Abstract
Background
Transjugular intrahepatic portosystemic shunt (TIPS) implantation is used for treatment of several complications in patients with liver cirrhosis. Recent studies have identified a survival benefit for patients on the waiting list after TIPS implantation, but the optimal time point for TIPS implantation prior to orthotopic liver transplantation (OLT) has not been established.
Study
This study retrospectively assessed patients undergoing TIPS implantation before or after listing for OLT at the Medical University of Vienna. n = 98 patients with TIPS on the waiting list between January 1993 and December 2013 were identified (n = 73 (74.5%) pre-listing TIPS, n = 25 (25.5%) post-listing TIPS). A matched control group at the time of OLT without TIPS (n = 60) was included.
Results
More patients with post-listing TIPS (28.0%, 7/25) showed clinical improvement and went off-list than patients with pre-listing TIPS (8.2%, 6/73, p = .0119). A similar proportion of patients with pre-listing TIPS (19.2%, 14/73) and post-listing TIPS (20.0%, 5/25) died on the OLT waiting list. Transplant surgery time was similar in patients with and without TIPS: 348(±13) vs. 337(±10) minutes (p = .5139). Estimated 1-year post-transplant survival was similar across all groups (pre-listing TIPS: 76.2%, post-listing TIPS: 86.0%, no TIPS: 91.2%, log-rank p = .1506).
Conclusion
TIPS should be considered in all liver transplant candidates, since it can obviate the need for OLT and optimize bridging to OLT.
Keywords: Orthotopic liver transplantation, waiting list, bridge to transplant, transjugular intrahepatic portosystemic shunt, portal hypertension
Key summary
Transjugular intrahepatic portosystemic shunt (TIPS) can be used prior to orthotopic liver transplantation (OLT) to treat complications of portal hypertension, but data is limited on the optimal time point of TIPS implantation and patient survival after transplantation.
Therefore, patients who received a TIPS prior to listing or after listing were retrospectively analysed and compared with a control group without TIPS implantation.
TIPS implantation has no negative impact on perioperative or postoperative outcome parameters (on-list mortality, perioperative bleeding, surgery time, postoperative survival) but leads to a significant reduction of hepatic venous pressure gradient (HVPG). In some patients, it can obviate the need for OLT, and it can therefore be safely used as bridging therapy before OLT.
Introduction
Surgical advancements, a better control of the underlying disease and refined organ preservation in combination with optimized immunosuppressive therapy have led to improved graft and patient survival rates after liver transplantation. However, there is still significant mortality on the liver transplantation waiting list.1 The donor organ shortage leads to long wait-list times, while patients with advanced liver cirrhosis may suffer from several severe complications such as variceal bleeding and refractory ascites while waiting for their transplantation. Optimal therapy and management on the waiting list are necessary in order to ‘bridge’ these patients to transplant and avoid intercurrent complications.
Portal hypertension is responsible for most severe complications of patients with decompensated liver cirrhosis,2 such as variceal bleeding3 or refractory ascites,4 spontaneous bacterial peritonitis5 and hepatorenal syndrome (HRS).6 In order to assess the risk for variceal bleeding, invasive as well as non-invasive diagnostic tools are available. While measurement of the hepatic venous pressure gradient (HVPG) remains the gold standard, non-invasive methods such as spleen and liver stiffness measurement (LSM) may be useful.7 In the case of significant liver cirrhosis (HVPG > 10 mmHg, LSM > 16.1 kPa8), medical treatment is currently limited to non-selective beta blockers (NSBB) and variceal ligation, which can prevent variceal bleeding.9 However, NSBB also exert non-haemodynamic beneficial effects,10 and in patients with advanced liver disease and ascites NSBBs may be detrimental to survival.11,12 Thus, insertion of a transjugular intrahepatic portosystemic shunt (TIPS) could be an effective option both for prevention of variceal bleeding13 and for control of refractory ascites.14,15
A TIPS leads to creation of a low-resistant connection between the hepatic vein and the intrahepatic portion of the (usually right branch of the) portal vein and can be used as effective treatment for refractory ascites and variceal (re-)bleeding in these patients.12,16 Nowadays, only covered stents (i.e. polytetrafluoroethylene (PTFE)-covered stents) are used, since they are associated with higher patency and superior outcomes as compared with bare metal stents.17
In recent years, early implantation of TIPS in patients with severe variceal bleeding (‘early TIPS’) has been shown to be associated with not only excellent bleeding control but also improved survival.18 Results, as measured by a decrease in HVPG, are encouraging, and early implantation seems – at least in the setting of acute variceal bleeding – to be more beneficial than standard medical and endoscopic therapy.19 Although data is available for end-stage liver disease patients, its impact on the course of liver transplantation has not been extensively studied, and the extent of available literature is limited.20 Notably, the implantation of an intrahepatic shunt should not complicate the technical feasibility of liver transplantation as long as there is no stent extension to the inferior caval vein that might complicate clamping during the operation. Furthermore, TIPS can treat (and avoid) portal vein thrombosis21,22 – a major complication of liver transplant candidates. In summary, there are several potential mechanisms that support a favourable role of TIPS implantation on the liver transplant waiting list – especially in patients with severe portal hypertension.
