Abstract
Background
Low‐density lipoprotein cholesterol (LDL‐C) control is higher among insured than uninsured adults, but data on time trends and contributing factors are incomplete and important for improving health equity.
Methods and Results
Awareness, treatment, and control of elevated LDL‐C were compared among insured versus uninsured and publicly versus privately insured adults, aged 21 to 64 years, in National Health and Nutrition Examination Surveys from 2001 to 2004, 2005 to 2008, and 2009 to 2012 using Adult Treatment Panel‐3 criteria. Compared with insured adults, uninsured adults were younger; were more often minority; reported lower incomes, less education, and fewer healthcare encounters; and had lower awareness and treatment of elevated LDL‐C (P<0.0001). LDL‐C control was higher among insured than uninsured adults in 2001 to 2004 (mean±SEM, 21.4±1.6% versus 10.5±2.6%; P<0.01), and the gap widened by 2009 to 2012 (35.1±1.9% versus 11.3±2.2%; P<0.0001). Despite more minorities (P<0.01), greater poverty, and less education (P<0.001), publicly insured adults had more healthcare visits/year than privately insured adults (P<0.001) and similar awareness, treatment, and control of LDL‐C from 2001 to 2012. In multivariable logistic regression, significant positive predictors of cholesterol awareness, treatment, and control included more frequent health care (strongest), increasing age, private healthcare insurance versus uninsured, and hypertension. Public insurance (versus uninsured) was a significant positive predictor of LDL‐C control, whereas income <200% versus ≥200% of federal poverty was a significant negative predictor.
Conclusions
LDL‐C control improved similarly over time in publicly and privately insured adults but was stagnant among the uninsured. Healthcare insurance largely addresses socioeconomic barriers to effective LDL‐C management, yet poverty retains an independent adverse effect.
Keywords: adult treatment panel‐3, cholesterol, health disparities, healthcare insurance
Subject Categories: Cardiovascular Disease, Epidemiology, Lipids and Cholesterol, Risk Factors, Primary Prevention
Clinical Perspective
What Is New?
Using Adult Treatment Panel‐3 criteria, treatment and control of elevated low‐density lipoprotein cholesterol improved similarly in adults with private and public insurance between 2001‐2004 and 2009‐2012, despite more minorities, lower incomes, and less education in the publicly insured group.
Treatment and control of elevated low‐density lipoprotein cholesterol did not improve among uninsured adults, despite a large increase in awareness, because the absolute disparity in control versus insured adults doubled from 10.9% to 23.8%.
What Are the Clinical Implications?
Less frequent health care emerged as more important than race‐ethnicity, income, and education in accounting for differences in low‐density lipoprotein cholesterol between insured and uninsured adults.
Providing private or public healthcare insurance that covers preventive healthcare services to uninsured adults emerges as an important variable in reducing and eliminating the rapidly growing gap in low‐density lipoprotein cholesterol control between insured and uninsured adults.
Treatment and control of hypercholesterolemia offer a major opportunity for preventing heart disease and stroke.1, 2, 3, 4, 5 In fact, estimates suggest that >240 000 myocardial infarctions and strokes could be prevented annually if all 44.8 million statin‐eligible but untreated US adults received statins, as recommended in the 2013 Cholesterol Guideline.1
Several reports indicate that income, healthcare insurance, frequency of health care, and minority race‐ethnicity status are strongly related to diagnosis, treatment, and control of hypercholesterolemia.6, 7, 8, 9, 10, 11 Of the variables affecting medical management of hypercholesterolemia, healthcare insurance emerges as more amenable to change than income or race‐ethnicity. Moreover, evidence suggests that higher incomes do not overcome lack of insurance in obtaining healthcare services for cardiovascular risk reduction.12 One estimate indicated there would be 811 000 fewer individuals with undiagnosed hypercholesterolemia and 241 000 fewer individuals with uncontrolled hypercholesterolemia if the uninsured population were reduced 50%.13
Cross‐sectional studies found that large gaps in the treatment and control of cardiovascular risk factors, including diabetes mellitus, hypercholesterolemia, and hypertension, in pre‐Medicare aged adults virtually disappear with Medicare insurance.5, 14, 15 Moreover, individuals with public and private healthcare insurance attained similar rates of awareness, treatment, and control of hypertension, despite the fact that those with public insurance, like the uninsured, were more often minority and had lower incomes and less education.16
Control of atherogenic low‐density lipoprotein cholesterol (LDL‐C) has improved over time,9, 11 and disparities in cholesterol screening between uninsured and publicly insured adults have been narrowing.17 Although greater equity in screening is relevant, the more important outcome is whether disparities in LDL‐C treatment and control between insured and uninsured are closing. The literature is less clear on this key point. In this report, differences in awareness, treatment, and control of hypercholesterolemia were assessed between insured and uninsured adults and between adults with public and private healthcare insurance from 2001 to 2012. The clinical epidemiological features of hypercholesterolemia were assessed using the Adult Treatment Panel‐3 guideline in effect during this time period.18 To inform potential interventions to improve current guideline‐recommended LDL‐C management,1 the independent effects of healthcare insurance, demographic, socioeconomic, educational, and healthcare variables were examined.
Methods
NHANES (The National Health and Nutrition Examination Surveys) are conducted by the National Center for Health Statistics.3, 5, 6, 8, 9, 10, 11 A representative sample is obtained of the US civilian noninstitutionalized population with oversampling of Hispanic and black individuals to allow for meaningful comparisons with whites. All adults participating in NHANES provided written informed consent, approved by the National Center for Health Statistics.
Participants included adults, aged 21 to 64 years, in NHANES, 2001 to 2012, who had fasting laboratory samples. Triglyceride values, required to calculate LDL‐C (in mg/dL), a key variable in this analysis, are only available from fasting samples.
Definitions
Race‐ethnicity was determined by self‐report and designated as non‐Hispanic white (white), non‐Hispanic black (black), Hispanic ethnicity, and other race‐ethnicity groups. The individual groups in the other category were not analyzed separately, given small sample sizes.
