Abstract
Background
Extrusion of the meniscus has been reported to be correlated with progression of osteoarthritis. In cases with osteochondral lesions after extrusion of the meniscus, meniscal transplantation was the only surgical intervention. Recently, a novel procedure called arthroscopic centralisation has been developed to restore the meniscus function by centralising the midbody of the extruded meniscus onto the rim of the tibial plateau using suture anchors.
Case report
A combination of novel techniques—retrograde osteochondral autograft transplantation to retain hyaline articular cartilage and arthroscopic centralisation to restore residual meniscal function—was used to repair an osteochondral lesion of the lateral tibial plateau possibly caused by extrusion of the lateral meniscus. Good clinical and radiographic outcomes were achieved at the 2-year follow-up.
Conclusion
A combination of retrograde osteochondral autograft transplantation and arthroscopic centralisation can be a good option to treat the osteochondral lesion of the tibial plateau caused by extrusion of the meniscus.
Keywords: arthroscopic centralisation, extrusion, lateral meniscus, osteochondral transplantation, tibial plateau
Introduction
Extrusion of the meniscus suggests loss of hoop function and would exacerbate cartilage degeneration by losing load-distributing function in the meniscus. It has been reported that extrusion of the meniscus is associated with the development of osteoarthritis (OA)1, 2 and knee pain in patients with OA.3 In cases with OA or osteochondral lesion after the extrusion of the meniscus, meniscal transplantation was the only surgical intervention to restore functional meniscus. However, a novel procedure, arthroscopic centralisation, has been recently developed to restore and maintain the meniscus function by repairing/preventing extrusion of the meniscus by centralising the midbody of the meniscus onto the rim of the tibial plateau, and good clinical and radiographic outcomes of this procedure were reported.4, 5
Repair of osteochondral defects remains challenging, and several techniques have been used to repair them such as bone marrow stimulation, osteochondral transplantation, and autologous chondrocyte implantation (ACI). Among these, osteochondral autologous transplantation is currently considered a reliable surgical technique that provides and retains proper hyaline articular cartilage.6, 7 This technique is often used in the femoral condyle; the treatment of osteochondral lesions on the tibial plateau cannot be achieved with the usual antegrade transplantation technique. However, recent reports introduced a novel arthroscopic retrograde osteochondral transplantation on the lateral plateau.8, 9
This case report presents a patient with an osteochondral lesion of the lateral tibial plateau with extrusion of the lateral meniscus who was treated with retrograde osteochondral autograft transplantation and arthroscopic centralisation. This study was approved by our institutional review board, and written informed consent was obtained from the patient.
Case Report
A 40-year-old male car mechanic was referred to the outpatient orthopaedic clinic with chief complaints of right knee pain and locking. He had undergone arthroscopic removal of a free body on his right knee at another hospital 2 years ago, and he had no symptoms after the surgery. However, 1 week prior to presentation, his right knee suddenly locked when he lifted an automobile tire. On examination, the range of motion was −10° to 145° without swelling. He had a neutral alignment without ligamentous instability, tenderness in the lateral joint space, and positive McMurray test with pain on the lateral side. Knee X-ray and computed tomography (CT) revealed an osteochondral lesion with bone cysts and a free body on the lateral tibial plateau (Figure 1). The long leg standing X-ray confirmed a neutral lower limb alignment with the femorotibial angle of 175° and mechanical axis of 51%. Magnetic resonance imaging (MRI) showed the osteochondral lesion on the lateral tibial plateau (Outerbridge classification Grade 4). In terms of the meniscus, after assessing all coronal slices, meniscus extrusion was measured on the image showing maximum extrusion as the distance from the most peripheral aspect of the meniscus to the border of the tibia, excluding any osteophytes, in 1-mm increments. Extrusion of the lateral meniscus was 4 mm in the middle part, and a degenerative change in the anterior part was observed (Figure 2). Treatment options, including conservative treatment, removal of the free body, and definitive surgery, were discussed with the patient, and he elected to undergo removal of the free body, retrograde osteochondral autograft transplantation for the osteochondral lesion, and arthroscopic centralisation for the extruded lateral meniscus.
Figure 1.
(A) Preoperative X-ray, (B) coronal, and (C) sagittal views of preoperative computed tomography showed the osteochondral lesion with bone cysts and a free body on the lateral tibial plateau.
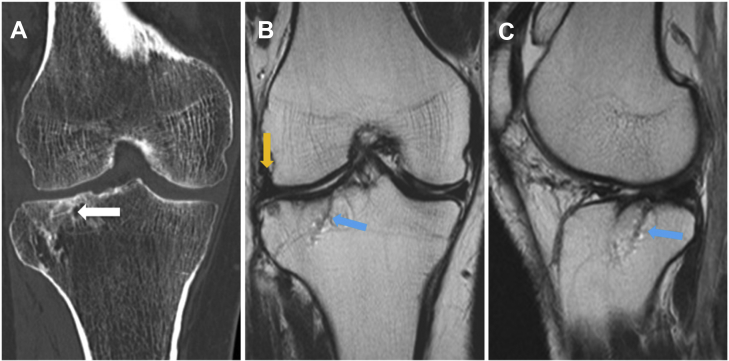
Figure 2.
