Abstract
Background
Cardiac rehabilitation (CR) is underutilized in the United States, with fewer than 20% of eligible patients participating in CR programs. Individual socioeconomic status is associated with CR utilization, but data regarding neighborhood characteristics and CR are sparse. We investigated the association of neighborhood socioeconomic context with CR participation in the SCCS (Southern Community Cohort Study).
Methods and Results
The SCCS is a prospective cohort study of 84 569 adults in the southeastern United States from 2002 to 2009, 52 117 of whom have Medicare or Medicaid claims. Using these data, we identified participants with hospitalizations for myocardial infarction, percutaneous coronary intervention, or coronary artery bypass surgery and ascertained their CR utilization. Neighborhood socioeconomic context was assessed using a neighborhood deprivation index derived from 11 census‐tract level variables. We analyzed the association of CR utilization with neighborhood deprivation after adjusting for individual socioeconomic status. A total of 4096 SCCS participants (55% female, 57% black) with claims data were eligible for CR. CR utilization was low, with 340 subjects (8%) participating in CR programs. Study participants residing in the most deprived communities (highest quintile of neighborhood deprivation) were less than half as likely to initiate CR (odds ratio 0.42, 95% confidence interval, 0.27–0.66, P<0.001) as those in the lowest quintile. CR participation was inversely associated with all‐cause mortality (hazard ratio 0.77, 95% confidence interval, 0.60–0.996, P<0.05).
Conclusions
Lower neighborhood socioeconomic context was associated with decreased CR participation independent of individual socioeconomic status. These data invite research on interventions to increase CR access in deprived communities.
Keywords: cardiac rehabilitation, neighborhood deprivation, cardiovascular mortality, socioeconomic position
Subject Categories: Cardiovascular Disease, Secondary Prevention, Health Services, Rehabilitation
Clinical Perspective
What Is New?
Neighborhood socioeconomic characteristics are strongly associated with cardiac rehabilitation attendance, even after adjusting for individual socioeconomic status.
What Are the Clinical Implications?
Patients living in deprived communities are at greater risk of cardiac rehabilitation nonattendance, illustrating the importance of developing novel methods to expand cardiac rehabilitation access to underserved populations.
Introduction
Cardiac rehabilitation (CR) is a suite of services including prescriptive exercise that is a critical component of the continuum of care for patients with cardiovascular disease (CVD).1, 2, 3 CR is indicated for patients with acute myocardial infarction, percutaneous coronary intervention, coronary artery bypass surgery, cardiac valve surgery, stable angina, and stable systolic heart failure. CR participation increases quality of life and decreases the risk of all‐cause mortality, CVD mortality,4 and recurrent CVD events.5 Unfortunately, CR is profoundly underutilized, with only 15% to 20% of eligible patients participating in CR programs nationally.6 CR participation rates are particularly low in underrepresented minorities,7, 8 and are lower than the national average in the southeastern United States.8
Barriers to participation in CR are myriad, spanning patient, physician, community, and health system factors, and there are marked ethnic and regional disparities in CR referral and participation rates.6 One of these patient factors, individual socioeconomic status, is directly associated with CR participation.9 Recently, the effect of a patient's environment (ie, neighborhood socioeconomic context) has been studied with regard to cardiovascular outcomes. High levels of neighborhood deprivation are associated with all‐cause10 and cardiovascular mortality11 independent of socioeconomic status. The effect of neighborhood deprivation on CR participation has not been characterized, however.
In this study, we used the SCCS (Southern Community Cohort Study), a prospective cohort of nearly 85 000 adults in the southeastern United States, to evaluate the effect of neighborhood deprivation on CR participation. The majority of SCCS participants have low income levels, and thus the SCCS represents an ideal population with which to study patterns of CR utilization in deprived communities.
Methods
Data Sources
The SCCS is an ongoing prospective cohort study of over 85 000 adults recruited in 12 southeastern states from 2002 to 2009 to investigate the determinants of cancer and other chronic diseases.12 Participants were recruited at community health centers or by mail, and completed a survey that collects baseline data on a variety of demographic, social, medical, and lifestyle factors. All study participants gave informed consent upon enrollment.
Data for SCCS participants who receive Medicare coverage were linked to the Centers for Medicare and Medicaid Services Research Identifiable Files by age, sex, date of birth, and Social Security numbers (which are available for >95% of the cohort). Similarly, data for SCCS participants with Medicaid coverage were linked to individual state Medicaid files. Mortality data were obtained from linkage to the National Death Index and the Social Security Administration's Death Master File. A list of centers providing CR services was obtained by identifying facilities associated with CR claims. We then obtained the geographic coordinates of these facilities.
The institutional review board of Vanderbilt University Medical Center approved the study, as did the SCCS Data and Biospecimen Use Committee.
Participants
The study sample initially included SCCS participants with linked Medicare or Medicaid data and who reside in the United States. Using International Classification of Diseases 9th Revision (ICD‐9) codes and Current Procedure Terminology codes, we identified participants who were hospitalized for a qualifying diagnosis (and thus eligible for CR) from 1999 to 2012 and had uninterrupted fee‐for‐service Medicare or Medicaid coverage for 1 year after the index hospitalization. Qualifying diagnoses included the following: acute myocardial infarction (ICD9 410.xx); percutaneous transluminal coronary angioplasty or coronary stenting (ICD‐9 00.66, 17.55, 36.0x or Current Procedure Terminology 92973, 92974, 92980–92982, 92984, 92995, 92996, G0290, G0291); and coronary artery bypass surgery (CABG, ICD‐9 36.10–36.16, 36.19, 36.2 or Current Procedure Terminology 33510–33514, 33516–33519, 33521–33523, 33533–33536, 33572, 35600, 93564, S2205–S2209).
Some patients had multiple eligibility diagnoses during the same admission. In these cases, any patient who had a CABG was placed in the CABG category regardless of other diagnoses. Participants who had both an acute myocardial infarction and percutaneous coronary intervention were placed in the acute myocardial infarction category. For patients with more than 1 qualifying admission, the earliest admission was considered the “index” admission.
