Abstract
Background
IMPROVE‐IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) showed that adding the nonstatin ezetimibe to statin therapy further reduced cardiovascular events in patients after an acute coronary syndrome. In a prespecified analysis, we explore results stratified by sex.
Methods and Results
In IMPROVE‐IT, patients with acute coronary syndrome and low‐density lipoprotein cholesterol of 50 to 125 mg/dL were randomized to placebo/simvastatin 40 mg or ezetimibe/simvastatin 10/40 mg. They were followed up for a median of 6 years for the primary composite of cardiovascular death, myocardial infarction, hospitalization for unstable angina, coronary revascularization ≥30 days, and stroke. Among 18 144 patients in IMPROVE‐IT, 4416 (24%) were women. At 12 months, the addition of ezetimibe to simvastatin significantly reduced low‐density lipoprotein cholesterol from baseline compared with simvastatin monotherapy in men and women equally (absolute reduction, 16.7 mg/dL in men and 16.4 mg/dL in women). Women receiving ezetimibe/simvastatin had a 12% risk reduction over those receiving placebo/simvastatin for the primary composite end point (hazard ratio, 0.88; 95% confidence interval, 0.79–0.99) compared with a 5% reduction for men (hazard ratio, 0.95; 95% confidence interval, 0.90–1.01; P=0.26 for interaction). When the total number of primary events was considered, women had an 18% reduction with the addition of ezetimibe (relative risk, 95% confidence interval, 0.81; 0.71–0.94) and men had a 6% reduction (relative risk, 0.94; 95% confidence interval, 0.87–1.02; P=0.08 for interaction). The addition of ezetimibe did not increase the rates of safety events in either women or men.
Conclusions
IMPROVE‐IT demonstrated that the benefit of adding ezetimibe to statin is present in both women and men, with a good safety profile supporting the use of intensive, combination, lipid‐lowering therapy to optimize cardiovascular outcomes.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unique identifier: NCT00202878.
Keywords: cholesterol, chronic ischemic heart disease, coronary artery disease, ezetimibe, lipids and lipoprotein metabolism, secondary prevention, sex, women
Subject Categories: Lipids and Cholesterol, Women, Secondary Prevention, Chronic Ischemic Heart Disease
Clinical Perspective
What Is New?
IMPROVE‐IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) was the longest of the large randomized trials of intensive lipid lowering. In 4416 women followed up for an average of 6 years, we found that women had similar reductions in low‐density lipoprotein cholesterol and relative clinical benefit as men with the addition of ezetimibe to statin therapy after acute coronary syndrome.
Ezetimibe did not increase the risk of safety events compared with placebo in either women or men.
Women were, on average, at higher risk of cardiovascular events than men, as determined by a novel score to assess risk in a secondary prevention population.
The higher average risk in women translated into a greater absolute reduction in first and total cardiovascular events with the addition of ezetimibe in women compared with men.
What Are the Clinical Implications?
Women after acute coronary syndrome who are treated with ezetimibe in addition to statin should anticipate having similar reductions in low‐density lipoprotein cholesterol and relative clinical benefit as men.
Because women are, on average, at higher risk than men, treating women after acute coronary syndrome with ezetimibe plus statin would be expected to result in even greater absolute reductions of cardiovascular events (both first and total events) compared with men.
Ezetimibe may be added to statin in women and in men after acute coronary syndrome without increasing the risk of muscle‐related or other adverse events.
Atherothrombotic cardiovascular disease remains one of the leading causes of death worldwide, and it is of equal importance in women and men. The role of low‐density lipoprotein cholesterol (LDL‐C) lowering by statins in safely reducing vascular events in both men and women1, 2, 3, 4, 5, 6 is well established. Previous studies have shown that women are usually 5 to 10 years older than men when they develop coronary heart disease, and they often have more comorbidities. However, women receive statins less frequently than men, and when they are treated, they are more likely to receive lower‐intensity therapy.7, 8, 9, 10, 11, 12
The Cholesterol Treatment Trialists' Collaboration meta‐analysis, with >174 000 participants in 27 primary and secondary prevention trials of statin therapy, showed that the proportional reductions of major vascular events per 1.0‐mmol/L reduction in LDL‐C during a median follow‐up of 4.9 years were similar overall for women (relative risk [RR], 0.84; 99% confidence interval [CI], 0.78–0.91) and men (RR, 0.78; 99% CI, 0.75–0.81; adjusted P=0.33 for heterogeneity by sex).6 However, it is not clear whether LDL‐C lowering with a nonstatin agent affects clinical outcomes to a similar degree in women and men. The IMPROVE‐IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) randomized 18 144 patients (4416 women).13, 14 In this prespecified analysis, we examined the impact of sex on the treatment effect of ezetimibe on lipid lowering, cardiovascular events, and adverse events.
Methods
Study Design and Study Population
The design and results of IMPROVE‐IT have been described previously.13, 14 Briefly, IMPROVE‐IT was a randomized, double‐blind, placebo‐controlled, multicenter trial designed to examine the efficacy and safety of ezetimibe added to simvastatin. The trial enrolled men and women aged >50 years who had been hospitalized within the previous 10 days for an acute coronary syndrome, including myocardial infarction (MI) with or without ST‐segment elevation or high‐risk unstable angina. To be eligible, an LDL‐C level measured within 24 hours after hospital admission for this acute coronary syndrome had to be 50 to 125 mg/dL for patients not receiving prior prescription lipid‐lowering therapy and 50 to 100 mg/dL for patients who had been receiving long‐term statin therapy. Major exclusion criteria included the prevalence of hemodynamic events, ischemic and arrhythmic events within 24 hours before enrollment, creatinine clearance <30 mL/min, active liver disease, or the use of statin therapy that had potency >40 mg of simvastatin at enrollment.
