Abstract
Controversy surrounds the remnant-preserving anterior cruciate ligament surgery. Advantages of remnant preservation have been reported in regard to better healing and knee function, although no consensus has been reached. This review article discussed the value and meaning of anterior cruciate ligament remnant preservation in several sections such as effects on healing, remnant classification, biomechanical evaluation, relation to proprioception, animal studies, and clinical studies. We hope that this review will facilitate further discussion and investigation for better treatment of anterior cruciate ligament injuries. So far, the current reviews have not provided sufficient scientific evidence to support the value of preserving the remnant.
Keywords: anterior cruciate ligament, healing, reconstruction, remnant, remnant preservation
Introduction
Ligament surgeons wish to achieve a better clinical outcome after anterior cruciate ligament (ACL) reconstruction. ACL reconstruction, a tendon graft surgery, is a gold standard treatment method for athletic patients who suffer from ACL insufficiency due to injury. Prolonged ACL insufficiency causes decreased athletic abilities, with repeated giving ways or fear of returning to original sports completely. In the long term, ACL injured knees develop arthritic changes combined with decreased meniscus function and articular cartilage injury. By contrast, athletic patients wish to return to sports as early as possible with higher performance, as possible after ACL reconstruction. Therefore, the healing process after ACL reconstruction should be accelerated as much as possible.
ACL surgeons have remaining unanswered questions regarding the ACL remnant and its handling. With ACL treatment history, proprioceptive function of the remnant was the focus in the earlier phase. A wide range of research has been conducted not only on surgical techniques for the remnant-preserving ACL reconstruction, but also on remnant cells for accelerating the healing process of the injured ACL.
How does one treat the ACL remnant? In this review article, in order to answer this question, we searched for articles in PubMed, with the keywords “anterior cruciate ligament” and “remnant,” from 2000 to June 2016. The search hit 157 titles. Forty-three articles were selected for replying to the question content. Another article before 2000 was added to reinforce the historical research direction. Secondary search for the comparative study between remnant-preserving and remnant-non-preserving surgeries found additional two articles. The authors attempted to answer each question accordingly. For the remaining questions, the authors included additional comments and questions for each issue.
ACL healing process after injury
Murray et al1 investigated the histology of injured ACL remnant tissues from operated cases. It was believed that the ACL had poor healing potential once injured; however, it was later reported that the ACL remnant also has healing potential and accomplished a similar healing process as other soft tissues. However, the report pointed out the concern that a layer of synovial tissue over the injured surface may disturb repair of the ligament. Contractile α-smooth muscle actin, which differentiates into myofibroblasts, causes lack of healing of the ruptured ACL. They suspected that contractile α-smooth muscle actin differentiates into myofibroblasts and causes lack of healing of the ruptured ACL.1 In another recent report regarding remnant healing, the ACL remnant that reattached to posterior cruciate ligament (PCL) was investigated focusing on α-smooth muscle actin and collagen Type 3. The results showed disorganized fibres with no definite direction and high collagen Type 3 expression.2 Previous findings suggest that proper mechanical stimulation to the remnant will be necessary for maturation and for obtaining higher function of the remnant. It remains unknown if the functional recovery of the remnant contributes to better knee joint function.
It is not very surprising on a small scale that injured ACL tissue requires the same healing process as other soft tissues. The real problems of the injured and reconstructed ACLs are the mechanical strength and anatomical healing. In our clinical experience, it is very rare to apply primary repair to an injured ACL (Figure 1).
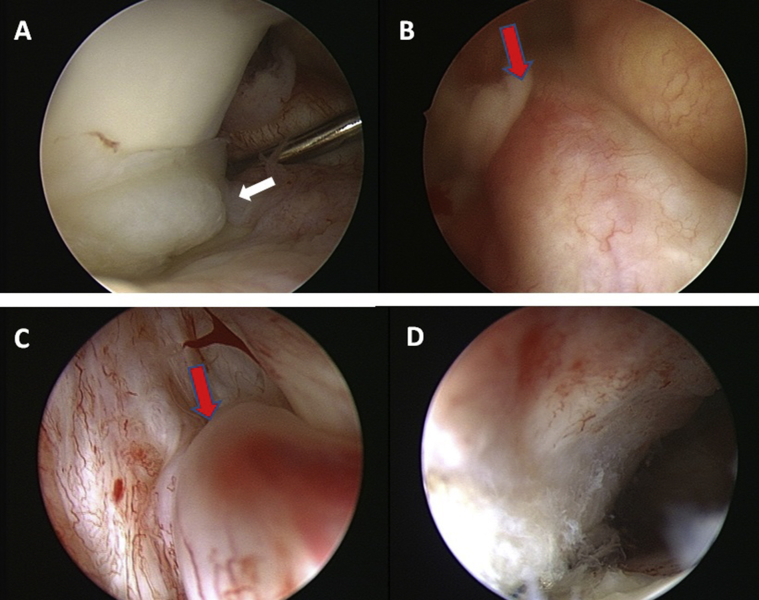
Figure 1.