Neighborhood Deprivation Index
Neighborhood socioeconomic status, as measured by a neighborhood deprivation index (NDI),13 was our primary explanatory variable. The SCCS‐NDI has been described in prior work.10 Briefly, a principal components analysis was performed on 20 census tract–level variables among all census tracts of SCCS participants. Based on this analysis, 11 census‐tract variables were used to construct the SCCS‐NDI: (1) percentage of persons age >25 who did not graduate high school; (2) percentage of males and females age ≥25 years who were unemployed; (3) percentage of males in professional occupations; (4) percentage of housing units with ≥1 occupant per room; (5) percentage of occupied housing units with renter/owner costs >50% of income; (6) percentage of persons with income below the 1999 poverty level; (7) percentage of female‐headed households with dependent children; (8) percentage of households with income <$30 000 per year; (9) percentage of households with public assistance income; (10) percentage of households with no car; and (11) median household value. The SCCS‐NDI was divided into quintiles, with quintile 1 representing the least deprived neighborhoods and quintile 5 representing the most deprived neighborhoods.
Outcomes
Participation in CR programs, defined as a binary variable (yes/no), was the primary outcome. We searched the outpatient Medicare and Medicaid files for CR claims (Current Procedural Terminology codes 93797, 93798, G0422, G0423, or S9472) occurring within 1 year after the index hospitalization.
Secondary outcomes included: (1) cardiac rehabilitation as a continuous variable, defined as the number of sessions attended; (2) all‐cause mortality; and (3) cardiovascular mortality, defined by ICD‐9 codes 390.0 to 458.9 or their equivalents from ICD‐8 or ICD‐10. We truncated follow‐up for mortality at 10 years to prevent confounding by small sample sizes beyond this time period.
Covariates
We obtained comorbidities from the baseline survey. Comorbid conditions of interest included chronic obstructive pulmonary disease, current smoking, depression, diabetes mellitus, hypertension, obesity, prior myocardial infarction, prior coronary artery bypass grafting, prior stroke, and prior transient ischemic attack. Depression was defined as a Center for Epidemiologic Studies Short Depression Scale 10 (CESD10) score of 10 or greater. Individual socioeconomic status was characterized by annual household income (<15 000, $15 000–$24 999, or >$25 000) and educational level (no high school diploma, high school diploma, or college diploma). We also calculated the distance between the participant's residence and the nearest CR center using geocodes.
Statistical Analysis
Baseline characteristics of SCCS participants who attended CR programs were compared with those who did not, using Pearson's χ2 test and Wilcoxon tests. We used logistic regression to evaluate the effect of individual covariates on CR participation rates. A Cox proportional hazards model for all‐cause and cardiovascular mortality was constructed using the same covariates. We also used Kaplan–Meier survival curves to compare all‐cause and cardiovascular mortality between SCCS participants who attended CR and those who did not. We performed sensitivity analyses to account for potential clustering of participants within census tracts (data nonindependence). The Huber‐White method was used to adjust standard errors of parametric estimates. Because these results were almost identical to the primary analyses, we reported the analyses without Huber‐White adjustment.
Results
There were 52 117 SCCS participants who received Medicare or Medicaid coverage from 1999 to 2012. Of these, 4552 were hospitalized for acute myocardial infarction, coronary artery bypass grafting (CABG), or percutaneous coronary intervention and had uninterrupted fee‐for‐service Medicare or Medicaid coverage for 1 year after the index admission. We excluded 456 SCCS participants because of missing data, yielding a final sample size of 4096 CR‐eligible patients. Of the 456 SCCS participants with missing data, 161 (35%) were excluded because of missing household income, 120 (26%) were excluded because of missing education levels, and 64 (14%) were excluded because of missing residence location.
A total of 340 SCCS participants in the sample (8%) initiated CR (Table 1). The number of CR sessions attended had a range of 1 to 36, with a median of 4 sessions and an interquartile range of 3 sessions. A majority of the 4096 study participants were black (57%). Most members of the cohort were poor (70% of participants had a household income of <$15 000) and 44% had not completed high school. Almost all participants had Medicare or Medicaid as their primary form of insurance, and 16% had some form of private insurance. There was a high burden of cardiovascular disease in this population, with 32% reporting a history of myocardial infarction, 18% reporting prior CABG, and 46% reporting a history of diabetes mellitus.
Table 1.
