Abstract
Background/objective
Anterior cruciate ligament (ACL) reconstructions often fail without graft rupture. The purpose of this study was to compare the characteristics of patients with elongated and ruptured bone-patellar tendon-bone (BTB) grafts that required revision surgery.
Methods
Twenty one patients who required revisions of a BTB-reconstructed ACL between 2010 and 2015 were enrolled in this study. All patients were evaluated for bone tunnel position using computed tomography. Tunnel angle was calculated with radiographs. Stability under anaesthesia, and meniscus and cartilage condition were evaluated during the revision surgery. Age at primary surgery, time between primary and revision surgery, activity level, original tunnel position of the graft, and meniscus and cartilage condition were compared between elongated and ruptured grafts.
Results
Age at primary surgery was not significantly different between the two groups (p = 0.528). Time between primary and revision surgery as well as activity level were also not significantly different between the two groups (p = 0.010 and p = 0.307, respectively). Femoral bone tunnel position was more proximal (p = 0.003), and radiographic tunnel angle was not significantly different between the two groups (p = 0.029). The rupture group was significantly more unstable on the pivot shift (p < 0.003). Meniscus degeneration, meniscus tear, and cartilage damage were not significantly different between the two groups (p = 0.030, p = 0.311, and p = 0.505, respectively).
Conclusion
The location of the original femoral tunnel was more proximal in patients with elongated grafts than in those with ruptured grafts. Different bone tunnel position from native ACL might lead to graft elongation.
Keywords: failure pattern, graft elongation, revision anterior cruciate ligament, tunnel position
Introduction
Anterior cruciate ligament (ACL) reconstruction is a generally successful procedure, with reported ipsilateral failure rates of 7%.1 A combination of factors typically contribute to a poor ACL reconstruction outcome. One of the most important of these is a technical error involving the malpositioning of the graft tunnel.2, 3 A malpositioned tunnel may contribute to knee instability, tunnel widening, and poor graft maturation.3, 4, 5 The traditionally used isometric tunnel position and anterior femoral tunnel placement are now considered to be malpositioned tunnels, which are associated with inferior stability and consequently worse clinical outcomes than anatomical tunnel position.6, 7
Primary ACL ruptures occur most frequently at the proximal attachment site.8 However, the failure pattern for ACL grafts is different. In an analysis of ACL reconstruction revisions, van Eck et al9, 10 reported that single- and double-bundle reconstructions had different failure patterns. The most common failure pattern after single-bundle reconstructions was elongation without rupture, whereas midsubstance ruptures were frequently observed after double-bundle reconstructions. Based on these reports, surgical method and selected graft type may influence the ACL reconstruction failure pattern because of differences in graft stability, impingement, and maturation. Along with their results, we sometimes experienced undisrupted elongated primary ACL grafts during revision surgeries, while the native ACL is often disrupted during a primary ACL reconstruction surgery. This suggests that reconstructed ACLs do not completely restore the function of the native ligament. The purpose of this study was to compare the tunnel position, survival time, aetiology, activity level, knee stability, and condition of the meniscus and articular cartilage of patients with elongated versus ruptured grafts after ACL reconstruction. We hypothesised that an elongated ACL graft without a rupture would have a malpositioned graft tunnel.
Methods
Study population
A total of 65 patients with knee instability after ACL reconstruction underwent revision surgeries between January 2010 and March 2015 at our institution. Only those patients who underwent primary ACL reconstruction with bone-patellar tendon-bone (BTB) grafts (27 patients) were enrolled in this study. A total of 22 patients underwent computed tomography (CT) of the knee to assess the primary surgery bone tunnel position. Written informed consent was obtained prior to study enrolment. Patients with multiple (≥ 2) revision surgeries on the knee of interest were not included in this series. One patient with bone fracture that extended to the femoral attachment site with an intact ACL was excluded from this study. This protocol was approved by the Ethics Committee of Hirosaki University Graduate School of Medicine.
Body mass index (BMI), Tegner activity level score before surgery or after injury in trauma cases, the existence and circumstances of the ACL re-injury (i.e., during sports activity), and the period between primary and revision surgery were recorded for each patient.
