | 1 | 0 | 0 |
| 19 | Einstein Aging Study (Bronx Aging Study) | 2 | 11 | 1 | 0 | 0 | 0 | 0 | 0 |
| 20 | Emergence and evolution of social self-management of Parkinson’s disease | 2 | 2 | 1 | 1 | 0 | 4 | 0 | 0 |
| 21 | Hallucinations and sleep disorders in PD: ten-year prospective longitudinal study | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| 22 | Harvard Alumni Health Study | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 23 | Health Professionals Follow-up Study | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 24 | Honolulu Asia Aging Study | 2 | 4 | 2 | 0 | 1 | 0 | 1 | 1 |
| 25 | Longitudinal study of normal cognition in Parkinson disease | 2 | 6 | 2 | 1 | 0 | 0 | 0 | 0 |
| 26 | Long-term outcomes of bilateral subthalamic nucleus stimulation in patients with advanced Parkinson’s disease | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 |
| 27 | Loss of ability to work and ability to live independently in Parkinson’s disease | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 28 | Major life events and development of major depression in Parkinson’s disease patients | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| 29 | Mayo Clinic cohort study of Personality and Aging (including Rochester Epidemiology project) | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 |
| 30 | Mayo clinic study of aging (Olmsted county resident) - Rochester Epidemiology project indexing system | 1 | 10 | 3 | 0 | 1 | 0 | 1 | 1 |
| 31 | Molecular Epidemiology of Parkinson’s Disease | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| 32 | Mood and motor trajectories in Parkinson’s disease: multivariate latent growth curve modeling | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| 33 | Mood and Subthalamic Nucleus Deep Brain Stimulation | 2 | 0 | 7 | 0 | 0 | 0 | 0 | 0 |
| 34 | Morris K Udall Parkinson’s Disease Research Center of Excellence cohort - Veteran affair | 2 | 3 | 2 | 1 | 0 | 1 | 0 | 1 |
| 35 | National Parkinson Foundation Quality Improvement Initiative | 3 | 2 | 0 | 0 | 0 | 1 | 0 | 1 |
| 36 | NeuroGenetics Research Consortium | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 37 | Nurses’ Health Study | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 |
| 38 | Oxford Parkinson’s Disease Centre | 6 | 3 | 2 | 1 | 2 | 1 | 0 | 2 |
| 39 | Parkinson’s Associated Risk Study | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1 |
| 40 | Parkinson’s Disease Biomarkers Program | 4 | 3 | 6 | 1 | 6 | 5 | 1 | 3 |
| 41 | Parkinson’s Disease Research Education and Clinical Center - Parkinson’s Genetic Research Study | 3 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 42 | Parkinson’s disease: increased motor network activity in the absence of movement | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 43 | Parkinson’s progression biomarkers initiative | 1 | 5 | 4 | 2 | 2 | 0 | 1 | 2 |
| 44 | Prospective cohort study of impulse control disorders in Parkinson’s disease | 2 | 1 | 2 | 1 | 0 | 0 | 0 | 0 |
| 45 | Rate of 6-18Ffluorodopa uptake decline in striatal subregions in Parkinson’s disease | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 46 | Religious Order Study | 6 | 11 | 4 | 1 | 0 | 0 | 0 | 0 |
| 47 | Rush Memory and Aging Project | 5 | 1 | 3 | 1 | 1 | 0 | 0 | 2 |
| 48 | Study of Osteoporotic Fractures (SOF) Research Group | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 2 |
| 49 | The effect of age of onset of PD on risk of dementia | 1 | 6 | 1 | 0 | 0 | 0 | 0 | 0 |
| 50 | University of California Los Angeles Center for Genes and Environmental in Parkinson’s Disease | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 51 | University of Miami Brain Endowment Bank | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 2 |
| 52 | UPDRS activity of daily living score as a marker of Parkinson’s disease progression | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 53 | Washington Heights-Inwood Columbia Aging | 1 | 6 | 0 | 1 | 0 | 0 | 0 | 0 |
Table 4.
Measurements classification and use in data sources (n = 108)
| Dimension | Measurement acronym | Measurement full name | Data sources (number and numbering) |
|---|---|---|---|
| Motor and neurological (n = 46) | |||
| Global | H&Y | Hoehn and Yahr | (n = 30) °1,2,3,4,5,7,9,10,13,14,16,17,18,20,21,25,26,27,31,33,34,35,38,40,41,42,44,45,50,51 |
| UPDRS-III | Unified Parkinson’s Disease Rating Scale - motor examination | (n = 41) °1,2,3,4,5,7,8,10,11,13,14,16,17,18,19,20,21,24,25,26,27,28,30,32,33,34,35,36,38,40,41,42,43,44,45,46,47,49,50,52,53 | |
| UPDRS-IV | Unified Parkinson’s Disease Rating Scale - motor complications | (n = 2) n°1,14 | |
| Gait and balance | Berg balance test | (n = 2) n°7,10 | |
| Flamingo test | (n = 1) n°38 | ||
| FGA | Functional Gait Assessment | (n = 2) n°7,10 | |
| FOGQ | Freezing of gait questionnaire | (n = 2) n°7,10 | |
| Gait speed | (n = 4) n°7,8,10,46 | ||