Characteristics of SCCS Participants Eligible for CR (N=4096)
| Characteristic | All (N=4096) | CR Nonparticipants (N=3756) | CR Participants (N=340) | P Value |
|---|---|---|---|---|
| Number of CR sessions attended | n/a | n/a | 4 (2, 5) | n/a |
| Eligibility diagnosis | ||||
| AMI | 32% (1323) | 32% (1207) | 34% (116) | <0.001a |
| PCI | 50% (2034) | 51% (1924) | 32% (110) | |
| CABG | 18% (739) | 17% (625) | 34% (114) | |
| Demographic | ||||
| Age (y) | 59 (52, 66) | 59 (52, 66) | 64 (57, 69) | <0.001b |
| Male | 45% (1839) | 44% (1663) | 52% (176) | <0.01a |
| Black | 57% (2331) | 58% (2170) | 47% (161) | <0.001a |
| Distance to nearest CR center, km | 8.3 (3.8, 24.5) | 8.3 (3.8, 25.2) | 8.3 (3.6, 17.7) | <0.05b |
| Neighborhood socioeconomic status | ||||
| Neighborhood deprivation index | 0.52 (−0.12, 1.45) | 0.57 (−0.09, 1.49) | 0.15 (−0.38, 0.96) | <0.001a |
| Individual socioeconomic status | ||||
| Education | ||||
| Did not complete high school | 44% (1788) | 45% (1681) | 31% (107) | <0.001a |
| Completed high school | 49% (2017) | 49% (1839) | 52% (178) | |
| Completed college | 7% (291) | 6% (236) | 16% (55) | |
| Household income | ||||
| <$15 000 | 70% (2847) | 71% (2675) | 51% (172) | <0.001a |
| $15 000 to $24 999 | 18% (738) | 18% (669) | 20% (69) | |
| >$25 000 | 12% (511) | 11% (412) | 29% (99) | |
| Health insurance | ||||
| Private | 16% (647) | 14% (538) | 32% (109) | <0.001a |
| Medicaid | 39% (1596) | 40% (1505) | 27% (91) | |
| Medicare | 45% (1853) | 46% (1713) | 41% (140) | |
| Comorbidities | ||||
| BMI | 30.2 (26.0, 35.4) | 30.3 (26.0, 35.6) | 29.9 (26.5, 33.9) | 0.54b |
| COPD | 16% (639) | 16% (586) | 16% (53) | 0.99a |
| CESD10 score | 9 (5, 13) | 9 (5, 14) | 7 (3, 11) | <0.001b |
| Diabetes mellitus | 46% (1875) | 46% (1723) | 45% (152) | 0.68a |
| Hypertension | 78% (3199) | 78% (2924) | 81% (275) | 0.20a |
| Smoking | 39% (1602) | 40% (1516) | 25% (86) | <0.001a |
| Stroke/TIA | 17% (705) | 18% (658) | 14% (47) | 0.08a |
Values are displayed as median, (25th%, 75th%) or percentages, n. AMI indicates acute myocardial infarction; BMI, body mass index; CABG, coronary artery bypass grafting; CESD10, Center for Epidemiologic Studies Short Depression Scale 10; COPD, chronic obstructive pulmonary disease; CR, cardiac rehabilitation; n/a, not applicable; PCI, percutaneous coronary intervention; SCCS, Southern Community Cohort Study; TIA, transient ischemic attack.
Pearson χ2 test.
Wilcoxon test.
A neighborhood deprivation index (SCCS‐NDI) was constructed to illustrate relative neighborhood socioeconomic status for each SCCS participant's census tract. The SCCS‐NDI had a relatively normal distribution (Figure 1). Individual components of the SCCS‐NDI, as well as their correlation coefficients with CR, are displayed in Table S1. The SCCS‐NDI was strongly associated with the odds of initiating CR after multivariable adjustment (Figure 2). Compared with the lowest quintile of neighborhood deprivation, SCCS participants residing in areas in the highest quintile of neighborhood deprivation were less than half as likely to initiate CR (OR 0.42, 95% confidence interval [CI], 0.27–0.66, P<0.001). When analyzed as a continuous variable, there was a 15% decrease in the odds of attending CR for each point increase in the SCCS‐NDI (OR 0.85, 95% CI, 0.75–0.96, P<0.01).
Figure 1.
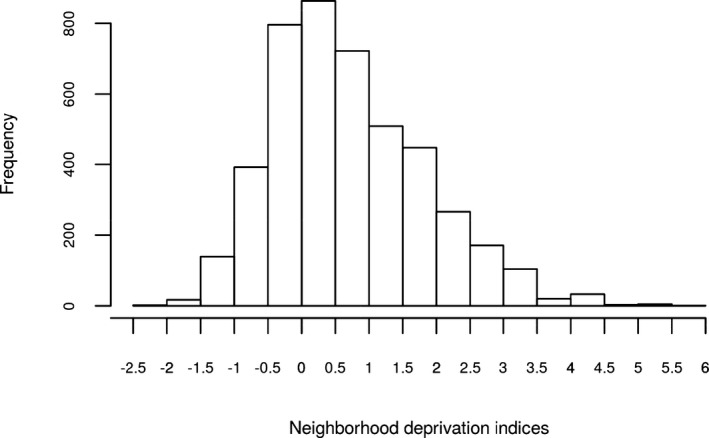
Distribution of neighborhood deprivation indices among Southern Community Cohort Study participants eligible for cardiac rehabilitation (N=4096).
Figure 2.
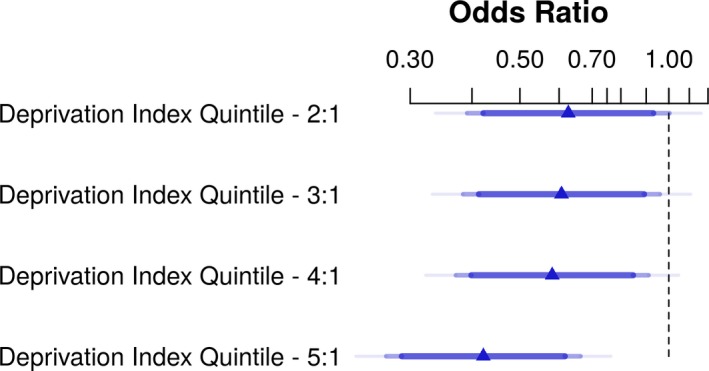
Forest plot of odds ratios of cardiac rehabilitation participation for each quintile of the neighborhood deprivation index, with 90%, 95%, and 99% confidence intervals (N=4096). The first quintile (referent) represents the lowest deprivation, and the fifth quintile represents the highest deprivation. Odds ratios are adjusted for eligibility diagnosis, age, sex, race, distance to the nearest cardiac rehabilitation center, education level, household income, health insurance type, and comorbidities.
Older SCCS participants were more likely to participate in CR than younger participants (Table 2). Those who completed college were more likely to attend CR programs as compared with those who did not complete high school (OR 1.61, 95% CI, 1.06–2.44, P<0.05), and study participants with a household income >$25 000 were more likely to initiate CR than those making less than $15 000 a year (OR 1.68, 95% CI, 1.17–2.42, P<0.01). Compared with SCCS participants with private insurance, those with only Medicaid or Medicare coverage were less likely to initiate CR. Smokers were also less likely to participate in CR programs as compared with nonsmokers (OR 0.65, 95% CI, 0.49–0.85, P<0.01). A change from the 25th quartile of distance from the patient's residence (3.8 km) to the 75th quartile (25 km) was associated with a 29% decrease in the odds of attending CR (OR 0.71, 95% CI, 0.59–0.84, P<0.001).
