Abstract
Background.
Mobility limitations are prevalent, potentially reversible precursors to mobility loss that may go undetected in older adults. This study evaluates standardized administration of an endurance walk test for identifying unrecognized and impending mobility limitation in community elders.
Methods.
Men and women (1480 and 1576, respectively) aged 70–79 years with no reported mobility limitation participating in the Health, Aging and Body Composition study were administered the Long Distance Corridor Walk. Walk performance was examined to determine unrecognized mobility deficits at baseline and predict new self-recognition of mobility limitation within 2 years.
Results.
On testing, 23% and 36% of men and women evidenced mobility deficits defined as a contraindication to exertion, meeting stopping criteria or exceeding 7 minutes to walk 400 m. Unrecognized deficits increased with age and were more prevalent in blacks, smokers, obese individuals, and infrequent walkers. Within 2 years, 21% and 34% of men and women developed newly recognized mobility limitation; those with baseline unrecognized deficits had higher rates, 40% and 54% (p <.001), respectively. For each additional 30 seconds over 5 minutes needed to walk 400 m, likelihood of newly recognized mobility limitation increased by 65% and 37% in men and women independent of age, race, obesity, smoking status, habitual walking, reported walking ease, and usual gait speed.
Conclusions.
A sizable proportion of elders who report no walking difficulty have observable deficits in walking performance that precede and predict their recognition of mobility limitation. Endurance walk testing can help identify these deficits and provide the basis for treatment to delay progression of mobility loss.
Keywords: Mobility, Walking, Limitation, Endurance, Performance, Testing
CAPACITY to walk unaided is a hallmark of independence, particularly for older adults. Mobility limitation, typically defined as reported difficulty walking for one-quarter mile or climbing one flight of stairs, represents an initial, potentially reversible stage of mobility loss; a precursor to mobility disability, the inability to ambulate without great difficulty or assistance (1,2). National surveys estimate upwards of 40% of persons 65 years old or older have mobility limitation (3,4), yet walking ability is not routinely or systematically assessed in clinical practice (5,6). Moreover, because few older adults, even those who report no walking difficulty, regularly walk (7–9), there is likely to be substantial unrecognized mobility limitation (10).
Timed gait over a short distance and performance on brief tests of lower extremity function consistently predict mobility limitation and disability (11–14). These measures, however, may be insufficiently challenging to capture the preponderance of persons with cardiorespiratory endurance-related or vascularly related threats to mobility (15–17). Symptom reports and perceptions of functional difficulty require a level of sustained exertion rarely achieved by the majority of older adults (18). Thus, questions about walking difficulty over a distance of one-quarter mile or more may be answered inaccurately simply because the respondent has not attempted to walk such a distance in quite some time. This study examines the prevalence of unrecognized mobility deficits in relation to habitual walking behavior and social-environmental characteristics and evaluates the utility of standardized administration of a self-paced endurance walk test, the Long Distance Corridor Walk (LDCW) for identifying such deficits and impending mobility limitations in community-dwelling persons aged 70–79 years. Specifically, this study analyzes rates of poor endurance walk performance and correlated sociodemographic and behavioral factors and determines the relationship between performance and newly self-recognized mobility limitation within 2 years independent of sociodemographic factors and common indicators of functional capacity, including walking speed over a short (6-meter) course. A secondary objective is to evaluate the potential value of the LDCW for identifying persons with covert mobility problems who otherwise demonstrate good function.
Methods
Study Population
The parent cohort consists of 3075 black and white community-dwelling men and women from designated ZIP code areas surrounding the Memphis, Tennessee and Pittsburgh, Pennsylvania study centers participating in the Health, Aging and Body Composition (Health ABC) study, a longitudinal investigation of the role of physiological, behavioral, sociodemographic, and disease-related factors in the development of functional limitation and disability. Potential participants were identified from Medicare beneficiary files, with a random sample of white and all age-eligible black adults invited to participate. Enhanced recruitment strategies were used to facilitate desired enrollment targets of black residents. Eligibility criteria included age between 70 and 79 years during the recruitment period (April 1997 through June 1998), capacity to self-respond to all questions and participate in all testing, no need for a walking aid and no reported difficulty walking one-quarter mile, climbing one flight of stairs without resting, or performing basic activities of daily living. Persons planning to leave the area within 3 years, reporting a diagnosis of a life-threatening cancer, or enrolled in a lifestyle intervention study were excluded.
Initial eligibility screening was conducted by telephone and confirmed at the in-home interview, which ascertained sociodemographic characteristics, medical history, and health-related behaviors including physical activity and physical function. A comprehensive clinical examination followed within 2 weeks and included, among other tests, an electrocardiogram; assessments of height, weight, blood pressure, and usual gait speed; and evaluation of eligibility for and administration of the LDCW. All participants provided written informed consent, and the institutional review boards at both study centers approved all protocols. Of the 3075 participants, 8 persons with incomplete follow-up data and 11 who died within the first 6 months were excluded from the analysis, yielding a sample of 3056 persons.