| PIGD | Postural Instability / Gait Difficulty scale | (n = 2) n°5,40 | |
| Tandem gait | (n = 1) n°48 | ||
| TUG | Time Up and Go test | (n = 6) n°7,10,35,38,40,47 | |
| Walk test | (n = 5) n°7,10,46,47,48 | ||
| Fine movement | Finger tapping | (n = 3) n°4,46,47 | |
| Purdue pegboard test | (n = 6) n°4,7,10,38,46,47 | ||
| Reaction time | (n = 1) n°24 | ||
| Unknown | (n = 1) n°15 | ||
| Cognition (n = 41) | |||
| Global | ACE | Addenbrooke’s Cognitive Examination | (n = 1) n°40 |
| AD-8 | Ascertian Dementia 8-item Informant | (n = 1) n°31 | |
| BDRS | Blessed Dementia Rating Scale | (n = 2) n°19,53 | |
| CAMCOG | Cambridge Cognitive Assessment | (n = 1) n°49 | |
| CASI | Cognitive Abilities Screening Instrument | (n = 1) n°24 | |
| CDR | Clinical Dementia Rating scale | (n = 5) n°3,4,6,19,30,53 | |
| Clock drawing test | (n = 1) n°4 | ||
| DRS2 | Dementia Rating Scale 2 | (n = 6) n°4,19,25,26,34,53 | |
| HDS | Hasegawa Dementia Rating Scale | (n = 1) n°24 | |
| MDRS | Mattis Dementia Rating Scale | (n = 2) n°4,26 | |
| MMSE | Mini Mental State Examination | (n = 30) °1,3,4,5,7,9,10,11,12,14,15,16,18,20,21,24,26,28,31,34,36,37,38,42,44,45,46,47,48,50 | |
| MoCA | Montreal Cognitive Assessment | (n = 9) n°1,4,5,20,34,38,40,41,43 | |
| IQCODE | Informant Questionnaire on Cognitive Decline in Elderly | (n = 1) n°24 | |
| SPMSQ | Short Portable Mental Status Questionnaire | (n = 1) n°40 | |
| TICS-M | Telephone Interview Cognitive Status Modified | (n = 2) n°31,37 | |
| Attention/ Working memory | Digit span | (n = 6) n°3,4,11,30,37,46 | |
| STROOP test | (n = 2) n°4,11 | ||
| Executive function | Comprehension | (n = 2) n°28,49 | |
| RBANS | Repeatable Battery for Assessment of Neuropsychological Status | (n = 1) n°8 | |
| Symbol digit | (n = 3) n°16,43,46 | ||
| Trail Making Test | (n = 4) n°3,4,19,30 | ||
| Verbal fluency | (n = 12) n°3,9,11,19,25,30,35,37,38,43,46,49 | ||
| Language | BNT | Boston Naming Test | (n = 5) n°3,25,30,37,46 |
| COWA | Controlled Oral Word Association | (n = 4) n°1,3,4,11 | |
| FAS | Letter-Number Sequencing and Phonemic verbal fluency | (n = 2) n°11,25 | |
| Naming | (n = 1) n°49 | ||
| NART | American National Adult Reading test | (n = 2) n°3,46 | |
| WAIS | Wechlser Adult Intelligence Scale | (n = 6) n°3,4,9,11,19,30 | |
| Memory | BIMC | Blessed Information Memory Concentration | (n = 2) n°6,19 |
| FCSRT | Free and Cue Selective Reminding Test | (n = 2) n°3,19 | |
| FOME | Fuld Object Memory Evaluation | (n = 1) n°19 | |
| HVLT | Hopkins Verbal Learning test | (n = 3) n°11,25,43 | |
| Memory | (n = 5) n°3,16,35,46,53 | ||
| RAVLT | Rey auditory verbal learning test | (n = 3) n°1,4,30 | |
| Recall | (n = 2) n°46,49 | ||
| WMS | Wechsler Memory Scale | (n = 2) n°9,30 | |
| Visual-spatial | BVRT | Benton Visual Retention Test | (n = 1) n°9 |
| CPM | Raven’s coloured progressive matrices | (n = 2) n°19,46 | |
| JLO | Benton Judgement Line Orientation | (n = 4) n°4,25,43,46 | |
| Orientation | (n = 1) n°53 | ||
| PARR | Picture Arrangement subtest | (n = 1) n°9 | |
| ROCF | Rey-Osterrieth Complex Figure test recall | (n = 1) n°11 | |
| Visual attention | (n = 1) n°19 | ||
| Unknown | (n = 1) n°15 | ||
| Psychiatric symptoms (n = 38) | |||
| Depression / Anxiety | AS | Apathy Evaluation Scale | (n = 3) n°4,32,33 |
| BAI | Beck Anxiety Inventory | (n = 4) n°18,30,33,44 | |
| BDI | Beck Depression Inventory | (n = 9) n°5,11,18,26,30,32,33,36,44 | |
| CESD-10 | Center for Epidemiological Studies Depression Scale | (n = 3) n°24,39,47 | |
| GDS | Geriatric Depression Screening scale | (n = 17) n°1,3,4,5,7,8,10,14,20,25,26,28,34,40,43,48,50 | |
| HAM-A | Hamilton Anxiety Rating Scale | (n = 2) n°33,40 | |
| HDRS | Hamilton Depression Rating Scale | (n = 3) n°4,15,33 | |
| Leeds | Leeds anxiety and depression scale | (n = 1) n°38 | |
| SCID | Structured Clinical Interview - Depression | (n = 2) n°28,40 | |
| STAI | State Trait Anxiety Inventory | (n = 4) n°18,24,39,43 | |
| UPDRS-I | Unified Parkinson’s Disease Rating Scale - mentation behavior and mood | (n = 7) n°1,14,17,25,27,43,52 | |
| ZUNG | Zung depression scale | (n = 1) n°19 | |
| TOC | OCI-R | Obsessive-Compulsive Inventory – Revised | (n = 1) n°18 |
| QUIP | Questionnaire for impulsive-compulsive disorders in parkinson’s disease-rating scale | (n = 2) n°40,43 | |
| YBOCS | Yale-Brown obsessive-compulsive scale | (n = 1) n°33 | |
| Other | CoNeg | composite negative score | (n = 1) n°29 |
| MMPI | Multiphasic Personality Inventory | (n = 1) n°29 | |
| NPI | NeuroPsychiatric Inventory questionnaire | (n = 3) n°1,34,47 | |
| QABB | Questionnaire About Buying Behaviour | (n = 1) n°40 | |
| Rush | Rush Hallucination Inventory | (n = 1) n°21 | |
| SCS | Sexual Compulsivity Scale | (n = 1) n°40 | |
| YMRS | Young Mania Rating Scale | (n = 1) n°33 | |
| Unknown | (n = 4) n°6,15,46,49 | ||
| Activities of daily living (n = 22) | |||
