Abstract
Background
Dispatch of basic life support–trained first responders equipped with automated external defibrillators in addition to advanced life support–trained emergency medical services personnel in out‐of‐hospital cardiac arrest (OHCA) has, in some minor cohort studies, been associated with improved survival. The aim of this study was to evaluate the association between basic life support plus advanced life support response and survival in OHCA at a national level.
Methods and Results
This prospective cohort study was conducted from January 1, 2012, to December 31, 2014. People who experienced OHCA in 9 Swedish counties covered by basic life support plus advanced life support response were compared with a propensity‐matched contemporary control group of people who experienced OHCA in 12 counties where only emergency medical services was dispatched, providing advanced life support. Primary outcome was survival to 30 days. The analytic sample consisted of 2786 pairs (n=5572) derived from the total cohort of 7308 complete cases. The median time from emergency call to arrival of emergency medical services or first responder was 9 minutes in the intervention group versus 10 minutes in the controls (P<0.001). The proportion of patients admitted alive to the hospital after resuscitation was 31.4% (875/2786) in the intervention group versus 24.9% (694/2786) in the controls (conditional odds ratio, 1.40; 95% confidence interval, 1.24–1.57). Thirty‐day survival was 9.5% (266/2786) in the intervention group versus 7.7% (214/2786) in the controls (conditional odds ratio, 1.27; 95% confidence interval, 1.05–1.54).
Conclusions
In this nationwide interventional trial, using propensity score matching, dispatch of first responders in addition to emergency medical services in OHCA was associated with a moderate, but significant, increase in 30‐day survival.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unique identifier: NCT02184468.
Keywords: automated external defibrillator, cardiac arrest, cardiopulmonary resuscitation, defibrillation, dispatch center, emergency medical services, firefighters, first responders, out‐of‐hospital cardiac arrest, survival
Subject Categories: Cardiopulmonary Arrest, Cardiopulmonary Resuscitation and Emergency Cardiac Care
Clinical Perspective
What Is New?
We show improved 30‐day survival in a large‐scale cohort study including >8000 people who experienced out‐of‐hospital cardiac arrest during 3 years. The people who experienced out‐of‐hospital cardiac arrest were subjected to a basic life support/advanced life support intervention with both firefighters and/or police officers (first responders) and emergency medical services, in comparison with emergency medical services dispatch only.
Using a contemporary control group and propensity score analysis enhances the value of the results.
What Are the Clinical Implications?
A basic life support/advanced life support program that includes both first responders and emergency medical services should be considered as one of many important prehospital measures for improving survival in out‐of‐hospital cardiac arrest.
Out‐of‐hospital cardiac arrest (OHCA) annually affects ≈275 000 people in Europe and ≈326 000 people in the United States, with an overall survival rate of ≈10%.1, 2, 3 Cardiopulmonary resuscitation (CPR) before ambulance arrival is associated with an increased chance of survival in cases of OHCA.4, 5, 6, 7 If CPR is provided within minutes of collapse, the length of time of persisting shockable rhythm may be extended, thus prolonging the time span for successful defibrillation.8 Subsequently, if defibrillation with an automated external defibrillator (AED) is performed within minutes of collapse, survival rates in bystander‐witnessed OHCA, with ventricular fibrillation as first rhythm with a presumed cardiac cause, have in some reports been as high as 70%.9, 10 Dispatch of basic life support (BLS)–trained firefighters and police officers (first responders) equipped with AEDs, in addition to dispatch of advanced life support (ALS)–trained emergency medical services (EMS) personnel, would presumably provide these life‐saving services faster because of proximity. In some prospective cohort studies, this has been associated with improved outcome.11, 12, 13 However, the impact of simultaneous BLS+ALS response in cases of OHCA on a larger scale remains unclear. The aim of this study was to evaluate the association between BLS+ALS response and 30‐day survival in OHCA at a national level in Sweden.
Methods
Study Design and Intervention
This was a nationwide, prospective, interventional trial in Sweden. The study intervention was dispatch of BLS‐trained first responders equipped with AEDs in addition to dispatch of ALS‐trained EMS personnel in cases of OHCA. This intervention was compared with a propensity‐matched contemporary control group of OHCA cases where EMS only was dispatched. The study was approved by the Regional Ethics Review Board in Gothenburg (registration number 2011/242–11). No informed consent was required.
Study Participants
Eligible patients were all suspected EMS‐treated OHCA (independent of witnessed status, cardiac rhythm, and previous morbidity) registered in the Swedish Register of Cardiopulmonary Resuscitation. The criterion to activate the BLS+ALS response system was cases in which the dispatcher suspected OHCA, according to the National Medical Index, using various dispatch codes representing cardiac arrest (Table S1). The exclusion criterion was children aged ≤8 years (pediatric life support training was not mandatory among all first responders). EMS crew‐witnessed OHCA, patients with obvious signs of death, and people with existing Do Not Attempt Resuscitation orders, where no CPR was initiated by the EMS, were also excluded. Patients included in the analysis of primary outcome were as follows: (1) OHCA receiving BLS+ALS response in the intervention counties and (2) propensity score analysis–matched ALS cases from the control counties fulfilling the above‐listed criteria. Thus, cases in intervention counties that, for any reason, were not receiving BLS+ALS response were not included in the analysis.