Endurance Walk Test
The LDCW constitutes a two-stage, self-paced endurance walk test performed over a 20-meter course (19,20). Stage one consists of a 2-minute warm-up walk in which participants are instructed to “cover as much ground as possible.” Stage two follows immediately and consists of a 400-meter walk done “as quickly as possible at a pace that can be maintained.” Prior to testing, participants were screened in accordance with the American College of Sports Medicine guidelines for exercise testing (21). Trained and certified examiners conducted a resting electrocardiogram and measured participants' standing blood pressure and radial pulse. Persons with any of the following electrocardiogram abnormalities—Wolff–Parkinson–White or ventricular pre-excitation, idioventricular rhythm, ventricular tachycardia, third degree or complete A-V block, evidence of acute injury or ischemia or marked T-wave abnormality; systolic or diastolic blood pressure exceeding 199 mmHg or 109 mmHg, respectively; or heart rate <40 or >110 beats per minute—were excluded from testing. Using a standardized questionnaire, participants were also asked whether they had a myocardial infarction, angioplasty, or heart surgery in the 3 months prior to their clinic visit or experienced new or worsening symptoms of chest pain, shortness of breath, fainting, or angina. Persons with any affirmative response were also excluded from attempting the LDCW.
Heart rate was continuously monitored during testing (Polar Pacer, Model 61190; Polar Electro, Oy, Finland) and participants were stopped if: (a) their heart rate exceeded 135 beats per minute, which represents 85%–90% of the age-predicted maximum heart rate for persons aged 70–79 years (22); or (b) they experienced debilitating pain (e.g., claudication, or musculoskeletal pain in the feet, knees, hips, or back), shortness of breath, syncope, or excessive fatigue. Distance covered in 2 minutes and time needed to complete 400 m were recorded as well as ending heart rate and blood pressure, and reason for stopping when applicable.
Self-Reported Walking Ability
As a condition of study eligibility, all participants were free of reported difficulty walking for one-quarter mile. To differentiate perceived walking ability at baseline and during the follow-up (15), participants were asked, “Because of a health or physical problem, do you have any difficulty walking for one mile that is about 8 to 12 blocks?” Those reporting no difficulty were asked how easy it is for them to walk for one mile: “very easy,” “somewhat easy,” or “not so easy.”
Other Covariates
Demographic factors included participant-designated race as white or black, sex, and study site. Smoking status was dichotomized as never or former smoker who quit by age 50 and current or former smoker who quit after age 50. Obesity was considered present if body mass index (BMI) derived from measured height and weight equaled or exceeded 30 kg/m2.
Walking frequency was determined from responses to two questions that distinguished walking for exercise and other types of walking, such as walking to the store or walking the dog from a standardized, interviewer-administered physical activity battery (23). Participants were asked how many times they did either type of walking in the past 7 days and the average length of each session in minutes. Persons walking a total of <30 minutes per week were considered to be infrequent or nonwalkers.
Usual gait speed constitutes the faster of two trials in which participants were asked to walk at their usual pace between taped lines placed 6 m apart (15).
Outcome Measures
Unrecognized mobility deficits
At baseline, unrecognized mobility deficits were considered present when a participant: (a) met established exclusion criteria (see above) indicating a contraindication to exertion or outright refused to attempt the LDCW; (b) met stopping criteria and did not complete the LDCW; or (c) needed >7 minutes to walk 400 m, which equates to a cardiorespiratory fitness level of <12 mL O2/kg/min (20), the minimum level deemed necessary to cross an intersection (24).
Newly recognized mobility limitation
Persons reporting difficulty walking for one-quarter mile or climbing one flight of stairs without resting due to a physical or health problem at two consecutive semiannual follow-up contacts with the first report of difficulty occurring within 24 months or 2 years of the baseline visit were considered to have newly self-recognized mobility limitation. Those reporting a lot of difficulty or inability for either task were considered to have mobility disability. The follow-up period covers 30 months. We selected 2 years because we were interested specifically in the short-term prognostic value of endurance walk testing and believe that 2 years is a salient time frame for both patients and their families. The requirement for two consecutive reports of difficulty distinguishes transient from persistent limitations.
Statistical Analysis
Because older men typically demonstrate better physical performance than women at a given level of reported functioning (25), analyses were conducted separately for men and women. Differences between walkers and nonwalkers were evaluated using the chi-square statistic. Logistic regression was used to estimate relative odds of: (a) unrecognized mobility deficits at baseline associated with walking frequency and sociodemographic factors, and (b) newly self-recognized mobility limitation associated with sociodemographic factors and indicators of functional capacity and (i) LDCW completion status among persons eligible for testing, and (ii) each 30-second increase in time to walk 400 m over 5 minutes in those completing testing. Analyses used SAS software (version 8.2; SAS Institute, Cary, NC).