Randomization and Study End Points
Patients were randomized in a 1:1 manner to placebo/simvastatin 40 mg or ezetimibe 10 mg/simvastatin 40 mg daily. The primary efficacy end point was a composite of cardiovascular death, major coronary event (nonfatal MI, rehospitalization for unstable angina, or coronary revascularization occurring ≥30 days after randomization), or nonfatal stroke. Prespecified safety variables included elevated liver enzyme and creatine kinase levels, episodes of myopathy or rhabdomyolysis, gallbladder‐related adverse events, and cancer. All primary end points (except coronary revascularization), cancer, and muscle‐related events were adjudicated by a blinded central event adjudication committee.
Statistical Analysis
The data were stratified by sex. Baseline characteristics were reported as frequencies and percentages for categorical variables and as medians and interquartile ranges for continuous variables. Baseline characteristics were compared using the χ2 test for categorical variables and the Wilcoxon test for continuous variables. All primary analyses were performed on an intention‐to‐treat basis. As a sensitivity analysis, safety events were analyzed during the on‐treatment period, which included events that occurred within 30 days after discontinuation of study drug.14
Efficacy results were presented as Kaplan‐Meier failure rates at 7 years, and safety outcomes were presented as the proportion of patients having the events in the study period. Time‐to‐event analyses used the log‐rank test with stratification by qualifying event. Cox proportional hazard models were used to evaluate heterogeneity. Cox regression was used to test for effect modification by evaluating the interaction terms for sex and treatment strategy for each outcome. We also compared the total number of primary end points between men and women using a negative binominal regression analysis, as previously described.15
The TIMI (Thrombolysis in Myocardial Infarction) Risk Score for Secondary Prevention (TRS 2°P), an integer‐based risk stratification tool derived in patients with established ischemic heart disease, for prediction of cardiovascular death, MI, or ischemic stroke, was used to evaluate risk and treatment efficacy by sex. The TRS 2°P was previously developed in a cohort of patients with established ischemic heart disease16 and subsequently validated in IMPROVE‐IT17 for the prediction of recurrent cardiovascular events and identification of high‐risk patients who had a greater relative and absolute risk reduction with the addition of ezetimibe. As previously described, each patient was assessed for the presence of the 9 clinical risk indicators at baseline: age ≥75 years, diabetes mellitus, hypertension, peripheral artery disease, prior stroke, prior coronary artery bypass graft, history of heart failure, active smoking, and renal dysfunction.
All analyses were performed using SAS software, version 9.4. A 2‐sided P<0.05 was considered to indicate statistical significance. The ethics committee at each participating center approved the protocol and amendments, and all the participants gave written informed consent.
Results
Patient Characteristics
Among 18 144 patients, 4416 (24%) were women and 13 728 (76%) were men. Baseline characteristics are summarized in Table 1. Women were significantly older and were more likely to have a history of hypertension, diabetes mellitus, heart failure, stroke, or transient ischemic attack and estimated glomerular filtration rate <60 ml/min/1.73 m2, whereas men were more likely to be smokers and have a history of coronary revascularization (P<0.05 for each). The use of prescription lipid‐lowering agents before the index event was similar (women, 36.5%; men, 35.2%; P=0.13).
Table 1.
Baseline Characteristics by Sex
| Baseline Characteristics | Women (n=4416) | Men (n=13 728) |
|---|---|---|
| Age, y | 66 (58–74) | 63 (56–70) |
| Age ≥75 y | 947 (21) | 1851 (14) |
| Hypertension | 3093 (70) | 8044 (59) |
| Current smoker | 1290 (29) | 4688 (34) |
| Diabetes mellitus | 1407 (32) | 3526 (26) |
| History of CHF | 238 (5.4) | 552 (4.0) |
| History of coronary revascularization | 908 (21) | 3579 (26) |
| History of stroke or TIA | 316 (7.2) | 755 (5.5) |
| Peripheral arterial disease | 268 (6.1) | 737 (5.4) |
| CABG | 299 (6.8) | 1385 (10) |
| eGFR <60 ml/min/1.73 m2 | 1378 (32) | 2135 (16) |
| BMI, kg/m2 | 28 (24–32) | 28 (25–31) |
| Prior statin use | 1567 (36) | 4679 (34) |
| Prior lipid‐lowering agent use | 1607 (37) | 4827 (35) |
| At qualifying event | ||
| STEMI | 1036 (24) | 4154 (30) |
| NSTEMI | 2136 (48) | 6419 (47) |
| Unstable angina | 1239 (28) | 3147 (23) |
| LDL‐C <100 mg/dL | 2601 (60) | 7976 (59) |
| LDL‐C <70 mg/dL | 553 (13) | 1927 (14) |
| Statin | 3323 (75) | 10 703 (78) |
| At randomization | ||
| LDL‐C <100 mg/dL | 3345 (77) | 10 802 (80) |
| LDL‐C <70 mg/dL | 1343 (31) | 4448 (33) |
| Aspirin | 4231 (96) | 13 361 (97) |
| Thienopyridine | 3608 (82) | 12 074 (88) |
| Dual antiplatelet | 3498 (79) | 11 838 (86) |
Data presented are median (interquartile range) for continuous variables and number (percentage) for categorical variables. P<0.05 for all comparisons, except for BMI (P=0.1), NSTEMI at QE (P=0.058), and LDL‐C <100 mg/dL at QE (P=0.318). BMI indicates body mass index; CABG, coronary artery bypass graft; CHF, congestive heart failure; eGFR, estimated glomerular filtration rate; LDL‐C, low‐density lipoprotein cholesterol; NSTEMI, non–ST‐segment–elevation myocardial infarction; STEMI, ST‐segment–elevation myocardial infarction; and TIA, transient ischemic attack.