Nevertheless, TIPS implantation itself has a 30-day mortality reported between 4% and 45%,11 and benefits as well as potential complications (e.g. hepatic encephalopathy) should be evaluated carefully. In a recent study that investigated the impact of TIPS implantation before listing for OLT in patients suffering from liver cirrhosis in the United Network for Organ Sharing (UNOS) database, TIPS implantation was associated with a lower risk of death.22
To our knowledge, however, there are few trials investigating the effects of TIPS implantation on the outcome of patients on the waiting list. Therefore, we conducted a retrospective, single-centre cohort study in a tertiary care hospital in order to investigate the influence of TIPS implantation on patients waiting for liver transplantation and on outcome thereafter.
Patients and methods
Study design and patient selection
We retrospectively reviewed adult patients listed for OLT between 1 January 1993 and 31 December 2013 at the Medical University of Vienna and who were evaluated for TIPS implantation before OLT. The retrospective study was approved by the Medical University of Vienna’s institutional review board (https://ekmeduniwien.at/cor/catalog/2016; EC Number 2119/2015). The routine evaluation for TIPS implantation includes an imaging study (computed tomography/magnetic resonance (CT/MR), also to exclude hepatocellular carcinoma (HCC) or other hepatic malignancy), a liver function test (Model of End Stage Liver Disease (MELD), CHILD), an echocardiography (to exclude significant cardiac impairment, especially pulmonary hypertension), a chest x-ray (to screen for hydrothorax), and paracentesis (to exclude non-portal hypertensive ascites). Bilirubin > 5 mg/dL (except for cholestatic liver disease, i.e. primary biliary cirrhosis/primary sclerosing cholangitis (PSC/PBC)) and recurrent spontaneous episodes of severe hepatic encephalopathy (HE) (West-Haven Grade III/IV) are considered as contraindications to TIPS. The mean MELD at listing in Vienna is 17, while the mean MELD at OLT in Vienna is 18.23
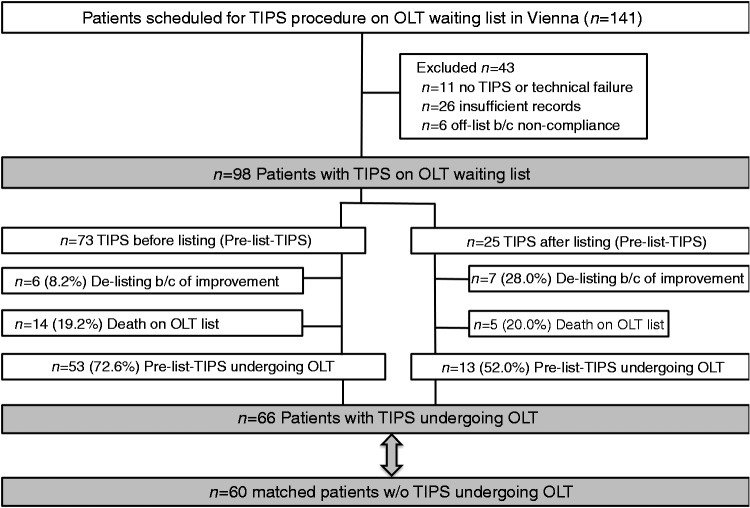
We could identify n = 141 patients in the indicated time period, of whom we had to exclude n = 11 who did not receive a TIPS implantation due to technical failure or for other reasons, n = 26 because of insufficient records and n = 6 who went off-list because of non-compliance (see Figure 1). In patients suffering from HCC, which represents a relative contraindication to TIPS implantation, the needle tract (i.e. the TIPS puncture channel) was outside the HCCs.