Table 2.
Multivariable‐Adjusted Predictors of CR Participation in the SCCS Study (N=4096)
| Characteristic | ORa | 95% CI | P Value |
|---|---|---|---|
| Eligibility diagnosis | |||
| AMI | Referent | ||
| PCI | 0.63 | 0.48, 0.84 | <0.01 |
| CABG | 1.78 | 1.34, 2.38 | <0.001 |
| Demographic | |||
| Age (y) | |||
| <50 | Referent | ||
| 50 to 64 | 1.57 | 1.04, 2.39 | <0.05 |
| ≥65 | 1.86 | 1.20, 2.89 | <0.01 |
| Male | 1.05 | 0.83, 1.35 | 0.67 |
| Black | 1.02 | 0.78, 1.33 | 0.89 |
| Distance to nearest CR center, km (change from 25th quartile to 75th quartile) | 0.71 | 0.59, 0.84 | <0.001 |
| Neighborhood socioeconomic status | |||
| Neighborhood deprivation index quintiles | |||
| 1 (least deprived) | Referent | ||
| 2 | 0.63 | 0.39, 1.0 | 0.051 |
| 3 | 0.61 | 0.38, 0.96 | <0.05 |
| 4 | 0.58 | 0.37, 0.91 | <0.05 |
| 5 (most deprived) | 0.42 | 0.27, 0.66 | <0.001 |
| Individual socioeconomic status | |||
| Education | |||
| Did not complete high school | Referent | ||
| Completed high school | 1.20 | 0.92, 1.58 | 0.18 |
| Completed college | 1.61 | 1.06, 2.44 | <0.05 |
| Household income | |||
| <$15 000 | Referent | ||
| $15 000 to $24 999 | 1.27 | 0.93, 1.73 | 0.14 |
| >$25 000 | 1.68 | 1.17, 2.42 | <0.01 |
| Health insurance | |||
| Private | Referent | ||
| Medicaid | 0.65 | 0.44, 0.94 | <0.05 |
| Medicare | 0.68 | 0.49, 0.95 | <0.05 |
| Comorbidities | |||
| COPD | 1.33 | 0.96, 1.85 | 0.09 |
| Depressionb | 0.79 | 0.61, 1.02 | 0.07 |
| Diabetes mellitus | 0.97 | 0.76, 1.24 | 0.80 |
| Hypertension | 1.25 | 0.93, 1.70 | 0.14 |
| Obesityc | 1.01 | 0.79, 1.29 | 0.96 |
| Prior stroke/TIA | 0.84 | 0.60, 1.17 | 0.29 |
| Smoking | 0.65 | 0.49, 0.85 | <0.01 |
AMI indicates acute myocardial infarction; BMI, body mass index; CABG, coronary artery bypass grafting; CESD10, Center for Epidemiologic Studies Short Depression Scale 10; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CR, cardiac rehabilitation; OR, odds ratio; PCI, percutaneous coronary intervention; SCCS, Southern Community Cohort Study; TIA, transient ischemic attack.
The presented effects are from a fully adjusted logistic regression model including all listed covariates.
Denotes CESD10 score ≥10.
Denotes BMI ≥30.
Among the 4096 SCCS participants in the study sample, there were 1073 all‐cause deaths and 426 cardiovascular disease–related deaths over a total of 20 403 person‐years of follow‐up. There was an inverse association between CR attendance and all‐cause mortality (hazard ratio 0.77, 95% CI, 0.60–0.996, P<0.05) after multivariable adjustment (Table 3). A survival curve for all‐cause mortality, stratified by CR participants and nonparticipants, is displayed in Figure 3. The association between neighborhood deprivation and all‐cause mortality approached statistical significance (hazard ratio 1.09 for 75th versus 25th quartile, 95% CI, 1.0–1.20, P=0.06). Black race, male sex, diabetes mellitus, obesity, and smoking were all associated with a higher risk of all‐cause mortality. Household income >$25 000 was associated with decreased all‐cause mortality.
Table 3.
Multivariable‐Adjusted Predictors of All‐Cause and CVD Mortality in the SCCS (N=4096)
| Characteristic | All‐Cause Mortality | CVD Mortality | ||||
|---|---|---|---|---|---|---|
| HRa | 95% CI | P Value | HRa | 95% CI | P Value | |
| Cardiac rehabilitation | 0.77 | 0.60, 0.996 | <0.05 | 0.65 | 0.43, 0.99 | <0.05 |
| Eligibility diagnosis | ||||||
| AMI | Referent | Referent | ||||
| PCI | 0.78 | 0.69, 0.90 | <0.001 | 0.66 | 0.53, 0.82 | <0.001 |
| CABG | 0.62 | 0.52, 0.75 | <0.0001 | 0.67 | 0.51, 0.89 | <0.01 |
| Demographic | ||||||
| Age (y) | ||||||
| <50 | Referent | Referent | ||||
| 50 to 64 | 1.39 | 1.17, 1.64 | <0.001 | 0.93 | 0.72, 1.19 | 0.56 |
| ≥65 | 1.94 | 1.60, 2.35 | <0.0001 | 1.26 | 0.94, 1.69 | 0.11 |