Evaluation of the tunnel position
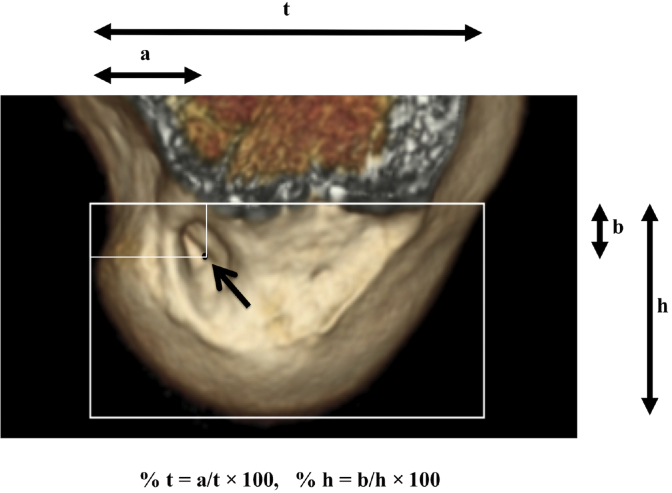
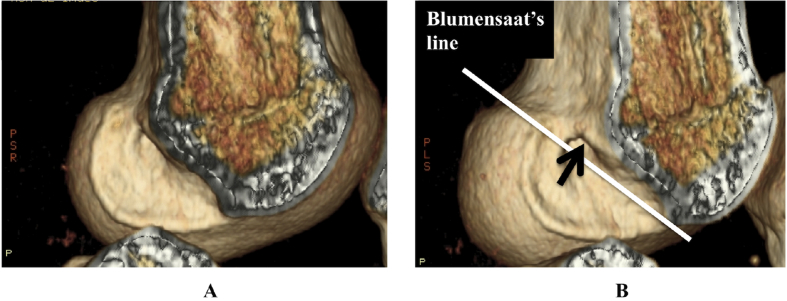
Tunnel position was measured on a three-dimensional CT (3D CT) of the knee obtained before the revision surgery by two different observers, with the average of these measurements considered the final value. Quadrant methods11 were used to classify the centre of the femoral bone tunnel. Sagittal views of the medial wall of the lateral femoral condyle were overlaid with a digital grid rotationally aligned to Blumensaat's line. The anterior, posterior, and distal edges of the grid were aligned to the respective cortices of the femoral condyles. Distance “t” is defined as the total sagittal diameter of the lateral femoral condyle measured along Blumensaat's line, and distance “h” is defined as the maximum intercondylar notch height. To decide the centre of the femoral tunnel, an ellipsis was fitted over the bone tunnel using ImageJ (National Institutes of Health, Bethesda, MD, USA). The centre of the femoral tunnel was defined as the intersection of the minor and long axis. This point was recorded as a percentage of the t (% t) and h (% h), measured from the posterior edge of the femoral condyle and Blumensaat's line, respectively, using ImageJ (Figure 1). When the centre of the femoral bone tunnel was above Blumensaat's line, indicating that the tunnel opened on the intercondylar roof, the % h was automatically assigned the value of 0 (Figure 2). The anatomical nomenclature refers to the knee in an extended position, and the ACL femoral footprint is described using anterior/posterior and proximal/distal positions. On the other hand, the arthroscopic nomenclature refers to the knee in a flexion position, and the ACL femoral footprint is described using shallow/deep and high/low positions. In this study, we used the term “proximal” when % h was small and the term “distal” when the % h was large.
Figure 1.
Femoral bone tunnel position on 3D CT. A sagittal view of the medial edge of the external condyle as viewed from medial side was overlaid with a digital grid rotationally aligned to Blumensaat's line. Distance “t” is defined as the total sagittal diameter of the lateral femoral condyle measured along Blumensaat's line, and distance “h” is defined as the maximum intercondylar notch height. The centre of the femoral tunnel was recorded as a percentage of the t (% t = a/t × 100) and h (% h = b/t × 100), measured from the posterior edge of the femoral condyle and Blumensaat's line, respectively.
Figure 2.
High-noon femoral bone tunnel. (A) When the centre of the femoral bone tunnel (arrow) was above Blumensaat's line (white line), indicating that the tunnel opened on the intercondylar roof, the % h was recorded as 0. (B) Femoral bone tunnel is visible when looking up at the intercondylar roof from the bottom.