Medical visits were defined by response to “How many times did you receive health care during the past year?” Responses were classified into 0 to 1, 2 to 3, and ≥4 visits/year.
Healthcare insurance during the past 12 months was defined by response to “Are you covered by health insurance or some other kind of healthcare plan?” Private insurance was defined by response to “Are you covered by private insurance?” or “Are you covered by Medi‐Gap?” Medicaid insurance was defined by response to “Are you covered by Medicaid?” Medicare insurance was defined by response to “Are you covered by Medicare?” Other government insurance was defined by responses to “Are you covered by: Civilian Health and Medical Program of the Uniformed Services/Veterans Affairs/military health care?,” “Indian Health Service?,” “state‐sponsored health plan?,” or “other government insurance?” Public insurance includes Medicaid, Medicare, and other government insurance. Uninsured individuals and those with private or public health insurance were included in the analysis.
Poverty index was calculated by dividing family income by the poverty guidelines, according to family size, appropriate year, and state.16, 19 Educational status was determined by the highest grade or level of school completed or highest degree received.
Hypercholesterolemia was defined by LDL‐C values relative to 3 levels of 10‐year Framingham coronary heart disease (CHD) risk18: level 1, LDL‐C ≥100 mg/dL in patients with diabetes mellitus or clinical cardiovascular disease (CVD; CHD risk equivalent) or calculated Framingham 10‐year CHD risk >20%; level 2, LDL‐C ≥130 mg/dL in subjects with 10‐year CHD risk 10% to 20% and subjects with 10‐year CHD risk <10% and at least 2 major CHD risk factors; and level 3, LDL‐C ≥160 mg/dL in subjects with 10‐year CHD risk <10% and 0 to 1 major risk factors.
Hypercholesterolemia was also defined by affirmative answers to “Are you now taking medication to lower your cholesterol?” or a positive match between medication(s) reportedly taken and known lipid‐lowering medication(s). Awareness of hypercholesterolemia was defined by positive responses to “Has a physician ever told you that you had high cholesterol?” as the numerator and all hypercholesterolemic patients as the denominator.
Treatment of hypercholesterolemia was defined by an affirmative answer to “Are you now taking medication to lower your cholesterol?” and/or a positive match between medication(s) reported or brought to the examination and known lipid‐lowering medication(s).
Control of hypercholesterolemia was defined as LDL‐C <100, <130, and <160 mg/dL among adults in levels 1, 2 and 3, respectively, as defined above.
Major CHD risk factors were defined as described with available NHANES data.18 CHD was defined by a positive response to “Has a physician ever told you that you had a myocardial infarction?” and/or “CHD?” or angina by the Rose questionnaire.20 CHD risk equivalents included stroke, defined by a positive response to the question “Has a physician ever told you that you had a stroke?,”21 and diabetes mellitus, as defined later. CHD risk factors included cigarette smoking, hypertension (blood pressure [BP] ≥140/≥90 mm Hg or taking antihypertensive medication), and low HDL cholesterol (<40 mg/dL). Family history of premature CHD was defined as CHD in a first‐degree relative before the age of 50 years, given limited documentation on family history of CHD in NHANES.22
Diabetes mellitus included diagnosed and undiagnosed diabetes mellitus.23 Diagnosed diabetes mellitus was defined by a positive response to 1 or more questions, “Have you ever been told by a physician that you have diabetes mellitus?,” “Are you now taking insulin?,” “Are you now taking diabetic pills to lower your blood glucose?” and a match between medication(s) reported or brought to the examination and known diabetes mellitus medication(s). Undiagnosed diabetes mellitus was defined as fasting glucose ≥126 mg/dL and/or glycosylated hemoglobin ≥6.5%.
Body mass index was defined as kilograms (weight) per meter squared (height).
BP was measured and reported, as described.16
Hypertension was defined by systolic BP ≥140 mm Hg, diastolic BP ≥90 mm Hg, and/or a positive response to the question “Are you currently taking medication to lower your BP?”16
CVD was defined by any of the following conditions: CHD, stroke, and congestive heart failure. Congestive heart failure was determined by response to the question “Has a physician ever told you that you had congestive heart failure?”21
Cigarette smoker was defined if a patient answered “every day” or “some days” to the household question “Do you now smoke cigarettes?”
Data Analysis
SAS Enterprise Guide 7.1 was used for all analyses to account for NHANES complex sampling design. Only participants with fasting laboratory data were included in this analysis, and fasting sample weights were used. Estimates for prevalent hypercholesterolemia are based on all adults in the fasting sample, whereas awareness, treatment, and control were restricted to individuals with hypercholesterolemia.
Standard errors of the mean (SEM) were estimated with Taylor series (linearization) method. PROC SURVEYMEANS was used for means. PROC SURVEYFREQ was used to estimate percentages. PROC SURVEYLOGISTIC was used to explore simultaneous effects of multiple covariates on awareness, treatment, and control of elevated LDL‐C. Rao‐Scott χ2 test in PROC SURVEYFREQ was used to test for differences in categorical variables; Wald F test in the PROC SURVEYREG was used to test for differences in continuous variables. For categorical variables with >2 categories, differences across categories were assessed. P<0.05 was accepted as statistically significant.
Results
The process for selecting the study sample of adults, aged 21 to 64 years, with hypercholesterolemia from NHANES 2001 to 2012, according to the National Cholesterol Education Program III guideline, is shown in Figure 1.18
Figure 1.