| Male | 1.28 | 1.13, 1.45 | <0.001 | 1.43 | 1.17, 1.75 | <0.001 |
| Black | 1.36 | 1.18, 1.56 | <0.0001 | 1.36 | 1.09, 1.71 | <0.05 |
| Neighborhood socioeconomic status | ||||||
| Neighborhood deprivation index (change from 25th quartile to 75th quartile) | 1.09 | 0.996, 1.196 | 0.06 | 1.15 | 0.99, 1.32 | 0.065 |
| Individual socioeconomic status | ||||||
| Education | ||||||
| Did not complete high school | Referent | Referent | ||||
| Completed high school | 1.10 | 0.97, 1.25 | 0.15 | 1.04 | 0.85, 1.28 | 0.71 |
| Completed college | 1.08 | 0.81, 1.43 | 0.62 | 1.07 | 0.70, 1.64 | 0.76 |
| Household income | ||||||
| <$15 000 | Referent | Referent | ||||
| $15 000 to $24 999 | 0.85 | 0.72, 1.01 | 0.06 | 0.96 | 0.74, 1.25 | 0.76 |
| >$25 000 | 0.70 | 0.54, 0.91 | <0.01 | 0.88 | 0.60, 1.29 | 0.52 |
| Health insurance | ||||||
| Private | Referent | Referent | ||||
| Medicaid | 1.11 | 0.89, 1.38 | 0.35 | 0.81 | 0.59, 1.13 | 0.22 |
| Medicare | 1.11 | 0.90, 1.37 | 0.33 | 0.95 | 0.70, 1.29 | 0.75 |
| Comorbidities | ||||||
| COPD | 1.13 | 0.95, 1.33 | 0.16 | 1.07 | 0.81, 1.40 | 0.64 |
| Depressionb | 1.06 | 0.94, 1.21 | 0.35 | 1.07 | 0.87, 1.31 | 0.52 |
| Diabetes mellitus | 1.54 | 1.35, 1.74 | <0.0001 | 1.37 | 1.12, 1.67 | <0.01 |
| Hypertension | 1.10 | 0.94, 1.29 | 0.23 | 1.39 | 1.06, 1.82 | <0.05 |
| Obesityc | 1.30 | 1.14, 1.47 | <0.0001 | 1.03 | 0.84, 1.26 | 0.81 |
| Prior stroke/TIA | 0.92 | 0.79, 1.08 | 0.32 | 1.12 | 0.88, 1.41 | 0.36 |
| Smoking | 1.43 | 1.25, 1.63 | <0.0001 | 1.24 | 1.01, 1.53 | <0.05 |
AMI indicates acute myocardial infarction; BMI, body mass index; CABG, coronary artery bypass grafting; CESD10, Center for Epidemiologic Studies Short Depression Scale 10; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; HR, hazard ratio; PCI, percutaneous coronary intervention; SCCS, SCCS, Southern Community Cohort Study; TIA, transient ischemic attack.
The presented effects are from a fully adjusted Cox regression model including all listed covariates.
Denotes CESD10 score ≥10.
Denotes BMI ≥30.
Figure 3.
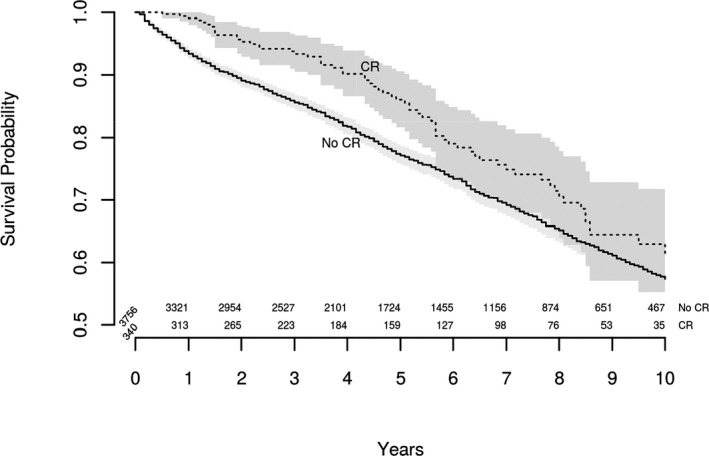
Kaplan–Meier survival curve for all‐cause mortality over 10 years of follow‐up, stratified by cardiac rehabilitation participants and nonparticipants (N=4096, P=0.01 by log‐rank test). CR indicates cardiac rehabilitation.
CR participation was associated with a 35% decrease in CVD mortality (hazard ratio 0.65, 95% CI, 0.43–0.99, P<0.05) after multivariable adjustment. The survival curve for CVD mortality, stratified by CR participants and nonparticipants, is shown in Figure 4. As with all‐cause mortality, the association between neighborhood deprivation and CVD mortality approached statistical significance (hazard ratio 1.15 for 75th versus 25th quartile, 95% CI, 0.99–1.32, P=0.07). Black race, male sex, diabetes mellitus, hypertension, and smoking were all associated with an increased risk of CVD mortality.
Figure 4.
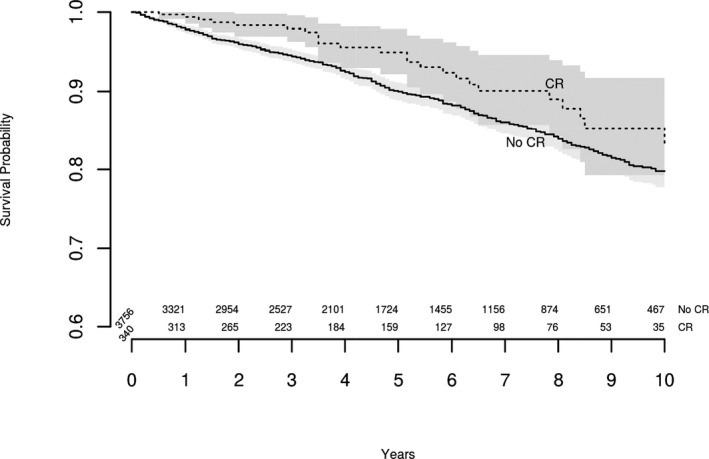
Kaplan–Meier survival curve for cardiovascular mortality over 10 years of follow‐up, stratified by cardiac rehabilitation participants and nonparticipants (N=4096, P=0.051 by log‐rank test). CR indicates cardiac rehabilitation.
Discussion
In this study of SCCS participants, we demonstrate that neighborhood socioeconomic status, as characterized by a neighborhood deprivation index, is strongly associated with the odds of attending CR programs even after adjusting for individual socioeconomic status. Moreover, CR is associated with decreased risk of all‐cause and CVD mortality in this population. To our knowledge, this is the first study examining the effect of neighborhood socioeconomic context on CR participation rates. This is also one of the only studies to evaluate the effect of CR on mortality in a majority black cohort.