Results
The study cohort mean age was 74 years, 51% were women and 42% were black, and equal numbers were from Memphis and Pittsburgh. As shown in Table 1, within this cohort of 70-year-olds reporting no walking difficulty, 42% of men and 51% of women walked <30 minutes in the previous week, of which >90% reported no walking at all. Within sex-strata, blacks and Memphis participants were more likely to walk infrequently as were current or recent male smokers, obese women, and women who did not complete high school. Overall, 55% of men and 38% of women reported that walking for 1 mile is very easy, and 85% and 71% had a usual gait speed exceeding 1.0 m/s, typically considered indicative of good mobility (12,14).
Table 1.
Baseline Characteristics of the Study Cohort by Sex and Walking Behavior.
| Men |
Women |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Total (N = 1480) | Walker (N = 861) | Nonwalker (N = 619) | Total (N = 1576) | Walker (N = 777) | Nonwalker (N = 799) | ||||
| Age, y | 73.8 ± 2.9 | 73.8 ± 2.9 | 73.7 ± 2.9 | 73.5 ± 2.9 | 73.5 ± 2.9 | 73.5 ± 2.9 | ||||
| Black race, No. (%) | 546 (36.9) | 271 (31.5) | 275 (44.4) | 726 (46.1) | 290 (37.3) | 436 (54.6) | ||||
| Memphis site, No. (%) | 743 (50.2) | 397 (46.1) | 346 (55.9) | 793 (50.3) | 356 (45.8) | 437 (54.7) | ||||
| High school graduate, No. (%) | 1078 (72.8) | 645 (74.9) | 432 (69.8) | 1209 (76.8) | 644 (82.9) | 566 (70.9) | ||||
| Current or recent smoker, No. (%) | 498 (33.8) | 265 (30.8) | 235 (37.9) | 411 (26.2) | 189 (24.3) | 224 (28.1) | ||||
| Obese, No. (%) | 317 (21.4) | 172 (20.0) | 145 (23.4) | 462 (29.3) | 176 (22.7) | 286 (35.8) | ||||
| Nonwalker, No. (%) | 619 (41.8) | 799 (50.7) | ||||||||
| Reports walking 1 mile is very easy, No. (%) | 786 (55.0) | 523 (60.8) | 293 (47.3) | 575 (37.8) | 387 (49.8) | 217 (27.2) | ||||
| Usual gait speed, m/s | 1.23 ± 0.25 | 1.26 ± 0.24 | 1.20 ± 0.24 | 1.12 ± 0.22 | 1.16 ± 0.22 | 1.08 ± 0.21 | ||||
| Gait speed ≥1.0 m/s, No. (%) | 1258 (85.0) | 742 (86.2) | 516 (83.4) | 1117 (70.9) | 599 (77.1) | 518 (64.8) | ||||
Note: Nonwalkers reported walking a total of <30 minutes in a typical week. Plus–minus values are means ± standard deviations. Race was self-determined. Recent smoker includes former smokers who quit after the age of 50 years. Obesity is defined as a body mass index calculated as weight in kilograms divided by height in meters squared that exceeds 30.
Despite reports of no walking difficulty, 23% of men and 36% of women exhibited evidence of unrecognized mobility deficits; 12% and 14%, respectively, met established criteria indicating that brisk walking may be unsafe (21), and 11% and 22% showed objective evidence of mobility deficits, either because they could not complete the LDCW (7% and 14%) or needed >7 minutes to walk 400 m “as quickly as possible” (see Table 2). Unrecognized deficits were substantially greater in women who walked infrequently relative to women who walked at least 30 minutes per week—43.7% versus 27.5% (p <.001). Respective differences were less remarkable in men—25.7% versus 21.0% (p =.041). As shown in Table 3, in both men and women, the likelihood of unrecognized mobility deficits increased with age and was greater in blacks, current or recent smokers, and obese individuals independent of other attributes.
Table 2.
Exclusion, Completion Status, and Performance on the Long Distance Corridor Walk by Sex and Walking Behavior.