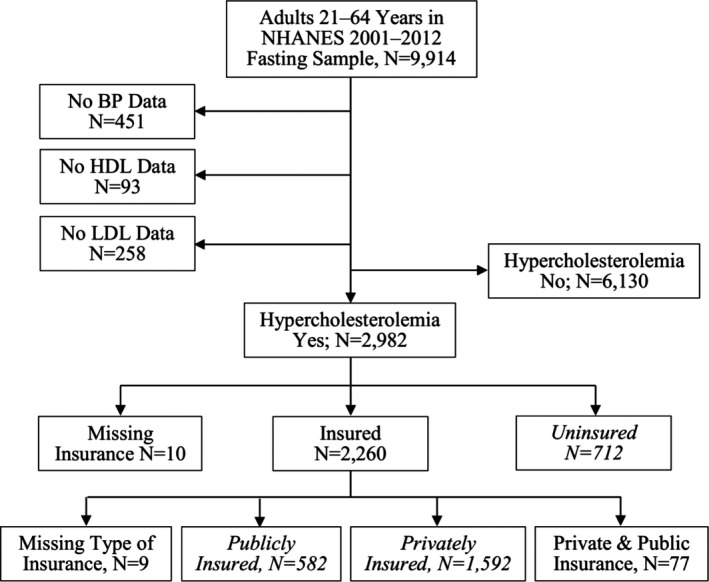
The process is depicted for selecting adults from the NHANES (National Health and Nutrition Examination Surveys), 2001 to 2012, fasting sample for analysis. Among 9914 adults, aged 21 to 64 years, in the NHANES fasting sample, 2982 met the definition for hypercholesterolemia. Data on the 712 uninsured, 582 publicly insured, and 1592 privately insured adults (italicized) were analyzed. BP indicates blood pressure; HDL, high‐density lipoprotein; and LDL‐C, low‐density lipoprotein.
Comparisons of Insured and Uninsured Adults
Of an estimated 53 468 994 US adults, aged 21 to 64 years, with high LDL‐C in NHANES 2001 to 2012, 18.1% were uninsured. The uninsured subset is younger, less likely to be white, and more likely to be minority, especially Hispanic. Approximately half of uninsured adults report little health care (<2 healthcare visits/year), and two thirds report incomes <200% of the federal poverty level, versus lower than one fourth of insured adults for both variables. Of uninsured adults, >60% deny any college education versus 40% of insured adults. Mean body mass index, prevalent hypertension, and HDL‐C are greater, whereas total cholesterol and LDL‐C are lower, for insured than uninsured adults. Prevalent diabetes mellitus and CVD are similar in both groups; the uninsured are more likely to smoke cigarettes (Table 1).
Table 1.
Characteristics of Adults, Aged 21 to 64 Years, With Hypercholesterolemia by Insurance Status
| Characteristics | Adults in NHANES 2001–2012 With Hypercholesterolemia | |||
|---|---|---|---|---|
| Insurance Status | ||||
| All Adults | Uninsured | Insured | P Value | |
| NHANES sample, Na | 2982 | 712 | 2260 | |
| US population, aged 21–64 y, with high LDL‐C, N (%) | 53 468 994 (31.2)b | 9 685 399 (18.1)c | 43 783 595 (81.9)c | |
| Age, y | 48.8±0.3 | 45.8±0.5 | 49.4±0.3 | <0.0001 |
| Sex, % | ||||
| Male | 55.6±1.0 | 56.3±2.6 | 55.5±1.1 | 0.80d |
| Female | 44.4±1.0 | 43.7±2.6 | 44.5±1.1 | |
| Race, % | ||||
| White | 71.2±1.7 | 54.3±3.3 | 75.0±1.6 | <0.0001d |
| Black | 11.3±1.0 | 12.0±1.5 | 11.1±1.0 | |
| Hispanic | 11.3±1.0 | 25.3±2.7 | 8.2±0.8 | |
| Other | 6.1±0.7 | 8.4±1.7 | 5.7±0.7 | |
| Healthcare visits/y, % | ||||
| 0–1 | 28.4±1.1 | 52.0±2.2 | 23.1±1.2 | <0.0001d |
| 2–3 | 29.5±1.0 | 22.1±2.2 | 31.2±1.2 | |
| ≥4 | 42.1±1.2 | 25.9±1.9 | 45.7±1.4 | |
| Poverty indexe | 3.2±0.1 | 1.9±0.1 | 3.4±0.1 | <0.0001 |
| Federal poverty level, % | ||||
| <100% | 12.6±0.9 | 26.4±2.5 | 9.6±0.9 | <0.0001d |
| 100%–200% | 18.8±1.1 | 40.6±2.9 | 14.1±1.1 | |
| ≥200% | 68.6±1.4 | 33.0±3.3 | 76.3±1.4 | |
| Education, % | ||||
| Less than high school | 18.7±0.9 | 33.9±2.0 | 15.3±0.9 | <0.0001d |
| High school | 25.9±1.0 | 30.4±2.3 | 24.9±1.2 | |
| Some college or more | 55.4±1.3 | 35.7±2.4 | 59.8±1.5 | |
| Body mass index, kg/m2 | 30.4±0.2 | 29.9±0.4 | 30.6±0.2 | 0.05 |
| Total cholesterol, mg/dL | 220.8±1.1 | 231.6±2.0 | 218.4±1.3 | <0.0001 |
| HDL cholesterol, mg/dL | 50.0±0.4 | 47.5±0.6 | 50.5±0.4 | <0.0001 |
| LDL‐C, mg/dL | 140.8±1.0 | 152.9±1.8 | 138.2±1.2 | <0.0001 |
| Hypertension, % | 42.0±1.3 | 33.0±2.7 | 43.9±1.4 | 0.0004 |
| Diabetes mellitus, % | 22.6±1.1 | 23.6±1.9 | 22.3±1.3 | 0.60 |
| Current cigarette smoker, % | 29.8±1.2 | 42.5±2.6 | 26.9±1.3 | <0.0001 |
| Cardiovascular disease, % | 12.9±0.8 | 11.4±1.5 | 13.2±0.9 | 0.30 |
Data are presented as mean±SEM unless otherwise indicated. HDL indicates high‐density lipoprotein; LDL‐C, low‐density lipoprotein cholesterol; and NHANES, National Health and Nutrition Examination Surveys.
Number in NHANES with fasting status and hypercholesterolemia.
Percentage of all US adults, aged 21 to 64 years.
Percentage of adults, aged 21 to 64 years, with hypercholesterolemia.
Difference in distribution between uninsured and insured adults.
Annual income/federal poverty level.