Setting
Of 21 counties in Sweden, 9 were selected for the intervention: Stockholm, Södermanland, Uppsala, Jönköping, Halland, Västra Götaland, Kalmar, Dalarna, and Jämtland (Figure 1). These counties were chosen on the basis of a geographical perspective and a population‐density perspective. Overall, these 9 counties comprise ≈5.7 million inhabitants and an estimated 59% of the Swedish population of 9.9 million inhabitants. The control group, for whom EMS only was dispatched, incorporated a total population of 3 991 498 (41%) in 12 counties. Population densities in both groups varied from densely populated areas (>5000 inhabitants/km2) to more rural regions (<100/km2). In 3 intervention counties (Västra Götaland, Kalmar, and Uppsala), not all the population was covered by the BLS+ALS response. In 2 of the intervention counties (Stockholm and Södermanland), the BLS+ALS response had been implemented before the study period. In 1 intervention county (Halland), only police officers were dispatched, and in 1 county (Stockholm), both firefighters and police officers were dispatched. Different counties joined the project stepwise from January 1, 2012, to February 1, 2014, as shown in Figure 2.
Figure 1.
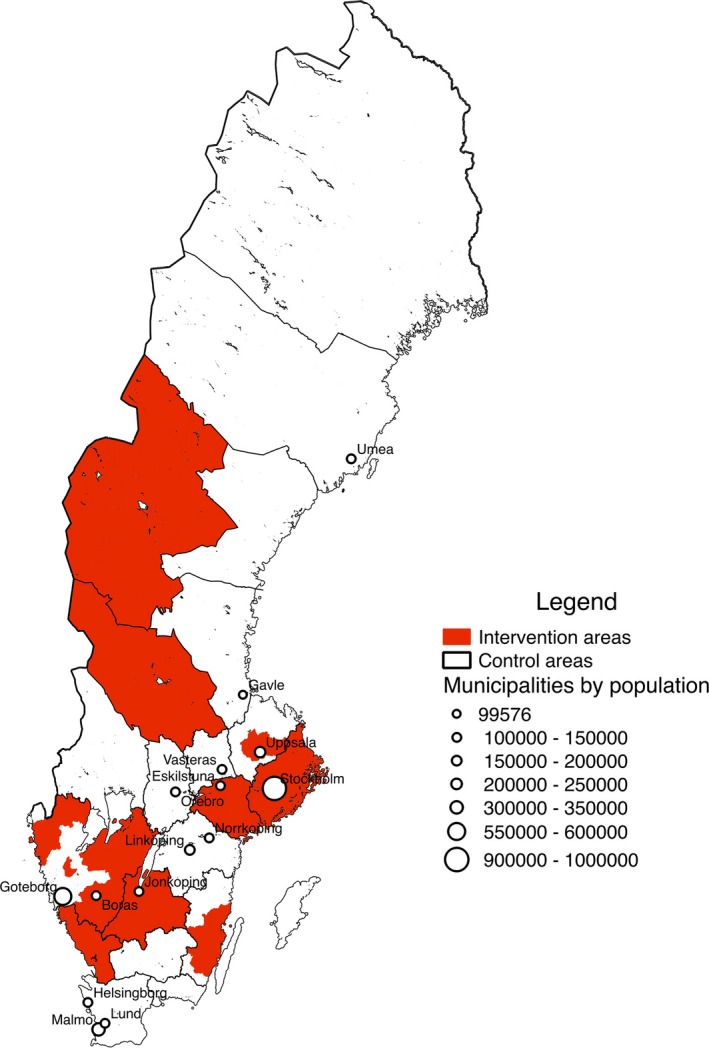
Map of Sweden with intervention and control counties.
Figure 2.
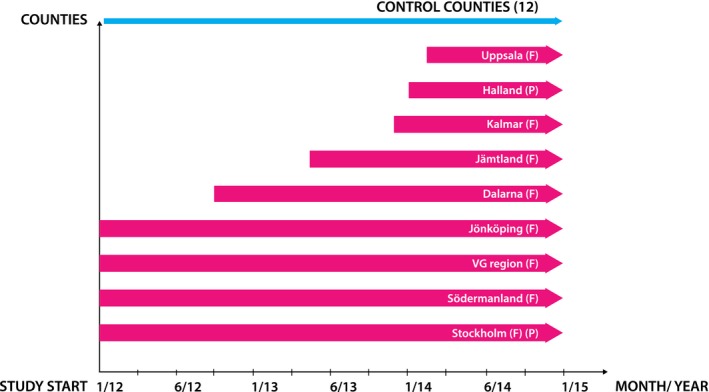
Timing of study participation for intervention counties. F indicates firefighters; P, police; VG, Västra Götaland.
EMS and Dispatch Organization
Ambulances in Sweden are usually staffed with registered or specialist nurses or emergency medical technicians, and 2 ambulances are dispatched in case of suspected OHCA. Annually, the staff is trained in ALS, according to European Resuscitation Council guidelines.14 When an emergency call is received at the Emergency Medical Communication Center (EMCC), the nearest available EMS is dispatched; simultaneously in the intervention counties, an alarm is transmitted to the Rescue Dispatch Center for dispatch of the fire brigade, who dispatch 1 fire vehicle staffed with up to 5 firefighters. For dispatching of the police, a telephone call is made from the EMCC to the Police Communication Center. All dispatchers follow the Swedish Index for Emergency Medical Assistance and international guidelines in adult BLS when assessing a suspected OHCA.15 In the intervention counties, all participating first responders underwent a 4‐hour course in adult BLS and defibrillation with an AED, according to international guidelines.15
In the control counties, no routine simultaneous BLS+ALS response took place. However, if no EMS was present in the vicinity of the person experiencing OHCA (ie, within 10–20 minutes from the scene), the dispatcher also had the option to dispatch the nearest fire brigade instead. This mode of operation is commonly used in less well‐populated areas of Sweden in connection with medical conditions, such as acute myocardial infarction and stroke, and cases of suspected OHCA. Most in this group of firefighters are part‐time employees and hold civil occupations, but they are alerted from their work in cases of emergency.
Outcomes
The primary outcome measure was 30‐day survival. Follow‐up time regarding survival differences between treated and control cases from event to 11 months is estimated and presented in Figure S1. Secondary outcomes were as follows: (1) the proportion of patients admitted alive to the hospital and (2) the time interval from emergency call to arrival at the scene of first responders or EMS. The main exposure was treatment, defined as dispatch of first responders to perform CPR and potentially defibrillation with an AED.