| Men |
Women |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Performance status | Total (N = 1480) | Walker (N = 861) | Nonwalker (N = 619) | Total (N = 1576) | Walker (N = 777) | Nonwalker (N = 799) | ||||||
| Excluded, No. (%) | 183 (12.4) | 94 (10.9) | 89 (14.4) | 218 (13.8) | 82 (10.6) | 136 (17.0) | ||||||
| Met clinical criteria, No. (%) | 81 (5.5) | 44 (5.1) | 37 (6.0) | 86 (5.5) | 35 (4.5) | 51 (6.4) | ||||||
| Abnormal ECG, No. (%) | 23 (1.6) | 9 (1.0) | 14 (2.3) | 19 (1.2) | 9 (1.2) | 10 (1.3) | ||||||
| Abnormal blood pressure, No. (%) | 28 (1.9) | 13 (1.5) | 15 (2.4) | 32 (2.0) | 13 (1.7) | 19 (2.4) | ||||||
| Abnormal heart rate, No. (%) | 21 (1.4) | 15 (1.7) | 6 (1.0) | 29 (1.8) | 10 (1.3) | 19 (2.4) | ||||||
| Recent event or surgery, No. (%) | 9 (0.6) | 7 (0.8) | 2 (0.3) | 6 (0.4) | 3 (0.4) | 3 (0.4) | ||||||
| Reported cardiac symptoms, No. (%) | 86 (5.8) | 42 (4.9) | 44 (7.1) | 112 (7.1) | 41 (5.3) | 71 (8.9) | ||||||
| Declined testing, No. (%) | 16 (1.1) | 8 (0.9) | 8 (1.3) | 20 (1.3) | 6 (0.8) | 14 (1.8) | ||||||
| Did not complete 400-meter walk, No. (%) | 109 (7.3) | 58 (6.7) | 51 (8.2) | 220 (14.0) | 79 (10.2) | 141 (17.7) | ||||||
| Stopped during/after 2 min walk, No. (%) | 42 (2.8) | 25 (2.9) | 17 (2.7) | 53 (3.4) | 19 (2.4) | 34 (4.3) | ||||||
| Stopped during 400-meter walk, No. (%) | 68 (4.6) | 33 (3.8) | 34 (5.5) | 167 (10.6) | 60 (7.8) | 107 (13.4) | ||||||
| Primary reason for stopping | ||||||||||||
| Heart rate exceeded 135 bpm, No. (%) | 51 (3.4) | 32 (3.7) | 19 (3.1) | 95 (6.0) | 46 (5.9) | 49 (6.1) | ||||||
| Leg pain, No. (%) | 31 (2.1) | 16 (1.8) | 15 (2.4) | 56 (3.6) | 16 (2.1) | 40 (5.0) | ||||||
| Foot, knee, hip, back pain, No. (%) | 6 (0.4) | 3 (0.4) | 3 (0.5) | 11 (0.7) | 2 (0.3) | 9 (1.1) | ||||||
| Chest pain, fainting, or dyspnea, No. (%) | 10 (0.7) | 3 (0.4) | 7 (1.1) | 24 (1.5) | 9 (1.2) | 15 (1.9) | ||||||
| Exhaustion, No. (%) | 6 (0.4) | 2 (0.3) | 4 (0.7) | 26 (1.6) | 5 (0.6) | 21 (2.6) | ||||||
| No reason given, No. (%) | 5 (0.3) | 2 (0.3) | 3 (0.5) | 8 (0.5) | 1 (0.1) | 7 (0.9) | ||||||
| Completed 400-meter walk, No. (%) | 1188 (80.3) | 709 (82.4) | 479 (77.4) | 1138 (72.2) | 616 (79.3) | 522 (65.3) | ||||||
| Very slow pace, >7 minutes, No. (%) | 48 (3.2) | 29 (3.4) | 19 (3.1) | 125 (7.9) | 53 (6.8) | 72 (9.0) | ||||||
| Slow pace, 5.5–7 minutes, No. (%) | 376 (25.4) | 193 (22.4) | 183 (29.6) | 510 (32.4) | 218 (28.1) | 292 (36.6) | ||||||
| Moderate pace, 4–5.5 minutes, No. (%) | 717 (48.4) | 450 (52.3) | 267 (43.1) | 498 (31.6) | 341 (43.9) | 157 (19.7) | ||||||
| Quick pace, ≤4 minutes, No. (%) | 47 (3.2) | 37 (4.3) | 10 (1.6) | 5 (0.3) | 4 (0.5) | 1 (0.1) | ||||||
| Unrecognized mobility deficits | 340 (22.9) | 181 (21.0) | 159 (25.7) | 563 (35.7) | 214 (27.5) | 349 (43.7) | ||||||
Note: Nonwalkers reported walking a total of <30 minutes in a typical week. Persons with unrecognized mobility deficits constitute those who were either excluded from the Long Distance Corridor Walk—that is, had a medical contraindication to exertion, were unable to complete the 400-meter walk, or needed >7 minutes to walk 400 meters as quickly as possible.
Table 3.
Relative Odds of Unrecognized Mobility Deficits in 70- to 79-Year-Old Men and Women by Walking Frequency and Selected Demographic and Behavioral Attributes.
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| Attributes | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Walks <30 min/wk | 1.30 (1.02–1.66) | 1.19 (0.93–1.53) | 2.04 (1.65–2.52) | 1.67 (1.34–2.09) | ||
| Age, y | 1.09 (1.05–1.14) | 1.11 (1.07–1.15) | ||||
| Black race | 1.72 (1.33–2.22) | 2.18 (1.74–2.74) | ||||
| Smoker | 1.45 (1.13–1.88) | 1.46 (1.15–1.87) | ||||
| Obese | 1.50 (1.12–2.00) | 1.96 (1.54–2.49) | ||||
Notes: Persons with unrecognized mobility deficits constitute those who were either excluded from the Long Distance Corridor Walk—that is, had a medical contraindication to exertion, were unable to complete the 400-meter walk, or needed >7 minutes to walk 400 meters as quickly as possible.
OR = odds ratio; CI = confidence interval.