Outcomes
Lipid profiles
The effects of ezetimibe on all of the lipid parameters were comparable between women and men (P value for interaction [P int]>0.10 for each). When comparing LDL‐C at randomization with that at 12 months, ezetimibe significantly reduced LDL‐C levels by 16.4 mg/dL in women and 16.7 mg/dL in men. Similarly, at 12 months, a significant reduction in the median triglyceride level and a significant increase in high‐density lipoprotein cholesterol level were observed in women and men (P<0.05 for each), without any treatment effect modification by sex (Table 2).
Table 2.
Changes in the Lipid Parameters by Sex
| Lipid Parameters | Sex | Treatment Arm | Median (IQR) | Changes at 12 Mo | |||
|---|---|---|---|---|---|---|---|
| At Qualifying Event | At 12 Mo | ||||||
| Median (IQR) | P Value | P int | |||||
| LDL‐C, mg/dL | Women | Ezetimibe/simvastatin | 95.0 (80.0 to 110.0) | 51.0 (40.0 to 65.0) | −41.0 (−59.0 to −24.0) | <0.001 | 0.74 |
| Placebo/simvastatin | 95.0 (79.0 to 110.0) | 69.0 (57.0 to 82.0) | −24.6 (−42.0 to −5.7) | ||||
| Men | Ezetimibe/simvastatin | 95.0 (79.0 to 110.0) | 49.0 (39.0 to 61.0) | −43.7 (−61.0 to −25.3) | <0.001 | ||
| Placebo/simvastatin | 95.0 (79.0 to 110.0) | 67.0 (55.0 to 80.0) | −27.0 (−44.9 to −7.0) | ||||
| HDL‐C, mg/dL | Women | Ezetimibe/simvastatin | 45.0 (36.0 to 55.0) | 54.0 (45.0 to 63.0) | 8.0 (2.0 to 15.0) | 0.01 | 0.75 |
| Placebo/simvastatin | 46.0 (37.0 to 57.0) | 53.0 (44.0 to 64.0) | 7.0 (0.4 to 13.9) | ||||
| Men | Ezetimibe/simvastatin | 39.0 (32.0 to 46.0) | 45.0 (39.0 to 53.0) | 6.0 (0.7 to 12.0) | <0.001 | ||
| Placebo/simvastatin | 39.0 (32.0 to 46.0) | 44.0 (38.0 to 53.0) | 5.6 (0 to 11.0) | ||||
| Triglyceride, mg/dL | Women | Ezetimibe/simvastatin | 115.0 (82.0 to 168.0) | 109.0 (80.0 to 145.0) | −6.0 (−42.0 to 23.0) | <0.001 | 0.19 |
| Placebo/simvastatin | 116.0 (83.0 to 168.0) | 118.0 (88.0 to 164.0) | 3.0 (−29.0 to 35.0) | ||||
| Men | Ezetimibe/simvastatin | 121.0 (86.0 to 174.0) | 103.0 (76.0 to 141.0) | −16.4 (−55.2 to 16.5) | <0.001 | ||
| Placebo/simvastatin | 122.0 (65.0 to 174.0) | 116.0 (83.0 to 166.0) | −3.2 (−39.7 to 33.3) | ||||
Changes in the lipid parameters were all comparable between men and women. HDL‐C indicates high‐density lipoprotein cholesterol; IQR, interquartile range; LDL‐C, low‐density lipoprotein cholesterol; and P int, P value for interaction.
Efficacy outcomes
Kaplan‐Meier event rates for the primary end point at 7 years with placebo/simvastatin were 34.0% in women and 34.9% in men. Women randomized to ezetimibe/simvastatin showed a significant 12% lower event rate compared with those randomized to placebo/simvastatin (hazard ratio [HR], 0.88; CI 0.79–0.99), whereas a 5% reduction was seen for men (HR, 0.95; 95% CI, 0.90–1.01) (Figure 1). These relative treatment effects between women and men did not differ statistically (P int=0.26), nor did they differ significantly for cardiovascular death, MI, and stroke (P int>0.1 for each; Figure 2). The benefit of adding ezetimibe to simvastatin in women was driven largely by a lower incidence of MI, in which a 22% reduction was observed (HR, 0.78; 95% CI, 0.66–0.93; Figure 2), and this benefit did not differ by sex (HR, 0.90; 95% CI, 0.82–1.00; P int=0.17).