Data Sources
Three different data sources were used: (1) The EMCC, which keeps a case number for individual patient identification. The EMCC also obtains and digitally records all important time measurements regarding the emergency call, such as time of dispatch and time of arrival of EMS, as well as geographical x and y coordinates for all cases of OHCA. (2) The Swedish Register of Cardiopulmonary Resuscitation, to which EMS crews report OHCA resuscitation interventions, according to the Utstein template. The register is of national quality and has been described previously.16 (3) The Swedish Civil Contingencies Agency database, which annually includes reports from all fire brigade missions in Sweden regardless of the type of event. The following data were obtained: The specific fire brigade reporting the cardiac arrest mission, the case number from the EMCC, and the time from dispatch to arrival at the scene.
Linking the data is performed by using the unique case number created when the dispatcher at the EMCC answers the call. This case number is transferred to both the ambulance and the fire/police department and later saved in all data sources. Validity checks were performed using the case number and the date/time stamp to make sure that the cases matched temporally. Cases that could not be matched were discarded in the flow chart.
Statistical Analysis
Sample size was estimated as 6000 bystander‐witnessed OHCA cases, for an increase in 30‐day survival from 9% to 12% on a national level, with power set at 0.80 with an α error of 0.05. To reduce the risk for observed confounding factors, a propensity score–matching analysis was used. The propensity score for treatment was calculated by using the MatchIt package in R (R for Mac version 3.2.3). We used 1:1 nearest neighbor matching without replacement and no specified caliper width to assign a suitable control case for each treated case. The following Utstein variables17 were used to calculate the propensity score for treatment: bystander CPR (yes versus no), sex (male versus female), age (in years), cause (cardiac versus noncardiac), witnessed status (witnessed versus not witnessed), location (home versus outside home), EMS response time (in categories), and dispatcher‐identified presence of cardiac arrest. Furthermore, the year and time of day (day/night) were also included. Variables not used in the propensity score calculation, but presented in baseline characteristics, were initial rhythm (ventricular fibrillation/ventricular tachycardia versus asystole/pulseless electrical activity [cardiac]), public defibrillation (yes versus no), and EMS response time (in minutes). Cases in both the intervention and control groups were discarded if they were ineligible for matching.
Differences in distributions of covariates were assessed by standardized mean differences (SMDs). Odds ratios and 95% confidence intervals for the outcome variables were calculated by means of conditional logistic regression, conditioned on the matched pairs from the propensity score calculation specified above. Kaplan–Meier plots with 11‐month survival were plotted to show long‐term differences between the treated and control cases. Time to event was calculated from the date of OHCA to the date of death (Figure S1).
We used Rosenbaum bounds to test how sensitive our results were to unobserved confounding.18 The sensitivity analysis was conducted using the rbounds package in R.
Results
From January 1, 2012, to December 31, 2014, 15 323 OHCAs occurred in Sweden, for which EMS crews started CPR. Of these OHCAs, 8988 (58.7%) occurred in intervention counties and 6335 (41.3%) occurred in control counties (Figure 3). After discarding EMS‐witnessed cases (n=1385), pediatric patients aged ≤8 years (n=90), and missing data from a private dispatch center (n=502), 7011 OHCAs remained in the intervention counties; 3543 (50.5%) involved a BLS+ALS response. These cases were matched with patients from control counties, leaving a total of 2786 pairs (n=5572) derived from 7308 complete cases for analysis of the primary outcome.
Figure 3.
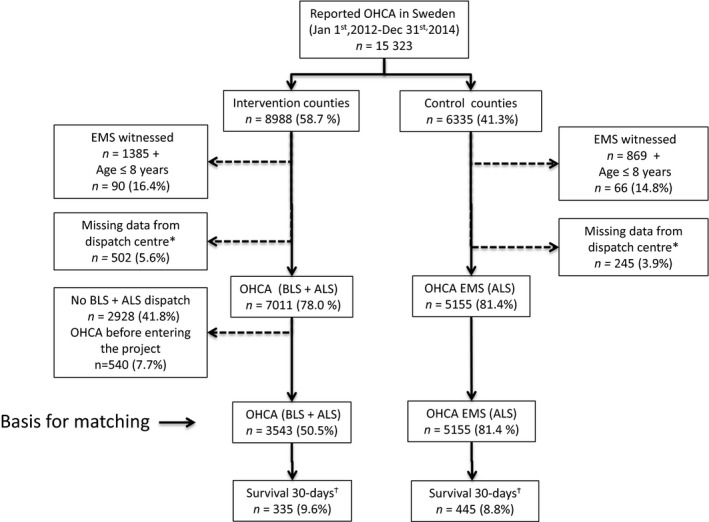
Flow chart of patient inclusion. ALS indicates advanced life support; BLS, basic life support; EMS, emergency medical services; OHCA, out‐of‐hospital cardiac arrest. *Missing OHCA cases from January 1, 2012, to November 26, 2013, in the intervention county of Södermanland (Sweden) because dispatch of ambulances during the time period was undertaken by a private company. †Missing outcome in the control and intervention groups (n=103 and n=66, respectively).
Baseline Characteristics Before Matching
Demographics and baseline characteristics are presented in Table 1. The proportion of cases indexed as probable OHCA at the EMCC was lower in the control group (70.3% [3623/5155]) compared with the intervention group (76.2% [2701/3543]; SMD, 0.135). The EMS response time distribution differs, with a higher proportion of cases with shorter response time in the control group (SMD, 0.126). The other baseline variables did not differ substantially and had an SMD of <0.1.
Table 1.