A 43-year-old male got his right ACL injured 6 years before during a baseball game. Locking sensation of the right knee began 2 years later after the initial injury. He had his right knee locked and needed arthroscopic surgery eventually. Preoperative MRI suggested a locked lateral meniscus and an injured ACL with well-preserved configuration. (A) The white arrow indicates the locked lateral meniscus. (B) Arthroscopic observation found an injured ACL with well-preserved volume. (C) The red arrow suggests the centre of the injured site is around the femoral side of the midsubstance. (D) Arthroscopic view of the femoral insertion from behind the remnant demonstrates well-preserved fibrous extension of the injured ACL. The authors think that the case in which an ACL repair is included as the surgeon's strategy for managing ACL injury in the acute phase would be similar to the case presented in this figure. However, since the authors think that ACL repair is functionally and mechanically inferior to reconstructive surgery, the case underwent a double-bundle reconstruction of the authors' standard surgery. ACL = anterior cruciate ligament; MRI = magnetic resonance imaging.
Classification and significance of ACL remnant
Crain et al3 described and classified the ACL remnant into four types, and investigated the mechanical contribution of anterior–posterior laxity after removal of the remnant based on the type. They found that the remnant reattached to the notch wall had the highest contribution to the anterior–posterior translation evaluated by the KT-1000. Since publication, Crain et al's3 classification of the ACL remnant has been used as a standard. Remnant morphology of the ACL bundles after injury was assessed with three-dimensional computed tomography. The study demonstrates that the morphological patterns of the ACL remnants on three-dimensional computed tomography were well matched with arthroscopic findings without probing.4 Oblique coronal and oblique sagittal magnetic resonance images have been recommended to evaluate ACL remnant tissue. Orthogonal sagittal and oblique coronal images could reveal the morphology better than other images.5
The authors observe the femoral attachment of the ACL without any removal of the tissue behind the remnant using a 30° scope through the anteromedial portal. The ACL remnant after rupture remains as synovial and adipose scar tissues, which clearly indicates the original footprint, especially in the posterior part of the original ACL6 (Figure 2). Scoring of femoral ACL attachment with 90° flexion position behind the remnant. The probing on the anterior surface of ACL scar was very important to evaluate the integrity of the front side of the attachment. Femoral attachment of the ruptured ACL was evaluated by five categories (each 0–2) with 10 points as full marks. Direct insertion integrity: two points were given when more than two-thirds of the ligamentous attachment remained, and zero point when less than one-third remained at each third. The direct insertion was evaluated in each one-third portion as proximal, middle and distal. Fibrous extension integrity: two points were given when the fan-like fibrous extension was observed in more than half of the articular surface, and zero point when the fibrous extension was not observed. Synovitis severity: two points were given when only yellow and thin synovial tissue covered the behind-remnant area, and zero point to the severe synovitis as a finger-like proliferation. One point was given between 0 and 2 in each category.6 The score of the remaining attachment area showed a positive correlation with the preoperative instability and meniscus status (Figure 3).
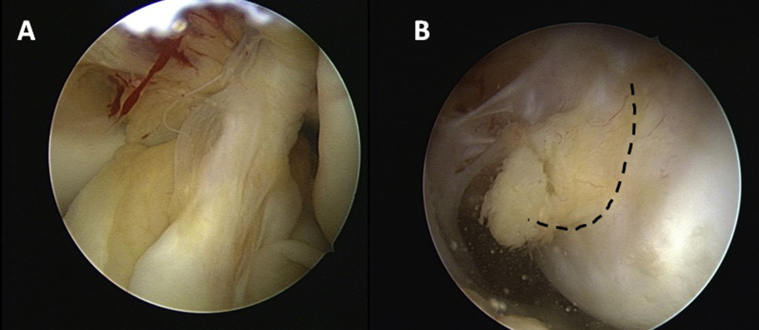
Figure 2.
(A) The injured ACL volume seems approximately one-third of the original one. (B) In femoral insertion, synovial and adipose proliferation indicates the injured portion, which delineates the normal fibrous extension (dotted line). ACL = anterior cruciate ligament.
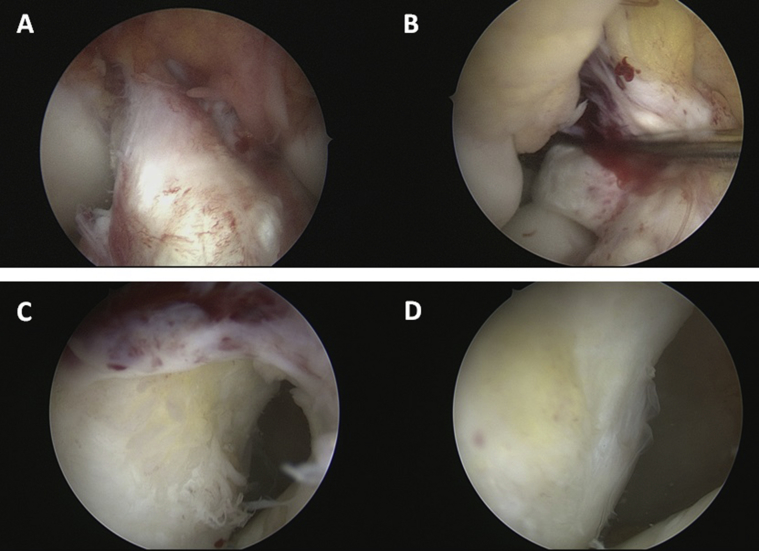
Figure 3.