| ACS | Activity Card Sort | (n = 1) n°20 | |
| ADCS-ADL | Alzheimer’s Disease Cooperative Study ADL Inventory | (n = 1) n°25 | |
| IADL | Katz Instrumental Activity of Daily Living | (n = 2) n°46,47 | |
| S&E | Schwab & England activities of daily living scale | (n = 10) n°5,14,18,26,34,38,41,43,44,53 | |
| UPDRS-II | Unified Parkinson’s Disease Rating Scale - self-evaluation of the activities of daily living | (n = 9) n°1,5,11,14,26,27,40,43,52 | |
| Unknown | (n = 3) n°15,17,51 | ||
| Sleep quality (n = 11) | |||
| Actigraphy | (n = 1) n°47 | ||
| ESS | Epworth Sleepiness Scale | (n = 4) n°5,14,38,43 | |
| FSS | Fatigue Severity Scale | (n = 1) n°40 | |
| ISI | Insomnia Severity Index | (n = 1) n°40 | |
| MSQ | Mayo clinic Sleep Questionnaire | (n = 2) n°4,30 | |
| PDSS | Parkinson’s disease sleep scale | (n = 1) n°40 | |
| PSQI | Pittsburg Sleep Quality Index | (n = 2) n°21,40 | |
| RBDSQ | REM Sleep Behaviour Disorder Screening Questionnaire | (n = 2) n°38,43 | |
| SA-SDQ | Sleep Apnea Scale of Sleep Disorders Questionnaire | (n = 1) n°40 | |
| SSS | Stanford Sleepiness Scale | (n = 1) n°40 | |
| Unknown | (n = 2) n°15,24 | ||
| Quality of life (n = 9) | |||
| EQ-5D | Euro Quality of Life 5 Dimension questionnaire | (n = 2) n°14,38 | |
| Neuro-QOL | Quality of Life in Neurological Disorders | (n = 1) n°34 | |
| NHP | Nottingham Health Profile | (n = 1) n°20 | |
| PDQUALIF | Parkinson’s Disease Quality of Life Scale | (n = 3) n°14,18,40 | |
| PDQ-39 | 39-item Parkinson’s disease quality of life | (n = 5) n°7,10,20,35,40 | |
| PIMS | Parkinson’s Impact Scale | (n = 1) n°40 | |
| SF-12 | The 12 item Short Form health survey | (n = 2) n°14,20 | |
| SF-36 | The 36 item Short Form health survey | (n = 1) n°40 | |
| SWAL-QOL | Swallow-specific quality of life | (n = 1) n°40 | |
| Autonomic symptoms (n = 7) | |||
| Bowel movement | (n = 1) n°24 | ||
| COMPASS | Composite autonomic symptom Scale | (n = 1) n°40 | |
| SCOPA-AUT | Scales for outcomes of Parkinson’s Disease – autonomic symptoms | (n = 3) n°4,5,43 | |
| Unknown | (n = 2) n°15,30 | ||
| Other (n = 20) | |||
| Olfaction | Brief-SIT | Brief Smell Identification Test | (n = 2) n°24,47 |
| 16-item sniffin’ Sticks Odour Identification test | (n = 1) n°38 | ||
| UPSIT | University of Pennsylvania Smell Identification Test | (n = 6) n°1,4,5,34,39,43 | |
| Restless legs syndrome | CH-RLSQ | Cambridge-Hopkins Restless Legs Syndrome Diagnostic Questionnaire | (n = 1) n°40 |
| IRLSSG | Instrument for the Assessment of Restless Legs Syndrome Severity | (n = 1) n°4 | |
| Caregiver | CSI | caregiver strain index | (n = 1) n°35 |
| deJong-Gierveld Loneliness Scale | (n = 1) n°47 | ||
| MCSI | Multidimensional Caregiver Strain Index | (n = 1) n°35 | |
| Caregiver interview | (n = 1) n°21 | ||
| Other | Agonal state questionnaire | (n = 1) n°51 | |
| CGI | Clinical Global Impression scale | (n = 1) n°38 | |
| CIRS | Chronic Illness Resource Survey | (n = 1) n°20 | |
| GHS | Global Health Score | (n = 1) n°8 | |
| GIS | Global Impression Scale | (n = 1) n°51 | |
| Howard-Dohlman device | (n = 1) n°48 | ||
| MNA | Mini Nutritional Assessment | (n = 1) n°40 | |
| MOS | Medical outcome study | (n = 1) n°20 | |
| MSSSS | Medical Outcomes Study Social Support Scale | (n = 1) n°28 | |
| Pain | (n = 1) n°40 | ||
| PASE | Physical Activity Scale for the Elderly | (n = 3) n°7,10,43 | |
| SRRS | Social Readjustment Rating scale | (n = 1) n°28 | |
| SSCI | Stigma Scale for Chronic Illness | (n = 1) n°20 | |
| Tremor rating | (n = 1) n°4 | ||
| Visual acuity | (n = 1) n°48 | ||
| Unknown | (n = 1) n°15 | ||
Most sources assessed motor and neurological functions (87%), cognition (77%) and psychiatric symptoms (72%). Activity level (42%), sleep quality (21%), quality of life (17%) and autonomic symptoms (13%) were reported to a lesser extent. The most commonly measurements used to assess motor and neurological symptoms were the Unified Parkinson’s Disease Rating Scale part III (UPDRS-III, 77% of included data sources) and the Hoehn and Yahr scale (H&Y, 57% of included data sources)(Table 4). To evaluate the cognitive impairment, the Mini Mental State Examination (MMSE, 57%) was the most frequent. Those most frequently used to assess psychiatric symptoms were the Geriatric Depression Scale (GDS, 32%) and Beck Depression Inventory (BDI, 15%). For the other dimensions, the most commonly used measurements were: the Epworth Sleepiness Scale (ESS, 8%, for sleep), the Schwab and England (S&E, 19%, for activities of daily living), the 39-item Parkinson’s disease Quality of life (PDQ-39, 9%, for the quality of life) and the autonomic part of the Scales for outcomes of Parkinson’s disease (SCOPA-AUT, 6%, for autonomic symptoms). In absolute frequency, the use of ESS, PDQ-39 and SCOPA-AUT is very low, even if they were the most frequently used measurements in their dimension.