(A) Coronal and (B) sagittal views of preoperative MRI showed the osteochondral lesion on the lateral tibial plateau (blue arrows) and 4-mm extrusion of the lateral meniscus with degenerative change in the anterior part (orange arrows). MRI = magnetic resonance imaging.
Surgical technique
A standard arthroscopic examination was performed via anteromedial and anterolateral portals. The osteochondral lesion, 10 mm × 10 mm in size, on the lateral tibial plateau was covered with fibrous tissues, and the free body was also included in the fibrous tissues (Figure 3A). Anterior to middle part of the lateral meniscus was degenerated and seemed to lose the hoop function (Figure 3B), and displacement of the lateral meniscus was confirmed by pushing the midbody of the meniscus out of the rim of the lateral tibial plateau using a probe (Figure 3C). Although a small chondral lesion was also found on the lateral femoral condyle, this lesion was left untreated as it was very small, International Cartilage Repair Society Grade 2 (<50% of cartilage depth) lesion, and was considered irrelevant to the patient's symptoms.
Figure 3.
Arthroscopic findings. (A)The osteochondral lesion, 10 mm × 10 mm in size, on the lateral tibial plateau was covered with fibrous tissues (arrow), and the free body was also included in the fibrous tissues. (B) The anterior to middle part of the lateral meniscus was degenerated and elongated. (C) Displacement of the lateral meniscus was confirmed by pushing the midbody of the meniscus out of the rim of the lateral tibial plateau using a probe.(D) The osteochondral plug, the chondral surface of which was oriented 45° obliquely, was inserted into the tibial tunnel in a retrograde fashion, and its cartilage surface was matched to the surrounding cartilage of the lateral tibial plateau (arrow). (E) The midbody of the lateral meniscus was sutured at the margin between the meniscus and the capsule to the lateral edge of the lateral tibial plateau using two JuggerKnot Soft Anchors (Biomet) (arrowheads). (F) Extruded meniscus was centralised after stabilisation of the midbody of the lateral meniscus. LFC = lateral femoral chondyle; LM = lateral meniscus.
A 3-cm long skin incision was made at the superomedial portion of the patellofemoral region. After an incision was made on the joint capsule, an osteochondral plug, 10 mm in diameter and 20 mm long, the chondral surface of which was oriented at 45° obliquely, was harvested from the most peripheral and proximal part of the medial patellar groove using the Osteochondral Autograft Transfer System (Arthrex, Naples, FL, USA). A 4-cm longitudinal skin incision was then made along the lateral border of the tibial tubercle. The fascia was incised, and the tibial anterior muscle was reflected laterally from the tibial cortex. With the arthroscope in the anteromedial portal, a tibial drill guide for anterior cruciate ligament (ACL) reconstruction was set at 45°, passed through the anterolateral portal, and positioned over the centre of the osteochondral lesion. A guide wire was inserted from the anterolateral surface of the tibia and over-reamed using a Coring Reamer with a diameter of 10 mm (Arthrex). The osteochondral plug was inserted into the tibial tunnel in a retrograde fashion, and its cartilage surface was matched to the surrounding cartilage of the lateral tibial plateau (Figure 3D). The remaining bony defect in the tibial tunnel was filled with the bony cylinder obtained by the Coring Reamer.
A midlateral portal was made with an arthroscopic view from the anterolateral portal, just proximal to the lateral meniscus and 1 cm anterior to the popliteal hiatus. The rim of the lateral tibial plateau, just anterior to the popliteal hiatus, was abraded by a motorised shaver to remove cartilage. The JuggerKnot Soft Anchor, loaded with a Maxbraid (Biomet, Warsaw, IN, USA), was inserted on the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus. A Micro Suture Lasso Small Curve with Nitinol Wire Loop (Arthrex) was then inserted through the midlateral portal. The tip of the Micro Suture Lasso penetrated the meniscus from superior to inferior at the margin between the meniscus and the capsule, and the Maxbraid was passed from inferior to superior using a suture relay technique. The same procedure was repeated for another strand of Maxbraid to create a mattress suture configuration. Another JuggerKnot Soft Anchor was inserted on the lateral edge of the lateral tibial plateau, 1 cm anterior to the first anchor, and the same procedure was repeated. The passed sutures were then tied through the midlateral portal using a self-locking sliding knot (Figure 3E). The extruded meniscus was centralised after stabilisation of the midbody of the lateral meniscus (Figure 3F).