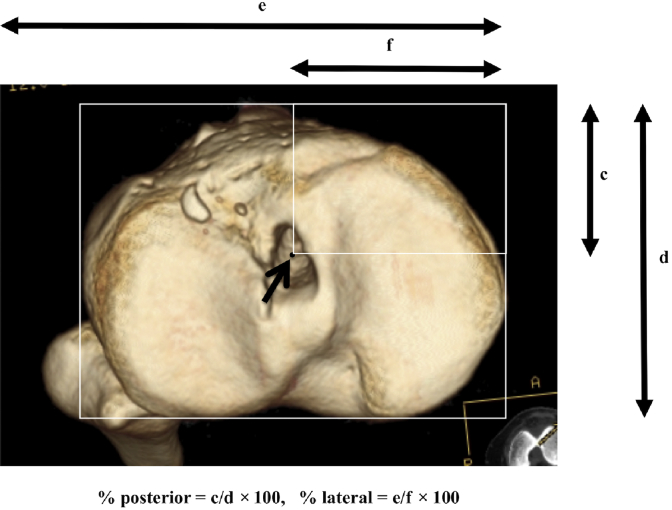
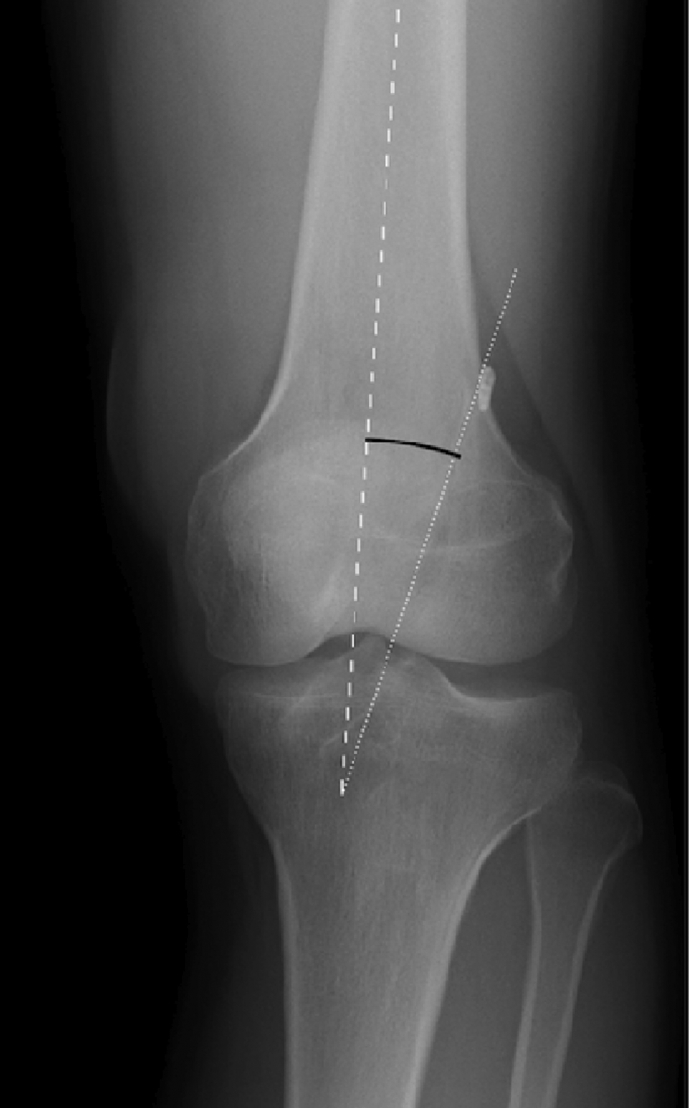
On the tibial side, the central points were determined by Parkinson's methods,12 which are similar to previously described analysis methods.13 The true proximal-to-distal view on the tibia14 was overlaid with the digital grid rotationally aligned to the most posterior cortical margins of the lateral and medial tibial condyles. The anterior, medial, and lateral edges of the grid were aligned to their respective tibial cortices. The centre of the tibial bone tunnel was also decided with fitted ellipsis. The point was recorded as a percentage of the anterior-posterior (% posterior) and medial-lateral (% lateral) dimensions of the grid, which were measured from the anterior and medial edges, respectively (Figure 3). The radiographic angle between the femoral and longitudinal axes of the femoral bone tunnel on a weight-bearing anteroposterior X-ray of the knee was assessed using ImageJ (Figure 4).
Figure 3.