Figure 1.
Patient flow chart. Flow chart depicting patient selection and inclusion as well as exclusion criteria.
During the analysed time period, 336 patients were evaluated for TIPS implantation and 332 successfully received TIPS implantation at our tertiary care centre (unpublished data). However, we do not have the data for the referring secondary care centres, which also occasionally perform TIPS implantations but not OLT.
Laboratory values
Patients were systematically followed at the outpatient clinic of the Division of Transplantation at the Medical University of Vienna. Data was extracted from the patients’ medical records. Laboratory values (serum creatinine, bilirubin, albumin, haemoglobin, platelet count, alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transpeptidase (GGT) and prothrombin time (PT)) were assessed at the time of TIPS implantation, at the time of listing for OLT, 3 months after listing, at the time of OLT, and 3, 6, 12, 18 and 24 months after OLT.
Statistical analysis
Groups were compared for baseline characteristics (such as age, gender, body mass index (BMI), hepatic malignancy, number of hospitalizations for liver-related causes, MELD score at listing and OLT, mean wait list time) and perioperative parameters (such as mean OLT operation time, the number of packed red blood cells (PRBCs) or fresh frozen plasma units (FFP) used during transplantation, as well as postoperative variables such as length of follow up, number of bleeding-related post-OLT revisions, and requirement for renal replacement therapy and kidney function assessed by serum creatinine levels 7 days post OLT). Student’s t-test was calculated for normally distributed values and Mann–Whitney U test for non-parametric values. Chi-squared test was used for categorical variables. Where indicated, analysis of variance (ANOVA) was used if more than two groups were compared. Kaplan–Meier curves for overall survival were plotted, and the log-rank test was used for comparing time-dependent outcomes of the different subgroups (pre-listing TIPS vs. post-listing TIPS vs. no TIPS). GraphPad Prism 6 (GraphPad Software, Inc., La Jolla, CA) was used for statistical analysis. A p-value < .05 was considered to denote statistical significance.
Results
Patient characteristics
Finally, n = 98 patients had a TIPS implanted either before listing (n = 73, pre-listing TIPS) or after listing for OLT (n = 25, post-listing TIPS). Type of TIPS was recorded, with n = 44 PTFE-TIPS and n = 19 bare metal stents. Of these n = 98 patients, n = 66 underwent OLT. A control group of n = 60 patients without TIPS was matched according to age, sex, BMI and underlying disease at the time of OLT. There were no statistically significant differences in the baseline characteristics between the TIPS group and the no-TIPS control group, except for a higher listing-MELD score in the control group (15.73 (±0.45) MELD in the pre-listing, 14.41 (±0.90) MELD in the post-listing and 17.98 (±0.90) MELD in the control group (p = .007) (Table 1). Among patients finally undergoing OLT after TIPS, the indications were prophylaxis of variceal rebleeding in n = 37, refractory ascites in n = 25, and acute portal vein thrombosis in n = 1. TIPS was highly effective in decreasing portal pressure, from an HVPG of 21.2 mmHg to a portal pressure gradient of 8.7 mmHg, corresponding to a mean decrease of 12.1 mmHg after the TIPS procedure.
Table 1.