(A) Frontal view of the injured ACL. (B) Probing clearly indicates laxity of the injured ACL. (C and D) Proximal, middle and distal portions of the direct insertion are scored as 2, 1, and 0, respectively. The fibrous extension is half preserved and pointed as 1. Little inflammatory synovial proliferation is found and pointed as 2. The number of total points is 6 in this case. ACL = anterior cruciate ligament.
Biomechanical evaluation of ACL remnant tissue
Nakamae et al7 evaluated anterior–posterior knee laxity using a navigation system to compare pre- and postremoval of ACL remnant tissue. They found that ACL remnants contributed to anterior–posterior knee laxity evaluated at 30° knee flexion for up to 1 year after injury. Biomechanical function of ACL remnants was relatively preserved up to 1 year after initial injury. However, the ACL remnant did not contribute to preserving rotational stability. Crain et al's3 classification was not useful in predicting ACL remnants' contribution to knee stability.8 Nakase et al9 also found that anterior laxity increased after Crain Type 3 remnant was removed using a navigation system during surgery. Nagai et al10 tested anterolateral rotatory instability pre- and postremoval of the ACL remnant using their three-dimensional electromagnetic measurement system. They found that ACL remnants attached to the lateral wall of the intercondylar notch partially contributed to anterior–posterior stability, but did not contribute to preserving rotational knee stability.
From the previous studies, remnant tissue has contributed to anterior–posterior knee laxity in some cases, but not to rotational stability. Moreover, it is questionable whether such remnant tissue can be utilized to reinforce graft tissue mechanically during ACL reconstruction.
Significance of ACL remnant preservation and proprioception of the knee
It is well known that many mechanoreceptors are distributed in the ACL tissue and remnant tissue contributes to proprioceptive function of the knee.11, 12 Mechanoreceptors exist not only in the intact ACL, but also in injured and even in reconstructed ones. Georgoulis et al13 reported the existence of mechanoreceptors in the ACL remnant 3 years after a rupture that attached to the PCL. Normal mechanoreceptors and proprioceptive fibres were positively stained with a monoclonal antibody for neurofilament protein in approximately 50% of ACL remnants.14 They also indicated differences among mechanoreceptors in healthy and injured ACLs and their clinical importance.15 Lee et al16 found mechanoreceptors in about one-third of their ACL remnants, which was less frequent than predicted. A morphologic and quantitative study of mechanoreceptors in the remnant stump of the human ACL suggests that the time from injury to surgery (log10 days) was negatively correlated with the number of total mechanoreceptors.17
Mechanoreceptors exist definitively in normal, injured, and grafted ACLs. However, the percentage of existence in injured and grafted ACLs is less than 100% and negatively correlated with the time from injury. Mechanoreceptors appear morphologically abnormal in the remnant and grafted tendons. Therefore, remnant-preserving surgery might be performed in an early phase after injury to maximize the remnant function reinforcing ACL reconstruction. Research regarding mechanoreceptor regeneration and its function in ACL reconstructed knees is still lacking.
Animal studies evaluating significance of remnant-preserving ACL surgery
Animal models have been used to evaluate the significance and meaning of remnant-preserving ACL reconstruction. Sun et al18 reported that reconstructed ACL in the 2-mm long tibial remnant group was mechanically stronger than that without any remnant tissue in a rabbit model. The same authors indicated significantly increased vascularity of the remnant-preserving group compared with that of the remnant debride group. The mechanical strength of the remnant-preserving group was higher even at 24 weeks after surgery.19 Song et al20 could not find any significance in an acute reconstruction model with and without remnant preservation. Takahashi et al21 mechanically investigated the significance of remnant-preserving ACL reconstruction using a sheep model until 12 weeks. Preservation of the ACL remnant tissue enhanced cell proliferation, revascularization, and regeneration of proprioceptive organs in the reconstructed ACL. The remnant-preserving group also showed reduced anterior knee translation. Contrarily, remnant preservation did not improve the structural properties of the graft.
Several animal models succeeded in demonstrating the significance of remnant-preserving surgery. Basic questions exist in that animal ACL reconstruction models were failure models. Is accelerated tissue healing advantageous to graft strength? It is still not clear whether the advantages of remnant-preserving technique are from high volume of graft tissue or biologic effects on tendon healing, or both, or neither.
Remnant-preserving ACL reconstruction
Arthroscopic findings of remnant footprint applied to remnant-preserving operative methods
The authors proposed a behind-remnant approach to observe the femoral footprint of the original ACL from the anteromedial portal without any debridement of the ruptured ACL tissue. The fibrous and synovial remnant tissues enable surgeons to image the shape and area of the original femoral footprint clearly. With this observation technique, ACL surgeons could identify the footprint to create the femoral tunnel anatomically without any debridement of the remnant22 (Figure 4). Sutter et al23 reported that the arthroscopic technique with a minimum amount of remnant debridement enables ACL surgeons to perform more accurate femoral placement. They visualized the existing footprint directly from the anteromedial portal combined with outside-in drilling.