Within 2 years, 21% and 34% of men and women met criteria for newly self-recognized mobility limitation by reporting difficulty walking one-quarter mile or climbing one flight of stairs at two consecutive semiannual contacts; 7% and 12% met criteria for mobility disability. Persons identified as having unrecognized deficits at baseline had higher rates of newly recognized limitation (40.0% vs 15.8% in men and 54.0% vs 23.6% in women; p <.001) and mobility disability (18.2% vs 3.7% in men and 23.1% vs 6.0% in women; p <.001) relative to those with no objective evidence of mobility deficits at baseline. The respective odds ratios and 95% confidence intervals for limitation and disability were 2.36 (1.75–3.18) and 4.02 (2.56–6.31) in men and 2.37 (1.85–3.04) and 2.93 (2.05–4.18) in women.
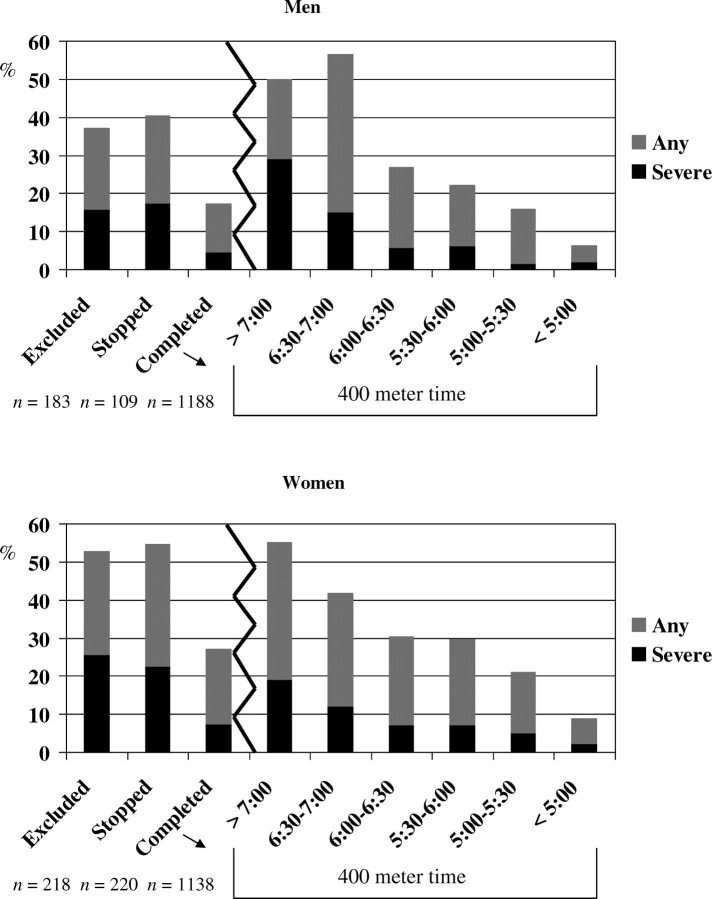
Figure 1 shows that, in both men and women, those excluded from attempting and those unable to complete the LDCW had much higher rates of newly recognized limitation than those completing the LDCW, but that among persons completing the LDCW, men needing at least 6 minutes and 30 seconds and women needing at least 7 minutes had greater or comparably high rates of newly recognized limitation. Even persons completing 400 m in 5 minutes and 30 seconds exhibited elevated risk. As shown in Table 4, both men and women attempting but not completing the LDCW or needing at least 7 minutes to walk 400 m were four times as likely to report newly self-recognized mobility limitation as those completing the LDCW. After accounting for demographic and behavioral factors, gait speed, and reported ease walking 1 mile, men and women unable to complete or performing poorly on the LDCW were 2.66 (1.79–3.94) and 2.28 (1.70–3.05) times more likely to have newly recognized limitations. Among those completing the LDCW, for each additional 30 seconds over 5 minutes needed to walk 400 m, men were 65% and women 37% more likely to develop mobility limitations after accounting for demographic, behavioral, and other functional attributes.
Figure 1.
Percentage of men and women developing newly recognized mobility limitation and severe limitation according to completion status for the Long Distance Corridor Walk and, among those completing the 400 m component, time to walk 400 m “as quickly as possible.” *Newly recognized mobility limitation is defined as two consecutive semiannual reports within 2 years of difficulty walking one-quarter mile or climbing one flight of stairs. Severe limitation constitutes reporting a lot of difficulty or inability to do either function
Table 4.
Relative Odds of Newly Recognized Mobility Limitation in 70- to 79-Year-Old Men and Women Associated With Inability to Complete or Poor Performance on the Long Distance Corridor Walk (LDCW) and Time to Walk 400 Meters.