Patient characteristics according to the subgroups defined as pre-listing TIPS, post-listing TIPS and matched control group without TIPS
| TIPS before listing | TIPS after listing | No TIPS | p value | |
|---|---|---|---|---|
| Patients (n) | 73 | 25 | 60 | n/a |
| Age at listing (mean ± SEM) | 53.51 (±1.20) | 55.92 (±2.6) | 51.27 (±1.097) | .2049 |
| Sex M/F (% male) | 54/19 (74) | 19/6 (76) | 46/14 (76.7) | .9342 |
| BMI (kg/m2) at listing (mean ± SEM) | 25.68 (±0.52) | 23.89 (±0.89) | 25.91 (±0.65) | .5689 |
| MELD score at listing (mean ± SEM) | 15.73 (±0.45) | 14.41 (±0.90) | 17.98 (±0.8957) | .0067 |
| MELD score at OLT for patients undergoing OLT (mean ± SEM) | 17.51 (±0.80) | 19.49 (±1.57) | 19.33 (±0.89) | .2665 |
IQR: interquartile range; MELD: Model for End-Stage Liver Disease; OLT: orthotopic liver transplantation; SEM: standard error of the mean.
All TIPS were routinely monitored using ultrasound examination until the time of OLT. In the case of TIPS stenosis/thrombosis, patency was restored by radiological intervention. At the time of OLT, all TIPS were open. In all but four available patients, 10 mm diameter TIPS was used. In three patients, TIPS diameter was 8 mm, and in one patient, TIPS diameter was 12 mm. In three patients, no data on type of TIPS was available.
Clinical improvement due to TIPS implantation
In our cohort, more patients with post-listing TIPS showed clinical improvement (7/25; 28.0%) and went off-list than patients with a pre-listing TIPS implantation (6/73; 8.2%; p = .0119). However, a similar proportion of patients of the pre-listing TIPS group (14/73, 19.2%) and the post-listing TIPS group (5/25, 20.0%) died on the waiting list.
MELD score evolution on the waiting list was similar for patients with pre-listing TIPS and post-listing TIPS (listing-MELD: 15.7 ± 0.5 vs. 14.4 ± 0.9, p = .1532; OLT-MELD: 17.5 ± 0.8 vs. 19.5 ± 1.6, p = .2697). Interestingly, MELD scores for patients in the combined TIPS group (pre-listing TIPS and post-listing TIPS combined) were significantly lower at the time of listing compared with the no-TIPS control group (15.9 ± 0.5 for TIPS vs. 18.0 ± 0.9 for no-TIPS; p = .0368), while this difference was not significant at the time of OLT (17.9 ± 0.7 for TIPS vs. 19.3 ± 0. 9 for no-TIPS; p = .2110).
Although TIPS implantation in general had no effect on the average time that patients were listed before undergoing OLT (213 (±29) days with TIPS vs. 156 (±18) days without TIPS implantation, p = .1054), patients with TIPS implantation had a significantly higher number of hospitalizations due to liver-related causes, mainly HE episodes (1.0 (interquartile range (IQR) 0.0–2.5) for TIPS vs. 0.0 (IQR 0.0–1.0) for no-TIPS, p = .0007; Table 1).
Effect of TIPS on transplant surgery, blood product requirement and postoperative complications
See Table 2 for patient characteristics and perioperative outcome. In our cohort, TIPS implantation had no effect on the mean surgery time for OLT when compared with the matched patients without TIPS implantation. Mean surgery time was 348 (±13) min in the TIPS groups compared with 337 (± 10) min in the no-TIPS group (p = .5139). A median of 3 (IQR 0–7) PRBCs were used in patients with TIPS during OLT, while a median of 5 (IQR 2–8) PRBCs were transfused in patients without TIPS (p = .2014). Concerning FFP, a median of 6 (IQR 4–10) and 8 (IQR 1–11) were used in TIPS vs. no TIPS patients, respectively (p = .9372). A similar proportion of patients had bleeding complications, as there were 4/66 patients (6.1%) who needed surgical intervention in the TIPS group and 6/60 patients (10%) in the group without prior TIPS implantation (p = .4139). Regarding kidney function, 6/66 patients (10%) in the TIPS group and 3/60 patients (5%) in the no-TIPS group required postoperative short-term renal replacement therapy (p = .3732). Serum creatinine levels 1 week after OLT were comparable between groups (1.13 ± 0.07 mg/dL in the TIPS vs. 1.12 ± 0.08 mg/dL in the no-TIPS group, p = .9704).
Table 2.