Comparisons of Adults With Private and Public Healthcare Insurance
The mean age of the 2 groups was not different, whereas the publicly insured group was more likely to be women and from minority race‐ethnicity groups than the privately insured group. Two thirds of adults with public insurance reported incomes <200% of the federal poverty level versus approximately 1 in 7 adults with private insurance. Approximately 64% of privately insured adults report at least some college education compared with ≈41% of publicly insured adults. Mean body mass index and percentages with hypertension, diabetes mellitus, CVD, and smoking cigarettes were greater for adults with public insurance. Yet, total cholesterol and LDL‐C are lower among adults with public insurance (Table 2).
Table 2.
Characteristics of Adults, Aged 21 to 64 Years, With Hypercholesterolemia and Private or Public Healthcare Insurance
| Characteristics | Adults in NHANES 2001–2012 With Hypercholesterolemia, by Insurance Type | ||
|---|---|---|---|
| Private (n=1592) | Public (n=582) | P Value | |
| US population, aged 21–64 y, with high LDL‐C, N (%) | 34 331 804 (64.2)a | 7 868 226 (14.7)a | |
| Age, y | 49.1±0.4 | 50.1±0.6 | 0.20 |
| Sex, % | |||
| Male | 57.0±1.4 | 49.3±2.5 | 0.008b |
| Female | 43.0±1.4 | 50.7±2.5 | |
| Race, % | |||
| White | 78.4±1.5 | 61.9±3.4 | <0.0001b |
| Black | 8.7±0.9 | 20.3±2.3 | |
| Hispanic | 7.4±0.7 | 12.0±2.1 | |
| Other | 5.5±0.8 | 5.8±1.1 | |
| Poverty index, %c | 3.8±0.05 | 1.8±0.1 | <0.0001 |
| <100% | 3.4±0.5 | 38.0±3.7 | <0.0001b |
| 100%–200% | 10.2±0.9 | 29.6±3.0 | |
| ≥200% | 86.4±1.1 | 32.4±3.4 | |
| Education, % | |||
| Less than high school | 10.7±0.8 | 35.6±2.8 | <0.0001b |
| High school | 25.2±1.4 | 23.7±1.8 | |
| Some college or more | 64.1±1.6 | 40.7±3.1 | |
| Healthcare visits/y, % | |||
| 0–1 | 25.8±1.4 | 13.7±2.0 | <0.0001b |
| 2–3 | 32.9±1.4 | 23.6±2.2 | |
| ≥4 | 41.3±1.5 | 62.7±2.4 | |
| Body mass index, kg/m2 | 30.3±0.2 | 31.7±0.5 | 0.02 |
| Taking BP medications, % | 37.5±1.6 | 51.3±2.6 | <0.0001 |
| Total cholesterol, mg/dL | 220.4±1.5 | 211.4±2.6 | 0.005 |
| HDL cholesterol, mg/dL | 50.6±0.5 | 49.3±0.8 | 0.20 |
| LDL‐C, mg/dL | 140.1±1.4 | 132.0±2.5 | 0.008 |
| Hypertension, % | 41.0±1.6 | 57.4±2.7 | <0.0001 |
| Current cigarette smoker, % | 23.1±1.4 | 42.0±3.1 | <0.0001 |
| Diabetes mellitus, % | 20.5±1.4 | 29.3±2.6 | 0.0004 |
| Cardiovascular disease, % | 9.8±0.9 | 27.0±2.4 | <0.0001 |
Data are presented as mean±SEM unless otherwise indicated. BP indicates blood pressure; HDL, high‐density lipoprotein; LDL‐C, low‐density lipoprotein cholesterol; and NHANES, National Health and Nutrition Examination Surveys.
Number (percentage) of adults, aged 21 to 64 years, with hypercholesterolemia.
Difference in distribution between private and public insurance.
Annual income/federal poverty level.
The prevalence of hypercholesterolemia (elevated LDL‐C) was 32.7% for insured adults (30.8% for private and 41.6% for public insurance) and 25.7% for those without insurance. Prevalence was defined, in part, by individuals reporting they were taking prescription medication to lower cholesterol. However, 154 individuals (population weight, 2 120 757) reported taking medications that did not match to known lipid‐lowering drugs but did match to known antihypertensive, antidiabetic, and other well‐defined therapeutic classes (data not shown).
In those with hypercholesterolemia, awareness, treatment, and control were greater among insured than uninsured adults but were not significantly different between adults with private and public insurance from 2001‐2004 to 2009‐2012 (Figure 2). Prevalent hypercholesterolemia was unchanged, and hypercholesterolemia awareness increased across insured and uninsured groups as well as adults with private and public insurance during this time period. Treatment and control of hypercholesterolemia increased over time in both insured groups but not in the uninsured group. Treatment and control were similar in both insured groups and higher than in the uninsured group.
Figure 2.
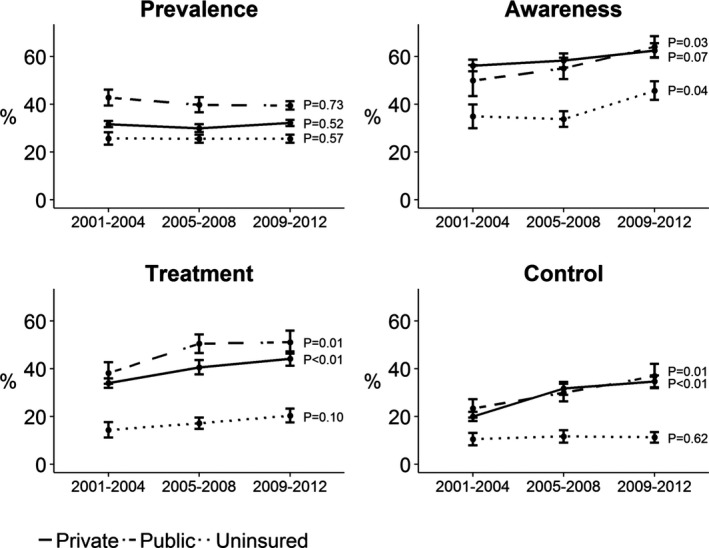
Prevalence, awareness, treatment, and control of hypercholesterolemia by insurance status and type. Prevalence, awareness, treatment, and control of hypercholesterolemia are provided for uninsured adults and for those with private or public healthcare insurance. P values represent the significance of changes over the 3 NHANES (National Health and Nutrition Examination Surveys) time periods within each of the 3 groups. Prevalence was highest in the publicly insured, lowest in the uninsured, and intermediate in the privately insured over time. Awareness, treatment, and control were all significantly lower among uninsured than the insured groups for all time periods. Awareness, treatment, and control were similar in publicly and privately insured adults at each time period.