Baseline Characteristics Before and After Propensity Score Matching
| Characteristics | Before Propensity Score Matching | After Propensity Score Matching | ||||
|---|---|---|---|---|---|---|
| Intervention (BLS+ALS) (n=3543)a | Control (ALS) (n=5155)a | Intervention (BLS+ALS) (n=2786)a | Control (ALS) (n=2786)a | |||
| SMD | SMD | |||||
| Year | ||||||
| 2012 | 961 (27.1) | 1541 (29.9) | 0.066 | 601 (21.6) | 586 (21.0) | 0.018 |
| 2013 | 1204 (34.0) | 1739 (33.7) | 1028 (36.9) | 1019 (36.6) | ||
| 2014 | 1378 (38.9) | 1875 (36.4) | 1157 (51.5) | 1181 (42.4) | ||
| Time of day | ||||||
| Day 7–18 | 2190 (65.9) | 3318 (64.4) | 0.033 | 1822 (65.4) | 1817 (65.2) | 0.004 |
| Sex | ||||||
| Female | 1132 (32.0) | 1639 (31.8) | 0.004 | 905 (32.5) | 878 (31.5) | 0.021 |
| Location | ||||||
| Outside home | 1040 (29.4) | 1431 (27.8) | 0.035 | 725 (26.0) | 710 (25.5) | 0.012 |
| Witnessed | ||||||
| Yes | 2001 (58.3) | 3062 (60.5) | 0.045 | 1632 (58.6) | 1655 (59.4) | 0.017 |
| BY‐CPR | ||||||
| Yes | 2039 (58.2) | 2870 (56.0) | 0.045 | 1650 (59.2) | 1623 (58.3) | 0.020 |
| Rhythm | ||||||
| VF/VT | 761 (22.0) | 1091 (22.2) | 0.003 | 595 (21.8) | 586 (21.8) | <0.001 |
| INDEXED as | ||||||
| Cardiac arrest | 2701 (76.2) | 3623 (70.3) | 0.135 | 2265 (81.3) | 2256 (81.0) | 0.008 |
| Cause | ||||||
| Cardiac | 3027 (88.8) | 4476 (89.1) | 0.011 | 2392 (85.9) | 2411 (86.5) | 0.020 |
| Public Defib | ||||||
| Yes | 65 (1.8) | 94 (1.8) | 0.001 | 50 (1.8) | 47 (1.7) | 0.008 |
| Age, median (Q1–Q3), y | 71 (60–81) | 71 (60–80) | 0.033 | 71 (61–81) | 71 (61–81) | 0.005 |
| Call—arrival EMS, median (Q1–Q3), minutes | 12 (8–17) | 12 (8–18) | 0.043 | 12 (8–17) | 12 (8–18) | 0.048 |
| Call—arrival EMS, minutes | 0.126 | 0.026 | ||||
| 0–4 | 56 (1.7) | 98 (2.0) | 49 (1.8) | 51 (1.8) | ||
| 5–7 | 530 (15.8) | 945 (19.4) | 441 (15.8) | 421 (15.1) | ||
| 8–11 | 987 (29.4) | 1269 (26.0) | 819 (29.4) | 808 (29.0) | ||
| 12–15 | 692 (20.6) | 892 (18.3) | 567 (20.4) | 569 (20.4) | ||
| >16 | 1091 (32.5) | 1676 (34.3) | 910 (32.7) | 937 (33.6) | ||
The percentages of cases with missing data for each variable before matching were the following in the intervention/control groups: year, 0%/0%; daytime, 6.3%/0%; sex, 0.1%/0%; location, 0%/0%; witnessed, 3.1%/1.8%; BY‐CPR, 1.1%/0.5%; VF/VT, 2.5%/4.5%; indexed as out‐of‐hospital cardiac arrest, 0%/0%; cause, 3.8%/2.5%; Public Defib, 0%/0%; age, 5.2%/1.9%; call—arrival EMS, 5.3%/5.3%. Variables used in propensity score matching: BY‐CPR, sex, age, cause, witnessed status, location, EMS response time, indexed as cardiac arrest, year, and time of day. ALS indicates advanced life support; BLS, basic life support; BY‐CPR, bystander cardiopulmonary resuscitation; EMS, emergency medical services; INDEXED, indexed as cardiac arrest at dispatch center; Public Defib, public access defibrillation; Q1, quartile 1; Q3, quartile 3; SMD, standardized mean difference; VF/VT, ventricular fibrillation/ventricular tachycardia.
Data are given as number (percentage) unless otherwise indicated.
After Propensity Score Matching
The intervention and control groups did not differ substantially in any of the covariates after propensity score matching. The largest SMD was found in response time (as a continuous variable), with a value of 0.048.
Primary Outcome
Outcome data before and after matching are presented in Table 2. The proportion of patients admitted alive to the hospital was 31.4% (875/2786) in the intervention group versus 24.9% (694/2786) in the control group (conditional odds ratio, 1.40; 95% confidence interval, 1.24–1.57). Thirty‐day survival was 9.5% (266/2786) in the intervention group versus 7.7% (214/2786) in the controls (conditional odds ratio, 1.27; 95% confidence interval, 1.05–1.54).
Table 2.