Postoperative treatment
The patient was nonweight-bearing on his right lower extremity for 2 weeks. The range of motion exercise from full extension to 120° of flexion was started at 2 days after the surgery. Partial weight-bearing was initiated after 2 weeks and was gradually increased as tolerated thereafter. Crutches were removed at 6 weeks. Deep squatting was prohibited for 2 months. Full range of motion was obtained at 3 months. After 3 months, the patient was allowed to resume his work as a car mechanic.
Clinical follow-up
CT taken 3 months after the surgery showed a good adaptation and union of the graft (Figure 4A). MRI taken 3 months after the surgery showed congruent chondral resurfacing of the lateral tibial plateau, although the bone plug showed low signal intensity in T2 images. Extrusion of the lateral meniscus was reduced to 1 mm (Figures 4B and 4C). The patient was followed for 2 years, and CT taken 2 years after the surgery showed complete union of the graft and remodelling of the subchondral bone to be congruent (Figure 5A). MRI taken 2 years after the surgery showed healing of the implanted plug (same intensity as surrounding bone) as well as same cartilage intensity as normal cartilage (Outerbridge classification Grade 0), and the position of the lateral meniscus was maintained (Figures 5B and 5C). At his 2-year follow-up, the patient reported no swelling or mechanical symptoms. He had a full range of knee motion, no lateral joint pain, and negative McMurray test. He was able to work as a car mechanic 8 h/d.
Figure 4.
Postoperative findings at 3 months after surgery. (A) Computed tomography showed good adaptation and union of the graft (white arrow). (B) Coronal and (C) sagittal views of magnetic resonance imaging showed congruent chondral resurfacing of the lateral tibial plateau although the bone plug and low signal intensity in T2 images (blue arrows). The midbody of the lateral meniscus (orange arrow) was well positioned without extrusion.
Figure 5.
Postoperative findings at 2 years after surgery. (A) Computed tomography showed complete union of the graft and remodelling of the subchondral bone to be congruent (white arrow). (B) Coronal and (C) sagittal views of magnetic resonance imaging showed healing of the implanted plug (same intensity as surrounding bone, blue arrows), and position of the lateral meniscus was maintained (orange arrow).
Discussion
This case report describes a combination of novel surgical techniques, arthroscopic retrograde osteochondral autograft transplantation, and arthroscopic centralisation, which were used to treat an osteochondral lesion of the lateral tibial plateau with extrusion of the lateral meniscus.
Several techniques have been reported to repair osteochondral defects, such as bone marrow stimulation,10, 11 ACI,12 and osteochondral transplantation. Bone marrow stimulation usually results in the formation of unstructured fibrous tissue which lacks the biomechanical and viscoelastic features of hyaline cartilage, and the results are often followed by degeneration in the repaired tissue.13 In terms of ACI, although clinical results of this technique are promising, there are some concerns; the newly regenerated cartilage often consists of fibrous tissues,14, 15, 16 possibly due to a limited number of chondrocytes and their low proliferation potential. Bony overgrowth, which causes thinning of the regenerated cartilage and violation of the tidemark, is also of concern.16
Compared with the aforementioned methods, the osteochondral autologous transplantation is to date the most established surgical technique to provide an osteochondral unit with hyaline cartilage. Cylindrical osteochondral grafts are harvested from the nonweight-bearing area of the proximal femoral condyle and are implanted into the defect. The osteochondral autologous transplantation is currently considered a reliable surgical technique that provides and retains proper hyaline articular cartilage.7
The osteochondral autologous transplantation is often used in the femoral condyle; the treatment of the osteochondral lesion on the tibial plateau cannot be achieved with a usual antegrade transplantation technique. However, recent reports showed a novel arthroscopic retrograde osteochondral transplantation on the tibial plateau.8, 9 In this technique, a guide wire was introduced and drilled using a tibial guide for ACL reconstruction, and a cannulated reamer or a core reamer was advanced to the centre of the defect through the tibia. An osteochondral cylinder was harvested from the nonweight-bearing area of the femoral trochlea at an angle that corresponded to the angle on the ACL guide, and the autograft was inserted to the bony hole in a retrograde fashion. Short-term results of these reports were good; the same technique was adopted in the current case.
In this case, the lateral meniscus was also extruded with anterior and middle parts degenerated and elongated. Extrusion of the meniscus was reported to have strong correlation with progression of OA.1, 2 Recently, a novel procedure called arthroscopic centralisation was developed for an extruded meniscus using suture anchors in which the meniscus was centralised at the edge of the tibial plateau.4, 5 With this procedure, the extrusion was improved on MRI, and clinical results were also improved at 2-year follow-up. In the current case, the osteochondral lesion of the lateral tibial plateau was considered to be caused by extrusion of the lateral meniscus as the patient had neither past history of knee trauma, ligamentous instability, nor previous surgeries such as ACL reconstruction and meniscectomy. If the retrograde osteochondral autograft transplantation alone was performed, the patient would suffer from recurrence of the osteochondral lesion without restoring meniscal function. However, simultaneous varus knee osteotomy was not an option in this case as the patient's lower limb alignment was neutral. Therefore, simultaneous arthroscopic centralisation of the extruded lateral meniscus was performed; thereby satisfactory 2-year results were achieved.
