Abstract
Objective
This study aimed to evaluate the accuracy of magnetic resonance imaging (MRI) in diagnosing lateral ankle ligament injuries and the effect of differences in time duration from injury to MRI.
Methods
Data were collected prospectively from 82 patients who underwent MRI and lateral ligament reconstruction, and were divided into either acute (≤3 months) or chronic (>3 months) group based on injury interval. Findings were classified as normal, partial, or complete tears of the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL). MRI results were compared with intraoperative findings and their accuracies were assessed using descriptive statistics.
Results
The accuracy of MRI for partial and complete tears of the ATFL was 74% and 79%, respectively, with sensitivity and specificity of 64% and 86% for partial tears, and 78% and 80% for complete tears, respectively. The accuracy of MRI was 66% and 88% for partial and complete tears of the CFL with a sensitivity and specificity of 41% and 87% for partial tears, and 61% and 95% for complete tears, respectively. A decrease in the MRI accuracy was observed in the chronic group.
Conclusion
MRI is accurate in diagnosing ATFL injuries. It is specific but not sensitive for CFL tears. The accuracy is higher in the acute setting of 3 months or less from time of injury to MRI.
Keywords: accuracy, ankle, ligaments, magnetic resonance imaging
Introduction
Ankle sprains are common injuries, and a significant risk factor for developing chronic ankle instability and pain.1, 2, 3, 4 Magnetic resonance imaging (MRI) is increasingly being utilized in assessing patients with residual symptoms after initial conservative treatment because of its superior soft-tissue resolution and good correlation with objective arthroscopic findings.5 The lateral ligamentous complex is involved in the majority of ankle sprain injuries, and comprises the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL).1, 6, 7, 8 The lateral complex hence remains the largest concern of orthopaedic surgeons for patients failing initial conservative treatment for acute ankle sprains and chronic ankle instability symptoms, especially in consideration of ligamentous tears.
Great variability exists in the accuracy of MRI, and the reliability of findings on MRI has not been confirmed.9 One study noted an MRI accuracy of 80% in detecting osteochondral lesions in the talus and peroneus brevis tendon tears,10 whereas another study reported a 19% detection rate of cartilage lesions found at surgery.11 For the few studies that evaluated the lateral ankle ligamentous complex, significantly different sensitivities and specificities for detecting ATFL and CFL tears have been reported.12, 13 In addition, these studies had focused only on patients with chronic symptoms and injuries and there remains a paucity in the literature on the accuracy of MRI in the acute setting. An MRI scan of acutely injured ankle ligaments may demonstrate the presence of haemorrhage in the joint space and soft-tissue swelling over the lateral malleolus as well as high bone signal at ligament avulsion sites, which may be absent in patients with recurrent or chronic problems.14 Hence, we hypothesized that the accuracy of MRI in the acute setting will be higher than in the chronic setting. Given the variability in the accuracy of ankle MRIs, it is difficult to justify its usage in identifying lateral ligamentous injuries due to the prohibitive costs of MRI and its eventual cost-effectiveness.15
The primary objective of this study was to evaluate the accuracy of MRI results in lateral ankle ligament injuries in comparison with intraoperative findings, which are used as the standard of reference. The secondary objective was to compare the accuracy of MRI between the acute and chronic groups of patients with ankle instability symptoms after injury. To the best of the authors’ knowledge, this is the first study to date to evaluate the relationship between accuracy of MRI and timing of scans.