The analysis reveals some interesting differences between sources on the number of measurements applied by dimension. Some sources evaluate only one dimension (source n°13) when others evaluate seven dimensions (source n°43). Completed sources have more frequent measurements of motor and neurological symptoms (92% vs 75%), psychiatric symptoms (76% vs 63%) and activities of daily living (43% vs 38%) than ongoing sources. US sources evaluate more frequently the cognitive impairment then international sources (86% vs 45%) but less frequently all the other dimensions. “Generic” sources evaluate three dimensions more frequently than specific sources including only Parkinsonian patients: cognition (86% vs 68%), sleep (32% vs 8%) and autonomic symptoms (25% vs 0%).
Lastly, the frequencies of these assessments are dependent on the primary objective of the sources but with an important overlap: 100% of the sources investigating motor symptoms used measurements of motor symptoms and mainly the UPDRS-III, but they also frequently assessed cognition (88%), sleep (25%) and quality of life (25%). The sources investigating non-motor symptoms frequently assessed cognition (82%), psychiatric symptoms (88%) most of the time with, respectively, the GDS (41%) and the MMSE (65%). The two genetic sources have several patient reported outcomes and they both measured motor and psychiatric symptoms.
Some measurements were used more often for some above-mentioned objectives. While the GDS and the UPDRS-III were used specifically in sources investigating, respectively, the non-motor symptoms and the motor symptoms as a primary objective, the BDI and the H&Y were used in sources investigating the other objectives.
Discussion
A large number of longitudinal real world data sources for PD have been identified. There is no consistency of the dimensions assessed, nor of the measurements used across sources, reflecting the absence of harmonization on the optimal choice of measurements.
There are a number of issues with collecting real world data such as limited size of the databases [1], inability to accurately determine specific outcomes [62], and more chance of bias and confounding factors [5]. Nevertheless, they have an important role to play in the evaluation of epidemiology, burden of disease and treatments patterns [6]; and in assisting health-care decision-makers, especially related to coverage and payment decisions [63]. In this context, a harmonization seems necessary. These results are quite consistent with those observed in Europe where a “consensus on domains incorporated in different studies [was observed] with a substantial variability in the choice of the evaluation method” [4]. There are a number of possible explanations for this absence of harmonization and some of them are discussed here.
First of all, some dimensions are broad. In consequence many measurements are available according to each source objective, design and population. This heterogeneity probably reflects both the absence of harmonization and the complexity of the evaluation of a dimension like cognition [64]. A single measurement cannot assess all necessary information. For example, the combination of patient reported outcomes and medical reported outcomes can be very informative and complement one another. In a consistent manner, the combination of Parkinson specific and generic measurements can be a necessity especially for “generic” data sources including not only Parkinsonian patients. In another example, while the objectives of the UPDRS-III and the H&Y (or of the GDS and the BDI) are close, the difference of their use according to the study primary objective of the source seems more linked to the investigator choice than to the suitability of the measurement.
Secondly, PD is characterized by several initial system disorders and treatment complications [65]. To date, motor subtyping has dominated the landscape of PD research but non-motor dimensions evaluations are increasing [9, 66], and thus the number of dimensions to evaluate. For non-motor dimensions, some have validated measurements such as psychiatry [67], activity disability [7], sleep [68] or quality of life [69]; but others have no clear review of validated and used scales [4]. Among the psychiatric scales, the two most frequently used were the GDS and the BDI. This finding highlights the well-known relationship between PD and depression, and the fact that when validated scales [70] are available, a harmonization of practice is observed. The lack of evaluation and validation of the measurements in PD is probably partly a source of such an heterogeneity.
Thirdly, clinical research purposes and outcomes are in permanent evolution over time [71, 72], as highlighted by the many differences between completed and ongoing sources. New trends are not well covered right now, either due to lack of measurements or due to lack of capture (i.e. utilization of available measurements in databases). Among the most important of those are the genetic testing, the caregiver burden and the costs. The important development of genetic testing has come in the last few years, with an increase of the mutations and treatment discoveries such as LRRK2 and its kinase inhibitors. But research is necessary to understand the role of genetic mutations in PD [73]. Sources based on caregiver burden and relevant validated measurements are very limited [7]. But the interest for these data is growing with the recognition of their physical, emotional and economic burden [74]. The only data source identified as measuring healthcare costs associated with PD was ongoing. It probably reflects both the recent growing interest of health economic evaluation and the fact that this type of study is more often conducted in automated healthcare databases [75].
Fourthly, there is a possible improvement of the access to the data source details. Given information is fragmented between different sources of information and study protocols or outcomes lists are not always available. In consequence identifying and gathering this information to produce an integrated view can be really difficult.
Finally, the variability of our results is greater than in the European study. This may be because the classification is based on dimensions assessing mostly symptoms, 5 out of 8 dimensions. This classification probably more appropriate for data sources with a primary objective of treatment evaluation (e.g. open-label extension), which are a minority of the included sources. The classification may not be as applicable to assess other data sources focused on the evaluation of burden. Real world evidence collection is done for various purposes and such a restricted classification can lead to ambiguous conclusions. It can lead to a perception of consensus while actually missing important aspects such as burden, function or complications of treatments.
Our study has several limitations. First of all, only one reader has conducted the record selection and the data extraction unlike systematic reviews. Nevertheless, the search methods identified a large number of PD data sources for extraction and comparison. No contact was established with investigators of the included studies to confirm data extraction results. To address this issue, a second step has been performed after the data extraction from the publications, to update and complete the published information with all other available sources. At risk/prodromal cohorts have not been separated from clinical PD cohorts, but the distinction between these two subgroups has recently been described as artificial [4].
Our study has several strengths. It is the first review of existing real world longitudinal data sources on PD in USA to our knowledge. Moreover, it was performed with broad research criteria and without any limitation on language, type of publication or type of measurements. This review creates an integrated view and should assist investigators and clinicians to identify and optimize the measurements that best match with their objectives and the already existing data sources.