Univariate and multivariate odds ratios of various independent variables with awareness, treatment, and control of elevated LDL‐C are provided in Table 3. Only a 10‐year increase of age, private health insurance versus uninsured, ≥2 versus <2 annual healthcare visits, and hypertension were univariate and multivariate predictors of awareness, treatment, and control of LDL‐C.
Table 3.
Demographic, Socioeconomic, and Clinical Factors to Awareness, Treatment, and Control of High LDL‐C
| Elevated LDL‐C, | Awareness | Treatment | Control | |||
|---|---|---|---|---|---|---|
| Independent Variable | Univariate | Multivariate | Univariate | Multivariate | Univariate | Multivariate |
| Age/10 ya |
1.75 (1.60–1.90)b |
1.6 (1.44–1.79)b |
2.22 (1.99–2.49)b |
1.92 (1.68–2.19)b |
2.10 (1.88–2.36)b |
1.94 (1.68–2.25)b |
| Male vs female |
0.70 (0.60–0.83)b |
0.79 (0.65–0.98)b |
0.95 (0.77–1.18) |
1.22 (0.91–1.63) |
0.94 (0.74–1.18) |
1.04 (0.77–1.41) |
| White vs Hispanic/black |
1.62 (1.35–1.94)b |
1.17 (0.94–1.47) |
1.49 (1.23–1.81)b |
1.17 (0.92–1.48) |
2.00 (1.64–2.49)b |
1.43 (1.12–1.82)b |
| ≥2 vs <2 healthcare visits/y |
3.22 (2.65–3.92)b |
2.45 (1.89–3.18)b |
5.78 (4.16–8.04)b |
4.35 (2.89–6.55)b |
4.77 (3.28–6.94)b |
4.11 (2.64–6.41)b |
| Some college or more vs less than high school |
1.66 (1.34–2.04)b |
1.58 (1.25–2.00)b |
1.34 (1.10–1.64)b |
1.17 (0.90–1.54) |
1.46 (1.19–1.80)b |
1.14 (0.90–1.44) |
| FPL <100% vs ≥200% |
0.57 (0.43–0.76)b |
1.04 (0.69–1.58) |
0.60 (0.45–0.80)b |
0.85 (0.54–1.36) |
0.42 (0.29–0.59)b |
0.57 (0.36–0.90)b |
| FPL 100%–199% vs ≥200% |
0.68 (0.52–0.88)b |
1.05 (0.74–1.49) |
0.62 (0.48–0.80)b |
0.80 (0.58–1.11) |
0.49 (0.37–0.65)b |
0.58 (0.41–0.81)b |
| Private healthcare insurance vs uninsured |
2.46 (1.92–3.17)b |
1.6 (1.14–2.25)b |
3.29 (2.50–4.35)b |
2.30 (1.55–3.42)b |
3.45 (2.53–4.71)b |
1.75 (1.19–2.57)b |
| Public healthcare insurance vs uninsured |
2.20 (1.64–2.97)b |
1.33 (0.89–1.98) |
4.10 (2.99–5.63)b |
2.16 (1.37–3.41)b |
3.59 (2.38–5.42)b |
2.11 (1.27–3.52)b |
| Hypertension (yes vs no) |
2.22 (1.84–2.67)b |
1.51 (1.19–1.91)b |
3.28 (2.67–4.04)b |
2.16 (1.68–2.76)b |
2.29 (1.82–2.89)b |
1.58 (1.19–2.10)b |
| Diabetes mellitus (yes vs no) |
1.10 (0.87–1.38) |
0.83 (0.62–1.10) |
1.84 (1.52–2.22)b |
1.45 (1.07–1.96)b |
1.23 (0.97–1.55) |
1.00 (0.73–1.36) |
| CVD (yes vs no) |
1.43 (1.12–1.83)b |
1.01 (0.72–1.42) |
2.97 (2.23–3.97)b |
2.25 (1.49–3.39)b |
1.79 (1.34–2.38)b |
1.28 (0.83–1.96) |
Data are presented as odds ratio (95% confidence interval). CVD indicates cardiovascular disease; FPL, federal poverty level; and LDL‐C, low‐density lipoprotein cholesterol.
Change in odds ratio per 10‐year increment of age.
Statistically significant (ie, 95% confidence intervals do not overlap 1.0 [line of identity]).
Aware of Elevated LDL‐C
All factors, except diabetes mellitus, were univariate predictors of awareness. Age, male sex, healthcare visit frequency, at least some college versus less education, private insurance (versus uninsured), and prevalent hypertension were multivariate predictors.
Treated LDL‐C
Of 12 variables, 11 were univariate predictors of treated LDL‐C, with the exception of male sex. In multivariate analysis, age, greater healthcare visit frequency, private and public insurance versus uninsured, and prevalent hypertension, diabetes mellitus, and CVD were significant predictors of treatment, whereas poverty was not.
Controlled LDL‐C
Of 12 univariate predictors, 10 were related to LDL‐C control, except male sex and diabetes mellitus. Multivariate predictors of LDL‐C control included increasing age, white race, greater healthcare visit frequency, private and public health insurance (versus uninsured), and hypertension. Incomes <100% and 100% to 199% versus ≥200% were linked with lower LDL‐C control.
Percentages of insured and uninsured adults with untreated and treated hypercholesterolemia and with treated controlled and treated uncontrolled LDL‐C are depicted (Figure 3). Uninsured adults were less likely to receive antilipid medication. Once they were taking antilipid medication, uninsured adults were slightly, but not significantly, less likely to attain LDL‐C control. Percentages of privately and publicly insured adults with untreated and treated hypercholesterolemia overall and according to 10‐year CHD risk categories are shown in Figure 3. The percentages taking antilipid therapy were not different. Statin therapy was reported more often by adults with controlled than uncontrolled LDL‐C for both insurance groups.