Figure 1.

Seven year Kaplan‐Meier estimate curves of primary end point by sex. The treatment effects were similar between women and men for the primary end point of cardiovascular death, major coronary event (nonfatal myocardial infarction, rehospitalization for unstable angina, or coronary revascularization event occurring at least 30 days after randomization), or nonfatal stroke (P=0.26 for interaction). The Kaplan‐Meier rates at 7 years were 34.0% with placebo/simvastatin and 31.0% with ezetimibe/simvastatin in women and 34.9% with placebo/simvastatin and 33.3% with ezetimibe/simvastatin in men. EZE indicated ezetimibe; HR, hazard ratio; PBO, placebo; Simva, Simvastatin.
Figure 2.
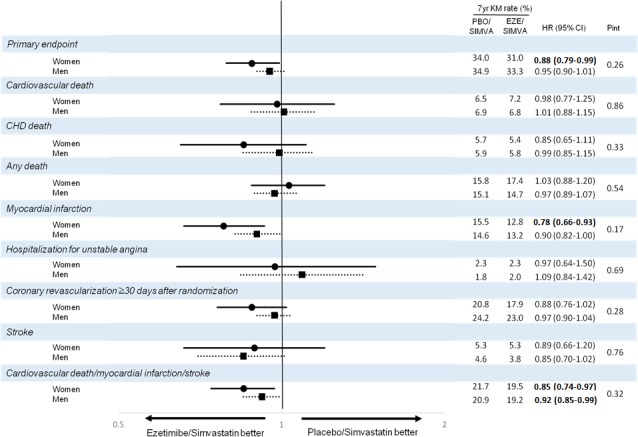
Efficacy outcomes by sex. Women had a significant 22% reduction of myocardial infarction and a 12% reduction of major adverse cardiac events (composite of cardiovascular death, myocardial infarction, and stroke) with ezetimibe compared with placebo. There were no significant treatment interactions by sex for any of the end points. CHD indicates coronary heart disease; CI, confidence interval; Eze, ezetimibe; HR, hazard ratio; KM, Kaplan‐Meier; PBO, placebo; P int, P value for interaction; Simva, simvastatin.
Total primary end points
There were 2132 and 7413 total primary end points in women and men, respectively. Of these, 1215 and 4099 events were first primary end points events, and an additional 917 and 3314 events occurred after the first primary end point in women and men, respectively. Overall, total primary end points were reduced by 174 events (65 first events and 109 subsequent events) in women (RR for ezetimibe/simvastatin versus placebo/simvastatin, 0.81; 95% CI, 0.71–0.94) and by 247 events (105 first events and 142 subsequent events) in men (RR for ezetimibe/simvastatin versus placebo/simvastatin, 0.94; 95% CI, 0.87–1.02; Figure 3). There was a trend toward a larger reduction in total number of events in women compared with men during the follow‐up period (P int=0.08).
Figure 3.
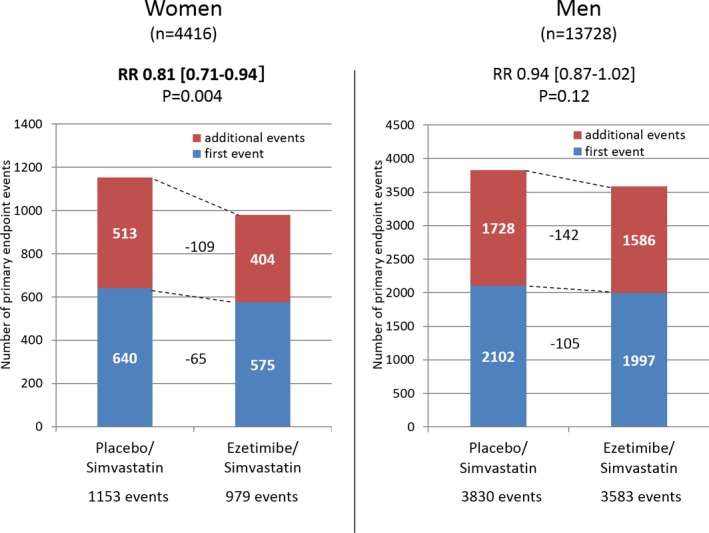
Total primary end point by sex. Adding ezetimibe to simvastatin reduced the total number of primary end points in both men and women (P=0.08 for interaction). RR indicates relative reduction.
Risk stratification
Using the TRS 2°P,16 women were approximately equally distributed across risk categories, with 35.6% of women classified as low risk (risk score, 0–1), 31.0% as intermediate risk (risk score, 2), and 33.4% as high risk (risk score, ≥3). In contrast, approximately half of the men (48.5%) were at low risk, 29.5% were at intermediate risk, and the remaining 22.0% were at high risk, which represented a significantly different distribution (lower risk profile in men) compared with women (P<0.001 by χ2; Figure 4).
Figure 4.