Patient characteristics and perioperative outcome of patients with versus without TIPS prior to OLT
| TIPS before OLT | No TIPS | p value | |
|---|---|---|---|
| Patients (n) | 66 | 60 | n/a |
| Age at listing (mean ± SEM) | 51.26 (± 1.357) | 51.27 (±1.097) | .9939 |
| Sex M/F (% male) | 52/14 (78.8) | 46/14 (76.7) | .7748 |
| Reason for OLT listing | |||
| Hepatic malignancy (n/n (%)) | 7/66 (10.6) | 6/60 (10.0) | .9111 |
| Alcoholic liver disease (n/n (%)) | 33/66 (50.0) | 31/60 (51.7) | .8517 |
| Viral hepatitis (n/n (%)) | 15/66 (22.7) | 14/60 (23.3) | .9357 |
| Cryptogenic cirrhosis (n/n (%)) | 5/66 (7.6) | 6/60 (10) | .6302 |
| Other liver diseases (n/n (%)) | 6/66 (9) | 3/60 (5) | .3732 |
| Perioperative outcome | |||
| Operating time (min, mean ± SEM) | 348 (±13) | 337 (±10) | .5139 |
| No. of PRBC intraoperatively (median (IQR)) | 3 (0–7) | 5 (2–8) | .2014 |
| No. of FFPs or Octaplas intraoperatively (median (IQR)) | 6 (4–10) | 8 (1–11) | .9372 |
| No. of postoperative bleeding-related revisions | 4/66 (6.1) | 6/60 (10) | .4139 |
| Patients requiring postoperative short-term renal replacement therapy | 6/66 (10) | 3/60 (5) | .3732 |
| Serum creatinine 7 days after OLT (mg/dL (mean ± SEM)) | 1.13 (±0.07) | 1.12 (±0.08) | .9704 |
FFP: fresh frozen plasma; IQR: interquartile range; OLT: orthotopic liver transplantation; PRBC: packed red blood cells; SEM: standard error of the mean.
Effect of TIPS on platelet counts and kidney function
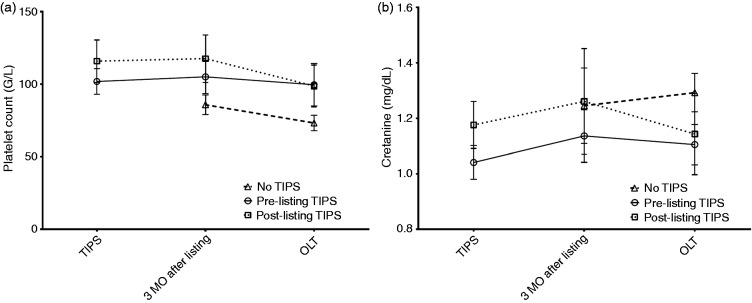
At the time of listing for OLT, patients who had received a pre-listing TIPS showed a tendency towards higher platelet counts at listing, although this was not statistically significant for patients with pre-listing TIPS as compared with patients without TIPS (120 ± 13 G/L vs. 94 ± 9 G/L, p = .130). At the time of OLT, the tendency towards higher platelet counts in patients with TIPS (pre-listing and post-listing TIPS) remained, although without statistical significance (99 ± 12 G/L with TIPS vs. 73 ± 5 G/L without TIPS, p = .0587) (Figure 2).
Figure 2.
Pre-transplant course of laboratory parameters. (a) Changes in platelet count in patients undergoing TIPS implantation before listing (pre-listing TIPS), after listing (post-listing TIPS) and patients without TIPS implantation (no TIPS). Although there was a tendency towards lower platelet counts in patients without TIPS implantation, differences did not reach statistical significance. (b) Serum creatinine levels in patients undergoing TIPS implantation before listing (pre-listing TIPS), after listing (post-listing TIPS) and without TIPS implantation (no TIPS).
Serum creatinine, as an indicator of kidney function, showed a tendency towards better renal function in pre-listing TIPS patients, but differences did not reach statistical significance at any time point. Interestingly, TIPS patients had a more stable renal function on the waiting list, while patients without a TIPS showed a steady increase in serum creatinine levels (Figure 2).