Outcome Before and After Propensity Score Matching
| Outcome | Before Propensity Score Matchinga | After Propensity Score Matchinga | Γb | |||
|---|---|---|---|---|---|---|
| Intervention (BLS+ALS) (n=3543) | Control (ALS) (n=5155) | Intervention (BLS+ALS) (n=2786) | Control (ALS) (n=2786) | |||
| OR (95% CI) or P Value | ||||||
| First R first on scene | 1571 (44.3) | 950 (18.4) | 1314 (47.2) | 570 (20.5) | 3.69 (3.23–4.21) | 3.3 |
| Defib by First R | 253 (7.1) | 333 (6.5) | 165 (5.9) | 112 (4.4) | 1.40 (1.09–1.80) | 1.14 |
| VF/VT | 154 (20.2) | 142 (13.0) | 132 (22.2) | 74 (12.6) | P<0.001c | |
| Admitted alive | 1143 (32.4) | 1331 (26.2) | 875 (31.4) | 694 (24.9) | 1.40 (1.24–1.57) | 1.26 |
| VF/VT | 426 (56.6) | 534 (49.5) | 332 (55.8) | 280 (47.8) | P 0.006c | |
| 30‐d Survival | 335 (9.6) | 445 (8.8) | 266 (9.5) | 214 (7.7) | 1.27 (1.05–1.54) | 1.09 |
| VF/VT | 217 (29.6) | 288 (27.0) | 181 (30.4) | 143 (24.4) | P 0.020c | |
| Call—arrival First R, median (Q1–Q3), minutes | 9 (7–13) | 10 (7–15) | 9 (7–13) | 10 (8–15) | P<0.001d | |
The percentages of cases with missing data for each variable before propensity score matching were the following in intervention/control groups: first responder first on scene, 0%/0%; defibrillation by first responder, 0%/0%; admitted alive, 0.6%/1.5%; 30‐day survival, 1.9%/2.0%; call—arrival first responder, 5.6%/5.8%. ALS indicates advanced life support; BLS, basic life support; Call—arrival First R indicates emergency call to arrival of first responders on scene; CI, confidence interval; Defib by First R, defibrillation by first responders; First R, first responders; OR, odds ratio; Q1, quartile 1; Q3, quartile 3; VF/VT, ventricular fibrillation/ventricular tachycardia.
Data are given as number (percentage) unless otherwise indicated.
Rosenbaum bounds.
χ2 Test.
Wilcoxon signed‐rank test.
Secondary Outcomes
Data on secondary outcomes are presented in Table 2. After propensity score matching, first responders were first to arrive on the scene in 1314 (47.2%) of cases in the intervention group, compared with 570 (20.5%) of cases in the control group (conditional odds ratio, 3.69; 95% confidence interval, 3.23–4.21).
The time from the emergency call to arrival at the scene of the first unit (first responder or EMS) was 9 minutes (interquartile range, 7–13 minutes) in the intervention group versus 10 minutes (interquartile range, 8–15 minutes) in the control group (P<0.001).
In a subgroup analysis of patients in ventricular fibrillation, we have used the 2 major EMCC dispatch codes for OHCA: (1) unconscious adult—unresponsive and not breathing normally and (2) unconscious adult—ongoing CPR. As seen in Table 3, the proportion of patients defibrillated before EMS arrival was 85 (24.6%) in the intervention group versus 49 (14.9%) in the control group (P=0.002). Thirty‐day survival for OHCA with ventricular fibrillation was 109 (31.5%) in the intervention group compared with 76 (23.1%) in the control group (P=0.018).
Table 3.
Outcome of VF Cases
| Outcome | Intervention Group | Control Group | P Value |
|---|---|---|---|
| (n=346) | (n=329) | ||
| First R first on scene | 162 (46.8) | 62 (18.8) | <0.001 |
| Defib by First R | 85 (24.6) | 49 (14.9) | 0.002 |
| Admitted alive | 208 (60.1) | 152 (46.2) | <0.001 |
| 30‐d Survival | 109 (31.5) | 76 (23.1) | 0.018 |
| Call arrival First R, median (IQR), minutes | 8.50 (7.00–11.25) | 9.00 (7.00–13.00) | 0.009 |
Data are given as number (percentage) unless otherwise indicated. Defib indicates defibrillation; First R, first responders; IQR, interquartile range; VF, ventricular fibrillation.
Sensitivity Analysis
The results from the Rosenbaum bounds analysis are shown in Table 2. There were 190 strata where the control cases survived and treated cases (intervention) died compared with 242 strata where the treated cases survived and the control cases died. This results in a Rosenbaum bounds of 1.09.
Discussion
We report data from a national, prospective, interventional trial in which dispatch of BLS‐trained first responders equipped with AEDs in addition to ALS‐trained EMS has been evaluated compared with EMS only in cases of OHCA. To our knowledge, this is to date the largest first‐responder study within the field of cardiac arrest, with >8000 patients included. Our main finding is that dual BLS+ALS response is associated with moderate, but significantly, improved 30‐day survival compared with dispatch of EMS only. Besides improved 30‐day survival, we also found a significant increase in the proportion of patients admitted to the hospital alive, which indicates that the benefit originates from prehospital actions. In the intervention counties, first responders were first on the scene, initiating CPR and connecting an AED in almost half of the OHCA cases. Among cases with a shockable rhythm, a first responder defibrillated 24.6% of them before EMS arrival. This finding is important, and we suggest that the time reduction achieved by using BLS+ALS response leads to a position in which more people can be defibrillated swiftly. In addition to the time benefit of 1 minute for arrival at the scene of the arrest, there may be several other strengths of intervention via a BLS+ALS system. Dispatch of first responders brings more trained personnel to perform resuscitation and may improve important factors, such as the quality of CPR, hands‐off time, and preshock pauses.19, 20
The observed 30‐day survival in the study (9.5% versus 7.7%) was lower than the anticipated (12% versus 9%) increase in survival for witnessed OHCA in Sweden. One reason for this might be that, in patients in whom the OHCA occurred after the EMS dispatch, no BLS+ALS dispatch was triggered at the EMCC (according to the study design) and, subsequently, these cases were not included in the analysis for primary outcome.