Neighborhood deprivation was originally quantified to study perinatal health outcomes,13 and associations were quickly identified with all‐cause mortality10, 16 and an increased risk of rehospitalization.17 The socioeconomic context of neighborhoods was subsequently analyzed with regard to cardiovascular outcomes and found to affect the risk of myocardial infarction11 as well as long‐term mortality after myocardial infarction.18 The interplay of neighborhood socioeconomic context and cardiovascular disease is complex. Neighborhood deprivation is associated with increased higher coronary artery calcium in young, asymptomatic men, and thus may contribute to subclinical atherosclerosis.19, 20 Deprived neighborhoods often have poor access to supermarkets and healthy food choices, leading to poorer diets and weight gain.21, 22, 23 Additionally, neighborhood deprivation is associated with negative health behaviors such as smoking and physical inactivity.24, 25, 26, 27 One of the mechanisms by which neighborhood deprivation affects cardiovascular outcomes may be by diminished access to CR. Barriers to attending CR programs include lack of transportation, caregiver responsibilities, work responsibilities, and copays.28, 29, 30, 31, 32, 33 Unsurprisingly, individual socioeconomic status (including income and education) is strongly associated with CR participation in prior studies.34 Neighborhood deprivation provides a useful lens with which to view barriers to CR attendance in addition to individual socioeconomic status.
Participants in the SCCS likely experience significant barriers to CR, given the disadvantaged nature of the cohort. Unsurprisingly, the proportion of SCCS participants that initiated CR in our study is very low (8%), and significantly lower than the national average of ≈20% of eligible patients.7, 8, 35 Those SCCS participants who did initiate CR attended fewer sessions (median 4, interquartile range 2–5) than Medicare patients nationally, who attend 24 to 25 sessions on average.7, 8, 35 Copays have a particularly detrimental impact on the number of CR sessions attended, especially among low‐income patients, as copays are applied for each session. For Medicare patients without supplemental insurance, copays are ≈$20 per session ($720 for a full course of 36 sessions), while Medicaid coverage is variable.36 Attending CR programs was likely financially prohibitive for many SCCS participants. The fact that SCCS patients with private insurance and those with higher income levels were more likely to attend CR programs supports this observation.
We also found that younger SCCS participants were less likely to attend CR. Work responsibilities are a significant barrier to CR in the younger SCCS population, as attending a full course of 36 CR sessions requires a 1‐hour commitment 3 times per week for 12 weeks in addition to travel time to and from appointments. Interestingly, active smokers were much less likely to attend CR programs. This association is unfortunate, as CR incorporates smoking cessation therapy, but it may represent an inherent resistance to risk factor modification and behavior change in this population.
Those SCCS participants who did attend CR programs appear to have experienced significant benefit in the form of decreased mortality. There was a 23% decrease in risk of all‐cause mortality and a 35% decrease in risk of CVD mortality associated with CR. These effects are slightly larger than those in other studies, which generally demonstrate that CR is associated with a 20% decrease in all‐cause mortality and a 25% decrease in CVD mortality.4, 37, 38, 39 It is certainly feasible that CR would be particularly effective in this cohort. SCCS participants have high burdens of cardiovascular risk factors and low income and educational levels. The risk factor education that occurs within CR, coupled with prescriptive exercise, is likely to be highly efficacious in this population. There is a possibility of healthy cohort bias in our mortality analyses, as patients with more comorbidities are inherently less likely to attend CR. However, we controlled extensively for comorbidities as well as socioeconomic factors in our analyses.
In demonstrating that patients in deprived neighborhoods are at significant risk for CR nonattendance, our analyses invite further research on methods to reach out to these communities. Specifically, home‐based CR programs may be well adapted to cardiovascular disease patients in deprived neighborhoods, as they offer the potential to ameliorate CR barriers such as transportation and work responsibilities. Home‐based CR programs have demonstrated efficacy in Europe and are now being trialed in the United States.40, 41, 42, 43, 44, 45 Additionally, efforts to decrease copays associated with CR would be very helpful in expanding access to deprived communities, as these costs are often prohibitive for many patients. Lastly, special efforts could be made to educate younger patients and smokers about the benefits of CR, as these patients are at highest risk of CR nonattendance.
Our analyses have limitations. First, our data were obtained from Centers for Medicare and Medicaid Services administrative claims linked to SCCS records. Claims data are not adjudicated and lack granular data on clinical characteristics. However, Centers for Medicare and Medicaid Services data have been used to effectively study many cardiovascular therapies, including CR, in prior work.3, 7, 8 Second, our analyses were limited to SCCS participants enrolled in fee‐for‐service Medicare and may not be generalizable to patients enrolled in Medicare private health plans. However, fee‐for‐service Medicare still accounted for 72% of Medicare beneficiaries in 2013.46 Third, 10% of participants were excluded because of missing data. However, a complete case analysis is appropriate in terms of statistical power given the large size of the sample. Fourth, our data on insurance coverage and comorbidities came from self‐report. However, self‐reported cardiovascular conditions such as hypertension, diabetes mellitus, and myocardial infarction are generally accurate, and the SCCS questionnaire is a comprehensive instrument.12, 47, 48 Lastly, we were unable to determine whether or not a SCCS participant was referred to CR with the available claims data. Future studies could examine the association of neighborhood deprivation with CR referral as well.
In summary, we found that lower neighborhood socioeconomic context, as quantified by a NDI, was associated with decreased CR participation independent of individual socioeconomic status. Participation in CR programs was associated with a significant decrease in all‐cause and cardiovascular mortality in this majority black cohort. Our work invites further study on barriers to CR use in deprived communities and strategies to circumvent these barriers through outreach efforts.