Conclusion
In conclusion, many longitudinal real world data sources on PD exist. Different types of measurements have been used over time. To allow comparison and pooling of these multiple data sources, it will be essential to harmonize practices in terms of types of measurements.
Acknowledgements
Highly appreciated is also the support of Sandrine Thoreau for assisting with the search strategy.
Funding
The study was funded by Lundbeck SAS. The funding source, beyond the employees involved as authors, did not participate in the design of the study; collection, analysis nor interpretation of the data; nor the writing of the manuscript.
Availability of data and materials
Not applicable.
Abbreviations
- BDI
Beck Depression Inventory
- ESS
Epworth Sleepiness Scale
- FDA
Food and Drug Administration
- GDS
Geriatric Depression Scale
- H&Y
Hoehn and Yahr scale
- MMSE
Mini Mental State Examination
- PD
Parkinson’s disease
- PDQ-39
39-item Parkinson’s disease Quality of life
- S&E
Schwab and England
- SCOPA-AUT
autonomic part of the Scales for outcomes of Parkinson’s disease
- UPDRS-III
Unified Parkinson’s Disease Rating Scale part III
- USA
United States of America
Appendix 1
Search strategy.
Equation 1: Disease selection
(EMB.EXACT(“Parkinson disease”) OR MESH.EXACT(“Parkinson Disease”) OR ab(“Parkinson*”)
OR ti(“Parkinson*”) OR EMB.EXACT(“antiparkinson agent”) OR MESH.EXACT(“Antiparkinson Agents”)) AND (human(yes) AND human(yes)).
Equation 2: Disease exclusion
(MESH.EXACT(“Parkinson Disease, Postencephalitic”) OR MESH.EXACT(“Parkinson Disease, Secondary”) OR EMB.EXACT(“Wolff Parkinson White syndrome”) OR EMB.EXACT(“experimental parkinsonism”) OR EMB.EXACT(“parkinsonism”) OR EMB.EXACT(“MPTPinduced parkinsonism”)) AND (human(yes) AND human(yes))
Equation 3: Study type selection
((EMB.EXACT(“register”) OR EMB.EXACT(“long term care”) OR EMB.EXACT(“retrospective study”) OR EMB.EXACT(“prospective study”) OR EMB.EXACT(“cohort analysis”) OR EMB.EXACT(“clinical practice”) OR EMB.EXACT(“longitudinal study”)) OR (MESH.EXACT(“Cohort Studies”) OR MESH.EXACT(“Registries”) OR MESH.EXACT(“Longitudinal Studies”) OR MESH.EXACT(“Long-Term Care”) OR MESH.EXACT (“Retrospective Studies”) OR MESH.EXACT(“Prospective Studies”) OR MESH.EXACT(“Practice Patterns, Physicians’”))) OR (((longitudinal OR retrospective OR prospective OR cohort OR “follow up” OR observational OR naturalistic OR “cross*sectional” OR epidemio* OR database) NEAR/1 (study OR studies)) OR “cohort analysis” OR “registry” OR “register*” OR “real-world” OR “treatment pattern*” OR “survey*” OR “medical records” OR “population-correlation” OR “population-based” OR “population-level”)
Equation 4: Study type exclusion
((MESH.EXACT(“Case-Control Studies”) OR MESH.EXACT(“Controlled Before-After Studies”) OR.
MESH.EXACT(“Feasibility Studies”) OR MESH.EXACT(“Clinical Trial”) OR MESH.EXACT(“Organizational Case Studies”) OR MESH.EXACT(“Evaluation Studies”)) OR (EMB.EXACT (“major clinical study”) OR EMB.EXACT(“in vivo study”) OR EMB.EXACT(“evaluation study”) OR EMB.EXACT(“in vitro study”) OR EMB.EXACT(“first in human study”) OR EMB.EXACT(“experimental study”) OR EMB.EXACT(“case study”) OR EMB.EXACT(“clinical study”) OR EMB.EXACT(“intervention study”) OR EMB.EXACT(“case control study”))).
Equation 5: Combination of the previous equation
(Equation 1 NOT Eq. 2) AND (Eq. 3 NOT Eq. 4)
Equation 6: Country selection
GI(“United States*”) OR ti(“America*”) OR ab(“America *”) OR ab(“usa”) OR ti(“usa”) OR ab(“us”) OR ti(“us”) OR ab(“u.s”) OR ti(“u.s”).
Equation 7: Application of the combination equation to the country of interest
Equation 6 AND Eq. 6
Appendix 2
List of outcomes extracted.
Acronym
○Full name
○Country (−ies)
○Database size (total number of patients and number of Parkinsonian patients)
○Database type
○Name of investigator (corresponding author of the publication, reference person)
○Funder(s)
○Medical imaging
○Scales list
○Scales dimension 1: Activities of daily living
○Scales dimension 2: Cognition
○Scales dimension 3: Motor or neurologic symptoms
○Scales dimension 4: Psychiatric symptoms
○Scales dimension 5: Sleep quality
○Scales dimension 6: Quality of life
○Scales dimension 7: Autonomic symptoms
○Scales dimension 8: Other
○Healthcare costs
○Genetics
○Comorbidities
○Current medications
○Severity of disease
○Caregiver burden
○Date of beginning of the study
○Date of end of the study
○Duration of follow-up
○Planned follow-ups
○Particular inclusion criteria
Authors’ contributions
AT: Research project execution, statistical analysis execution, manuscript writing, review and critique. LJ: Research project conception and organization, statistical analysis review and critique, manuscript review and critique. LI: Research project conception and organization, statistical analysis review and critique, manuscript review and critique. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
LJ is a current employee and AT was a resident in Lundbeck SAS and LI was an employee of Lundbeck SAS at the time the research was carried out.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Audrey Tanguy, Email: audrey.tanguy07@gmail.com.
Linus Jönsson, Email: LIJS@lundbeck.com.
Lianna Ishihara, Phone: +33 1 79 41 29 22, Email: liannaish@yahoo.com.