Materials and methods
Study design
In this institutional review board-approved study (Reference number: nuh/2014-00019), data were collected prospectively for patients who underwent lateral ligament reconstruction surgery at a high-volume tertiary institution from January 2012 to December 2014. The inclusion criteria were patients who (1) had a history of acute ankle sprain injury; (2) had residual symptoms of pain, swelling, or instability after conservative treatment including rest, analgesia, ankle guard, and physiotherapy for at least 6 weeks; (3) had positive clinical findings suggestive of ligamentous injury such as positive anterior drawer test and/or talar tilt test; (4) were evaluated with MRI prior to surgery as part of the departmental protocol and as an objective supportive investigation; and (5) subsequently underwent reconstruction of the ATFL and/or the CFL via a modified Broström procedure. The exclusion criteria were (1) previous ankle surgeries; (2) previously diagnosed ankle ligament tears prior to current presentation; (3) new injury from time of MRI to surgery; (4) no MRI was performed prior to surgery due to reasons such as severe trauma or open injuries; and (5) presence of other injuries detected on MRI other than ATFL/CFL tears. The indications for surgery were (1) persistence of symptoms after at least 6 weeks of conservative treatment; and (2) presence of ligamentous tear on MRI; or (3) positive anterior drawer/talar tilt test if MRI is negative. The patients were divided into acute or chronic groups arbitrarily. Acute was defined by an interval of 3 months or less from time of injury to time of MRI, whereas chronic was defined as an interval of more than 3 months. A sample of convenience was used.
Radiological investigations
MRI was obtained from the institutional radiology provider. Patients without MR images at consultation were referred for MRI noting the history of lateral ankle instability. All patients had an MRI with a 3.0-T magnet, and MRI scans were performed without contrast or arthrogram. All MRI results were interpreted by the same team of fellowship-trained radiologists. We reviewed the original radiologist’s MRI report and verified it with the MRI images itself, and recorded the assessment of the ligaments, separating the results of the ATFL and CFL.
Outcome measurements
Results were classified as normal, partial tear, or complete tear as described by Joshy et al.16 Partial tear was defined as partial adhesion of the ligament fibres and a coarse cut fibre surface with intact continuity. Complete tear was defined as definite discontinuity of the ligament and adhesion of adjacent tissue.14, 17 Patients with both ATFL and CFL injuries were analysed as two distinct injuries. The MRI results were compared with the operative findings, which were used as the standard of reference. All surgeries were performed by two experienced foot and ankle surgeons. The ATFL and CFL were routinely assessed intraoperatively.
Statistical analysis
Patient characteristics were analysed descriptively. Mean and standard deviation were reported for numerical variables, whereas the number of patients and percentages were reported for categorical variables. Performance of MRI was assessed using descriptive statistics to generate sensitivity, specificity, and positive predictive and negative predictive values with 95% confidence intervals. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) version 22.0 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
A total of 114 patients underwent lateral ankle ligament reconstruction from January 2012 to December 2014, of which 82 (72%) fulfilled the inclusion criteria. There were 40 (49%) patients in the acute group and 42 (51%) in the chronic group. Patient characteristics are presented in Table 1. No significant characteristics were detected between the acute and chronic groups.
Table 1.
Patient characteristics.
| Characteristics | Total (n = 82) | Acute (n = 40) | Chronic (n = 42) | p |
|---|---|---|---|---|
| Age (y), mean (range) | 25.3 (17–48) | 25.8 (17–47) | 24.8 (17–48) | 0.285 |
| Sex | 0.408 | |||
| Male, n (%) | 71 (87) | 35 (87) | 36 (86) | |
| Female, n (%) | 11 (13) | 5 (13) | 6 (14) | |
| Race | 0.210 | |||
| Chinese, n (%) | 59 (72) | 30 (75) | 29 (69) | |
| Malay, n (%) | 14 (17) | 3 (8) | 11 (26) | |
| Indian, n (%) | 6 (7) | 4 (10) | 2 (5) | |
| Others, n (%) | 3 (4) | 3 (8) | 0 (0) | |
| Body mass index, (kg/m2), mean ± standard deviation | 25.0 ± 5.3 | 23.9 ± 4.6 | 26.1 ± 5.6 | 0.091 |
Comparison of MRI results versus intraoperative findings
Table 2 compares the positive and negative findings on MRI with intraoperative findings overall. A total of 11 ATFLs and 24 CFLs were reported normal on MRI but were found torn intraoperatively; 34 partial tears and 37 complete tears of the ATFL were reported on MRI, whereas operative evaluation yielded 45 partial tears and 36 complete tears. There were also false positives of five partial and nine complete tears of the ATFL on MRI. For the CFL, 21 partial tears and 14 complete tears were reported on MRI, whereas 37 partial tears and 18 complete tears were found intraoperatively. As much as 15 partial and 11 complete tears of the CFL were diagnosed correctly on MRI, but 22 partial and seven complete tears of the CFL were missed on MRI. Six partial and three complete tears of the CFL were falsely positive on MRI. Table 3, Table 4 compare the same format of results for the acute and chronic groups of patients, respectively.