Postoperative course of patients with and without TIPS before OLT
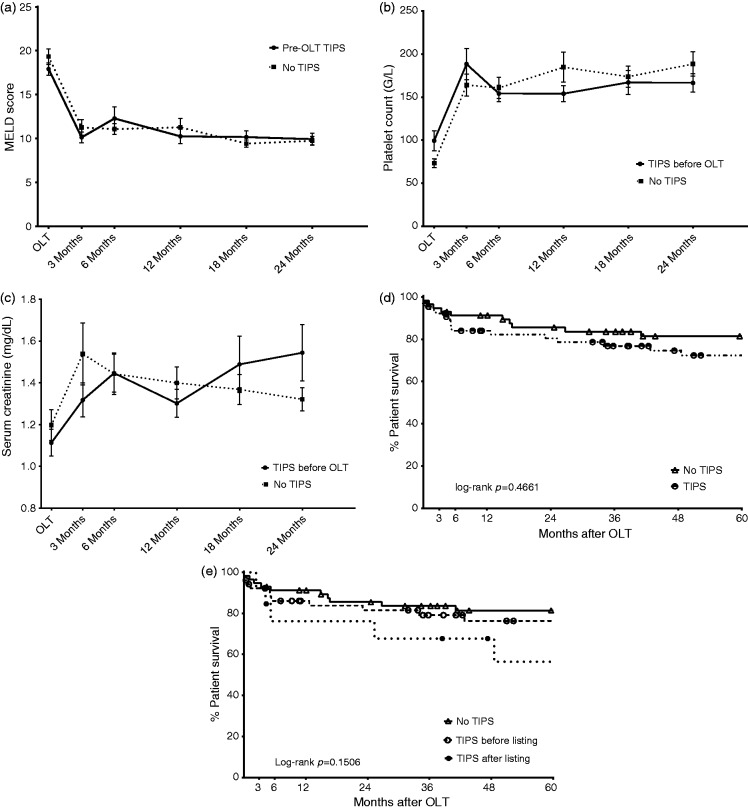
After OLT, the post-operative course was similar between patients who had received TIPS implantation and those who had not (Figure 3). The MELD score showed a significant reduction after OLT and remained low in both groups, while platelet counts recovered and remained high in the post-transplant course. Kidney function did not significantly improve after OLT, as serum creatinine levels in both groups increased.
Figure 3.
Post-transplant course of patients with or without TIPS before OLT. (a) MELD score evolution after OLT. (b) Platelet count after OLT. (c) Serum creatinine levels after OLT. (d) Five-year post-transplant patient survival in patients with or without pre-transplant TIPS implantation. (e) Five-year post-transplant patient survival. Subgroups of patients receiving pre-transplant TIPS implantation were evaluated separately.
Overall survival was similar between patients with and without TIPS before OLT, with an estimated 1-year post-transplant survival of 76.2% in the pre-listing TIPS group, 86.0% in the post-listing TIPS group and 91.2% in the no-TIPS group.
Five-year overall survival was 76.2% in the pre-listing TIPS group, 56.4% in the post-listing TIPS group and 81.4% in the no-TIPS group (log-rank p = .1506).
Interestingly, patients who were de-listed because of clinical and laboratory improvements showed a similar 5-year survival rate to that of patients undergoing OLT (Supplementary Figure 1).
Discussion
Our study demonstrates that TIPS implantation does not complicate liver transplantation and does not improve survival on the waiting list. Additionally, our results indicate that TIPS should be implanted before considering listing the patient for liver transplantation, because a significant proportion of decompensated patients (especially those with refractory ascites) will show clinical improvement and not require OLT in the absence of further deterioration of liver function. However, depending on waiting list time and mortality, and if resources permit, listing of patients prior to TIPS procedure could be desirable in order to shorten waiting list time in the case of post-TIPS deterioration of liver function, considering an approximately 25% waiting list mortality at our centre.23 The waiting list mortality of our TIPS patients on-list was only 19.4% (19/98). This would also suggest that implantation of a TIPS is a sufficient strategy to bridge patients to OLT.
A recent study by Berry et al. has shown a lower mortality rate on the waiting list for patients receiving a TIPS implantation in their UNOS registry analysis.22 In our study, we could not evaluate the effect of TIPS implantation on mortality reduction on the waiting list, as we did not have a suitable control group. However, mortality rates of patients receiving either pre-listing TIPS or post-listing TIPS implantation were comparable to the published results of the aforementioned study by Berry et al., being 19.2% and 20%, respectively.