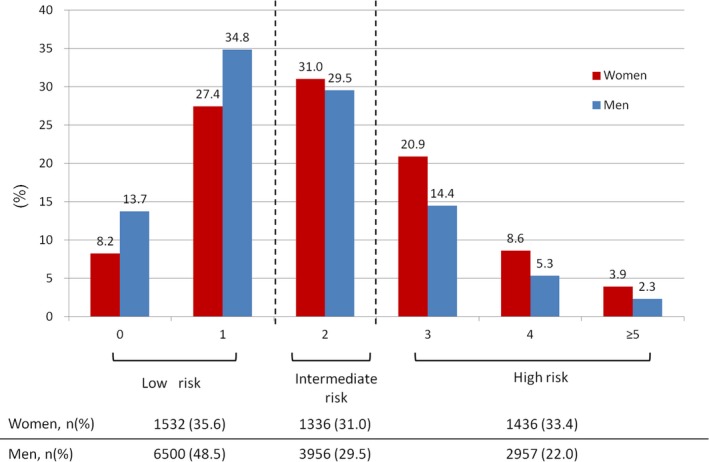
Risk stratification by sex. Approximately half of the men were categorized as low risk, and fewer men were at high risk compared with women.
The benefit of ezetimibe/simvastatin compared with placebo/simvastatin in women for cardiovascular death, MI, or ischemic stroke was most evident in the high‐risk group, demonstrating 7‐year Kaplan‐Meier rates of 38.3% for placebo/simvastatin versus 30.9% for ezetimibe/simvastatin. These findings demonstrated a significant 27% relative risk reduction (HR, 0.73; 0.60–0.89; P=0.001) and a 7.4% absolute reduction (95% CI, 1.4%–13.5%; P=0.016; Figure 5), translating to a number needed to treat of 13 in women (P int=0.046 for treatment and risk group). Men in the high‐risk group experienced 7‐year Kaplan‐Meier rates of 41.1% with placebo/simvastatin versus 35.2% with ezetimibe/simvastatin, with a 15% relative risk reduction (HR, 0.85; 95% CI, 0.74–0.96) and a 5.9% absolute reduction (95% CI, 1.6%–10.1%; Figure 5), yielding a number needed to treat of 17 in men in the high‐risk group (P int=0.13 for treatment and risk group).
Figure 5.

Cumulative incidence of cardiovascular death, myocardial infarction, and ischemic stroke by risk stratification and treatment group in women and men. Each risk indicator (ie, congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, prior stroke, prior coronary artery bypass grafting, peripheral arterial disease, estimated glomerular filtration rate <60 ml/min/1.73 m2, and current smoking) is assigned 1 point. Low risk, 0 or 1 risk indicator; intermediate risk, 2 risk indicators; and high risk, ≧3 risk indicators. Women categorized as high risk benefitted the most from adding ezetimibe to simvastatin, whereas no benefit was observed in women who were categorized as low risk. Eze indicates ezetimibe; HR, hazard ratio; PBO, placebo; Simva, simvastatin.
A similar benefit was observed across the individual composite end points among women in the high‐risk group, in whom the addition of ezetimibe/simvastatin demonstrated a 1.7% absolute risk reduction of cardiovascular death, a significant 5.5% absolute risk reduction of MI, and a 3.3% absolute risk reduction of ischemic stroke.
In the intermediate‐ and lower‐risk groups, there were no significant differences between the 2 treatment groups in either women or men. There was no effect modification of treatment on the outcome of cardiovascular death, MI, or stroke by sex in either an unadjusted analysis (P int=0.29) or after adjustment for the TRS 2°P (P int=0.33).
Safety outcomes
During the study period, 14.5% of women and 12.7% of men permanently discontinued the study drug because of adverse events. Similar to the findings in the overall population, randomization to ezetimibe/simvastatin did not increase the study drug discontinuation rate in either women (14.6% ezetimibe/simvastatin versus 14.3% placebo/simvastatin) or men (12.4% ezetimibe/simvastatin versus 13.1% placebo/simvastatin; P int=0.45).
Overall, rates of the prespecified adverse events of interest (transaminase levels that exceeded 3 times the upper limit of normal, gallbladder‐related adverse events, muscle‐related adverse events, and cancer) were low and more frequently reported in women than in men, with the exception of cancer (Table 3); the overall rate of cancer in men was 10.8% compared with 8.3% in women. No significant treatment differences were observed in either women or men in safety events, including cancer (P>0.05 for each; Table 3), and there was no strong evidence of effect modification by sex on the safety profile of ezetimibe (P int>0.05 for each safety end point). The adverse events were even less frequent in the on‐treatment population, confirming that the addition of ezetimibe did not increase adverse events (P>0.1 for each; Table 4).
Table 3.