Table 2.
Comparison of MRI results with intraoperative findings.
| Degree of injury | ATFL |
CFL |
||
|---|---|---|---|---|
| Surgery (+) | Surgery (−) | Surgery (+) | Surgery (−) | |
| Normal | ||||
| MRI (+) | 0 | 11 | 23 | 24 |
| MRI (−) | 1 | 70 | 4 | 31 |
| Partial tear | ||||
| MRI (+) | 29 | 5 | 15 | 6 |
| MRI (−) | 16 | 32 | 22 | 39 |
| Complete tear | ||||
| MRI (+) | 28 | 9 | 11 | 3 |
| MRI (−) | 8 | 37 | 7 | 61 |
+ indicates presence of; − indicates absence of.
ATFL = anterior talofibular ligament; CFL = calcaneofibular ligament; MRI = magnetic resonance imaging.
Table 3.
Comparison of MRI results and operative findings (acute).
| Degree of injury | ATFL |
CFL |
||
|---|---|---|---|---|
| Surgery (+) | Surgery (−) | Surgery (+) | Surgery (−) | |
| Normal | ||||
| MRI (+) | 0 | 2 | 9 | 13 |
| MRI (−) | 0 | 38 | 2 | 16 |
| Partial tear | ||||
| MRI (+) | 16 | 1 | 10 | 2 |
| MRI (−) | 7 | 16 | 12 | 16 |
| Complete tear | ||||
| MRI (+) | 15 | 6 | 5 | 1 |
| MRI (−) | 2 | 17 | 2 | 32 |
+ indicates presence of; − indicates absence of.
ATFL = anterior talofibular ligament; CFL = calcaneofibular ligament; MRI = magnetic resonance imaging.
Table 4.
Comparison of MRI results and operative findings (chronic).
| Degree of injury | ATFL |
CFL |
||
|---|---|---|---|---|
| Surgery (+) | Surgery (−) | Surgery (+) | Surgery (−) | |
| Normal | ||||
| MRI (+) | 0 | 9 | 14 | 11 |
| MRI (−) | 1 | 32 | 2 | 15 |
| Partial tear | ||||
| MRI (+) | 13 | 4 | 5 | 4 |
| MRI (−) | 9 | 16 | 10 | 23 |
| Complete tear | ||||
| MRI (+) | 13 | 3 | 6 | 2 |
| MRI (−) | 6 | 20 | 5 | 29 |
+ indicates presence of; − indicates absence of.
ATFL = anterior talofibular ligament; CFL = calcaneofibular ligament; MRI = magnetic resonance imaging.
Performance of MRI in detecting lateral ankle ligament injuries
Table 5 presents the overall analysis of the performance of MRI in detecting lateral ankle ligament injuries. The accuracies in detecting partial and complete ATFL tears are 74% and 79%, respectively. The sensitivity and specificity are 64% and 86%, respectively, for partial tears, and 78% and 80%, respectively, for complete tears. The accuracies of MRI in detecting partial and complete CFL tears were 66% and 88%, respectively. The sensitivity and specificity are 41% and 87%, respectively, for partial tears, and 61% and 95%, respectively, for complete tears. Table 6 compares the same format of overall accuracy results for the acute and chronic groups.
Table 5.