To analyse the net effect of a TIPS on the waiting list, we included a control group without TIPS. However, considering that patients undergoing TIPS implantation are potentially sicker than patients who do not need an intervention, matching a control group is challenging. Therefore, we matched patients who had similar baseline characteristics at the time of transplantation, being aware of the limitations of this method. Surgical procedures and perioperative management as well as medical therapy for portal hypertension have changed during the study period; thus, we cannot completely exclude some bias introduced by optimized patient management over time due to an era effect.
Since the indication of TIPS (i.e. emergency TIPS versus elective TIPS) may have influenced the prognosis, we have assessed the indications among the group of patients receiving TIPS and finally OLT, but found that even ‘bleeding’ TIPS were mostly performed as elective procedures similar to TIPS for refractory ascites. Early TIPS was only recently adopted for daily clinical practice and thus did not influence our results.
Considering the perioperative outcome, TIPS implantation did not lead to a higher risk of intraoperative complications or a longer operation time. Clamping of the inferior caval vein was possible in all cases, although stent dislocation can complicate the clamping procedure. Notably, the piggyback OLT technique was not used in any of the reported patients; this could potentially be complicated due to dislocated TIPS stent grafts or stents extending far into the inferior caval vein.
On the other hand, there was a trend towards lower need for blood product transfusions. This might be explained by effective treatment of portal hypertension by TIPS and, thus, less severe portal hypertensive bleeding during surgery. However, TIPS implantation had no effect on the rate of surgical complications (including bleeding complications) after OLT.
Since previous studies have shown a decreased risk for HRS with TIPS implantation,15 we also assessed renal function after OLT with versus without TIPS. However, TIPS did not impact on postoperative renal function, as assessed by serum creatinine levels 1 week after OLT and the requirement for renal replacement therapy.
Interestingly, patients who went off-list because of clinical improvement after TIPS had a similar 5-year overall survival rate when compared with patients undergoing OLT. Although this finding only represents a single-centre experience and the number of patients is low, this finding was unexpected and should be validated in further prospective studies.
In conclusion, our data suggests that liver transplant candidates should always be evaluated for TIPS, since successful reduction of portal pressure might obviate the need for OLT by avoiding further clinical deterioration related to portal hypertension. Thus, in our hands, TIPS represents an essential tool for the management of portal hypertension in the liver transplant setting.
Supplementary Material
Conflict of interest
TR has received travel support and speaker fees from W.L. Gore. All other authors do not have any conflict of interest related to this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The retrospective study was approved by the Medical University of Vienna's institutional review board (https://ekmeduniwien.at/cor/catalog/2016, EC Number 2119/2015).
Informed consent
All datasets were anonymized prior to statistical analysis. In line with the EC policies for retrospective studies, no written informed consent was obtained from the individual patients.
References
- 1.Massie AB, Luo X, Alejo JL, et al. Higher mortality in registrants with sudden model for end-stage liver disease increase: Disadvantaged by the current allocation policy. Liver Transpl 2015; 21: 683–689. [DOI] [PubMed] [Google Scholar]
- 2.de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol 2015; 63: 743–752. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Tsao G, Bosch J. Varices and variceal hemorrhage in cirrhosis: A new view of an old problem. Clin Gastroenterol Hepatol 2015; 13: 2109–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sola E, Sole C, Gines P. Management of uninfected and infected ascites in cirrhosis. Liver Int 2016; 36(Suppl 1): 109–115. [DOI] [PubMed] [Google Scholar]