References
- 1.Kowal SL, Dall TM, Chakrabarti R, Storm MV, Jain A. The current and projected economic burden of Parkinson’s disease in the United States. Mov Disord. 2013;28:311–318. doi: 10.1002/mds.25292. [DOI] [PubMed] [Google Scholar]
- 2.Use of Real-World Evidence to Support Regulatory Decision-Making for Medical Devices: FDA Draft Guidance for Industry and Staff. Food Drug Administration. http://www.fda.gov/ucm/groups/fdagov-public/@fdagov-meddev-gen/documents/document/ucm513027.pdf. Accessed 29 Nov 2017.
- 3.Bot BM, Suver C, Neto EC, et al. The mPower study, Parkinson disease mobile data collected using ResearchKit. Scientific Data. 2016;3:160011. doi: 10.1038/sdata.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lerche S, Liepelt-Scarfone I, Alves G, et al. Methods in Neuroepidemiology characterization of European longitudinal cohort studies in Parkinson’s disease – report of the JPND working group BioLoc-PD. Neuroepidemiology. 2015;45:282–297. doi: 10.1159/000439221. [DOI] [PubMed] [Google Scholar]
- 5.Mahajan R. Real world data: additional source for making clinical decisions. Int J Appl Basic Med Res. 2015; doi:10.4103/2229-516X.157148. [DOI] [PMC free article] [PubMed]
- 6.Annemans L, Aristides M, Kubin M. Real life data: a growing need. ISPOR Connections. http://www.ispor.org/news/articles/oct07/rld.asp. Accessed 29 Nov 2017.
- 7.Shulman LM, Armstrong M, Ellis T, et al. Disability rating scales in Parkinson’s disease: critique and recommendations. Mov Disord. 2016;31:1455–1465. doi: 10.1002/mds.26649. [DOI] [PubMed] [Google Scholar]
- 8.Doty RL. Olfaction in Parkinson’s disease and related disorders. Neurobiol Dis. 2012;46:527–552. doi: 10.1016/j.nbd.2011.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravina B, Tanner C, Dieuliis D, et al. A longitudinal program for biomarker development in Parkinson's disease: a feasibility study. Mov Disord. 2009;24(14):2081–2090. doi: 10.1002/mds.22690. [DOI] [PubMed] [Google Scholar]
- 10.Tang CC, Poston KL, Dhawan V, et al. Abnormalities in metabolic network activity precede the onset of motor symptoms in Parkinson's disease. J Neurosci. 2010;30(3):1049–1056. doi: 10.1523/JNEUROSCI.4188-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomperts SN, Locascio JJ, Rentz D, et al. Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia. Neurology. 2013;80(1):85–91. doi: 10.1212/WNL.0b013e31827b1a07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caviness JN, Hentz JG, Belden CM, et al. Longitudinal EEG changes correlate with cognitive measure deterioration in Parkinson's disease. J Parkinsons Dis. 2015;5(1):117–124. doi: 10.3233/JPD-140480. [DOI] [PubMed] [Google Scholar]
- 13.Alcalay RN, Mirelman A, Saunders-Pullman R, et al. Parkinson disease phenotype in Ashkenazi Jews with and without LRRK2 G2019S mutations. Mov Disord. 2013;28(14):1966–1971. doi: 10.1002/mds.25647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Brien RJ, Resnick SM, Zonderman AB, et al. Neuropathologic studies of the Baltimore longitudinal study of aging (BLSA) J Alzheimers Dis. 2009;18(3):665–675. doi: 10.3233/JAD-2009-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duncan RP, Leddy AL, Cavanaugh JT, et al. Detecting and predicting balance decline in Parkinson disease: a prospective cohort study. J Parkinsons Dis. 2015;5(1):131–139. doi: 10.3233/JPD-140478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahoney JR, Verghese J, Holtzer R, et al. The evolution of mild parkinsonian signs in aging. J Neurol. 2014;261(10):1922–1928. doi: 10.1007/s00415-014-7442-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bohnen NI, Koeppe RA, Minoshima S, et al. Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study. J Nucl Med. 2011;52(6):848–855. doi: 10.2967/jnumed.111.089946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dibble LE, Cavanaugh JT, Earhart GM, et al. Charting the progression of disability in Parkinson disease: study protocol for a prospective longitudinal cohort study. BMC Neurol. 2010;10:110. doi: 10.1186/1471-2377-10-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Suilleabhain PE, Oberle R, Bartis C, et al. Clinical course in Parkinson's disease with elevated homocysteine. Parkinsonism Relat Disord. 2006;12(2):103–107. doi: 10.1016/j.parkreldis.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Evatt ML, Delong MR, Khazai N, et al. Prevalence of vitamin d insufficiency in patients with Parkinson disease and Alzheimer disease. Arch Neurol. 2008;65(10):1348–1352. doi: 10.1001/archneur.65.10.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duncan RP, Leddy AL, Cavanaugh JT, et al. Comparative utility of the BESTest, mini-BESTest, and brief-BESTest for predicting falls in individuals with Parkinson disease: a cohort study. Phys Ther. 2013;93(4):542–550. doi: 10.2522/ptj.20120302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holloway R, Marek K, Biglan K, et al. Long-term effect of initiating pramipexole vs levodopa in early Parkinson disease. Arch Neurol. 2009;66(5):563–570. doi: 10.1001/archneurol.2009.32. [DOI] [PubMed] [Google Scholar]
- 23.Golbe LI, Di Iorio G, Sanges G, et al. Clinical genetic analysis of Parkinson's disease in the Contursi kindred. Ann Neurol. 1996;40(5):767–775. doi: 10.1002/ana.410400513. [DOI] [PubMed] [Google Scholar]
- 24.Liu C, Cholerton B, Shi M, et al. CSF tau and tau/Aβ42 predict cognitive decline in Parkinson's disease. Parkinsonism Relat Disord. 2015;21(3):271–276. doi: 10.1016/j.parkreldis.2014.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jasinska-Myga B, Putzke JD, Wider C, et al. Depression in Parkinson's disease. Can J Neurol Sci. 2010;37(1):61–66. doi: 10.1017/S0317167100009665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rabinak CA, Nirenberg MJ. Dopamine agonist withdrawal syndrome in Parkinson disease. Arch Neurol. 2010;67(1):58–63. doi: 10.1001/archneurol.2009.294. [DOI] [PubMed] [Google Scholar]