Performance of MRI in various degrees of ligamentous injury.
| Degree of injury | Ligament | Sensitivity/% (95% CI) | Specificity/% (95% CI) | PPV (95% CI) | NPV (95% CI) | Accuracy |
|---|---|---|---|---|---|---|
| Normal | ATFL | 0 (0–94) | 86 (77–93) | 0 (0–32) | 99 (91–100) | 85 |
| CFL | 85 (65–91) | 56 (42–69) | 49 (34–64) | 89 (72–96) | 66 | |
| Partial tear | ATFL | 64 (49–78) | 86 (70–95) | 85 (68–94) | 67 (51–79) | 74 |
| CFL | 41 (25–58) | 87 (73–94) | 71 (48–88) | 64 (51–76) | 66 | |
| Complete tear | ATFL | 78 (60–89) | 80 (66–90) | 76 (58–88) | 82 (67–91) | 79 |
| CFL | 61 (36–81) | 95 (86–99) | 79 (49–94) | 90 (79–95) | 88 |
ATFL = anterior talofibular ligament; CFL = calcaneofibular ligament; CI = confidence interval; MRI = magnetic resonance imaging; NPV = negative predictive value; PPV = positive predictive value.
Table 6.
Comparison of performance of MRI by duration classification.
| Degree of injury | Ligament | Acute |
Chronic |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sn | Sp | PPV | NPV | Acc | Sn | Sp | PPV | NPV | Acc | ||
| Normal | ATFL | 0 | 95 | 0 | 100 | 95 | 0 | 78 | 0 | 97 | 76 |
| CFL | 82 | 55 | 41 | 89 | 63 | 88 | 58 | 56 | 88 | 69 | |
| Partial tear | ATFL | 70 | 94 | 94 | 70 | 80 | 9 | 80 | 33 | 44 | 43 |
| CFL | 45 | 89 | 83 | 57 | 65 | 33 | 85 | 56 | 70 | 67 | |
| Complete tear | ATFL | 88 | 74 | 71 | 89 | 80 | 68 | 87 | 81 | 77 | 79 |
| CFL | 71 | 97 | 83 | 94 | 93 | 55 | 94 | 75 | 85 | 83 | |
Acc = accuracy; ATFL = anterior talofibular ligament; CFL = calcaneofibular ligament; MRI = magnetic resonance imaging; NPV = negative predictive value; PPV = positive predictive value; Sn = sensitivity; Sp = specificity.
Discussion
The ATFL is the weakest ligament of the lateral ligamentous complex, followed by the CFL.18 Hence, there is a predictable sequence of injury in lateral ankle sprains, first involving the ATFL, followed by the CFL, and finally, the PTFL.19, 20 The ATFL and CFL are commonly injured, whereas the PTFL is rarely torn except in cases of complete dislocation of the ankle.21 The most common mechanism of injury is inversion stress and the MRI may show the ATFL to be attenuated, lax, or discontinuous. The CFL may also be injured due to increased severity of the inversion stress, and is almost always associated with an ATFL injury.1 Injury to the PTFL is uncommon and is almost always associated with injury to both the ATFL and CFL.1 No cases of PTFL injury were observed in this study.
Treatment of the Grade 3 ankle sprains remains controversial. One study has reported that conservative treatment leads to satisfactory results.22 Majority of the current literature shows that despite proper conservative treatment, patients may continue to experience residual pain, swelling, and instability requiring eventual surgery.23, 24, 25 This figure was found to be at 39% in a long-term follow-up study.4 Pijnenburg et al22 reported that surgery led to a superior long-term outcome. Therefore, surgical intervention has proven beneficial for patients who have residual symptoms of instability after failing conservative treatment.