Figure 3.
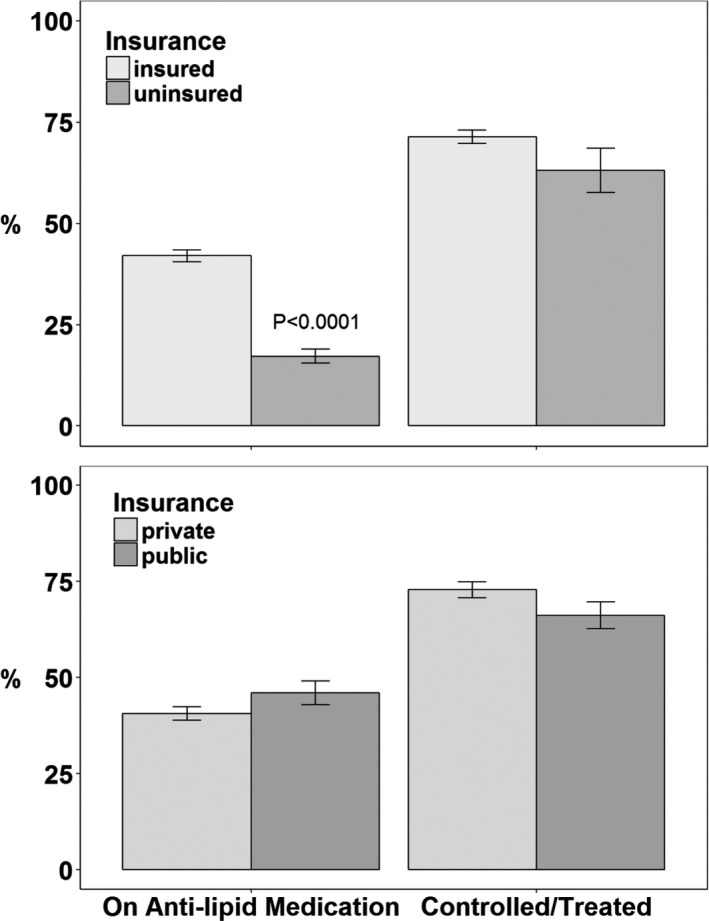
Treatment and control of hypercholesterolemia by insurance status and type. Top panel: Adults with and without healthcare insurance. Bottom panel: Adults with private versus public healthcare insurance. The left side of each panel depicts the percentage of hypercholesterolemic adults taking lipid‐lowering medication. The right side shows the percentage of treated adults with low‐density lipoprotein cholesterol controlled to their Adult Treatment Panel‐3 goal.
Discussion
The principal new finding of this report is that hypercholesterolemia was controlled in approximately 1 in 9 to 10 uninsured adults, aged 21 to 64 years, in the United States and did not improve between 2001 to 2004 and 2009 to 2012. For insured adults, LDL‐C control increased from approximately 1 in 5 to 1 in 3 during this time as the disparity in LDL‐C between insured and uninsured adults more than doubled from 10.9% to 23.8%. Even with insurance, most adults with hypercholesterolemia had uncontrolled LDL‐C.
In a prior report from NHANES 2005 to 2008, control of hypercholesterolemia, defined as total cholesterol <240 mg/dL, was comparable among adults with private and public insurance and higher than adults without health insurance.8 Another report applied the National Cholesterol Education Program (NCEP) III guidelines to prevalence, treatment, and control of LDL‐C in both 1999 to 2002 and 2005 to 2008,9 but insurance data were presented only for 2005 to 2008. Treatment and control of hypercholesterolemia were not different in adults with private and public insurance but were lower in uninsured adults. Our study indicates that disparities in controlling hypercholesterolemia between the insured and uninsured have been growing, whereas parity between adults with public and private healthcare insurance persisted from 2001 to 2004 through 2009 to 2012.
CVD remains a major health concern. In the United States, >1 500 000 adults experience a myocardial infarction or stroke annually, and ≈500 000 die from these events.24, 25 Although not minimizing the importance of controlling hypertension and diabetes mellitus, treating all statin‐eligible but untreated individuals in the United States by the 2013 Cholesterol Guideline was estimated to prevent >240 000 cardiovascular events annually.5
There is long‐standing interest in factors associated with limited detection and treatment of hypercholesterolemia, including low incomes, lack of health insurance, infrequent health care, and minority race‐ethnicity.6, 7, 8, 9, 10, 11 The Framingham Heart Study also identified insurance as a key variable in control of both hypertension and hypercholesterolemia, with adjustment only for age and related family members.7 In a more robust multivariate model, healthcare insurance emerged as an independent predictor of hypertension, but not cholesterol, control in the ARIC (Atherosclerosis Risk in Communities) Study.26
A key objective of this report was to increase clarity about modifiable factors affecting success with the NCEP III guideline in effect from 2001 to 201318 on the prevalence, awareness, treatment, and control of hypercholesterolemia. The insights derived from this analysis are intended to help inform education, policy, and healthcare delivery strategies to prevent more CVD with the 2013 Cholesterol Guideline.1, 5
An important initial step in managing hypercholesterolemia is awareness. Although awareness increased in the uninsured over time, it remained lower than in insured adults (Figure 2). In another report, awareness increased over time in uninsured adults, and the disparity with insured adults narrowed.17 Greater awareness of hypercholesterolemia among uninsured adults was especially prominent in health professional shortage areas.27 In this study, private, but not public, healthcare insurance was independently associated with awareness, although confidence intervals for the 2 payer types overlapped. Lower incomes were associated with less awareness in univariate, but not in multivariate, analysis, which suggests that income per se is not an independent driver of awareness. In contrast, female sex, increasing age, more frequent health care, at least some college education, and hypertension were independently linked with awareness.