The main impact on 30‐day survival in our trial was seen in patients with shockable rhythm, and this is in line with previous findings.11, 12, 21 This raises the question of which patients to include in a cardiac arrest study. When narrowing down the dispatch codes to the 2 major ones for adult cardiac arrests, and analyzing outcome for shockable rhythms, we found a stronger effect of the intervention compared with the whole group. This is discussed by Weisfeldt,22 who advocates inclusion only of witnessed arrests with shockable rhythms in randomized arrest trials. However, we also recognize that narrowing the triggering criteria for dispatch of first responders to only those with certain cardiac arrest would lead to the risk that some cases who would truly benefit from the intervention will not receive the treatment. The importance of having a community‐wide perspective needs to be underlined when resources other than EMS are used in treating medical emergencies. Although the effect of this type of intervention may be seen only in subgroups of the cardiac arrest population, we suggest wide inclusion criteria when dispatching, as it seems difficult for dispatchers at the EMCC to recognize an OHCA accurately during the first crucial minutes.23, 24, 25
A positive association between BLS+ALS response and survival in cases of OHCA has been found in other more regional settings, where EMS only has been compared with BLS+ALS response with a second tier of firefighters,13 police officers,11 or both.26, 27 However, there are some important differences. First, compared with previous studies, we have a broad nationwide perspective in which the intervention counties embrace >50% of the population. Second, we used a contemporary control population and not a historical control group, which has most often been the case in earlier studies. Third, we have used matched pairs with similar covariate distribution for known outcome predictors in OHCA to reduce confounding. Randomized clinical trials are considered to represent the gold standard in clinical evaluations, but in the present setting in Sweden, such a trial was not possible in the light of ethical considerations arising from the results of previous research.12, 28
In the intervention group, first responders were first on the scene in 1314 (47.2%) of the 2786 cases (Table 2). This is in line with the results of previous studies and probably, to a large extent, explains the shortened time intervals and improved outcome. However, one surprising finding was that, in matched cases in the control group, first responders were first on the scene in 20% of cases. This is explained by the fact that if no EMS was present in the vicinity of the person experiencing OHCA (ie, within 10–20 minutes), the dispatcher also had the option to dispatch the nearest fire brigade instead. It is important to stress that the control counties had no routine simultaneous BLS+ALS response. One can speculate that the positive outcome difference in this trial (ie, increased 30‐day survival and admission to the hospital) might have been even larger if true BLS+ALS cases were to have been compared with cases in control counties with no first responders.
It is difficult to compare outcomes in different settings, populations, dispatch organizations, and types of EMS systems. Several studies have included a limited number of OHCA patients and have covered short time spans, thus making comparisons challenging.29, 30 However, if we extrapolate the survival rates from this study (Table 2), with an increase in survival from 7.7% to 9.5%, 99 more lives could be saved annually, with a reported incidence of 5500 OHCA treatments in 2016 in Sweden.31
The study has several strengths. First, it covers a 3‐year time period and includes a large sample of OHCA patients. It includes a spread of patients from both urban and rural parts, as well as from highly versus sparsely populated areas. Second, unlike most other BLS+ALS studies, the intervention group was not compared with historical controls, but with OHCA cases occurring during the same time period. Thus, we could avoid confounding by guideline changes in CPR treatment. Third, we have used matched pairs with similar covariate distribution for known outcome predictors in OHCA to reduce confounding.
The study also has several limitations. First, it was not a randomized controlled trial, thus making it more difficult to draw true conclusions about causality. Second, propensity score matching is a method to control for confounding factors in interventional studies, and we matched for the most commonly used variables in cardiac arrest research; however, residual confounding among variables not matched for could still be present. A low λ number for the primary outcome, 30‐day survival, indicates this (Table 2), meaning that an unobserved confounder that changes the odds of receiving treatment with 1.09 and predicts outcome would change the inference of the study. An example of a factor that may have affected the results is socioeconomic status among people experiencing OHCA, as has been demonstrated in earlier OHCA studies.32, 33
Third, when using registry data, the results have limitations arising from missing or incorrectly reported variables. Fourth, we did not control for in‐hospital measures, such as therapeutic hypothermia, coronary angiography, and revascularization. Fifth, neurological outcome was not presented because of scarce data for patient‐reported outcome measures for surviving OHCA patients during the study period.
Sixth, this study rationale did not have an intention to examine the cost‐effectiveness of the intervention. Even if additional costs could be a potential barrier to a large‐scale implementation to improve survival from OHCA, previous data indicate that with BLS+ALS dispatch the return on investment is high. The cost‐effectiveness shows levels that are lower than the threshold value for economic efficiency used in Sweden.34 Seventh, only ≈40% of all OHCAs in the intervention counties were dispatched as BLS+ALS. There are several traceable explanations for this: exclusion criteria (aged ≤8 years, EMS crew‐witnessed OHCA, and patients with obvious signs of death), missing data at dispatch centers, and the fact that some interventional counties did not enter the study from the start (Figure 2). Still, many cases were not dispatched as BLS+ALS. We believe the 2 most probable reasons for this study flaw are as follows: (1) OHCA occurring between the call to the dispatch center and arrival of already dispatched EMS and (2) failure of OHCA recognition at the dispatch center. This probable failure of OHCA recognition is a well‐known factor24, 25 and occurs despite extensive educational efforts at dispatch centers; we believe this illustrates a real‐life situation problem. This might be a limitation in terms of selection bias (ie, dispatchers chose/had some incentive to BLS+ALS dispatch in some cases but not others). Furthermore, we have analyzed those cases not included in the propensity score analysis, with the same main finding for primary outcome (Tables S2 and S3).
Conclusions
In conclusion, this nationwide intervention trial showed that BLS+ALS response was associated with moderate, but significantly, increased 30‐day survival in cases of OHCA. Furthermore, a higher proportion of patients were admitted alive to the hospital compared with those in a control group in which only EMS was dispatched. Response times could be reduced, and first responders were first on the scene in almost half of the cases and could initiate CPR and attach an AED before EMS arrival. The benefit of BLS+ALS response appears to be more powerful in the subgroup of patients in shockable rhythms. These results support the implementation of a BLS+ALS response system with trained first responders equipped with AEDs as one of several evidence‐based interventions that have been demonstrated to improve survival from OHCA.