- 27.San Luciano M, Lipton RB, Wang C, et al. Clinical expression of LRRK2 G2019S mutations in the elderly. Mov Disord. 2010;25(15):2571–2576. doi: 10.1002/mds.23330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tickle-Degnen L, Saint-Hilaire M, Thomas CA, et al. Emergence and evolution of social self-management of Parkinson's disease: study protocol for a 3-year prospective cohort study. BMC Neurol. 2014;14:95. doi: 10.1186/1471-2377-14-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goetz CG, Ouyang B, Negron A, et al. Hallucinations and sleep disorders in PD: ten-year prospective longitudinal study. Neurology. 2010;75(20):1773–1779. doi: 10.1212/WNL.0b013e3181fd6158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Logroscino G, Sesso HD, Paffenbarger RS, Jr, et al. Physical activity and risk of Parkinson's disease: a prospective cohort study. J Neurol Neurosurg Psychiatry. 2006;77(12):1318–1322. doi: 10.1136/jnnp.2006.097170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen H, Zhang SM, Schwarzschild MA, et al. Survival of Parkinson's disease patients in a large prospective cohort of male health professionals. Mov Disord. 2006;21(7):1002–1007. doi: 10.1002/mds.20881. [DOI] [PubMed] [Google Scholar]
- 32.Wong KT, Grove JS, Grandinetti A, et al. Association of fibrinogen with Parkinson disease in elderly Japanese-American men: a prospective study. Neuroepidemiology. 2010;34(1):50–54. doi: 10.1159/000260070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pigott K, Rick J, Xie SX, et al. Longitudinal study of normal cognition in Parkinson disease. Neurology. 2015;85(15):1276–1282. doi: 10.1212/WNL.0000000000002001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liang GS, Chou KL, Baltuch GH, et al. Long-term outcomes of bilateral subthalamic nucleus stimulation in patients with advanced Parkinson's disease. Stereotact Funct Neurosurg. 2006;84(5-6):221–227. doi: 10.1159/000096495. [DOI] [PubMed] [Google Scholar]
- 35.Jasinska-Myga B, Heckman MG, Wider C, et al. Loss of ability to work and ability to live independently in Parkinson's disease. Parkinsonism Relat Disord. 2012;18(2):130–135. doi: 10.1016/j.parkreldis.2011.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rod NH, Bordelon Y, Thompson A, et al. Major life events and development of major depression in Parkinson's disease patients. Eur J Neurol. 2013;20(4):663–670. doi: 10.1111/ene.12019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bower JH, Grossardt BR, Maraganore DM, et al. Anxious personality predicts an increased risk of Parkinson's disease. Mov Disord. 2010;25(13):2105–13. doi: 10.1002/mds.23230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts RO, Geda YE, Knopman DS, et al. The Mayo Clinic study of aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30(1):58–69. doi: 10.1159/000115751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Markopoulou K, Biernacka JM, Armasu SM, et al. Does α-synuclein have a dual and opposing effect in preclinical vs. clinical Parkinson's disease? Parkinsonism Relat Disord. 2014;20(6):584–589. doi: 10.1016/j.parkreldis.2014.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zahodne LB, Marsiske M, Okun MS, et al. Mood and motor trajectories in Parkinson's disease: multivariate latent growth curve modeling. Neuropsychology. 2012;26(1):71–80. doi: 10.1037/a0025119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okun MS, Wu SS, Fayad S, et al. Acute and chronic mood and apathy outcomes from a randomized study of unilateral STN and GPi DBS. PLoS One. 2014;9(12):e114140. doi: 10.1371/journal.pone.0114140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cholerton BA, Zabetian CP, Quinn JF, et al. Pacific Northwest Udall center of excellence clinical consortium: study design and baseline cohort characteristics. J Parkinsons Dis. 2013;3(2):205–214. doi: 10.3233/JPD-130189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Okun MS, Siderowf A, Nutt JG, et al. Piloting the NPF data-driven quality improvement initiative. Parkinsonism Relat Disord. 2010;16(8):517–521. doi: 10.1016/j.parkreldis.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 44.Kay DM, Zabetian CP, Factor SA, et al. Parkinson's disease and LRRK2: frequency of a common mutation in U.S. movement disorder clinics. Mov Disord. 2006;21(4):519–523. doi: 10.1002/mds.20751. [DOI] [PubMed] [Google Scholar]
- 45.Chen H, Schernhammer E, Schwarzschild MA, et al. A prospective study of night shift work, sleep duration, and risk of Parkinson's disease. Am J Epidemiol. 2006;163(8):726–730. doi: 10.1093/aje/kwj096. [DOI] [PubMed] [Google Scholar]
- 46.Szewczyk-Krolikowski K, Menke RA, Rolinski M, et al. Functional connectivity in the basal ganglia network differentiates PD patients from controls. Neurology. 2014;83(3):208–214. doi: 10.1212/WNL.0000000000000592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Qiang JK, Wong YC, Siderowf A, et al. Plasma apolipoprotein A1 as a biomarker for Parkinson disease. Ann Neurol. 2013;74(1):119–127. doi: 10.1002/ana.23872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ofori E, Pasternak O, Planetta PJ, et al. Increased free water in the substantia nigra of Parkinson's disease: a single-site and multi-site study. Neurobiol Aging. 2015;36(2):1097–1104. doi: 10.1016/j.neurobiolaging.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Swanson CR, Li K, Unger TL, et al. Lower plasma apolipoprotein A1 levels are found in Parkinson's disease and associate with apolipoprotein A1 genotype. Mov Disord. 2015;30(6):805–812. doi: 10.1002/mds.26022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ko JH, Mure H, Tang CC, et al. Parkinson's disease: increased motor network activity in the absence of movement. J Neurosci. 