Once hypercholesterolemia is recognized, effective management is the next step. All variables in the logistic regression model, except male sex, were univariate predictors of treatment. Treatment of high LDL‐C increased over time among all insured adults and for those with private or public healthcare insurance separately. Despite greater hypercholesterolemia over time in the uninsured group, treatment did not increase significantly. In multivariate analysis, older age, more frequent health care, private and public healthcare insurance, hypertension, diabetes mellitus, and CVD were all positively associated with treatment, but income was not. Thus, insured individuals, and especially those with greater cardiovascular risk who use health care frequently, are more likely to receive treatment for hypercholesterolemia. Another study reported that a usual source of care was the best predictor of receiving a statin for hypercholesterolemia.28
The 2013 Cholesterol Guideline does not include treatment goals for LDL‐C,1 unlike NCEP III18 rather, risk‐based intensity of statin therapy is given. Similar to treatment, LDL‐C control increased over time for privately and publicly insured adults separately but not for uninsured adults (Figure 2). Like awareness and treatment, older age, more frequent health care, private health insurance, and hypertension were independently associated with better LDL‐C control. Unlike awareness and treatment, lower household incomes and racial‐ethnic minority status (black or Hispanic) were independently linked with poorer LDL‐C control, whereas public healthcare insurance (versus uninsured) was associated with better control. Previous studies also found that income was independently associated with cholesterol control.28, 29 These data suggest that even when treated, individuals with lower incomes and minority race‐ethnicity status are less likely to receive adequate therapy. Although publicly and privately insured adults had better LDL‐C control than uninsured adults, once treated, there was not a significant difference in the proportion of insured and uninsured adults whose LDL‐C was controlled (Figure 3).
For modifiable variables, frequency of health care was the strongest independent predictor of awareness, treatment, and control of hypercholesterolemia. Although more than half of the uninsured with hypercholesterolemia report <2 healthcare visits annually, this was also true for nearly 1 in 4 privately insured individuals. Individuals who report using healthcare services less than twice annually are much less likely to be aware, treated, and controlled. Prior analyses of NHANES reported a higher frequency of health care in those with treated9 and controlled hypercholesterolemia,9, 11 but the independent contribution was not provided. Framingham and ARIC reports did not address visit frequency.7, 26 Unfortunately, successful efforts to raise awareness of hypercholesterolemia among uninsured adults have not increased treatment and control. Thus, efforts to increase awareness of risk factors through screening must be combined with follow‐up care of individuals with treatable risk.
Healthcare insurance, another modifiable variable, was associated with treatment and/or control of hypercholesterolemia in several reports6, 7, 8, 9, 10, 11, 12 and independently associated with control7 in one report, but not in another report.26 Because frequency of care was included in the multivariate model, it is unclear whether this association is predominantly related to out‐of‐pocket cost of medications, which was not available for analysis. Previous research documents that out‐of‐pocket costs are strongly and inversely related to medication adherence.30 In fact, generic statins, which are generally less costly than proprietary options, are associated with better adherence and fewer cardiovascular events than proprietary statins.31 Atorvastatin and rosuvastatin, the only 2 statins qualified for high‐intensity therapy in the 2013 Cholesterol Guideline, are now generic.
Limitations of this report include the small sample size, especially for uninsured and publicly insured adults, which diminished power for detecting differences within and between groups at various time intervals from 2001 to 2012. As with prior reports,3, 9, 11 hypercholesterolemia was defined, in part, by adults reportedly taking prescription medication to lower their cholesterol. Yet, 154 participants, representing >2 000 000 US adults, reported taking medications to lower cholesterol that belonged to other drug classes. LDL‐C control in NCEP III is an imperfect proxy for adequate intensity statin therapy in the 2013 Cholesterol Guideline.
In summary, full implementation of the 2013 Cholesterol Guideline could significantly reduce the burden of preventable CVD and related health disparities.1, 2, 3, 4, 5 On the basis of analysis of NHANES 2001 to 2012, according to NCEP III criteria, frequency of health care was the single most important factor in the awareness, treatment, and control of elevated LDL‐C. Although awareness of hypercholesterolemia is increasing among uninsured adults, control is not. Thus, educational, healthcare policy, and healthcare delivery strategies to increase awareness of hypercholesterolemia must be linked to increasing the number of individuals who have access to and regularly use primary care to effectively manage their cholesterol‐related vascular risk. Improving health insurance coverage and reducing out‐of‐pocket costs for evidence‐based cholesterol treatment emerge as other important factors in effective cholesterol management. A rapid learning health system is essential. This system can promptly assess responses to quality improvement initiatives and refine protocols and resource allocation to optimize evidence‐based CVD prevention.
Sources of Funding
This research was supported, in part, by funding from the Centers for Disease Control and Prevention, through the South Carolina Department of Health and Environmental Control, and from the Health Research Services Administration, through the Medical University of South Carolina. The funding agencies did not participate in the design and conduct of the study; in collection, management, analysis, and interpretation of the data; or in preparation, review, and approval of the article.
Disclosures
Egan has received royalties from UpToDate, research support from Medtronic and Quintiles, income as a consultant from AstraZeneca, Medtronic, and Valencia, and honoraria for lectures from Merck‐Serono and Emcure. None of the other authors has any disclosures to report.