Sources of Funding
Sources of funding were the Swedish Heart–Lung Foundation, the National Board of Health and Welfare in Sweden, and the Laerdal Foundation for Acute Medicine in Norway. The sponsors had no role in the study design, analysis, and interpretation of the data, or writing of the manuscript
Disclosures
None.
Supporting information
Table SI. Dispatch Codes for Cardiac Arrest Used at the Emergency Medical Coordination Center
Table SII. Baseline Characteristics of Patients Not Included in Control or Intervention Group
Table SIII. Outcome Variables for Patients Not Included in Control or Intervention Group
Table SIV. Discarded Unmatched Cases
Table SV. Indexed as CA Using the 2 Major Dispatch Codes: Unconscious Adult—Unresponsive and Not Breathing Normally, Unconscious Adult—Ongoing Cardiopulmonary Resuscitation
Table SVI. Indexed as CA Using the 2 Major Dispatch Codes: Unconscious Adult—Unresponsive and Not Breathing Normally, Unconscious Adult—Ongoing Cardiopulmonary Resuscitation
Figure SI. Kaplan–Meier survival curve for control and intervention groups after propensity score matching.
Figure SII. Histogram of propensity scores before and after matching.
Figure SIII. Jitter plot of propensity scores for matched and unmatched cases.
Figure SIV. Proportion of cases arrived at scene in different time intervals in control and intervention groups.
Acknowledgments
We sincerely thank all first responders, emergency medical services crews, dispatchers, research coordinators, and medical directors in the counties who participated in this study.
(J Am Heart Assoc. 2017;6:e005873 DOI: 10.1161/JAHA.117.005873.)
References
- 1. Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS‐treated out‐of‐hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. [DOI] [PubMed] [Google Scholar]
- 2. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out‐of‐hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. [DOI] [PubMed] [Google Scholar]
- 3. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics 2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 4. Lund I, Skulberg A. Cardiopulmonary resuscitation by lay people. Lancet. 1976;2:702–704. [DOI] [PubMed] [Google Scholar]
- 5. Cummins RO, Eisenberg MS, Hallstrom AP, Litwin PE. Survival of out‐of‐hospital cardiac arrest with early initiation of cardiopulmonary resuscitation. Am J Emerg Med. 1985;3:114–119. [DOI] [PubMed] [Google Scholar]
- 6. Waalewijn RA, Tijssen JG, Koster RW. Bystander initiated actions in out‐of‐hospital cardiopulmonary resuscitation: results from the Amsterdam Resuscitation Study (ARRESUST). Resuscitation. 2001;50:273–279. [DOI] [PubMed] [Google Scholar]
- 7. Hasselqvist‐Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out‐of‐hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. [DOI] [PubMed] [Google Scholar]
- 8. Waalewijn RA, Nijpels MA, Tijssen JG, Koster RW. Prevention of deterioration of ventricular fibrillation by basic life support during out‐of‐hospital cardiac arrest. Resuscitation. 2002;54:31–36. [DOI] [PubMed] [Google Scholar]
- 9. Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. [DOI] [PubMed] [Google Scholar]
- 10. Ringh M, Jonsson M, Nordberg P, Fredman D, Hasselqvist‐Ax I, Hakansson F, Claesson A, Riva G, Hollenberg J. Survival after public access defibrillation in Stockholm, Sweden: a striking success. Resuscitation. 2015;91:1–7. [DOI] [PubMed] [Google Scholar]
- 11. Myerburg RJ, Fenster J, Velez M, Rosenberg D, Lai S, Kurlansky P, Newton S, Knox M, Castellanos A. Impact of community‐wide police car deployment of automated external defibrillators on survival from out‐of‐hospital cardiac arrest. Circulation. 2002;106:1058–1064. [DOI] [PubMed] [Google Scholar]
- 12. Hollenberg J, Riva G, Bohm K, Nordberg P, Larsen R, Herlitz J, Pettersson H, Rosenqvist M, Svensson L. Dual dispatch early defibrillation in out‐of‐hospital cardiac arrest: the SALSA‐pilot. Eur Heart J. 2009;30:1781–1789. [DOI] [PubMed] [Google Scholar]
- 13. Saner H, Morger C, Eser P, von Planta M. Dual dispatch early defibrillation in out‐of‐hospital cardiac arrest in a mixed urban‐rural population. Resuscitation. 2013;84:1197–1202. [DOI] [PubMed] [Google Scholar]
- 14. Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, Perkins GD. European Resuscitation Council guidelines for resuscitation 2010 section 4: adult advanced life support. Resuscitation. 2010;81:1305–1352. [DOI] [PubMed] [Google Scholar]
- 15. Koster RW, Baubin MA, Bossaert LL, Caballero A, Cassan P, Castren M, Granja C, Handley AJ, Monsieurs KG, Perkins GD, Raffay V, Sandroni C. European Resuscitation Council guidelines for resuscitation 2010 section 2: adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81:1277–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stromsoe A, Svensson L, Axelsson AB, Goransson K, Todorova L, Herlitz J. Validity of reported data in the Swedish Cardiac Arrest Register in selected parts in Sweden. Resuscitation. 2013;84:952–956. [DOI] [PubMed] [Google Scholar]
- 17. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, Deakin CD, Finn JC, Grasner JT, Hazinski MF, Iwami T, Koster RW, Lim SH, Ma MH, McNally BF, Morley PT, Morrison LJ, Monsieurs KG, Montgomery W, Nichol G, Okada K, Ong ME, Travers AH, Nolan JP. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out‐of‐hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–340. [DOI] [PubMed] [Google Scholar]