Tibial bone tunnel position on 3D CT. The 3D model of the knee was viewed from the medial aspect with both femoral condyles superimposed, akin to a true lateral image. The proximal tibia was viewed directly from above. The digital grid was overlaid and rotationally aligned to the most posterior cortical margin of the lateral and medial tibial condyles. The anterior, medial, and lateral edges of the grid were aligned to their respective tibial cortices. The centre of the tibial bone tunnel (arrow) was recorded as a percentage of the anterior-posterior (% posterior = c/d × 100) and medial-lateral (% lateral = e/f × 100) dimensions of the grid as measured from the anterior and medial edges, respectively.
Figure 4.
Radiographic angle between the femoral axis and femoral bone tunnel on bilateral weight-bearing anteroposterior X-rays.
Evaluation of stability
The anterior drawer, Lachman test, and pivot shift test were performed under anaesthesia by an experienced knee surgeon on each patient prior to revision surgery.
Failure patterns of the ACL grafts
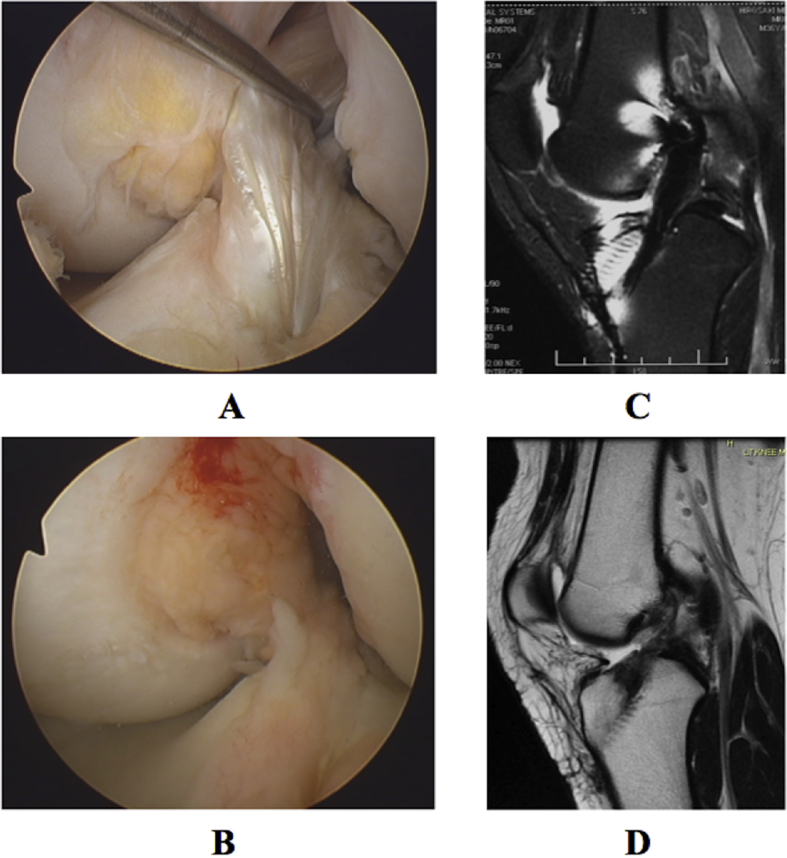
The failed graft was first assessed with a probe to identify and describe the continuity of any remnants. Failure patterns were classified as either “elongation” (Figure 5A), “rupture” (Figure 5B), or “other”. Cases of a failed ACL reconstruction where the graft remnant was pathologically reattached to a place other than the bone tunnel, such as to the posterior cruciate ligament, were classified as ruptures. Cases of partial rupture were classified as ruptures. Cases in which the graft remnant was smooth without a stump but the volume of the midsubstance was small were classified as elongation. CT and magnetic resonance imaging data (Figures 5C and 5D) were reviewed when classification was difficult.
Figure 5.
Arthroscopic view and magnetic resonance imaging (MRI). (A) Arthroscopic view of the elongation group; (B) arthroscopic view of the rupture group; (C) MRI of the elongation group; and (D) MRI of the rupture group.