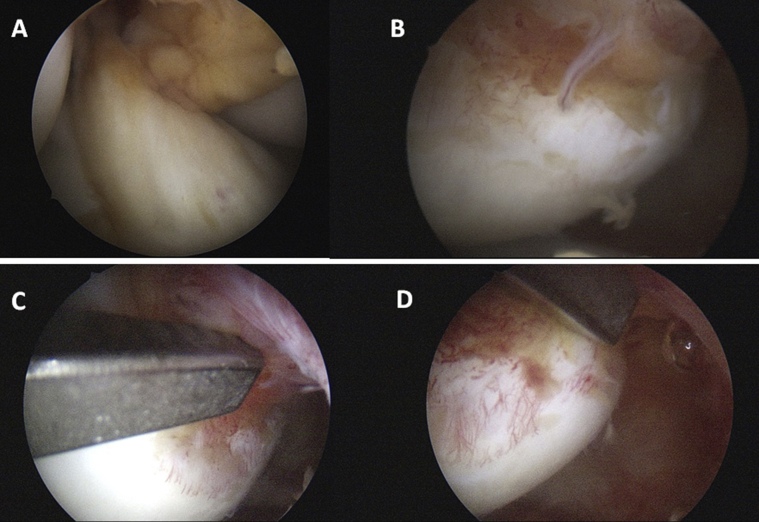
Figure 4.
(A) Frontal view of the injured ACL. (B) A view of the injured ACL from behind the remnant indicates the injured portion of the femoral attachment clearly. (C) Femoral guide position of the posterolateral bundle. (D) Femoral guide position of the anteromedial bundle. ACL = anterior cruciate ligament.
Clinical outcomes and significance
Kondo et al24 reported that remnant preservation in anatomic double-bundle ACL reconstruction did not significantly improve subjective and functional results in short-term evaluation. They found that the degree of initial graft coverage significantly affected postoperative knee stability. The study did not eliminate the important selection bias of cases with well-preserved remnant from those with not-well-preserved remnant. A randomized clinical trial for remnant-preserving surgery has been reported to investigate the effect of remnant preservation on tibial tunnel enlargement in a single-bundle ACL reconstruction technique using a hamstring autograft. Remnant preservation in ACL reconstruction can resist tibial tunnel enlargement, but this technique does not affect the short-term clinical outcome of ACL reconstruction.25 Another randomized clinical trial was performed with an allograft. The study showed that remnant preservation ACL reconstruction using an allograft had no evident advantages in clinical short-term outcome, with regard to stability, synovial coverage, and proprioception recovery, over the standard technique.26 Lu et al27 performed a prospective clinical study to compare two femoral tunnel creating methods, that is, based on bony landmarks versus existing footprint, during a double-bundle anatomic reconstruction. Double-bundle ACL reconstruction using the existing footprint remnant for tunnel placement demonstrated better functional results with respect to faster range of knee motion recovery, higher subjective outcome scores, and better arthroscopic second look with no revision cases at 2-year follow-up.
Second-look findings and clinical outcome after remnant-preserving technique
Based on the series of 66 consecutive patients who underwent second-look arthroscopy after remnant-preserving ACL reconstruction, cases with 50% or more preserved remnant showed thicker graft tissue with better synovial coverage.28 An arthroscopic second-look study has been performed to evaluate the effect of remnant preservation on the ACL graft using a bone-patellar bone-bone allograft. Fifty-one patients with a single-bundle allograft were involved in the study. The results suggested that Crain Type 3 and 4 ACL remnants demonstrated poorer synovial coverage.29 Another study indicated that second-look arthroscopy demonstrated better synovial coverage of the graft after remnant-preserving and retensioning ACL reconstruction.30
Other effects and remaining questions
Ahn et al31 reported an ACL reconstruction technique using remnant preservation and femoral tensioning. They found cyclops-like mass lesions in 12 cases; however, the mass did not cause any knee pain or extension deficit. Another analysis of cyclops lesions after different ACL reconstructions was performed with a comparison of the single-bundle and remnant bundle preservation techniques. One hundred consecutive patients operated on with the remnant-preserving technique were compared with 36 consecutive control patients with the single-bundle technique. The prevalence of a cyclops lesion was similar in both groups with postoperative magnetic resonance imaging evaluation.32
It has been reported that remnant-preserving surgery has advantages to reduce the graft rupture rate, based on the retrospective study of 218 patients. Preserving the remnant tissue of the ACL may facilitate recovery of function and decrease graft rupture after primary reconstruction.33
Review and meta-analysis with respect to the outcome of remnant-preserving technique
There have been several review studies regarding the efficacy of remnant-preserving ACL reconstruction. The assessment methods included proprioception, vascularization, and ligamentization. The results did not lead to firm evidence that preservation of the remnant confers clinically relevant advantages over its excision.