- 18. Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wik L, Kramer‐Johansen J, Myklebust H, Sorebo H, Svensson L, Fellows B, Steen PA. Quality of cardiopulmonary resuscitation during out‐of‐hospital cardiac arrest. JAMA. 2005;293:299–304. [DOI] [PubMed] [Google Scholar]
- 20. Takei Y, Nishi T, Matsubara H, Hashimoto M, Inaba H. Factors associated with quality of bystander CPR: the presence of multiple rescuers and bystander‐initiated CPR without instruction. Resuscitation. 2014;85:492–498. [DOI] [PubMed] [Google Scholar]
- 21. Nordberg P, Hollenberg J, Rosenqvist M, Herlitz J, Jonsson M, Jarnbert‐Petterson H, Forsberg S, Dahlqvist T, Ringh M, Svensson L. The implementation of a dual dispatch system in out‐of‐hospital cardiac arrest is associated with improved short and long term survival. Eur Heart J Acute Cardiovasc Care. 2014;3:293–303. [DOI] [PubMed] [Google Scholar]
- 22. Weisfeldt ML. Stop randomizing all cardiac arrests. Circulation. 2016;134:2035–2036. [DOI] [PubMed] [Google Scholar]
- 23. Berdowski J, Beekhuis F, Zwinderman AH, Tijssen JG, Koster RW. Importance of the first link: description and recognition of an out‐of‐hospital cardiac arrest in an emergency call. Circulation. 2009;119:2096–2102. [DOI] [PubMed] [Google Scholar]
- 24. Vaillancourt C, Charette M, Kasaboski A, Hoad M, Larocque V, Crete D, Logan S, Lamoureux P, McBride J, Cheskes S, Wells GA, Stiell IG. Cardiac arrest diagnostic accuracy of 9‐1‐1 dispatchers: a prospective multi‐center study. Resuscitation. 2015;90:116–120. [DOI] [PubMed] [Google Scholar]
- 25. Moller TP, Andrell C, Viereck S, Todorova L, Friberg H, Lippert FK. Recognition of out‐of‐hospital cardiac arrest by medical dispatchers in emergency medical dispatch centres in two countries. Resuscitation. 2016;109:1–8. [DOI] [PubMed] [Google Scholar]
- 26. Stiell IG, Wells GA, Field BJ, Spaite DW, De Maio VJ, Ward R, Munkley DP, Lyver MB, Luinstra LG, Campeau T, Maloney J, Dagnone E. Improved out‐of‐hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: OPALS study phase II. JAMA. 1999;281:1175–1181. [DOI] [PubMed] [Google Scholar]
- 27. Malta Hansen C, Kragholm K, Pearson DA, Tyson C, Monk L, Myers B, Nelson D, Dupre ME, Fosbol EL, Jollis JG, Strauss B, Anderson ML, McNally B, Granger CB. Association of bystander and first‐responder intervention with survival after out‐of‐hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255–264. [DOI] [PubMed] [Google Scholar]
- 28. Nordberg P, Jonsson M, Forsberg S, Ringh M, Fredman D, Riva G, Hasselqvist‐Ax I, Hollenberg J. The survival benefit of dual dispatch of EMS and fire‐fighters in out‐of‐hospital cardiac arrest may differ depending on population density: a prospective cohort study. Resuscitation. 2015;90:143–149. [DOI] [PubMed] [Google Scholar]
- 29. Shuster M, Keller JL. Effect of fire department first‐responder automated defibrillation. Ann Emerg Med. 1993;22:721–727. [DOI] [PubMed] [Google Scholar]
- 30. Smith KL, Peeters A, McNeil JJ. Results from the first 12 months of a fire first‐responder program in Australia. Resuscitation. 2001;49:143–150. [DOI] [PubMed] [Google Scholar]
- 31. Stromsoe A, Afzelius S, Axelsson C, Sodersved Kallestedt ML, Enlund M, Svensson L, Herlitz J. Improvements in logistics could increase survival after out‐of‐hospital cardiac arrest in Sweden. J Intern Med. 2013;273:622–627. [DOI] [PubMed] [Google Scholar]
- 32. Vaillancourt C, Lui A, De Maio VJ, Wells GA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out‐of‐hospital cardiac arrest victims. Resuscitation. 2008;79:417–423. [DOI] [PubMed] [Google Scholar]
- 33. Ahn KO, Shin SD, Hwang SS, Oh J, Kawachi I, Kim YT, Kong KA, Hong SO. Association between deprivation status at community level and outcomes from out‐of‐hospital cardiac arrest: a nationwide observational study. Resuscitation. 2011;82:270–276. [DOI] [PubMed] [Google Scholar]
- 34. Sund B, Svensson L, Rosenqvist M, Hollenberg J. Favourable cost‐benefit in an early defibrillation programme using dual dispatch of ambulance and fire services in out‐of‐hospital cardiac arrest. Eur J Health Econ. 2012;13:811–818. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table SI. Dispatch Codes for Cardiac Arrest Used at the Emergency Medical Coordination Center
Table SII. Baseline Characteristics of Patients Not Included in Control or Intervention Group
Table SIII. Outcome Variables for Patients Not Included in Control or Intervention Group
Table SIV. Discarded Unmatched Cases
Table SV. Indexed as CA Using the 2 Major Dispatch Codes: Unconscious Adult—Unresponsive and Not Breathing Normally, Unconscious Adult—Ongoing Cardiopulmonary Resuscitation
Table SVI. Indexed as CA Using the 2 Major Dispatch Codes: Unconscious Adult—Unresponsive and Not Breathing Normally, Unconscious Adult—Ongoing Cardiopulmonary Resuscitation
Figure SI. Kaplan–Meier survival curve for control and intervention groups after propensity score matching.
Figure SII. Histogram of propensity scores before and after matching.
Figure SIII. Jitter plot of propensity scores for matched and unmatched cases.
Figure SIV. Proportion of cases arrived at scene in different time intervals in control and intervention groups.