Meniscus and cartilage damage
Meniscal tears, meniscal degeneration, and articular cartilage damage at the time of revision were identified by the operating surgeon using arthroscopic images and a probe. Menisci with horizontal or flap tears,15 or that displayed wear with brush-like damage at the margins were defined as degenerative. Cartilage was scored from grade 1 to 3 according to Noyes' grading system16: grade 1, an intact cartilage surface; grade 2, a damaged cartilage surface with cracks, surface blisters, fissures, fibrillations, and fragmentations; and grade 3, exposed bone.
Statistical analysis
Prism 6.0b (GraphPad Software, La Jolla, CA, USA) was used for statistical analysis of the elongation and rupture groups. Welch's t test was used to compare age at primary surgery, BMI, time between primary and revision surgeries, tunnel positions on 3D CT, and radiographic femoral tunnel angle between the elongation and rupture group. Nonparametric Tegner activity level was evaluated using the Mann–Whitney U test. Fisher's exact test was used to compare sex, re-injury rate and circumstance, Lachman test grade, and condition of the meniscus and cartilage. Chi-square tests were used for the anterior drawer and pivot shift tests because they had three categories. We performed multiple statistical analyses (5 confounding factors: existence of trauma, period between primary and revision surgeries, primary graft tunnel position, stability and cartilage and meniscus damage) between the two groups. To reduce type 1 error, Bonferroni correction was adopted, and p values < 0.01 (0.05/5) were considered significant. Then, a post hoc power calculation was conducted for bone tunnel positions based on the mean values and standard deviation using G*Power (version 3.1.9.2, Faul and Erfdelder 2009). Power of this analysis with 21 patients was 1.000 for femoral % low, 0.998 for femoral % t, 0.773 for % posterior, and 0.483 for tibial % lateral to detect the 5% significance levels in this present study.
Results
Demographic data
Based on intraoperative ACL graft evaluation, 10 grafts were ruptured and 11 were elongated. No case was classified as the other group.
In the rupture group, there were five male and five female patients. Average age at primary surgery was 17.8 ± 1.6 (range, 12–30) years, and age at revision surgery was 22.6 ± 2.9 (range 16–45) years. BMI was 25.4 ± 1.1, and Tegner activity level before revision surgery was 6.2 ± 0.7. Seven patients sustained a sports-related trauma that appeared to lead to instability. The average time between the primary and revision surgeries was 56.8 ± 19.3 months.
In the elongation group, there were seven male and four female patients. Average age at primary surgery was 19.3 ± 1.0 years, and age at revision surgery was 30.8 ± 1.6 (range, 21–37) years. BMI was 24.7 ± 0.7, and Tegner activity level before revision surgery was 5.3 ± 0.6. Six patients sustained traumatic episodes that appeared to lead to their instability. Three patients had sports-related traumas. The average time between the primary and revision surgeries was 138.1 ± 21.1 months.
Age at primary surgery was not significantly different (p = 0.436) between the rupture and elongation groups. Age at revision surgery of the rupture group was not significantly different between the two groups (p = 0.021). Sex (p = 0.528), BMI (p = 0.587), and Tegner activity level (p = 0.307) were not significantly different. Traumatic injuries were also not significant (p = 0.362). Sports-related injuries occurred more frequently in the rupture group, but there was no significant difference between the two groups (p = 0.030). The average time between surgeries was not significantly different (p = 0.010; Table 1).
Table 1.
Demographic data.
| Rupture group | Elongation group | p | |
|---|---|---|---|
| No. of patients | 10 | 11 | |
| Sex (male:female) | 5:5 | 7:4 | 0.528 |
| Age at primary surgery (years old) | 17.8 ± 1.6 | 19.3 ± 1.0 | 0.436 |
| Age at revision surgery (years old) | 22.6 ± 2.9 | 30.8 ± 1.6 | 0.021 |
| Body mass index (kg/m2) | 25.4 ± 1.1 | 24.7 ± 0.7 | 0.587 |
| Tegner activity level scale | 6.2 ± 0.7 | 5.3 ± 0.6 | 0.307 |
| No. of patients with trauma | 8 | 6 | 0.362 |
| No. of sports-related injuries | 8 | 3 | 0.030 |
| Period between surgeries (months) | 56.8 ± 19.3 | 138.1 ± 21.1 | 0.010 |
* p < 0.01.
Data are presented as mean ± SD.