The possible advantages suggested in experimental studies are still not supported by clinical findings on the basis of a literature search. The conclusion of the review paper was that it is necessary to find a more direct way to assess proprioceptive function after ACL reconstruction and to appropriately conduct powered and rigorously prospective randomized double-blind studies, comparing the clinical outcomes of excising the remnant and leaving the remnant in situ.34
A systematic review showed significant postoperative improvements in patients undergoing remnant-preserving ACL reconstructions in all the studies. However, further comparisons between remnant-preserving ACL reconstruction and standard ACL reconstruction showed inconsistent results in seven comparative studies, with six reporting equivalent postoperative clinical outcomes between groups. No significant difference was found in the rate of total complications between groups.35
The current evidence from another systematic review suggests that short-term clinical outcomes of patients with the remnant augmentation technique are comparable with those of patients undergoing the standard technique, although it is insufficient to justify the remnant-preserving augmentation as a routine treatment for ACL ruptures.36 A literature search of randomized controlled clinical trials was performed comparing the clinical outcomes and complications of ACL reconstruction with remnant-preserving and standard single-bundle techniques. Six randomized controlled clinical trial were included, with a total of 378 patients. The outcome of single-bundle ACL reconstruction with the remnant-preserving technique is similar to that with the standard technique in terms of anterior stability and functional recovery of the knee.37
The authors re-searched the studies that evaluated the differences between remnant-preserving and standard surgeries. The re-search found six articles, four of which investigated the difference by magnetic resonance imaging and computed tomography image,27, 32, 38, 39 and four conducted clinical comparative studies.25, 26, 27, 38 Table 1 shows a summary of the six articles.
Table 1.
Summary of six comparative studies investigating differences between a remnant-preserving and a standard technique.
| Study reference no. | publication year | Study design | Study period: (remnant; control) | Remnant recruited (male, female) Control recruited (male; female) |
Age (y) (remnant/control) | Remnant control involved | Follow-up | Graft material | Reconstruction method | Outcome measures | Clinical measurements | MRI or radiographic evaluation Second-look evaluation |
Clinical evaluation | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gohil et al38 | 2007 | RCT | Not listed | R: 24 (14, 10) C: 25 (13, 12) |
R: 30.5 C: 35.5 |
R: 24 C: 25 |
1 y | Auto; hamstring | SB quadrupled hamstring | MRI (3 time points of 2 mo, 6 mo, 12 mo); clinical assessment | KT-1000 IKDC evaluation |
Remnant: earlier revascularization of midsubstance at 2 mo; signal reduction at 6 mo No difference of cyclops |
No differences in IKDC scores, ROM, KT measurements |
Earlier revascularization at 2 mo; no evidence of earlier recovery of the graft strength |
| Ahn et al39 | 2010 | Retrospective comparative cohort study | R: 07/2007–12/2008, C: 09/200–08/2005 |
R: 35 C: 6 |
R:29.2 C: not listed |
R: 41 C: 41 |
6.3 ± 0.7 | Auto; hamstring | SB quadrupled hamstring | MRI (1 time point of 6 mo; 5 measurements) |
Remnant: larger graft, SNQ (ns), cyclops (ns) |
More progressive remodelling of ACL graft with no increase of cyclops | ||
| Cha et al32 | 2012 | Retrospective comparative cohort study | 02/2007–8/2008; 05/2004–06/2009 | R: 100 (85, 15) C: 36 (31, 5) |
R: 31.9 C: 27.6 |
MRI/ pathology R: 100/4 C: 36/20 |
MRI: 214 d postop | Auto; hamstring | SB quadrupled hamstring | MRI; pathology | Graft lesion score (0, 1, 2, 3 = cyclops): R (4%, 60%, 2%, 7%), C (3%, 50%, 39%, 8%) (ns) Cyclops (+, –): R (12%, 88%), C (15%, 85%) (ns) |
The prevalence of cyclops lesions was not different | ||
| Hong et al25 | 2012 | RCT | 08/2008–04/2010 | R: 45 (33, 12) C: 45 (34, 11) |
R: 34 C: 28 |
Clinical/second look R: 39/28 C: 41/28 |
R: 25.8 C: 25.5 |
Allo | SB quadrupled hamstring | Clinical, second look, proprioception | Manual laxity tests KT-1000, Lysholm proprioception evaluation (passive angle) |
R: KT 1.6, Lysholm 99, passive angle 3.6 C: KT 1.8, Lysholm 95, passive angle 3.9 |
A short-term study showed no evident advantages | |
| Zhang et al26 | 2014 | RCT | 2006–2009 | R: 31 C: 31 |
R: 24 C: 25 |
R: 27 (21/6) C: 24(19/5) |
R: 24.4 C: 25.2 |
Auto; hamstring | SB quadrupled hamstring | Clinical, radiographic | KT-1000; Lysholm | R: KT 1.4, Lysholm 93 C: KT 1.7, Lysholm 91 (ns) |
Remnant preservation may decrease tunnel enlargement. They do not affect the short-term clinical outcome | |
| Lu et al27 | 2015 | RCT | 03/2009–05/2011 | R: 36 (36,0)* C: 36 (36,0) |
R: 29 C: 31 |
R: 36 C: 36 |
R: 35 C: 40 |
Auto; hamstring | DB double × 2 | 3D CT, clinical, second look | Pivot shift, KT-2000 Tegner, Lysholm, IKDC subjective |
R: PL has variation on femoral and tibial sides. C: both tunnels consistently placed with small differences Second-look evaluation was better in the R group. |
KT: R 0.68, C: 1.23 (ns) Tegner and Lysholm scores, ROM recovery was better in the remnant group. | Remnant-preservation group was superior to control in both clinical and second-look evaluations |
Remnant: a group using remnant-preserving technique, Control: a group of using standard technique.