The results of our findings are consistent with two previous similarly designed studies. Park et al13 and Kumar et al12 both reported the sensitivity and specificity of MRI of ATFL and CFL tears. Kumar et al12 reported the ATFL sensitivity and specificity to be 87% and 60%, respectively, with an accuracy of 71%, whereas the CFL sensitivity and specificity were 47% and 83%, respectively, with an accuracy of 72%. Park et al13 reported a lower sensitivity for both ATFL and CFL (ATFL, 44–75%; CFL, 50–83%) but a higher specificity (ATFL, 78–88%; CFL, 78–88%). Our study shows ATFL sensitivity of 64–78% and specificity of 80–86%, whereas CFL sensitivity was 45–71% with specificity of 89–97%, and these values support the results of Park et al,13 that is, lower sensitivity but higher specificity for lesions in the ATFL and the CFL.
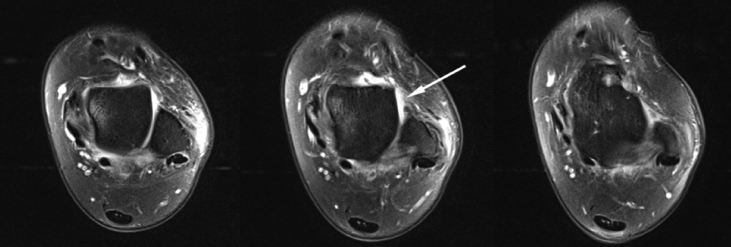
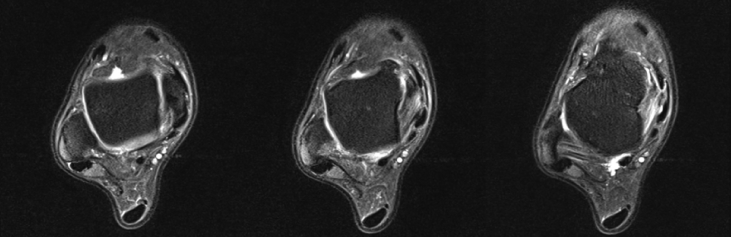
In this study, we observed a high degree of correlation between MRI and intraoperative findings. However, mismatches were noted. A total of 37 cases showed complete ATFL tear on MRI, but nine were shown to be falsely positive during surgery, as well as eight false negatives (sensitivity, 78%; specificity, 80%). An example is shown in Figure 1, where it was reported as a complete tear of the ATFL on MRI, but was shown to be falsely positive during surgery (i.e., normal ATFL). There were more cases of MRI misdiagnosis for partial tears of the ATFL. A total of 16 partial tears of the ATFL were missed on MRI, and five partial tears diagnosed on MRI were shown to be false positives (sensitivity, 64%; specificity, 86%). Similar results were noted with CFL tears. Figure 2 shows a case of a false-negative report of normal ATFL on MRI, but was shown to be completely torn during surgery.
Figure 1.
False-positive magnetic resonance imaging report of a complete tear of the left ankle anterior talofibular ligament that was found to be normal intraoperatively.
Figure 2.
False-negative magnetic resonance imaging report of normal right ankle anterior talofibular ligament that was found to be a complete tear intraoperatively.
The superiority of MRI in providing a high soft-tissue contrast in imaging is well established.5 However, limitations exist, which could possibly account for the discrepancy between MRI and operative findings. First, two studies to date have reported that the validity of MRI could possibly be affected by the position of the ankle joint during the imaging process.26, 27 Differences in the tautness or laxity of the ligaments in plantarflexion or dorsiflexion have been proposed to affect the interpretation of the integrity of the ligaments. There are currently no standardized protocols for ankle positioning during MRI. Second, small lesions in cases of partial tears are often difficult to detect by MRI due to a total volume effect related to the 3-mm section thickness.28 This may account for the overall lower performance for partial tears in contrast to complete tears reported in this study. Lastly, Kim et al29 recently described the site of the ligament injury as a factor for increased rates of false-negative diagnoses. The study noted an increase in false-negative diagnoses with injuries occurring at the fibular or talar attachment site due to fibrous adhesions from the healing process, which makes torn ligaments appear intact. This could possibly explain the case featured in Figure 2 where a completely torn CFL was reported as partially torn on MRI.