(J Am Heart Assoc. 2017;6:e006105 DOI: 10.1161/JAHA.117.006105.)29097386
References
- 1. Stone NJ, Robinson JG, Lichtenstein AH, Merz CNB, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PWF. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. JACC. 2014;63:2889–2934. [DOI] [PubMed] [Google Scholar]
- 2. Taylor F, Huffman MD, Macedo TH, Moore TH, Burke M, Davey Smith G, Ward K, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Data Syst Rev. 2013;1:1–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pencina MJ, Navar‐Boggan AM, D'Agostino RB, Williams K, Neely B, Sniderman AD, Peterson ED. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014;370:1422–1431. [DOI] [PubMed] [Google Scholar]
- 4. Pandya A, Sy S, Cho S, Weinstein MC, Gaziano TA. Cost‐effectiveness of 10‐year risk thresholds for initiation of statin therapy for primary prevention of cardiovascular disease. JAMA. 2015;214:142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Egan BM, Li J, White K, Fleming DO, Connell K, Hernandez GT, Ferdinand KC, Sinopoli A. 2013 ACC/AHA Cholesterol Guideline and Implications for Healthy People 2020 Cardiovascular Disease Prevention Goals. J Am Heart Assoc. 2016;5:e003558 DOI: 10.1161/JAHA.116.003558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Hypertension, diabetes, and elevated cholesterol among insured and uninsured adults. Health Aff. 2009;28:w1151–w1159. [DOI] [PubMed] [Google Scholar]
- 7. Brooks EL, Preis SR, Hwang SJ, Murabito JM, Benjamin EJ, Kelly‐Hayes M, Sorlie P, Levy D. Health insurance and cardiovascular disease risk factors. Am J Med. 2010;3:741–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schober SE, Makuc DM, Zhang C, Kennedy‐Stephenson J, Burt V. Health insurance affects diagnosis and control of hypercholesterolemia and hypertension among adults aged 20–64: United States, 2005–2008. NCHS Data Brief, no. 57, January, 2011. Available at: https://www.cdc.gov/nchs/data/databriefs/db57.pdf. Accessed February 27, 2017. [PubMed]
- 9. Kuklima EV, Shaw KM, Hong Y. Vital signs: prevalence, treatment, and control of high levels of low‐density lipoprotein cholesterol—United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60:109–114. [PubMed] [Google Scholar]
- 10. Decker SL, Kostova D, Kenney GM, Long SK. Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs. uninsured low‐income adults potentially eligible for Medicaid under the Affordable Care Act. JAMA. 2013;309:2579–2586. [DOI] [PubMed] [Google Scholar]
- 11. Mercado C, DeSimone AK, Odom E, Gillespie C, Ayala C, Loustalot F. Prevalence of cholesterol treatment eligibility and medication use among adults—United States, 2005–2012. MMWR Morb Mortal Wkly Rep. 2014;64:1305–1311. [DOI] [PubMed] [Google Scholar]
- 12. Ross JR, Bradley EH, Busch SH. Use of healthcare services by lower‐income and higher‐income uninsured adults. JAMA. 2006;295:2027–2036. [DOI] [PubMed] [Google Scholar]
- 13. Hogan DR, Goodarz D, Ezzata M, Clarke PM, Jha AK, Salomon JA. Estimating the impact of insurance expansion on undiagnosed and uncontrolled chronic conditions. Health Aff. 2015;9:1554–1562. [DOI] [PubMed] [Google Scholar]
- 14. McWilliams JM, Meara E, Zalavsky AM, Ayanian JZ. Health of previously uninsured adults after acquiring Medicare coverage. JAMA. 2007;298:2886–2894. [DOI] [PubMed] [Google Scholar]
- 15. McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med. 2007;357:143–153. [DOI] [PubMed] [Google Scholar]
- 16. Egan BM, Li J, Small J, Nietert PJ, Sinopoli A. The growing gap in hypertension control between insured and uninsured adults: NHANES 1988–2010. Hypertension. 2014;64:997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Prior HHS poverty guidelines and federal register references . Office of the Assistant Secretary for Planning and Evaluation: US Department of Health and Human Services. https://aspe.hhs.gov/prior-hhs-poverty-guidelines-and-federal-register-references. Accessed February 27, 2017.
- 18. Abdus S, Selden TM. Preventive services for adults: how have differences across subgroups changed over the past decade? Med Care. 2013;451:999–1007. [DOI] [PubMed] [Google Scholar]
- 19. Adults . Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 20. Rose GA, Blackburn H, Gillium RF, Prineas RJ. Cardiovascular Survey Methods. 2nd ed Geneva, Switzerland: World Health Organization; 1982. [Google Scholar]
- 21. Muntner P, DeSalvo KB, Wildman RP, Raggi P, He J, Whelton PK. Trends in the prevalence, awareness, treatment, and control of cardiovascular disease risk factors among non‐institutionalized patients with a history of myocardial infarction and stroke. Am J Epidemiol. 2006;163:913–920. [DOI] [PubMed] [Google Scholar]
- 22. Hyre AD, Munter P, Menke A, Raggi P, He J. Trends in ATP‐III‐defined high blood cholesterol prevalence, awareness, treatment and control among U.S. adults. Ann Epidemiol. 2007;17:548–555. [DOI] [PubMed] [Google Scholar]
- 23. American Diabetes Association . Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(suppl 1):S11–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stroke Facts . http://www.cdc.gov/stroke/facts.htm. Accessed February 27, 2017.
- 25. Heart Disease Facts . http://www.cdc.gov/heartdisease/facts.htm. Accessed March 2, 2016.
- 26. Fowler‐Brown A, Corbie‐Smith G, Garrett J, Lurie N. Risk of cardiovascular events and death: does insurance matter? J Gen Intern Med. 2007;22:502–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Durant RW, Parmar G, Shuaib F, Le A, Brown TM, Roth DL, Hovater M, Halanych JH, Shikany JM, Prenieas RJ, Samdarshi TJ, Safford MM. Awareness and management of chronic disease, insurance status, and health professional shortage areas in the Reasons for Geographic And Racial Differences in Stroke (REGARDS): a cross‐sectional study. BMC Health Serv Res. 2012;12:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Winters P, Tancredi D, Fiscella K. The role of usual source of care in cholesterol treatment. J Am Board Fam Med. 2010;23:179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Franks P, Tancredi D, Winters P, Fiscella K. Cholesterol treatment with statins: who is left out and who makes it to goal? BMC Health Serv Res. 2010;10:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Eaddy MT, Cook CL, O'Day K, Burch SP, Cantrell R. How patient cost‐sharing trends affect adherence and outcomes. P T. 2012;37:45–55. [PMC free article] [PubMed] [Google Scholar]
- 31. Gagne JJ, Choudhry NK, Kseelheim AS, Polinski JM, Huthchins D, Matlin OS, Brennan TA, Avorn J, Shrank WH. Comparative effectiveness of generic and brand‐name statins on patient outcomes. Ann Intern Med. 2014;161:400–407. [DOI] [PubMed] [Google Scholar]