| Relative Odds of Recognized Mobility Limitation in Test-Eligible Persons Completing Versus Not Completing or Performing Poorly on the LDCW |
|||||||
|---|---|---|---|---|---|---|---|
| Men (N = 1297) |
Women (N = 1358) |
||||||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||
| Did not complete or poor performance on the LDCW | 4.08 (2.86–5.80) | 2.66 (1.79–3.94) | 3.92 (3.04–5.07) | 2.28 (1.70–3.05) | |||
| Age, y | – | 1.04 (0.99–1.10) | – | 1.02 (0.97–1.06) | |||
| Black race | – | 0.95 (0.69–1.30) | – | 0.94 (0.71–1.24) | |||
| Walks < 30 min/wk | – | 1.64 (1.22–2.21) | – | 1.29 (0.99–1.67) | |||
| Current/recent smoker | – | 1.09 (0.79–1.49) | – | 1.11 (0.83–1.47) | |||
| Obese | – | 1.61 (1.15–2.25) | – | 1.77 (1.34–2.35) | |||
| Reports walking 1 mile is other than “very easy” | – | 2.43 (1.79–3.30) | – | 3.39 (2.51–4.58) | |||
| Gait speed < 1.0 m/s | – | 2.15 (1.44–3.20) | – | 1.33 (0.99–1.79) | |||
| Relative Odds of Recognized Mobility Limitation for Each Additional 30 Seconds Needed to Walk 400 Meters | |||||||
| Men (N = 1188) | Women (N = 1138) | ||||||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||
| Each 30 seconds over 5 minutes | 1.77 (1.59–1.96) | 1.65 (1.46–1.88) | 1.54 (1.41–1.67) | 1.37 (1.23–1.53) | |||
| Age, y | – | 1.00 (0.95–1.06) | – | 0.99 (0.94–1.04) | |||
| Black race | – | 0.80 (0.56–1.14) | – | 0.84 (0.61–1.15) | |||
| Walks < 30 min/wk | – | 1.41 (1.01–1.96) | – | 1.07 (0.79–1.43) | |||
| Current/recent smoker | – | 1.01 (0.72–1.43) | – | 0.95 (0.68–1.32) | |||
| Obese | – | 1.37 (0.94–2.01) | – | 1.65 (1.20–2.28) | |||
| Reports walking 1 mile is other than “very easy” | – | 1.87 (1.32–2.61) | – | 2.87 (2.07–4.00) | |||
| Gait speed < 1.0 m/s | – | 1.15 (0.71–1.86) | – | 0.96 (0.67–1.38) | |||
Notes: Newly recognized mobility limitation is defined as two consecutive semi-annual reports within 2 years of difficulty walking one-quarter mile or climbing one flight of stairs. Poor performance on the Long Distance Corridor Walk constitutes needing more than 7 minutes to walk 400 meters “as quickly as possible.”
OR = odds ratio; CI = confidence interval.
As evident from Table 4, both having a gait speed <1.0 m/s and reporting that walking 1 mile is other than very easy predicted development of newly self-recognized mobility limitation. To evaluate the added value of the LDCW we examined rates of newly self-recognized mobility limitation in participants who met neither of these conditions; that is, exhibited good mobility on less demanding measures. In these 739 men and 502 women, rates of newly self-recognized limitation in those unable to complete the LDCW or needing more than 5.5 minutes to walk 400 m versus those completing 400 m in <5.5 minutes were 20.1% versus 6.3% in men (p <.001) and 14.9% versus 9.2% in women (p =.048). Thus, it would appear for men in particular that endurance walk testing may be especially important in those who meet none of the usual criteria suggestive of mobility deficits.
Discussion
A substantial proportion of community-dwelling men and women in their 70s who reported no walking difficulty showed evidence of prevalent mobility deficits and/or impending limitation, readily ascertained through standardized administration of an endurance walk test. As nearly half did not routinely walk, it is not surprising that overall, 30% had unrecognized deficits and 27% developed self-recognized mobility limitation within 2 years; of these persons, one third had mobility disability. Rates were higher in particular subgroups. For instance, 48% of black women met criteria for unrecognized deficits and 42% had self-recognized limitation within 2 years. These data indicate a sizable population on the verge of meaningful mobility loss, many of whom appear to be unaware of their mobility deficits and risk status. Further, it is clear that standard questions about walking difficulty may be less sensitive or yield less accurate results in select subgroups (those who tend to have poorer health behaviors—smokers and obese persons, for instance).
Previously, we demonstrated the prognostic value of the LDCW for identifying prevalent subclinical cardiovascular disease (26) and all-cause and cardiovascular mortality, cardiovascular events and functional limitation over 4–6 years (27). Here we demonstrate the utility of test performance for identifying individuals with prevalent mobility deficits or impending limitation. The link between fitness and functional capacity is well established (24,28), but rarely has objectively measured fitness been applied to identification of covert or impending mobility limitations (29). Although findings apply to the LDCW as administered in the Health ABC study, other endurance walk tests, including treadmill-based protocols, may provide comparable prognostic information. Self-paced corridor walks however, may be more practical for older adults in both clinical and community settings (30–32), and the LDCW in particular encourages a near maximal effort in older ambulatory adults (19).