Sources of Funding
The Southern Community Cohort Study was supported by a grant from the National Cancer Institute (R01 CA092447) and funds from the American Recovery and Reinvestment Act (3R01 CA092447‐08S1). Dr Bachmann was supported by grant number K12HS022990 from the Agency for Healthcare Research and Quality. Dr Gupta was supported by K23‐HL128928‐01A1 from the National Heart, Lung, and Blood Institute of the National Institutes of Health. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the above agencies.
Disclosures
None.
Supporting information
Table S1. Census Tract Components of the Southern Community Cohort Study Neighborhood Deprivation Index, Stratified by Cardiac Rehabilitation Use (N=4096)
Acknowledgments
The authors would like to acknowledge the Million Hearts Initiative co‐led by the Centers for Medicaid & Medicare Services and Centers for Disease Control and Prevention. Million Hearts hosts the Cardiac Rehabilitation Collaborative, within which the authors had many discussions with other cardiac rehabilitation professionals that helped shape this study.
(J Am Heart Assoc. 2017;6:e006260 DOI: 10.1161/JAHA.117.006260.)
This manuscript was handled independently by Holli A. DeVon, PhD, as a guest editor.
References
- 1. Arena R, Williams M, Forman DE, Cahalin LP, Coke L, Myers J, Hamm L, Kris‐Etherton P, Humphrey R, Bittner V, Lavie CJ; American Heart Association Exercise CR, Prevention Committee of the Council on Clinical Cardiology CoE, Prevention, Council on Nutrition PA, Metabolism . Increasing referral and participation rates to outpatient cardiac rehabilitation: the valuable role of healthcare professionals in the inpatient and home health settings: a science advisory from the American Heart Association. Circulation. 2012;125:1321–1329. [DOI] [PubMed] [Google Scholar]
- 2. Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW; American Heart Association Science A, Coordinating C . Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. [DOI] [PubMed] [Google Scholar]
- 3. Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long‐term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, Skidmore B, Stone JA, Thompson DR, Oldridge N. Exercise‐based rehabilitation for patients with coronary heart disease: systematic review and meta‐analysis of randomized controlled trials. Am J Med. 2004;116:682–692. [DOI] [PubMed] [Google Scholar]
- 5. Kwan G, Balady GJ. Cardiac rehabilitation 2012: advancing the field through emerging science. Circulation. 2012;125:e369–e373. [DOI] [PubMed] [Google Scholar]
- 6. Prince DZ, Sobolev M, Gao J, Taub CC. Racial disparities in cardiac rehabilitation initiation and the effect on survival. PM R. 2013;6:486–492. [DOI] [PubMed] [Google Scholar]
- 7. Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. [DOI] [PubMed] [Google Scholar]
- 8. Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. [DOI] [PubMed] [Google Scholar]
- 9. Valencia HE, Savage PD, Ades PA. Cardiac rehabilitation participation in underserved populations. Minorities, low socioeconomic, and rural residents. J Cardiopulm Rehabil Prev. 2011;31:203–210. [DOI] [PubMed] [Google Scholar]
- 10. Signorello LB, Cohen SS, Williams DR, Munro HM, Hargreaves MK, Blot WJ. Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health. 2014;104:e98–e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stjarne MK, Fritzell J, De Leon AP, Hallqvist J; Group SS . Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology. 2006;17:14–23. [DOI] [PubMed] [Google Scholar]
- 12. Signorello LB, Hargreaves MK, Steinwandel MD, Zheng W, Cai Q, Schlundt DG, Buchowski MS, Arnold CW, McLaughlin JK, Blot WJ. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97:972–979. [PMC free article] [PubMed] [Google Scholar]
- 13. Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, Elo I, Burke JG, O'Campo P. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83:1041–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. SAS Institute . Statistical analysis software, version 9.4. 2016.
- 15. R Core Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: http://www.R-project.org/. 2015. [Google Scholar]
- 16. Major JM, Doubeni CA, Freedman ND, Park Y, Lian M, Hollenbeck AR, Schatzkin A, Graubard BI, Sinha R. Neighborhood socioeconomic deprivation and mortality: NIH‐AARP diet and health study. PLoS One. 2010;5:e15538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, Greenberg C, Smith M. Neighborhood socioeconomic disadvantage and 30‐day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gerber Y, Benyamini Y, Goldbourt U, Drory Y; Israel Study Group on First Acute Myocardial I . Neighborhood socioeconomic context and long‐term survival after myocardial infarction. Circulation. 2010;121:375–383. [DOI] [PubMed] [Google Scholar]
- 19. Kershaw KN, Diez Roux AV, Bertoni A, Carnethon MR, Everson‐Rose SA, Liu K. Associations of chronic individual‐level and neighbourhood‐level stressors with incident coronary heart disease: the Multi‐Ethnic Study of Atherosclerosis. J Epidemiol Community Health. 2015;69:136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dragano N, Hoffmann B, Stang A, Moebus S, Verde PE, Weyers S, Mohlenkamp S, Schmermund A, Mann K, Jockel KH, Erbel R, Siegrist J; Heinz Nixdorf Recall Study Investigative G . Subclinical coronary atherosclerosis and neighbourhood deprivation in an urban region. Eur J Epidemiol. 2009;24:25–35. [DOI] [PubMed] [Google Scholar]
- 21. Sharkey JR, Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the ground‐truthed food environment in a large rural area. J Nutr. 2008;138:620–627. [DOI] [PubMed] [Google Scholar]
- 22. Ford PB, Dzewaltowski DA. Neighborhood deprivation, supermarket availability, and BMI in low‐income women: a multilevel analysis. J Community Health. 2011;36:785–796. [DOI] [PubMed] [Google Scholar]