Evaluation of the tunnel position
With respect to femoral tunnel position, % t was 31.4 ± 3.9% in the rupture group and 37.7 ± 3.4% in the elongation group. There was no significant difference between these groups (p = 0.227). % t in the rupture group was 21.1± 5.5% compared with 2.4 ± 1.4% in the elongation group. Three patients of the rupture group and seven patients of the elongation group had femoral tunnels in the high-noon position. For those high-noon positions, % h was defined as 0. The rupture group had significantly more proximal femoral bone tunnels (p = 0.003).
With respect to tibial tunnel position, % posterior was 45.0 ± 2.0% in the rupture group and 40.6 ± 2.3% in the elongation group. There was no significant difference between these groups (p = 0.165). The rupture group was 44.4 ± 1.4% lateral compared with 46.2 ± 1.3% in the elongation group (p = 0.373).
Femoral tunnel angle was 18.1 ± 3.0% in the rupture group and 8.9 ± 2.5% in the elongation group. There was no significant difference between the two groups (p = 0.029) (Table 2).
Table 2.
Tunnel position of the original graft.
| Rupture group | Elongation group | p | |
|---|---|---|---|
| Femoral % t (%) | 31.4 ± 3.9 | 37.7 ± 3.4 | 0.227 |
| Femoral % h (%) | 21.1 ± 5.5 | 2.4 ± 1.4 | 0.003* |
| Tibial % posterior (%) | 45.0 ± 2.0 | 40.6 ± 2.3 | 0.165 |
| Tibial % lateral (%) | 44.4 ± 1.4 | 46.2 ± 1.3 | 0.373 |
| Radiological femoral tunnel angle (°) | 18.1 ± 3.0 | 8.9 ± 2.5 | 0.029 |
* p < 0.01.
Stability evaluation
On anterior drawer testing, two patients were grade II and eight were grade III in the rupture group, whereas one patient was grade I, seven were grade II, and three were grade III in the elongation group. The anterior drawer test in the elongation group was not significantly different between the two groups (p = 0.049; Table 3). In the Lachman test, one patient was grade II and nine were grade III in the rupture group, whereas six patients were grade II and five were grade III in the elongation group. The Lachman test was not significantly different between the two groups (p = 0.031; Table 3).
Table 3.
Clinical result at revision surgery.
| Rupture group (n = 10) | Elongation group (n = 11) | p | |
|---|---|---|---|
| ADT (I:II:III) | 0:2:8 | 1:7:3 | 0.049 |
| Lachman test (I:II:III) | 0:1:9 | 0:6:5 | 0.031 |
| Pivot shift test (I:II:III) | 1:1:8 | 1:9:1 | 0.003* |
| Meniscus degeneration | 3 | 9 | 0.030 |
| Meniscus tear | 9 | 7 | 0.311 |
| Cartilage damage (I:II:III) | 6:4:0 | 5:6:0 | 0.553 |
ADT = anterior drawer test.
* p < 0.05.
In the pivot shift test, one patient was grade I, one was grade II, and eight were grade III in the rupture group, whereas one patient was grade I, nine were grade II, and one was grade III in the elongation group. There was a significant difference between the two groups (p = 0.003; Table 3).
Meniscus and cartilage damage
Degenerative menisci were observed in 3 out of 10 patients of the rupture group and 9 out of 11 patients in the elongation group (p = 0.030). Meniscal tears were observed in 9 out of 10 patients in the rupture group and 7 out of 11 patients in the elongation group (p = 0.311). There was no exposed cartilage in any patient. Six out of the 10 patients in the rupture group and 5 out of 11 patients in the elongation group had intact cartilage, which was not significant (p = 0.505; Table 3).
Discussion
Here we identified differences in the characteristics of patients with elongated and ruptured ACL grafts prior to revision. In this study, elongated grafts were observed in 11 out of 21 patients. van Eck et al9 reported that the most common graft failure pattern after single-bundle ACL reconstruction was graft elongation (58%).
We evaluated femoral and tibial tunnel position using 3D CT. The femoral tunnel position of the elongated group was significantly more proximal than that of the rupture group. The tibial tunnel position was not significantly different between the two groups. The elongation group had more “high-noon” femoral tunnels.17 High-noon tunnels produce a more vertical ACL than anatomically placed tunnels. Our radiographic data showed a tendency of vertical tunnel angle in the elongation group by virtue of it having more “high-noon” tunnel positions, although there was no significant difference. In a previous clinical study, more vertical femoral tunnels and lower Lysholm scores were observed in a group of residual pivot shift patients,18 while a laterally placed femoral tunnel was found to resist rotational loads more effectively.19, 20, 21 A vertical femoral tunnel may not prevent rotational instability, putting the reconstructed ACL under microstresses that may lead to elongation over time. On the other hand, tunnel positions of the rupture group were in a more anatomical position than those of the elongation group, which might cause similar failure pattern to native ACL rupture.