When sufficient time and/or space are unavailable, the multivariate analyses indicate that simply asking individuals whether walking 1 mile would be easy for them and/or administering a short walk test can aid identification of persons with covert mobility limitation (30). All three measures showed an independent association with newly self-recognized mobility limitation (Table 4), suggesting that each contributes a unique dimension of mobility status. Evaluating the sensitivity, specificity, and positive predictive value of these assessments for identifying impending mobility limitation we found for both men and women, reporting that walking 1 mile is other than very easy had the highest sensitivity (.68 and.84) but lowest specificity (.62 and.50) and positive predictive value (.33 and.47) whereas gait speed <1.0 m/s had the lowest sensitivity (.30 and.43) but highest specificity (.89 and.78). Poor LDCW performance exhibited intermediate sensitivity and specificity (.43 and.82 for men and.56 and.75 for women). Such statistics are influenced by the cutpoints selected, however. Using a more restrictive definition of poor performance on the LDCW, needing >6.5 minutes to complete 400 m, for instance, improves sensitivity to.53 and.64 with little diminution of specificity (.81 and.69). A more refined analysis extends beyond the scope of the current work. In sum, each measure is highly predictive of mobility deficits, yet all remain underutilized in clinical practice.
Some important limitations should be noted. First, because the LDCW requests participants to “walk as quickly as possible,” symptoms may arise from walking at a faster than customary pace, which would tend to overestimate prevalent unrecognized deficits. Nevertheless, the degree to which such symptoms indicate limited reserve capacity may also render the LDCW a more sensitive test of impending limitation. Second, due to safety concerns, participants were stopped when their test heart rate exceeded 135 beats per minute (accounting for 44% of those who stopped). Examining this group separately, we found that 14% and 38% of men and women developed newly recognized mobility limitation in contrast to 64% and 67% who stopped for other reasons (p <.001). Thus, stopping persons when their heart rate exceeded 135 beats per minute may have been overly cautious. By including such persons among “the stoppers,” we may have underestimated the true prognostic significance of inability to complete the LDCW. Last, we must acknowledge that test performance may have directly influenced participant discovery of existing walking difficulty. Insofar as such discovery may prompt remedial action, this may be an additional benefit of endurance walk testing.
Summary
Sedentary lifestyle and its consequences contribute not only to poor health and functional decline, but also to delayed recognition and possible treatment of functional deficits. Routine assessment of walking capacity, either by direct questioning of ability to walk distances or objective testing over short or long distances, is therefore necessary to identify persons most in need and likely to benefit from targeted habilitation efforts. Endurance walk tests such as the LDCW can greatly facilitate this process, particularly in persons who otherwise demonstrate good mobility. Given the potential to reverse or modify the functional deficits that underlie mobility difficulty (33–35), routine assessment of walking ability appears in order.
Acknowledgments
This research was supported by the Intramural Research Program of the National Institutes of Health, National Institute on Aging (NIA) and NIA contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106.
References
- 1. Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. [DOI] [PubMed] [Google Scholar]
- 2. Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Further evidence for the importance of subclinical functional limitation and subclinical disability assessment in gerontology and geriatrics. J Gerontol B Psychol Sci Soc Sci. 2005;60:146–151. [DOI] [PubMed] [Google Scholar]
- 3. Shumway-Cook A, Ciol MA, Yorkston KM, Hoffman JM, Chan L. Mobility limitations in the Medicare population: prevalence and sociodemographic and clinical correlates. J Am Geriatr Soc. 2005;53:1217–1221. [DOI] [PubMed] [Google Scholar]
- 4. National Center for Health Statistics, Data Warehouse on Trends in Health and Aging., Available at: http://www.cdc.gov/nchs/agingact.htm. Last accessed June, 2006.
- 5. Cavazzini C, Conti M, Bandinelli S, et al. Screening for poor performance of lower extremity in primary care: the Camucia Project. Aging Clin Exp Res. 2004;16:331–336. [DOI] [PubMed] [Google Scholar]
- 6. Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. [DOI] [PubMed] [Google Scholar]
- 7. Walsh JME, Pressman AR, Cauley JA, Browner WS. Predictors of physical activity in community-dwelling elderly white women. J Gen Intern Med. 2001;16:721–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Simonsick EM, Guralnik JM, Fried LP. Who walks? Factors associated with walking behavior in disabled older women with and without self-reported walking difficulty. J Am Geriatr Soc. 1999;47:672–680. [DOI] [PubMed] [Google Scholar]