Graft lesion score (0, 1, 2, 3 = cyclops).
ACL = anterior cruciate ligament; C = control group; MRI = magnetic resonance imaging; ns = not significantly different; R = remnant-preserving group; RCT = randomized controlled clinical trial; SNQ = signal of anterior cruciate ligament graft—signal of quadriceps tendon/signal of background; 3D CT = three-dimensional computed tomography.
At least the tibial remnant was preserved from the beginning of the 20-year experience of double-bundle semitendinosus tendon ACL reconstruction performed by the author. Anterior laxity has been improved along with the experience; however, patients' subjective evaluation has not changed much.40 The authors believe that the remaining remnant volume should be discussed before discussing the significance and meaning of the remnant-preserving technique. The preoperative condition of patients with ACL injuries was different depending upon the remnant volume. The remnant volume was also weakly correlated with the postoperative outcome regarding objective stability and subjective recovery. As remnant tissue reflects the preoperative condition of the patients; a randomized clinical trial should be conducted to evaluate the significance and meaning of the remnant-preserving postoperative outcome only in patients with sufficient remnant volume.41
ACL remnant-derived cells and their usefulness
Matsumoto et al42 found that ACL femoral tunnels stuffed using ruptured tissue produced less tunnel enlargement, as assessed by multidetector CT. The existence of mesenchymal stem cells (MSCs) in the ACL remnant was also reported by another research group.43 ACL-derived cells from younger patients enhanced early bone–tendon healing in an immunodeficient rat model of ACL reconstruction.44 ACL remnants of adolescent patients had more CD34+ cells, and those cells had a higher potential for proliferation and multilineage differentiation in vitro.45 That authors' group also revealed that the ACL remnant tissue harvested within 3 months after injury yields higher healing potential, suggesting that early surgical intervention may achieve better clinical results.46
The series of research from the group suggest that remnant tissue and cells derived from the remnant would be added as a new strategy to enhance healing of the ACL graft. Based on the authors' research in the field of MSCs, there is little doubt that MSCs exist in the ACL remnant.47 However, with regard to its clinical application, the potential advantages of remnant-derived MSCs are questionable. The number of MSCs would be very limited. There are insufficient biological advantages to convince surgeons to implement this procedure.
Conclusion
Remnant-preserving ACL reconstruction has higher potential for early healing, superior functional recovery, earlier return to sports, and lower occurrence of reinjury, although the scientific evidence to support the potential is not yet sufficient.
Conflicts of interest
The authors have no conflict of interest statement regarding this review article.
References
- 1.Murray M.M., Martin S.D., Martin T.L., Spector M. Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am. 2000;82:1387–1397. doi: 10.2106/00004623-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen D.T., Ramwadhdoebe T.H., van der Hart C.P., Blankevoort L., Tak P.P., van Dijk C.N. Intrinsic healing response of the human anterior cruciate ligament: an histological study of reattached ACL remnants. J Orthop Res. 2014;32:296–301. doi: 10.1002/jor.22511. [DOI] [PubMed] [Google Scholar]
- 3.Crain E.H., Fithian D.C., Paxton E.W., Luetzow W.F. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21:19–24. doi: 10.1016/j.arthro.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Adachi N., Ochi M., Takazawa K. Morphologic evaluation of remnant anterior cruciate ligament bundles after injury with three-dimensional computed tomography. Knee Surg Sports Traumatol Arthrosc. 2016;24:148–153. doi: 10.1007/s00167-014-3354-1. [DOI] [PubMed] [Google Scholar]
- 5.Kosaka M., Nakase J., Toratani T. Oblique coronal and oblique sagittal MRI for diagnosis of anterior cruciate ligament tears and evaluation of anterior cruciate ligament remnant tissue. Knee. 2014;21:54–57. doi: 10.1016/j.knee.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Muneta T., Koga H., Nakamura T., Horie M., Watanabe T., Sekiya I. Behind-remnant arthroscopic observation and scoring of femoral attachment of injured anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2015 Mar 13 doi: 10.1007/s00167-015-3574-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Nakamae A., Ochi M., Deie M. Biomechanical function of anterior cruciate ligament remnants: how long do they contribute to knee stability after injury in patients with complete tears? Arthroscopy. 2010;26:1577–1585. doi: 10.1016/j.arthro.2010.04.076. [DOI] [PubMed] [Google Scholar]
- 8.Maeda S., Ishibashi Y., Tsuda E., Yamamoto Y., Toh S. Intraoperative navigation evaluation of tibial translation after resection of anterior cruciate ligament remnants. Arthroscopy. 2011;27:1203–1210. doi: 10.1016/j.arthro.2011.03.080. [DOI] [PubMed] [Google Scholar]