Safety Outcomes by Sex (Intention to Treat Population)
| End Points | Sex | Placebo/Simvastatin | Ezetimibe/Simvastatin | P Valuea | P int b |
|---|---|---|---|---|---|
| Permanently stopped study drug because of adverse events | Women | 274 (14.6) | 272 (14.3) | 0.85 | 0.45 |
| Men | 739 (12.4) | 778 (13.1) | 0.27 | ||
| ALT, AST, or both ≥3× ULN | Women | 57 (2.6) | 56 (2.5) | 0.92 | 0.50 |
| Men | 151 (2.2) | 168 (2.5) | 0.31 | ||
| Gallbladder‐related AEs | Women | 95 (4.3) | 86 (3.9) | 0.45 | 0.91 |
| Men | 226 (3.3) | 196 (2.9) | 0.17 | ||
| Rhabdomyolysis | Women | 10 (0.5) | 5 (0.2) | 0.21 | 0.33 |
| Men | 8 (0.1) | 8 (0.1) | >0.99 | ||
| Rhabdomyolysis or myopathy | Women | 15 (0.7) | 10 (0.4) | 0.32 | 0.21 |
| Men | 13 (0.2) | 17 (0.2) | 0.47 | ||
| Rhabdomyolysis, myopathy, or myalgia with CK elevation ≥5× ULN | Women | 24 (1.1) | 13 (0.6) | 0.07 | 0.054 |
| Men | 34 (0.5) | 40 (0.6) | 0.49 | ||
| Cancer | Women | 145 (8.3) | 144 (8.2) | 0.97 | 0.83 |
| Men | 587 (10.8) | 604 (10.8) | 0.53 |
Ezetimibe did not increase the risk of adverse myotoxic events or cancer regardless of sex. Data shown are number (percentage), except for cancer, which is shown as 7‐year Kaplan‐Meier rates. AE indicates adverse event; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CK, creatine kinase; P int, P value for interaction; and ULN, upper limit of normal.
P value comparing treatment within the same sex group.
P int comparing treatment effects between women and men.
Table 4.
Safety Outcomes by Sex (Receiving Treatment)
| End Points | Sex | Placebo/Simvastatin | Ezetimibe/Simvastatin | P Valuea | P int b |
|---|---|---|---|---|---|
| ALT, AST, or both ≥3× ULN | Women | 50 (2.3) | 52 (2.4) | 0.92 | 0.82 |
| Men | 143 (2.1) | 153 (2.3) | 0.56 | ||
| Gallbladder‐related AEs | Women | 72 (3.4) | 63 (2.9) | 0.38 | 0.93 |
| Men | 180 (2.7) | 151 (2.3) | 0.13 | ||
| Rhabdomyolysis | Women | 10 (0.5) | 4 (0.2) | 0.12 | 0.22 |
| Men | 8 (0.1) | 8 (0.1) | >0.99 | ||
| Myopathy | Women | 4 (0.2) | 5 (0.2) | NA | 0.76 |
| Men | 5 (0.1) | 8 (0.1) | 0.42 | ||
| Rhabdomyolysis, myopathy, or myalgia with CK elevation ≥5× ULN | Women | 21 (1.0) | 12 (0.6) | 0.12 | 0.16 |
| Men | 34 (0.5) | 35 (0.5) | 0.90 | ||
| Cancer | Women | 102 (4.8) | 111 (5.1) | 0.62 | 0.41 |
| Men | 453 (6.7) | 454 (6.8) | 0.92 |
Data shown are number (percentage). Treatment effects were all comparable between men and women. AE indicates adverse event; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CK, creatine kinase; NA, not applicable; P int, P value for interaction; and ULN, upper limit of normal.
P value comparing treatment within the same sex group.
P int comparing treatment effects between women and men.
Discussion
IMPROVE‐IT showed that the addition of ezetimibe to simvastatin resulted in a significant reduction of cardiovascular events.14 The current analysis extends these findings and demonstrates that the lipid‐lowering effects of ezetimibe are similar in women and men, with similar reductions of cardiovascular events in women and men. In addition, the safety profile of ezetimibe was similar in women and men, and not different from the placebo group. Our results, which are derived from the largest and longest single trial of more intensive lipid lowering, which included 4416 women, are consistent with the results of the Cholesterol Treatment Trialists' meta‐analyses, in which women and men had similar proportional reductions in cardiovascular events.6 In the current analysis, we further demonstrated that the addition of ezetimibe to simvastatin reduced the total number of events (both first and recurrent) in both women and men.
Previous studies suggest that women hospitalized with an acute coronary syndrome are older and had a higher prevalence of cardiovascular risk factors, including hypertension, hypercholesterolemia, and diabetes mellitus.1, 2, 3, 5 Recently, Bohula et al demonstrated the usefulness of TRS 2°P in identifying high‐risk patients who derive greatest benefit from the addition of ezetimibe to statin therapy in the overall IMPROVE‐IT population.17 When analyzing sex differences in baseline risk using this score, women had more risk indicators compared with men; as such, a significantly higher percentage of women was classified as high risk. This is consistent with our finding of a greater absolute reduction of both primary and total events with the addition of ezetimibe in women than men, despite similar reductions in LDL‐C. Using this simple risk stratification scheme,16 we observed that high‐risk women with ≥3 risk factors had ≈3 times higher rates of cardiovascular events compared with women with ≤1 risk factor. In this high‐risk group, the benefit of ezetimibe appears to start early, contributing to a robust 27% relative and 7.4% absolute risk reduction in the primary end point at 7 years (Figure 5). These results, together with the favorable safety profile of ezetimibe, are important considerations when evaluating the risk‐benefit balance. Furthermore, ezetimibe is now generic in many countries, and this makes its addition to a statin in high‐risk patients particularly attractive.
The current analysis shows that intensive LDL‐C lowering therapy with the addition of ezetimibe to simvastatin reduced the first events and total number of events in women, particularly among women who were at high risk. The benefit of adding ezetimibe in secondary prevention in women appears to be most apparent in the reduction of MI. This may differ from aspirin, with men appearing to derive benefit primarily in the reduction of MI and women in the reduction of ischemic stroke.18
More important, safety events were not increased with ezetimibe in women or men. Although there have been relatively few reports of sex‐specific relationships on adverse events, including muscle‐related events, women are considered to be at higher risk of such events than men, which may contribute to undertreatment. This may be, in part, implicated by sex‐based differences in statin metabolism.19 It is reassuring that our study showed that there was no evidence of increased myopathy, other muscle‐related adverse events, or any other adverse events in women or men, irrespective of treatment assignment.