- 5.Schwabl P, Bucsics T, Soucek K, et al. Risk factors for development of spontaneous bacterial peritonitis and subsequent mortality in cirrhotic patients with ascites. Liver Int 2015; 35: 2121–2128. [DOI] [PubMed] [Google Scholar]
- 6.Bucsics T, Schwabl P, Mandorfer M, et al. The trigger matters - outcome of hepatorenal syndrome versus specifically-triggered AKI in cirrhotic patients with ascites. Liver Int 2016; 36: 1649–1656. [DOI] [PubMed] [Google Scholar]
- 7.Buechter M, Kahraman A, Manka P, et al. Spleen and liver stiffness is positively correlated with the risk of esophageal variceal bleeding. Digestion 2016; 94: 138–144. [DOI] [PubMed] [Google Scholar]
- 8.Schwabl P, Bota S, Salzl P, et al. New reliability criteria for transient elastography increase the number of accurate measurements for screening of cirrhosis and portal hypertension. Liver Int 2015; 35: 381–390. [DOI] [PubMed] [Google Scholar]
- 9.Reiberger T, Ulbrich G, Ferlitsch A, et al. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with haemodynamic non-response to propranolol. Gut 2013; 62: 1634–1641. [DOI] [PubMed] [Google Scholar]
- 10.Reiberger T, Ferlitsch A, Payer BA, et al. Non-selective betablocker therapy decreases intestinal permeability and serum levels of LBP and IL-6 in patients with cirrhosis. J Hepatol 2013; 58: 911–921. [DOI] [PubMed] [Google Scholar]
- 11.Freedman AM, Sanyal AJ, Tisnado J, et al. Complications of transjugular intrahepatic portosystemic shunt: A comprehensive review. Radiographics 1993; 13: 1185–1210. [DOI] [PubMed] [Google Scholar]
- 12.Rossle M, Gerbes AL. TIPS for the treatment of refractory ascites, hepatorenal syndrome and hepatic hydrothorax: A critical update. Gut 2010; 59: 988–1000. [DOI] [PubMed] [Google Scholar]
- 13.Sauerbruch T, Mengel M, Dollinger M, et al. Prevention of rebleeding from esophageal varices in patients with cirrhosis receiving small-diameter stents versus hemodynamically controlled medical therapy. Gastroenterology 2015; 149: 660–8 e1. [DOI] [PubMed] [Google Scholar]
- 14.Bureau C, Garcia-Pagan JC, Otal P, et al. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: Results of a randomized study. Gastroenterology 2004; 126: 469–475. [DOI] [PubMed] [Google Scholar]
- 15.Gines P, Uriz J, Calahorra B, et al. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology 2002; 123: 1839–1847. [DOI] [PubMed] [Google Scholar]
- 16.Lo GH, Liang HL, Chen WC, et al. A prospective, randomized controlled trial of transjugular intrahepatic portosystemic shunt versus cyanoacrylate injection in the prevention of gastric variceal rebleeding. Endoscopy 2007; 39: 679–685. [DOI] [PubMed] [Google Scholar]
- 17.Perarnau JM, Le Gouge A, Nicolas C, et al. Covered vs. uncovered stents for transjugular intrahepatic portosystemic shunt: A randomized controlled trial. J Hepatol 2014; 60: 962–968. [DOI] [PubMed] [Google Scholar]
- 18.Garcia-Pagan JC, Caca K, Bureau C, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med 2010; 362: 2370–2379. [DOI] [PubMed] [Google Scholar]
- 19.Garcia-Pagan JC, Di Pascoli M, Caca K, et al. Use of early-TIPS for high-risk variceal bleeding: Results of a post-RCT surveillance study. J Hepatol 2013; 58: 45–50. [DOI] [PubMed] [Google Scholar]
- 20.Wroblewski T, Rowinski O, Zurakowski J, et al. Transjugular Intrahepatic Porto-Caval Shunt (TIPS) in treatment of portal hypertension in liver transplant recipiens. Ann Transplant 2008; 13: 42–45. [PubMed] [Google Scholar]
- 21.Salem R, Vouche M, Baker T, et al. Pretransplant portal vein recanalization-transjugular intrahepatic portosystemic shunt in patients with complete obliterative portal vein thrombosis. Transplantation 2015; 99: 2347–2355. [DOI] [PubMed] [Google Scholar]
- 22.Berry K, Lerrigo R, Liou IW, et al. Association between transjugular intrahepatic portosystemic shunt and survival in patients with cirrhosis. Clin Gastroenterol Hepatol 2016; 14: 118–123. [DOI] [PubMed] [Google Scholar]
- 23.Gyori GP, Silberhumer GR, Zehetmayer S, et al. Dynamic changes in MELD score not only predict survival on the waiting list but also overall survival after liver transplantation. Transpl Int 2012; 25: 935–940. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.