- 9.Nakase J., Toratani T., Kosaka M., Ohashi Y., Tsuchiya H. Roles of ACL remnants in knee stability. Knee Surg Sports Traumatol Arthrosc. 2013;21:2101–2106. doi: 10.1007/s00167-012-2260-7. [DOI] [PubMed] [Google Scholar]
- 10.Nagai K., Araki D., Matsushita T. Biomechanical function of anterior cruciate ligament remnants: quantitative measurement with a 3-dimensional electromagnetic measurement system. Arthroscopy. 2016;32:1359–1366. doi: 10.1016/j.arthro.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 11.Schutte M.J., Dabezies E.J., Zimny M.L., Happel L.T. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am. 1987;69:243–247. [PubMed] [Google Scholar]
- 12.Adachi N., Ochi M., Uchio Y., Iwasa J., Ryoke K., Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73:330–334. doi: 10.1080/000164702320155356. [DOI] [PubMed] [Google Scholar]
- 13.Georgoulis A.D., Pappa L., Moebius U. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001;9:364–368. doi: 10.1007/s001670100240. [DOI] [PubMed] [Google Scholar]
- 14.Dhillon M.S., Bali K., Vasistha R.K. Immunohistological evaluation of proprioceptive potential of the residual stump of injured anterior cruciate ligaments (ACL) Int Orthop. 2010;34:737–741. doi: 10.1007/s00264-009-0948-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dhillon M.S., Bali K., Prabhakar S. Differences among mechanoreceptors in healthy and injured anterior cruciate ligaments and their clinical importance. Muscles Ligaments Tendons J. 2012;2:38–43. [PMC free article] [PubMed] [Google Scholar]
- 16.Lee B.I., Min K.D., Choi H.S. Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc. 2009;17:1095–1101. doi: 10.1007/s00167-009-0831-z. [DOI] [PubMed] [Google Scholar]
- 17.Gao F., Zhou J., He C. A morphologic and quantitative study of mechanoreceptors in the remnant stump of the human anterior cruciate ligament. Arthroscopy. 2016;32:273–280. doi: 10.1016/j.arthro.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Sun L., Wu B., Tian M., Liu B., Luo Y. Comparison of graft healing in anterior cruciate ligament reconstruction with and without a preserved remnant in rabbits. Knee. 2013;20:537–544. doi: 10.1016/j.knee.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Wu B., Zhao Z., Li S., Sun L. Preservation of remnant attachment improves graft healing in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1362–1371. doi: 10.1016/j.arthro.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 20.Song G.Y., Zhang J., Li X., Li Y., Feng H. Biomechanical and biological findings between acute anterior cruciate ligament reconstruction with and without an augmented remnant repair: a comparative in vivo animal study. Arthroscopy. 2016;32:307–319. doi: 10.1016/j.arthro.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi T., Kondo E., Yasuda K. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: a biomechanical and histological study. Am J Sports Med. 2016;44:1708–1716. doi: 10.1177/0363546516643809. [DOI] [PubMed] [Google Scholar]
- 22.Muneta T., Koga H., Nakamura T. A new behind-remnant approach for remnant-preserving double-bundle anterior cruciate ligament reconstruction compared with a standard approach. Knee Surg Sports Traumatol Arthrosc. 2015;23:3743–3749. doi: 10.1007/s00167-014-3300-2. [DOI] [PubMed] [Google Scholar]
- 23.Sutter E.G., Anderson J.A., Garrett W.E., Jr. Direct visualization of existing footprint and outside-in drilling of the femoral tunnel in anterior cruciate ligament reconstruction in the knee. Arthrosc Tech. 2015;4:e107–e113. doi: 10.1016/j.eats.2014.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kondo E., Yasuda K., Onodera J., Kawaguchi Y., Kitamura N. Effects of remnant tissue preservation on clinical and arthroscopic results after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:1882–1892. doi: 10.1177/0363546515587713. [DOI] [PubMed] [Google Scholar]
- 25.Hong L., Li X., Zhang H. Anterior cruciate ligament reconstruction with remnant preservation: a prospective, randomized controlled study. Am J Sports Med. 2012;40:2747–2755. doi: 10.1177/0363546512461481. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Q., Zhang S., Cao X., Liu L., Liu Y., Li R. The effect of remnant preservation on tibial tunnel enlargement in ACL reconstruction with hamstring autograft: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2014;22:166–173. doi: 10.1007/s00167-012-2341-7. [DOI] [PubMed] [Google Scholar]
- 27.Lu W., Wang D., Zhu W. Placement of double tunnels in ACL reconstruction using bony landmarks versus existing footprint remnant: a prospective clinical study with 2-year follow-up. Am J Sports Med. 2015;43:1206–1214. doi: 10.1177/0363546515570850. [DOI] [PubMed] [Google Scholar]
