Abstract
Purpose
The incidence of syphilitic infections continues to rise and represents a major public health concern, particularly in patients co-infected with human immunodeficiency virus (HIV). The infection has a multitude of clinical presentations and is often referred to as the ‘great imitator.’ We present a rare case of an isolated presumed syphilitic optic nerve gumma and characterize it using newer imaging modalities.
Observations
A 36-year-old HIV-positive man, compliant with treatment, presented with a five day history of decreased vision in the left eye. On examination his visual acuity was 20/30 with mild dyschromatopsia and an inferior altitudinal field defect in the left eye. Funduscopy demonstrated small cup to disc ratios bilaterally and a swollen and hyperemic left optic disc. Following five months of stable vision, the patient's vision in the left eye declined to 20/60, associated with diffuse visual field loss and continued swelling of the left optic disc. Subsequent magnetic resonance imaging with contrast demonstrated enhancement of the left optic nerve, and his serologies were positive for syphilis. Fluorescein angiography and optical coherence tomography were used to better characterize the lesion being most consistent with a syphilitic optic nerve gumma.
Conclusions and importance
Gummas of the central nervous system are a rare presentation of neurosyphilis and the last reported gumma of the optic nerve was in 1990. Such lesions have not been characterized using newer imaging modalities including optical coherence tomography and fluorescein angiography, both of which may assist in the diagnosis of this rare entity. With the increased prevalence of syphilis and remarkable response to therapy, syphilitic gummas should be considered in at-risk patients presenting with an optic neuropathy.
Keywords: Syphilis optic neuropathy
1. Introduction
Syphilitic infections are a major public health issue and the prevalence continues to rise, particularly in patients co-infected with human immunodeficiency virus (HIV).1 The infection can present in a myriad of ways and thus is often referred to as the ‘great imitator.’ Vision loss related to syphilis can result from uveitis, chorioretinitis, interstitial keratitis, optic neuropathy, retinitis, encephalitis and infarction.2, 3 In severe cases, syphilitic gummas can form as the body attempts to contain the infection. Gummas are a subtype of granuloma in which the infectious spirochetes are walled off and surrounded by inflammatory cells, fibroblasts and capillaries. Gummas of the optic nerve head are exceptionally rare with the last reported case published in 1990.4 To our knowledge, this rare entity has not been further imaged with modalities such as fluorescein angiography and optical coherence tomography (OCT). We describe the first case of a presumed optic nerve gumma based on its clinical, angiographic, and OCT features.
1.1. Case report
A 36-year-old HIV-positive man presented with 5 days of ‘looking through a fog’ in his left eye. He denied headache, ocular pain, trauma and pain with eye movement. His ocular history was notable only for myopia. His HIV infection was well controlled (on efavirenz-emtricitabine-tenofovir) with a normal CD4 count and undetectable viral load.
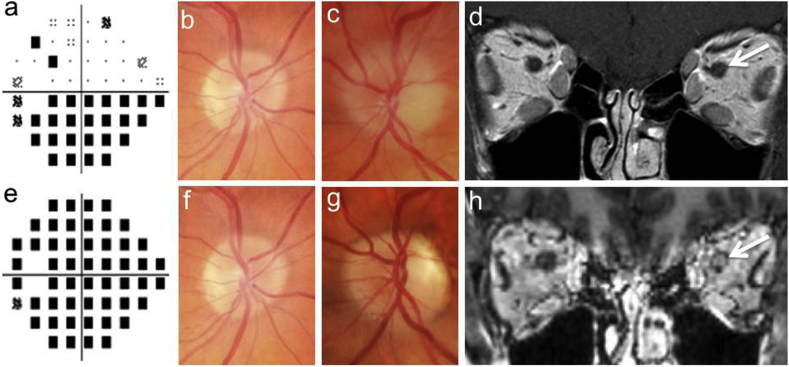
On examination his visual acuities were 20/20 OD and 20/30 OS. He had mild dyschromatopsia in the left eye (6/8 Ishihara plates) but his pupils were normal with no relative afferent pupillary defect (RAPD). Automated Humphrey visual field testing revealed a dense inferior altitudinal defect OS (Fig. 1a). Funduscopic examination revealed a normal optic disc OD with a small cup-to-disc ratio (Fig. 1b) and a swollen and hyperemic disc OS (Fig. 1c). Magnetic resonance imaging (MRI) of the brain and orbit was normal without optic nerve enhancement (Fig. 1d). The patient was initially diagnosed with non-arteritic anterior ischemic optic neuropathy (NAION).
Fig. 1.
Development of presumed left optic nerve head gumma over time. At initial presentation the patient had an inferior altitudinal defect on the pattern deviation of the automated Humphrey visual field (a) a hyperemic and swollen left optic disc (c) a normal right optic disc (b) and no signs of optic nerve enhancement on the coronal T1 post-contrast magnetic resonance imaging (MRI) (d). Five months later, the patient's visual field progressed (e), the left optic nerve head was elevated and hyperemic with superotemporal pallor (g) with the right optic nerve head remaining unchanged (f) and the MRI showed left optic nerve enhancement on the coronal T1 post-contrast BRAVO MRI (H).