While age at primary surgery was not significantly different between the groups, the time between primary and revision surgery was tended to be long in the elongated group. Elongated graft failure may be a consequence of gradual graft degeneration, while rupture shortly after primary surgery may be the result of excessive external force.
In this study, no statistically significant difference was observed in Tegner activity score and traumatic origin between the rupture and elongation groups. However, sports-related injuries were more frequent in the rupture group, although this was not significantly different. This may suggest that patients had recovered enough to return to their previous level of sport activity, which exposed them to the same risk factors that contributed to the original rupture.
Stability was significantly persistent in the elongation group compared with the rupture group, as measured by pivot shift test. However, this residual stability was still insufficient for high-activity patients, and all patients required revision surgery.
While meniscal tears and overall cartilage condition was similar between the groups, meniscus degeneration was more observed in the elongation group, although there was no significant difference. The extended time between primary and revision surgery may have contributed to accelerated meniscal degeneration. However, a high-noon femoral tunnel position may also contribute to meniscal degeneration secondary to increased instability compared with an anatomic graft position.
Overall, an elongated graft meant an unruptured unstable knee. Vertically reconstructed ACL did not mimic the native ACL so that failure pattern was different from native ACL. Those unstable reconstructed ACLs might survive longer because they did not receive enough tension to rupture. However, surgeons should reconstruct the ACL anatomically in order to make a more stable knee. Moreover, adequate graft tension, biological augmentation, and effective rehabilitation programs for preventing reconstructed ACL failure are necessary.
Our study had several limitations. First, our sample size was small. ACL reconstruction is usually performed with either BTB or semitendinosus tendon grafts. Semitendinosus grafts are often used for double-bundle reconstructions where evaluating a two-graft tunnel is complicated and tendon-to-bone healing is slower than bone-to-bone healing.22 To reduce confounding, we only enrolled the patients who had undergone primary ACL reconstruction with BTB grafts in this study. Second, because surgeons were not blinded to CT information, their evaluation on the cartilages and the menisci might have been influenced by the information of tunnel locations. However, we believe that this method is more accurate than video analysis by a third person as only the surgeon can actually assess soft tissue condition at the time of surgery.
The time gap between trauma and revision surgery was different because of social factors (e.g., school, game schedule, willingness to undergo surgery) that influenced the timing of the revision. Finally, the target tunnel position has recently changed from an isometric to an anatomic point. Not enough time has elapsed to permit a long-term study of anatomically positioned ACL reconstructions, which may limit the number of elongations observed compared with previous isometric placement techniques. Elongation of anatomically placed ACL grafts may be observed when long-term data become available. Further work is necessary to confirm this hypothesis.
Conclusions
Femoral tunnel position was more proximal in the elongation group at revision surgery. Current study suggests that reconstructed ACL with malposition is least effective for knee stability and that leads to different failure pattern from native ACL.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
We are deeply grateful to Dr Eiji Sasaki and Daisuke Chiba for their statistical advice. We would also like to express our gratitude to Dr Norihiro Sasaki and Keiichiro Maniwa for their helpful discussions about this paper. Finally, special thanks to Dr Hironori Otsuka, who taught K.I. many ACL surgery techniques.