- 9. Simonsick EM, Lafferty ME, Phillips CL, et al. Risk due to inactivity in physically capable older adults. Am J Public Health. 1993;83:1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brach JS, VanSwearingen JM, Newman AB, Kriska AM. Identifying early decline of physical function in community-dwelling older women: performance-based and self-report measures. Phys Ther. 2002;82:320–328. [PubMed] [Google Scholar]
- 11. Guralnik JM, Ferrucci L, Simonsick EM, Salive M, Wallace RB. Lower extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the Short Physical Performance Battery. J Gerontol Med Sci. 2000;55A:M221–M231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rantanen T, Guralnik JM, Ferrucci L, et al. Coimpairments as predictors of severe walking disability in older women. J Am Geriatr Soc. 2001;49:21–27. [DOI] [PubMed] [Google Scholar]
- 14. Cesari M, Kritchevsky SB, Penninx BWHJ, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition study. J Am Geriatr Soc. 2005;53:1675–1680. [DOI] [PubMed] [Google Scholar]
- 15. Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol Med Sci. 2001;56A:M644–M649. [DOI] [PubMed] [Google Scholar]
- 16. McDermott M, Guralnik JM, Albay M, Bandinelli S, Miniati B, Ferrucci L. Impairments of muscles and nerves associated with peripheral arterial disease and their relationship with lower extremity functioning: the InCHIANTI Study. J Am Geriatr Soc. 2004;52:405–410. [DOI] [PubMed] [Google Scholar]
- 17. Sayers SP, Guralnik JM, Newman AB, Brach JS, Fielding RA. Concordance and discordance between two measures of lower extremity function: 400 meter self-paced walk and SPPB. Aging Clin Exp Res. 2006;18:100–106. [DOI] [PubMed] [Google Scholar]
- 18. Macera CA, Ham SA, Yore MM, et al. Prevalence of physical activity in the United States: Behavioral Risk Factor Surveillance System, 2001. Prev Chronic Dis. 2005;2:A17. [PMC free article] [PubMed] [Google Scholar]
- 19. Simonsick EM, Montgomery PS, Newman AB, Bauer DC, Harris T. Measuring fitness in healthy older adults: the Health ABC Long Distance Corridor Walk. J Am Geriatr Soc. 2001;49:1544–1548. [DOI] [PubMed] [Google Scholar]
- 20. Simonsick EM, Fan E, Fleg JL. Estimating cardiorespiratory fitness in well-functioning older adults: treadmill validation of the Long Distance Corridor Walk. J Am Geriatr Soc. 2006;54:127–132. [DOI] [PubMed] [Google Scholar]
- 21. American College of Sports Medicine. Guidelines for Exercise Testing and Prescription, 5th Ed. Kenney WL, ed. Baltimore: Williams & Wilkins; 1995:269–287. [Google Scholar]
- 22. Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;137:153–156. [DOI] [PubMed] [Google Scholar]
- 23. Brach JS, Simonsick EM, Kritchevsky S, Yaffe K, Newman AB. The association between physical function and lifestyle activity and exercise in the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2004;52:502–509. [DOI] [PubMed] [Google Scholar]
- 24. Binder EF, Birge SJ, Spina R, et al. Peak aerobic power is an important component of physical performance in older women. J Gerontol Med Sci. 1999;54A:M353–M356. [DOI] [PubMed] [Google Scholar]
- 25. Guralnik JM, Simonsick EM, Ferrucci, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol Med Sci. 1994;49A:M85–M94. [DOI] [PubMed] [Google Scholar]
- 26. Newman AB, Haggerty CL, Kritchevsky SB, Nevitt MC, Simonsick EM, for the Health ABC Collaborative Research Group. Walking performance and cardiovascular response: associations with age and morbidity – The Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2003;58:715–720. [DOI] [PubMed] [Google Scholar]
- 27. Newman AB, Simonsick EM, Naydeck BL, et al. Association of Long-Distance Corridor Walk performance with mortality, cardiovascular disease, mobility limitation and disability. JAMA. 2006;295:2018–2026. [DOI] [PubMed] [Google Scholar]
- 28. Morey MC, Pieper CF, Cornoni-Huntley J. Is there a threshold between peak oxygen uptake and self-reported physical functioning in older adults? Med Sci Sports Exerc. 1998;30:1223–1239. [DOI] [PubMed] [Google Scholar]
- 29. Rolland YM, Cesari M, Miller ME, Penninx BW, Atkinson HH, Pahor M. Reliability of the 400-m usual-pace walk test as an assessment of mobility limitation in older adults. J Am Geriatr Soc. 2004;52:972–976. [DOI] [PubMed] [Google Scholar]
- 30. Hollenberg M, Ngo LH, Turner D, Tager IB. Treadmill exercise testing in an epidemiologic study of elderly subjects. J Gerontol Biol Sci. 1998;53A:B259–B267. [DOI] [PubMed] [Google Scholar]
- 31. Huggett DL, Connelly DM, Overend TJ. Maximal aerobic capacity testing of older adults: a critical review. J Gerontol A Biol Sci Med Sci. 2005;60:57–66. [DOI] [PubMed] [Google Scholar]
- 32. Wang CY, Olson SL, Protas EJ. Physical-performance tests to evaluate mobility disability in community-dwelling elders. J Aging Phys Act. 2005;13:184–197. [DOI] [PubMed] [Google Scholar]
- 33. Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Van Ness PH. A prehabilitation program for the prevention of functional decline: effect on higher-level physical function. Arch Phys Med Rehabil. 2004;85:1043–1049. [DOI] [PubMed] [Google Scholar]
- 34. Binder EF, Schechtman KB, Ehsani AA, et al. Effects of exercise training on frailty in community-dwelling older adults: results of a randomized, controlled trial. J Am Geriatr Soc. 2002;50:1921–1928. [DOI] [PubMed] [Google Scholar]
- 35. The LIFE study investigators. Effects of a physical activity intervention on measures of physical performance: results of the Lifestyle Interventions and Independence for Elders pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. [DOI] [PubMed] [Google Scholar]