This is the first study to date to evaluate the accuracy of MRI between the acute and chronic groups of patients with ankle instability symptoms. In addition, this is the largest study of comparison between MRI and operative findings. Based on the comparison shown in Table 6, MRI has better accuracy in diagnosing both normal ligament and torn ATFL in the acute group. For the CFL, MRI has better accuracy in the acute group of patients as well as in the chronic group except for complete chronic CFL tears. A considerable drop in sensitivity was noted in detecting both partial and complete tears of the ATFL [partial tear of the ATFL, 70% sensitivity (acute) vs. 9% sensitivity (chronic); complete tear of the ATFL, 88% sensitivity (acute) vs. 68% sensitivity (chronic)], as well as for the CFL [partial tear of the CFL: 45% sensitivity (acute) vs. 33% sensitivity (chronic); complete tear of the CFL: 71% sensitivity (acute) vs. 55% sensitivity (chronic)]. This is an expected reflection of the difficulty of making an MRI diagnosis in patients with recurrent or chronic problems as opposed to those with acutely injured ankles. An MRI scan of acutely injured ankle ligaments may demonstrate the presence of haemorrhage in the joint space and soft-tissue swelling over the lateral malleolus as well as high bone signal at ligament avulsion sites, which may be absent in patients with recurrent or chronic problems.14 Therefore, in the context of chronic symptoms and a high suspicion of ligament pathology, negative MRI results should be viewed with caution due to the lower sensitivity and negative predictive values observed in the chronic group. However, MRI can still provide useful information on associated pathologies, which can mimic chronic symptoms of ligament tears. These include chondral lesions and loose bodies, which can be diagnosed by MRI.12
Other methods of diagnosing ligament pathology have been evaluated in some studies. Stress radiography has shown promising results in providing a reliable dynamic test of the integrity of the lateral ligaments.30 Ultrasonography has demonstrated an equally high efficacy for detecting lateral ligament tears while being a considerably cheaper alternative to MRI.31 Of note, Cheng et al32 constructed a similarly designed study (n = 120) to ours, evaluating the accuracy of ultrasonography instead of MRI, using operative findings as the standard of reference. The authors reported the sensitivity, specificity, and accuracy of ultrasonography to be 98.9%, 96.2%, and 84.2%, respectively, for ATFL tears, and 93.8%, 90.9%, and 83.3%, respectively, for CFL tears. Based on the study by Cheng et al,32 the sensitivity, specificity, and accuracy of ultrasonography are equal to, or even superior to, MRI based on our results. However, another study by Oae et al17 reported sonographic sensitivity of 100% and a specificity of 33%, using arthroscopy as the standard of reference, and hence evidence regarding the accuracy of ultrasonography is still variable, and more studies evaluating the accuracy of ultrasonography are needed. Ultrasonography itself also presents its own limitation, being dependent on the expertise of the technician.13 It is still important to consider the fact that the costs of MRI remain prohibitive, which affects the cost-effectiveness of using MRI as a modality to evaluate lateral ankle injuries.28 From these studies, ultrasonography has shown promise in being as efficacious as MRI as an imaging modality to evaluate lateral ankle ligament injuries, but there is still not enough literature describing its accuracy in comparison with MRI.
Although the construct of our study is sound and thorough, there are a few limitations worth noting. First, the relatively small number of patients included may have limited the analysis of the outcomes in each subgroup. However, to the best of the authors’ knowledge, this is the largest study to date. Second, there is lack of control of interobserver variability in the interpretation of MRI results, which could increase the variability in MRI accuracy. However, a previous study had reported a low interobserver variability in MRI diagnosis for ligament lesions.32 Third, there may be an inherent bias in patient selection, because no patient will be operated on if they do not have symptoms of ankle instability, but this reflects the reality of practice. Lastly, this study mainly evaluated MRI reporting in a clinical setting and may not be a true reflection of the accuracy of the MRI in diagnosing lateral ligament injuries.