IMPROVE‐IT enrolled 4416 women and observed them for a median of 6 years, which gave us a unique opportunity to identify and evaluate infrequent adverse events in women. Our findings are in line with a previous study by Bennett et al, which tested the efficacy and safety of statin monotherapy (lovastatin, pravastatin, simvastatin, or atorvastatin) versus ezetimibe plus statin and did not find any sex‐specific differences in ezetimibe‐related adverse effects.20
Several limitations of the present analysis are noteworthy. First, LDL‐C levels were calculated using the Friedewald equation, which may underestimate low levels of LDL‐C. Second, although sex was a prespecified subgroup, we did not adjust for multiple comparisons. Third, as Murphy et al has previously reported, total events analyses may violate the assumption of independence of events, and hence these results need to be cautiously interpreted.15 Fourth, as with other trials, women were underrepresented (24% of participants), and intrinsically, the association between sex and ezetimibe use on outcomes may have been diluted. Despite this, we had the opportunity to study women for >25 000 patient‐years of follow‐up, with 1215 first primary end point events and 2132 total primary end point events. Because of the strict eligibility criteria characteristic of clinical trials, the patients in this study may have been at lower risk than in the general population. However, in this trial, women were an average age of 66 years at enrollment and 72 years at trial completion. Indeed, almost 1000 women were ≥75 years at enrollment.
Conclusion
This prespecified analysis of IMPROVE‐IT demonstrated that adding ezetimibe to statin reduces LDL‐C and cardiovascular events after an acute coronary syndrome, in both women and men. These robust efficacy and safety data support the use of intensive lipid‐lowering therapy with ezetimibe added to a statin, particularly in a high‐risk population of women as well as men, to optimize cardiovascular outcomes.
Sources of Funding
IMPROVE‐IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) was sponsored by Merck & Co, Inc.
Disclosures
Kato has no relationship relevant to the contents of this article to disclose. Blazing has served as an advisory board member for Merck and has provided consulting for AstraZeneca and Novartis. Bohula has received modest consulting fees from Merck and reported research relationships with Eisai and Daiichi‐Sankyo. Park has received grant support from Merck. Murphy has received grant support and honoraria from Merck. Cannon has received grants and/or personal fees from Accumetrics, Arisaph, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Janssen, Daiichi‐Sankyo, Merck, Bristol‐Myers Squibb, CSL Behring, Essentialis, Kowa, Takeda, Lipimedix, Pfizer, Regeneron, Sanofi, Alnylam, and Amgen. Braunwald has received grant support from Merck (to his institution), and has served as an unpaid consultant and advisor to Merck. Giugliano has received grant support from Amgen and Merck (to his institution) and honoraria from the American College of Cardiology, Amgen, Bristol‐Myers Squibb, CVS Caremark, Daiichi Sankyo, GlaxoSmithKline, Merck, Pfizer, and Sanofi. All other authors have reported that they have no relationship relevant to the contents of this article to disclose.
(J Am Heart Assoc. 2017;6:e006901 DOI: 10.1161/JAHA.117.006901.)29151034
References
- 1. Gutierrez J, Ramirez G, Rundek T, Sacco RL. Statin therapy in the prevention of recurrent cardiovascular events: a sex‐based meta‐analysis. Arch Intern Med. 2012;172:909–919. [DOI] [PubMed] [Google Scholar]
- 2. Truong QA, Murphy SA, McCabe CH, Armani A, Cannon CP; TIMI Study Group . Benefit of intensive statin therapy in women: results from PROVE IT‐TIMI 22. Circ Cardiovasc Qual Outcomes. 2011;4:328–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miettinen TA, Pyorala K, Olsson AG, Musliner TA, Cook TJ, Faergeman O, Berg K, Pedersen T, Kjekshus J. Cholesterol‐lowering therapy in women and elderly patients with myocardial infarction or angina pectoris: findings from the Scandinavian Simvastatin Survival Study (4S). Circulation. 1997;96:4211–4218. [DOI] [PubMed] [Google Scholar]
- 4. Kostis WJ, Cheng JQ, Dobrzynski JM, Cabrera J, Kostis JB. Meta‐analysis of statin effects in women versus men. J Am Coll Cardiol. 2012;59:572–582. [DOI] [PubMed] [Google Scholar]
- 5. Lewis SJ, Sacks FM, Mitchell JS, East C, Glasser S, Kell S, Letterer R, Limacher M, Moye LA, Rouleau JL, Pfeffer MA, Braunwald E. Effect of pravastatin on cardiovascular events in women after myocardial infarction: the cholesterol and recurrent events (CARE) trial. J Am Coll Cardiol. 1998;32:140–146. [DOI] [PubMed] [Google Scholar]