This report has some limitations. Since this is a report of a single case, conclusions cannot be generalised regarding the efficacy of this technique without further clinical comparative studies. In addition, the patient was followed-up only for 2 years; follow-up for a longer period of time is required to confirm the effectiveness of this technique.
In conclusion, a combination of novel techniques—the retrograde osteochondral autograft transplantation to retain proper hyaline articular cartilage and arthroscopic centralisation to restore residual meniscal function—was used to repair an osteochondral lesion of the lateral tibial plateau possibly caused by extrusion of the lateral meniscus. Good clinical and radiographic outcomes were achieved at the 2-year follow-up.
Conflicts of interest
The authors have no conflicts of interest relevant to this article. No financial or material support of any kind was received for the work described in this article.
References
- 1.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee D.H., Lee B.S., Kim J.M. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19:222–229. doi: 10.1007/s00167-010-1274-2. [DOI] [PubMed] [Google Scholar]
- 3.Wenger A., Englund M., Wirth W., Hudelmaier M., Kwoh K., Eckstein F. Relationship of 3D meniscal morphology and position with knee pain in subjects with knee osteoarthritis: a pilot study. Eur Radiol. 2012;22:211–220. doi: 10.1007/s00330-011-2234-z. [DOI] [PubMed] [Google Scholar]
- 4.Koga H., Muneta T., Yagishita K. Arthroscopic centralization of an extruded lateral meniscus. Arthrosc Tech. 2012;1:e209–e212. doi: 10.1016/j.eats.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koga H., Muneta T., Watanabe T. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32:2000–2008. doi: 10.1016/j.arthro.2016.01.052. [DOI] [PubMed] [Google Scholar]
- 6.Harris J.D., Siston R.A., Pan X., Flanigan D.C. Autologous chondrocyte implantation: a systematic review. J Bone Joint Surg Am. 2010;92:2220–2233. doi: 10.2106/JBJS.J.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch T.S., Patel R.M., Benedick A., Amin N.H., Jones M.H., Miniaci A. Systematic review of autogenous osteochondral transplant outcomes. Arthroscopy. 2015;31:746–754. [Google Scholar]
- 8.Ueblacker P., Burkart A., Imhoff A.B. Retrograde cartilage transplantation on the proximal and distal tibia. Arthroscopy. 2004;20:73–78. doi: 10.1016/j.arthro.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Matsusue Y., Kotake T., Nakagawa Y., Nakamura T. Arthroscopic osteochondral autograft transplantation for chondral lesion of the tibial plateau of the knee. Arthroscopy. 2001;17:653–659. doi: 10.1053/jars.2001.22400. [DOI] [PubMed] [Google Scholar]
- 10.Cerynik D.L., Lewullis G.E., Joves B.C., Palmer M.P., Tom J.A. Outcomes of microfracture in professional basketball players. Knee Surg Sports Traumatol Arthrosc. 2009;17:1135–1139. doi: 10.1007/s00167-009-0765-5. [DOI] [PubMed] [Google Scholar]
- 11.Lotz M. Cytokines in cartilage injury and repair. Clin Orthop Relat Res. 2001:S108–S115. doi: 10.1097/00003086-200110001-00011. [DOI] [PubMed] [Google Scholar]
- 12.Brittberg M., Lindahl A., Nilsson A., Ohlsson C., Isaksson O., Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331:889–895. doi: 10.1056/NEJM199410063311401. [DOI] [PubMed] [Google Scholar]
- 13.Steadman J.R., Briggs K.K., Rodrigo J.J., Kocher M.S., Gill T.J., Rodkey W.G. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;19:477–484. doi: 10.1053/jars.2003.50112. [DOI] [PubMed] [Google Scholar]
- 14.Horas U., Pelinkovic D., Herr G., Aigner T., Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Joint Surg Am. 2003;85-A:185–192. doi: 10.2106/00004623-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Tins B.J., McCall I.W., Takahashi T. Autologous chondrocyte implantation in knee joint: MR imaging and histologic features at 1-year follow-up. Radiology. 2005;234:501–508. doi: 10.1148/radiol.2342031970. [DOI] [PubMed] [Google Scholar]
- 16.Adachi N., Sato K., Usas A. Muscle derived, cell based ex vivo gene therapy for treatment of full thickness articular cartilage defects. J Rheumatol. 2002;29:1920–1930. [PubMed] [Google Scholar]