In conclusion, MRI was able to accurately diagnose lateral ankle ligament tears in most cases. Diagnosis of a complete ATFL tear on MRI is more sensitive than that of complete CFL tear. The MRI findings of CFL injury were diagnostically specific but were not sensitive. The accuracy of MRI is higher in the acute setting of within 3 months from the time of injury to MRI.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
No financial or material support of any kind was received for the work described in this article. We would like to thank the clinical coordinators from the Department of Orthopaedic Surgery, National University Hospital for their effort and contribution in the collation of data used in the analysis of this study.
References
- 1.Erickson S.J., Smith J.W., Ruiz M.E., Fitzgerald S.W., Kneeland J.B., Johnson J.E. MR imaging of the lateral collateral ligament of the ankle. AJR Am J Roentgenol. 1991;156:131–136. doi: 10.2214/ajr.156.1.1898546. [DOI] [PubMed] [Google Scholar]
- 2.Garrick J.G. The frequency of injury, mechanism of injury and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241–242. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- 3.Jacobson J.A. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am. 1999;37:713–735. doi: 10.1016/s0033-8389(05)70125-1. [DOI] [PubMed] [Google Scholar]
- 4.Laurin C., Mathieu J. Sagittal mobility of the normal ankle. Clin Orthop Relat Res. 1975:99–104. doi: 10.1097/00003086-197505000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Braun H.J., Dragoo J.L., Hargreaves B.A., Levenston M.E., Gold G.E. Application of advanced magnetic resonance imaging techniques in evaluation of the lower extremity. Radiol Clin North Am. 2013;51:529–545. doi: 10.1016/j.rcl.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fong D.T., Hong Y., Chan L.K., Yung P.S., Chan K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Li H.Y., Hua Y.H., Wu Z.Y., Chen B., Chen S.Y. Strength of suture anchor versus transosseous tunnel in anatomic reconstruction of the ankle lateral ligaments: a biomechanical study. Arthroscopy. 2013;29:1817–1825. doi: 10.1016/j.arthro.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Wang J., Hua Y., Chen S., Li H., Zhang J., Li Y. Arthroscopic repair of lateral ankle ligament complex by suture anchor. Arthroscopy. 2014;30:766–773. doi: 10.1016/j.arthro.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 9.Watson A.D. Ankle instability and impingement. Foot Ankle Clin. 2007;12:177–195. doi: 10.1016/j.fcl.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 10.DIGiovanni B.F., Fraga C.J., Cohen B.E., Shereff M.J. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21:809–815. doi: 10.1177/107110070002101003. [DOI] [PubMed] [Google Scholar]
- 11.Rolf C.G., Barclay C., Riyami M., George J. The importance of early arthroscopy in athletes with painful cartilage lesions of the ankle: a prospective study of 61 consecutive cases. J Orthop Surg Res. 2006;1:4. doi: 10.1186/1749-799X-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar V., Triantafyllopoulos I., Panagopoulos A., Fitzgerald S., van Niekerk L. Deficiencies of MRI in the diagnosis of chronic symptomatic lateral ankle ligament injuries. Foot Ankle Surg. 2007;13:171–176. [Google Scholar]
- 13.Park H.J., Cha S.D., Kim S.S., Rho M.H., Kwag H.J., Park N.H. Accuracy of MRI findings in chronic lateral ankle ligament injury: comparison with surgical findings. Clin Radiol. 2012;67:313–318. doi: 10.1016/j.crad.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 14.Cass J.R., Morrey B.F. Ankle instability: current concepts, diagnosis and treatment. Mayo Clin Proc. 1984;59:165–170. doi: 10.1016/s0025-6196(12)60769-1. [DOI] [PubMed] [Google Scholar]
- 15.Tocci S.L., Madom I.A., Bradley M.P., Langer P.R., DiGiovanni C.W. The diagnostic value of MRI in foot and ankle surgery. Foot Ankle Int. 2007;28:166–168. doi: 10.3113/FAI.2007.0166. [DOI] [PubMed] [Google Scholar]