- 6. Cholesterol Treatment Trialists' (CTT) Collaboration , Fulcher J, O'Connell R, Voysey M, Emberson J, Blackwell L, Mihaylova B, Simes J, Collins R, Kirby A, Colhoun H, Braunwald E, La Rosa J, Pedersen TR, Tonkin A, Davis B, Sleight P, Franzosi MG, Baigent C, Keech A. Efficacy and safety of LDL‐lowering therapy among men and women: meta‐analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385:1397–1405. [DOI] [PubMed] [Google Scholar]
- 7. Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L, Get With the Guidelines Steering C, Investigators . Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803–2810. [DOI] [PubMed] [Google Scholar]
- 8. Enriquez JR, Pratap P, Zbilut JP, Calvin JE, Volgman AS. Women tolerate drug therapy for coronary artery disease as well as men do, but are treated less frequently with aspirin, beta‐blockers, or statins. Gend. Med. 2008;5:53–61. [DOI] [PubMed] [Google Scholar]
- 9. Koopman C, Vaartjes I, Heintjes EM, Spiering W, van Dis I, Herings RM, Bots ML. Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and treatment of coronary heart disease, 1998–2010. Eur Heart J. 2013;34:3198–205. [DOI] [PubMed] [Google Scholar]
- 10. Poon S, Goodman SG, Yan RT, Bugiardini R, Bierman AS, Eagle KA, Johnston N, Huynh T, Grondin FR, Schenck‐Gustafsson K, Yan AT. Bridging the gender gap: Insights from a contemporary analysis of sex‐related differences in the treatment and outcomes of patients with acute coronary syndromes. Am Heart J. 2012;163:66–73. [DOI] [PubMed] [Google Scholar]
- 11. Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, Brogan GX Jr, Boden WE, Roe MT, Ohman EM, Gibler WB, Newby LK, Investigators C . Gender disparities in the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes: large‐scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. [DOI] [PubMed] [Google Scholar]
- 12. Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, Lindley KJ, Vaccarino V, Wang TY, Watson KE, Wenger NK. American Heart Association Cardiovascular Disease in W , Special Populations Committee of the Council on Clinical Cardiology CoE , Prevention CoC , Stroke N , Council on Quality of C , Outcomes R . Acute myocardial infarction in women: A Scientific statement from the American Heart Association. Circulation. 2016;133:916–947. [DOI] [PubMed] [Google Scholar]
- 13. Cannon CP, Giugliano RP, Blazing MA, Harrington RA, Peterson JL, Sisk CM, Strony J, Musliner TA, McCabe CH, Veltri E, Braunwald E, Califf RM; IMPROVE‐IT Investigators . Rationale and design of IMPROVE‐IT (IMProved Reduction of Outcomes: Vytorin Efficacy International Trial): comparison of ezetimbe/simvastatin versus simvastatin monotherapy on cardiovascular outcomes in patients with acute coronary syndromes. Am Heart J. 2008;156:826–832. [DOI] [PubMed] [Google Scholar]
- 14. Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, Darius H, Lewis BS, Ophuis TO, Jukema JW, De Ferrari GM, Ruzyllo W, De Lucca P, Im K, Bohula EA, Reist C, Wiviott SD, Tershakovec AM, Musliner TA, Braunwald E, Califf RM; IMPROVE‐IT Investigators . Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–2397. [DOI] [PubMed] [Google Scholar]
- 15. Murphy SA, Cannon CP, Blazing MA, Giugliano RP, White JA, Lokhnygina Y, Reist C, Im K, Bohula EA, Isaza D, Lopez‐Sendon J, Dellborg M, Kher U, Tershakovec AM, Braunwald E. Reduction in total cardiovascular events with ezetimibe/simvastatin post‐acute coronary syndrome: the IMPROVE‐IT trial. J Am Coll Cardiol. 2016;67:353–361. [DOI] [PubMed] [Google Scholar]
- 16. Bohula EA, Bonaca MP, Braunwald E, Aylward PE, Corbalan R, De Ferrari GM, He P, Lewis BS, Merlini PA, Murphy SA, Sabatine MS, Scirica BM, Morrow DA. Atherothrombotic risk stratification and the efficacy and safety of vorapaxar in patients with stable ischemic heart disease and previous myocardial infarction. Circulation. 2016;134:304–313. [DOI] [PubMed] [Google Scholar]
- 17. Bohula EA, Morrow DA, Giugliano RP, Blazing MA, He P, Park JG, Murphy SA, White JA, Kesaniemi YA, Pedersen TR, Brady AJ, Mitchel Y, Cannon CP, Braunwald E. Atherothrombotic risk stratification and ezetimibe for secondary prevention. J Am Coll Cardiol. 2017;69:911–921. [DOI] [PubMed] [Google Scholar]
- 18. Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, Hennekens CH, Buring JE. A randomized trial of low‐dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–1304. [DOI] [PubMed] [Google Scholar]
- 19. Anderson GD. Sex and racial differences in pharmacological response: where is the evidence? Pharmacogenetics, pharmacokinetics, and pharmacodynamics. J Womens Health (Larchmt). 2005;14:19–29. [DOI] [PubMed] [Google Scholar]
- 20. Bennett S, Sager P, Lipka L, Melani L, Suresh R, Veltri E. Consistency in efficacy and safety of ezetimibe coadministered with statins for treatment of hypercholesterolemia in women and men. J Womens Health (Larchmt). 2004;13:1101–1107. [DOI] [PubMed] [Google Scholar]