- 23. Powell‐Wiley TM, Ayers C, Agyemang P, Leonard T, Berrigan D, Ballard‐Barbash R, Lian M, Das SR, Hoehner CM. Neighborhood‐level socioeconomic deprivation predicts weight gain in a multi‐ethnic population: longitudinal data from the Dallas Heart Study. Prev Med. 2014;66:22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stimpson JP, Ju H, Raji MA, Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. Am J Health Behav. 2007;31:215–222. [DOI] [PubMed] [Google Scholar]
- 25. Laraia BA, Karter AJ, Warton EM, Schillinger D, Moffet HH, Adler N. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE). Soc Sci Med. 2012;74:1082–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stoddard PJ, Laraia BA, Warton EM, Moffet HH, Adler NE, Schillinger D, Karter AJ. Neighborhood deprivation and change in BMI among adults with type 2 diabetes: the Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36:1200–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schmitz N, Nitka D, Gariepy G, Malla A, Wang J, Boyer R, Messier L, Strychar I, Lesage A. Association between neighborhood‐level deprivation and disability in a community sample of people with diabetes. Diabetes Care. 2009;32:1998–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Reges O, Vilchinsky N, Leibowitz M, Khaskia A, Mosseri M, Kark JD. Systemic determinants as barriers to participation in cardiac prevention and rehabilitation services after acute coronary syndrome. Int J Cardiol. 2013;168:4865–4867. [DOI] [PubMed] [Google Scholar]
- 29. Mendes M. Barriers to participation in cardiac rehabilitation programs. Rev Port Cardiol. 2011;30:509–514. [PubMed] [Google Scholar]
- 30. Grace SL, Gravely‐Witte S, Kayaniyil S, Brual J, Suskin N, Stewart DE. A multisite examination of sex differences in cardiac rehabilitation barriers by participation status. J Womens Health (Larchmt). 2009;18:209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, Koepsell E, Roger VL. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. De Angelis C, Bunker S, Schoo A. Exploring the barriers and enablers to attendance at rural cardiac rehabilitation programs. Aust J Rural Health. 2008;16:137–142. [DOI] [PubMed] [Google Scholar]
- 33. Witt BJ, Thomas RJ, Roger VL. Cardiac rehabilitation after myocardial infarction: a review to understand barriers to participation and potential solutions. Eura Medicophys. 2005;41:27–34. [PubMed] [Google Scholar]
- 34. Sun EY, Jadotte YT, Halperin W. Disparities in cardiac rehabilitation participation in the United States: a systematic review and meta‐analysis. J Cardiopulm Rehabil Prev. 2016;37:2–10. [DOI] [PubMed] [Google Scholar]
- 35. Gurewich D, Prottas J, Bhalotra S, Suaya JA, Shepard DS. System‐level factors and use of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2008;28:380–385. [DOI] [PubMed] [Google Scholar]
- 36. Centers for Medicaid & Medicare Services . Physician fee schedule search. 2016.
- 37. Oosenbrug E, Marinho RP, Zhang J, Marzolini S, Colella TJ, Pakosh M, Grace SL. Sex differences in cardiac rehabilitation adherence: a meta‐analysis. Can J Cardiol. 2016;32:1316–1324. [DOI] [PubMed] [Google Scholar]
- 38. Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise‐based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta‐analysis. J Am Coll Cardiol. 2016;67:1–12. [DOI] [PubMed] [Google Scholar]
- 39. Almodhy M, Ingle L, Sandercock GR. Effects of exercise‐based cardiac rehabilitation on cardiorespiratory fitness: a meta‐analysis of UK studies. Int J Cardiol. 2016;221:644–651. [DOI] [PubMed] [Google Scholar]
- 40. Zwisler AD, Norton RJ, Dean SG, Dalal H, Tang LH, Wingham J, Taylor RS. Home‐based cardiac rehabilitation for people with heart failure: a systematic review and meta‐analysis. Int J Cardiol. 2016;221:963–969. [DOI] [PubMed] [Google Scholar]
- 41. Piotrowicz E, Baranowski R, Bilinska M, Stepnowska M, Piotrowska M, Wojcik A, Korewicki J, Chojnowska L, Malek LA, Klopotowski M, Piotrowski W, Piotrowicz R. A new model of home‐based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail. 2010;12:164–171. [DOI] [PubMed] [Google Scholar]
- 42. Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: cochrane systematic review and meta‐analysis. BMJ. 2010;340:b5631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Jolly K, Taylor RS, Lip GY, Davies M, Davis R, Mant J, Singh S, Greenfield S, Ingram J, Stubley J, Bryan S, Stevens A. A randomized trial of the addition of home‐based exercise to specialist heart failure nurse care: the Birmingham Rehabilitation Uptake Maximisation study for patients with Congestive Heart Failure (BRUM‐CHF) study. Eur J Heart Fail. 2009;11:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jolly K, Lip GY, Taylor RS, Raftery J, Mant J, Lane D, Greenfield S, Stevens A. The Birmingham Rehabilitation Uptake Maximisation study (BRUM): a randomised controlled trial comparing home‐based with centre‐based cardiac rehabilitation. Heart. 2009;95:36–42. [DOI] [PubMed] [Google Scholar]
- 45. Dalal HM, Evans PH, Campbell JL, Taylor RS, Watt A, Read KL, Mourant AJ, Wingham J, Thompson DR, Pereira Gray DJ. Home‐based versus hospital‐based rehabilitation after myocardial infarction: a randomized trial with preference arms—Cornwall Heart Attack Rehabilitation Management Study (CHARMS). Int J Cardiol. 2007;119:202–211. [DOI] [PubMed] [Google Scholar]
- 46. Medicare Advantage . The Henry J. Kaiser Family Foundation, Menlo Park, CA, May 11, 2016. http://www.kff.org/medicare/fact-sheet/medicare-advantage/. Accessed June 30, 2015. [Google Scholar]
- 47. Buchowski MS, Schlundt DG, Hargreaves MK, Hankin JH, Signorello LB, Blot WJ. Development of a culturally sensitive food frequency questionnaire for use in the Southern Community Cohort Study. Cell Mol Biol (Noisy‐le‐grand). 2003;49:1295–1304. [PubMed] [Google Scholar]
- 48. Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self‐reported diagnoses leading to hospitalization: a comparison of self‐reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147:969–977. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Census Tract Components of the Southern Community Cohort Study Neighborhood Deprivation Index, Stratified by Cardiac Rehabilitation Use (N=4096)