- 16.Joshy S., Abdulkadir U., Chaganti S., Sullivan B., Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010;16:78–80. doi: 10.1016/j.fas.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 17.Oae K., Takao M., Uchio Y., Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010;39:41–47. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 18.Siegler S., Block J., Schneck C.D. The mechanical characteristics of collateral ligaments of human ankle joint. Foot Ankle. 1988;8:234–242. doi: 10.1177/107110078800800502. [DOI] [PubMed] [Google Scholar]
- 19.Renström P.A., Konradsen L. Ankle ligament injuries. Br J Sports Med. 1997;31:11–20. doi: 10.1136/bjsm.31.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perrich K.D., Goodwin D.W., Hecht P.J., Cheung Y. Ankle ligaments on MRI: appearance of normal and injured ligaments. AJR Am J Roentgenol. 2009;193:687–695. doi: 10.2214/AJR.08.2286. [DOI] [PubMed] [Google Scholar]
- 21.Verhaven E.F., Shahabpour M., Handelberg F.W., Vaes P.H., Opdecam P.J. The accuracy of three-dimensional magnetic resonance imaging in the diagnosis of ruptures of the lateral ligaments of the ankle. Am J Sports Med. 1991;19:583–587. doi: 10.1177/036354659101900605. [DOI] [PubMed] [Google Scholar]
- 22.Pijnenburg A.C., Bogaard K., Krips R., Marti R.K., Bossuyt P.M., van Dijk C.N. Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomised, prospective trial. J Bone Joint Surg Br. 2003;85(4):525–530. doi: 10.1302/0301-620x.85b4.13928. [DOI] [PubMed] [Google Scholar]
- 23.Colville M.R. Surgical treatment of unstable ankle. J Am Acad Orthop Surg. 1998;6:368–377. doi: 10.5435/00124635-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral instability. J Athl Train. 2002;37:364–375. [PMC free article] [PubMed] [Google Scholar]
- 25.Konradsen L., Bech L., Ehrenbjerg M., Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12:129–135. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 26.Boonthathip M., Chen L., Trudell D., Resnick D. Lateral ankle ligaments: MR arthrography with anatomic correlation in cadavers. Clin Imaging. 2011;35:42–48. doi: 10.1016/j.clinimag.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 27.Golanó P., Vega J., de Leeuw P.A., Malagelada F., Manzanares M.C., Götzens V. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557–569. doi: 10.1007/s00167-010-1100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takao M., Innami K., Matsushita T., Uchio Y., Ochi M. Arthroscopic and magnetic resonance image appearance and reconstruction of the anterior talofibular ligament in cases of apparent functional ankle instability. Am J Sports Med. 2008;36:1542–1547. doi: 10.1177/0363546508315537. [DOI] [PubMed] [Google Scholar]
- 29.Kim Y.S., Kim Y.B., Kim T.G., Lee S.W., Park S.H., Lee H.J. Reliability and validity of magnetic resonance imaging for the evaluation of the anterior talofibular ligament in patients undergoing ankle arthroscopy. Arthroscopy. 2015;31:1540–1547. doi: 10.1016/j.arthro.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 30.Oloff L.M., Sullivan B.T., Heard G.S., Thornton M.C. Magnetic resonance imaging of traumatized ligaments of the ankle. J Am Podiatr Med Assoc. 1992;82:25–32. doi: 10.7547/87507315-82-1-25. [DOI] [PubMed] [Google Scholar]
- 31.Lesniak B.P., Loveland D., Jose J., Selley R., Jacobson J.A., Bedi A. Use of ultrasonography as a diagnostic and therapeutic tool in sports medicine. Arthroscopy. 2014;30:260–270. doi: 10.1016/j.arthro.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 32.Cheng Y., Cai Y., Wang Y. Value of ultrasonography for detecting chronic injury of lateral ligaments of ankle joint compared with ultrasonography findings. Br J Radiol. 2014;87:20130406. doi: 10.1259/bjr.20130406. [DOI] [PMC free article] [PubMed] [Google Scholar]