- 28.Kim M.K., Lee S.R., Ha J.K., Ra H.J., Kim S.B., Kim J.G. Comparison of second-look arthroscopic findings and clinical results according to the amount of preserved remnant in anterior cruciate ligament reconstruction. Knee. 2014;21:774–778. doi: 10.1016/j.knee.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 29.Guo L., Chen H., Luo J.M., Yang L., Gu L.C., Fu D.J. An arthroscopic second-look study on the effect of remnant preservation on synovialization of bone-patellar tendon-bone allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2016;32:868–877. doi: 10.1016/j.arthro.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 30.Noh J.H., Kyung H.S., Roh Y.H., Kang T.S. Remnant-preserving and re-tensioning technique to cover the graft in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015 Nov 12 doi: 10.1007/s00167-015-3854-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Ahn J.H., Wang J.H., Lee Y.S., Kim J.G., Kang J.H., Koh K.H. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy. 2011;27:1079–1089. doi: 10.1016/j.arthro.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Cha J., Choi S.H., Kwon J.W., Lee S.H., Ahn J.H. Analysis of cyclops lesions after different anterior cruciate ligament reconstructions: a comparison of the single-bundle and remnant bundle preservation techniques. Skelet Radiol. 2012;41:997–1002. doi: 10.1007/s00256-011-1347-4. [DOI] [PubMed] [Google Scholar]
- 33.Takazawa Y., Ikeda H., Kawasaki T. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113505076. eCollection 2013 Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Papalia R., Franceschi F., Vasta S., Di Martino A., Maffulli N., Denaro V. Sparing the anterior cruciate ligament remnant: is it worth the hassle? Br Med Bull. 2012;104:91–111. doi: 10.1093/bmb/ldr053. [DOI] [PubMed] [Google Scholar]
- 35.Song G.Y., Zhang H., Zhang J. The anterior cruciate ligament remnant: to leave it or not? Arthroscopy. 2013;29:1253–1262. doi: 10.1016/j.arthro.2013.03.078. [DOI] [PubMed] [Google Scholar]
- 36.Hu J., Qu J., Xu D., Zhang T., Zhou J., Lu H. Clinical outcomes of remnant preserving augmentation in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:1976–1985. doi: 10.1007/s00167-013-2749-8. [DOI] [PubMed] [Google Scholar]
- 37.Tie K., Chen L., Hu D., Wang H. The difference in clinical outcome of single-bundle anterior cruciate ligament reconstructions with and without remnant preservation: a meta-analysis. Knee. 2016;23:566–574. doi: 10.1016/j.knee.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 38.Gohil S., Annear P.O., Breidahl W. Anterior cruciate ligament reconstruction using autologous double-hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularization. A randomized prospective study with one-year follow-up. J Bone Joint Surg Br. 2007;89:1165–1171. doi: 10.1302/0301-620X.89B9.19339. [DOI] [PubMed] [Google Scholar]
- 39.Ahn J.H., Lee S.H., Choi S.H., Lim T.K. Magnetic resonance imaging evaluation of anterior ligament reconstruction using quadrupled hamstring tendon autografts: comparison of remnant bundle preservation and standard technique. Am J Sports Med. 2015;38:1768–1777. doi: 10.1177/0363546510368132. [DOI] [PubMed] [Google Scholar]
- 40.Muneta T. Twenty-year experience of a double-bundle anterior cruciate ligament reconstruction. Clin Orthop Surg. 2015;7:143–151. doi: 10.4055/cios.2015.7.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muneta T., Koga H., Ju Y.J., Horie M., Nakamura T., Sekiya I. Remnant volume of anterior cruciate ligament correlates preoperative patients' status and postoperative outcome. Knee Surg Sports Traumatol Arthrosc. 2013;21:906–913. doi: 10.1007/s00167-012-2023-5. [DOI] [PubMed] [Google Scholar]
- 42.Matsumoto T., Kuroda R., Matsushita T. Reduction of tunnel enlargement with use of autologous ruptured tissue in anterior cruciate ligament reconstruction: a pilot clinical trial. Arthroscopy. 2014;30:468–474. doi: 10.1016/j.arthro.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 43.Fu W., Li Q., Tang X., Chen G., Zhang C., Li J. Mesenchymal stem cells reside in anterior cruciatess ligament remnants in situ. Int Orthop. 2016;40:1523–1530. doi: 10.1007/s00264-015-2925-1. [DOI] [PubMed] [Google Scholar]
- 44.Nakano N., Matsumoto T., Takayama K. Age-dependent healing potential of anterior cruciate ligament remnant-derived cells. Am J Sports Med. 2015;43:700–708. doi: 10.1177/0363546514561436. [DOI] [PubMed] [Google Scholar]
- 45.Uefuji A., Matsumoto T., Matsushita T. Age-related differences in anterior cruciate ligament remnant vascular-derived cells. Am J Sports Med. 2014;42:1478–1486. doi: 10.1177/0363546514529092. [DOI] [PubMed] [Google Scholar]
- 46.Zhang S., Matsumoto T., Uefuji A. Anterior cruciate ligament remnant tissue harvested within 3-months after injury predicts higher healing potential. BMC Musculoskelet Disord. 2015;16:390. doi: 10.1186/s12891-015-0855-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koga H., Engebretsen L., Brinchmann J.E., Muneta T., Sekiya I. Mesenchymal stem cell-based therapy for cartilage repair: a review. Knee Surg Sports Traumatol Arthrosc. 2009;17:1289–1297. doi: 10.1007/s00167-009-0782-4. [DOI] [PubMed] [Google Scholar]