References
- 1.Wiggins A.J., Grandhi R.K., Schneider D.K., Stanfield D., Webster K.E., Myer G.D. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akhtar M.A., Bhattacharya R., Ohly N., Keating J.F. Revision ACL reconstruction – causes of failure and graft choices. Br J Sports Med. 2011;45:A15–16. [Google Scholar]
- 3.Morgan J.A., Dahm D., Levy B., Stuart M.J. MARS Study Group Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012;25:361–368. doi: 10.1055/s-0031-1299662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ménétrey J., Duthon V.B., Laumonier T., Fritschy D. “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc. 2008;16:224–231. doi: 10.1007/s00167-007-0474-x. [DOI] [PubMed] [Google Scholar]
- 5.Musahl V., Plakseychuk A., Van Scyoc A. Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med. 2005;33:712–718. doi: 10.1177/0363546504271747. [DOI] [PubMed] [Google Scholar]
- 6.Zantop T., Diermann N., Schumacher T., Schanz S., Fu F.H., Petersen W. Anatomical and nonanatomical double-bundle anterior cruciate ligament reconstruction: importance of femoral tunnel location on knee kinematics. Am J Sports Med. 2008;36:678–685. doi: 10.1177/0363546508314414. [DOI] [PubMed] [Google Scholar]
- 7.Illingworth K.D., Hensler D., Working Z.M., Macalena J.A., Tashman S., Fu F.H. A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am J Sports Med. 2011;39:2611–2618. doi: 10.1177/0363546511420128. [DOI] [PubMed] [Google Scholar]
- 8.DeHaven K.E. Diagnosis of acute knee injuries with hemarthrosis. Am J Sports Med. 1980;8:9–14. doi: 10.1177/036354658000800102. [DOI] [PubMed] [Google Scholar]
- 9.van Eck C.F., Kropf E.J., Romanowski J.R. Factors that influence the intra-articular rupture pattern of the ACL graft following single-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1243–1248. doi: 10.1007/s00167-011-1427-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Eck C.F., Kropf E.J., Romanowski J.R. ACL graft re-rupture after double-bundle reconstruction: factors that influence the intra-articular pattern of injury. Knee Surg Sports Traumatol Arthrosc. 2011;19:340–346. doi: 10.1007/s00167-010-1297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernard M., Hertel P., Hornung H., Cierpinski Th. Femoral insertion of the ACL: radiographic quadrant method. Am J Knee Surg. 1997;10:14–21. [PubMed] [Google Scholar]
- 12.Parkinson B., Gogna R., Robb C., Thompson P., Spalding T. Anatomic ACL reconstruction: the normal central tibial footprint position and standardized technique for measuring tibial tunnel location on 3D CT. Knee Surg Sports Traumatol Arthrosc. 2015 Jul 1 doi: 10.1007/s00167-015-3683-8. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Tsukada H., Ishibashi Y., Tsuda E., Fukuda A., Toh S. Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci. 2008;13:122–129. [Google Scholar]
- 14.Forsythe B., Kopf S., Wong A.K. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010;92:1418–1426. doi: 10.2106/JBJS.I.00654. [DOI] [PubMed] [Google Scholar]
- 15.Englund M., Roos E.M., Roos H.P., Lohmander L.S. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford) 2001;40:631–639. doi: 10.1093/rheumatology/40.6.631. [DOI] [PubMed] [Google Scholar]
- 16.Noyes F.R., Stabler C.L. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med. 1989;17:505–513. doi: 10.1177/036354658901700410. [DOI] [PubMed] [Google Scholar]
- 17.Strobel M.J., Castillo R.J., Weiler A. Reflex extension loss after anterior cruciate ligament reconstruction due to femoral “high noon” graft placement. Arthroscopy. 2001;17:408–411. doi: 10.1053/jars.2001.21821. [DOI] [PubMed] [Google Scholar]
- 18.Lee M.C., Seong S.C., Lee S. Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy. 2007;23:771–778. doi: 10.1016/j.arthro.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Loh J.C., Fukuda Y., Tsuda E., Steadman R.J., Fu F.H., Woo S.L. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o'clock and 10 o'clock femoral tunnel placement. Arthroscopy. 2003;19:297–304. doi: 10.1053/jars.2003.50084. [DOI] [PubMed] [Google Scholar]
- 20.Scopp J.M., Jasper L.E., Belkoff S.M., Moorman C.T., 3rd The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy. 2004;20:294–299. doi: 10.1016/j.arthro.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Yamamoto Y., Hsu W.H., Woo S.L., Van Scyoc A.H., Takakura Y., Debski R.E. Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med. 2004;32:1825–1832. doi: 10.1177/0363546504263947. [DOI] [PubMed] [Google Scholar]
- 22.Papageorgiou C.D., Ma C.B., Abramowitch S.D., Clineff T.D., Woo S.L. A multidisciplinary study of the healing of an intraarticular anterior cruciate ligament graft in a goat model. Am J Sports Med. 2001;229:620–626. doi: 10.1177/03635465010290051501. [DOI] [PubMed] [Google Scholar]