2013;33(10):4540–4549. doi: 10.1523/JNEUROSCI.5024-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chahine LM, Xie SX, Simuni T, et al. Longitudinal changes in cognition in early Parkinson's disease patients with REM sleep behavior disorder. Parkinsonism Relat Disord. 2016;27:102–106. doi: 10.1016/j.parkreldis.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bastiaens J, Dorfman BJ, Christos PJ, et al. Prospective cohort study of impulse control disorders in Parkinson's disease. Mov Disord. 2013;28(3):327–333. doi: 10.1002/mds.25291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gallagher CL, Oakes TR, Johnson SC, et al. Rate of 6-[18F]fluorodopa uptake decline in striatal subregions in Parkinson's disease. Mov Disord. 2011;26(4):614–620. doi: 10.1002/mds.23503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bennett DA, Schneider JA, Arvanitakis Z, et al. Overview and findings from the religious orders study. Curr Alzheimer Res. 2012;9(6):628–645. doi: 10.2174/156720512801322573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bennett DA, Schneider JA, Buchman AS, et al. Overview and findings from the rush memory and aging project. Curr Alzheimer Res. 2012;9(6):646–663. doi: 10.2174/156720512801322663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneider JL, Fink HA, Ewing SK, et al. The association of Parkinson's disease with bone mineral density and fracture in older women. Osteoporos Int. 2008;19(7):1093–1097. doi: 10.1007/s00198-008-0583-5. [DOI] [PubMed] [Google Scholar]
- 57.Aarsland D, Kvaløy JT, Andersen K, et al. The effect of age of onset of PD on risk of dementia. J Neurol. 2007;254(1):38–45. doi: 10.1007/s00415-006-0234-8. [DOI] [PubMed] [Google Scholar]
- 58.Ritz B, Rhodes SL, Bordelon Y, et al. α-Synuclein genetic variants predict faster motor symptom progression in idiopathic Parkinson disease. PLoS One. 2012;7(5):e36199. doi: 10.1371/journal.pone.0036199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Papapetropoulos S, Mash DC. Motor fluctuations and dyskinesias in advanced/end stage Parkinson's disease: a study from a population of brain donors. J Neural Transm (Vienna) 2007;114(3):341–345. doi: 10.1007/s00702-006-0603-6. [DOI] [PubMed] [Google Scholar]
- 60.Harrison MB, Wylie SA, Frysinger RC, et al. UPDRS activity of daily living score as a marker of Parkinson's disease progression. Mov Disord. 2009;24(2):224–230. doi: 10.1002/mds.22335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Louis ED, Tang MX, Schupf N. Mild parkinsonian signs are associated with increased risk of dementia in a prospective, population-based study of elders. Mov Disord. 2010;25(2):172–178. doi: 10.1002/mds.22943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Marras C, Chaudhuri KR. Nonmotor features of Parkinson’s disease subtypes. Mov Disord. 2016;31(8):1095–1102. doi: 10.1002/mds.26510. [DOI] [PubMed] [Google Scholar]
- 63.Garrison LP, Jr, Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR real-world data task force report. Value Health. 2007;10(5):326–335. doi: 10.1111/j.1524-4733.2007.00186.x. [DOI] [PubMed] [Google Scholar]
- 64.Litvan I, Goldman JG, Tröster AI, et al. Diagnostic criteria for mild cognitive impairment in Parkinson's disease: Movement Disorder Society task force guidelines. Mov Disord. 2012;27(3):349–356. doi: 10.1002/mds.24893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.De Virgilio A, Greco A, Fabbrini G, et al. Parkinson's disease: autoimmunity and neuroinflammation. Autoimmun Rev. 2016;15(10):1005–1011. doi: 10.1016/j.autrev.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 66.Sagna A, Gallo JJ, Pontone GM. Systematic review of factors associated with depression and anxiety disorders among older adults with Parkinson's disease. Parkinsonism Relat Disord. 2014;20(7):708–715. doi: 10.1016/j.parkreldis.2014.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martinez-Martin P, Leentjens AF, de Pedro-Cuesta J, Chaudhuri KR, Schrag AE, Weintraub D. Accuracy of screening instruments for detection of neuropsychiatric syndromes in Parkinson's disease. Mov Disord. 2016;31(3):270–279. doi: 10.1002/mds.26522. [DOI] [PubMed] [Google Scholar]
- 68.Zea-Sevilla MA, Martinez-Martin P. Rating scales and questionnaires for assessment of sleep disorders in Parkinson's disease: what they inform about? J Neural Transm. 2014;121:33. doi: 10.1007/s00702-014-1217-z. [DOI] [PubMed] [Google Scholar]
- 69.Martinez-Martin P, Jeukens-Visser M, Lyons KE, et al. Health-related quality-of-life scales in Parkinson's disease: critique and recommendations. Mov Disord. 2011;26(13):2371–2380. doi: 10.1002/mds.23834. [DOI] [PubMed] [Google Scholar]
- 70.Goodarzi Z, Mrklas KJ, Roberts DJ, Jette N, Pringsheim T, Holroyd-Leduc J. Detecting depression in Parkinson disease: a systematic review and meta-analysis. Neurology. 2016;87(4):426–437. doi: 10.1212/WNL.0000000000002898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Engler K, Lessard D, Lebouché B. A review of HIV-specific patient-reported outcome measures. Patient. 2016; doi:10.1007/s40271-016-0195-7. [DOI] [PubMed]
- 72.Goldman J, Weintraub D. Advances in the treatment of cognitive impairment in Parkinson’s disease. Mov Disord. 2015;30(11):1471–1489. doi: 10.1002/mds.26352. [DOI] [PubMed] [Google Scholar]
- 73.Wallings R, Manzoni C, Bandopadhyay R. Cellular processes associated with LRRK2 function and dysfunction. FEBS J. 2015;282(15):2806–2826. doi: 10.1111/febs.13305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Boland D, Stacy M. The economic and quality of life burden associated with Parkinson’s disease: a focus on symptoms. Am J Manag Care. 2012;18(7):S168–S175. [PubMed] [Google Scholar]
- 75.Noyes K, Liu H, Temkin-Greener H. Cost of caring for Medicare beneficiaries with Parkinson's disease: impact of the CMS-HCC risk-adjustment model. Dis Manag. 2006;9(6):339–348. doi: 10.1089/dis.2006.9.339. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