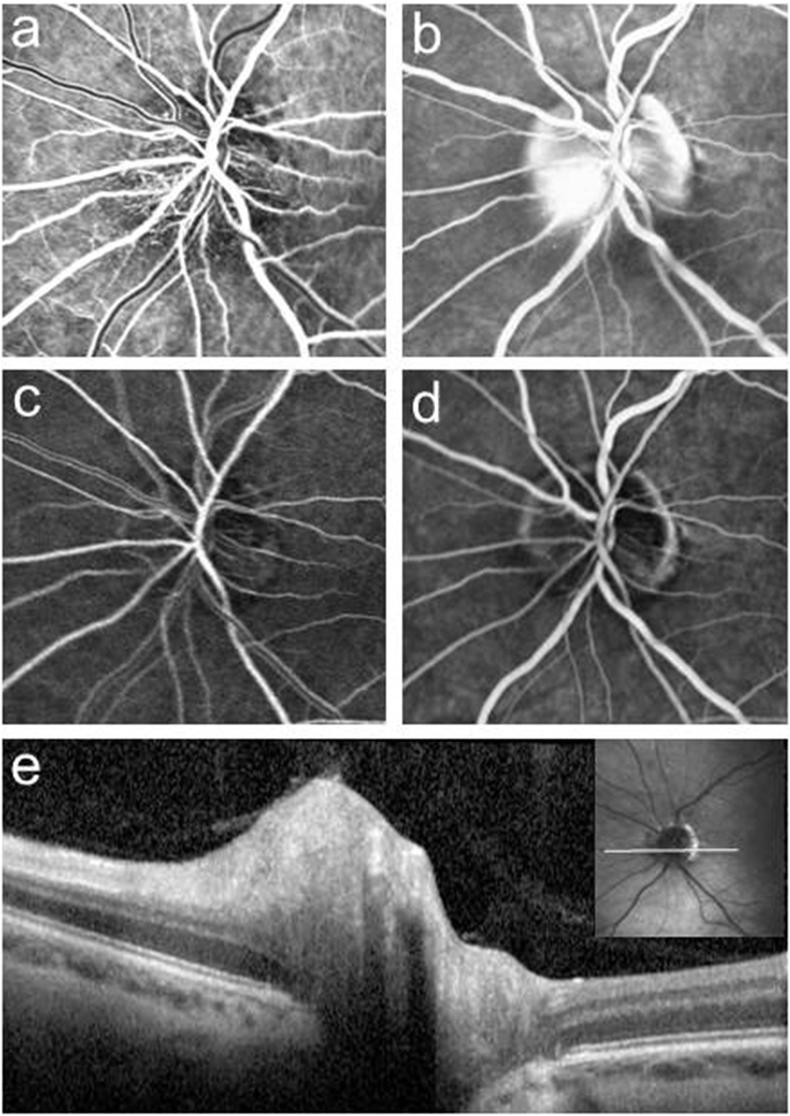
After five months of stable vision, the patient re-presented with five days of worsening vision OS. He was otherwise asymptomatic. A complete review of systems was negative. On exam he now had a visual acuity of 20/60 OS, a left RAPD, diffuse visual field loss (Fig. 1e) and an elevated, hyperemic disc with superotemporal pallor (Fig. 1g). Repeat MRI showed enhancement of the left optic nerve (Fig. 1h). Fluorescein angiography demonstrated a prominent focal nasal area of telangiectatic vessels with associated leakage corresponding to the area of disc elevation and hyperemia (Fig. 2a and b). OCT of that area demonstrated an elevated hyper-reflective heterogeneous lesion (Fig. 2e). A laboratory workup was initiated confirming the presence of syphilis (RPR 1:512, VDRL 1:2).
Fig. 2.
Fluorescein angiography and optical coherence tomography imaging of presumed left optic nerve head gumma. Early (a) and late (b) fluorescein angiography of the left optic nerve head gumma before treatment, demonstrating nasal telangiectatic vessels and late leakage. Early (c) and late (d) images after treatment, showing resolution. Optical coherence tomography of the affected area of the nerve clearly demonstrates the elevated gumma (e).
Upon further questioning the patient admitted to a prior history of syphilis in 2009 that was treated with intramuscular penicillin. The patient was diagnosed with a probable optic nerve gumma and treated with 14 days of IV penicillin. He refused lumbar puncture. Two weeks following treatment, his vision improved to 20/20 OS and his optic disc swelling and fluorescein angiographic findings resolved (Fig. 2c and d).
2. Discussion
Neurosyphilis is often diagnosed in asymptomatic patients who come to medical attention with cerebrospinal fluid serologic evidence of the disease without the presence of neurologic symptoms. The disease has increased in prevalence over the last two decades partly as a result of neurosyphilis being more recognized in patients co-infected with HIV.5 Syphilis involving the afferent visual system most commonly involves the intracranial optic nerve and chiasm due to either direct inflammation or secondarily as a result of basilar meningitis.4 Typically, syphilitic optic neuropathy can present as a perineuritis, retrobulbar neuritis or an optic neuritis with disc swelling (papillitis). It is often characterized by mild to moderate optic nerve swelling and may present with peripapillary hemorrhages and rarely venous engorgement.6, 7 Fluorescein angiography demonstrates diffusely increased disc fluorescence in late phases. Rarely, subtle telangiectatic vessels have been noted on the optic nerve head with late leakage.8
Gummas of the central nervous system are a rare presentation of neurosyphilis and are often misdiagnosed as other entities, particularly intracerebral malignancies.9 Gummas of the optic nerve are even less common, last reported in 1990 and prior to this by Koff in 1939.4, 10 Histopathology of these lesions dates back prior to 1910 when Verhoeff identified spirochetes within the gumma.11 Primary optic nerve gummas are not often considered an etiology for syphilitic optic neuropathy given the rarity of this presentation. However, when present, the affected optic disc has been described as looking fully swollen and at times, with neovasculariztion and refractile bodies.4
Due to this exceptionally uncommon presentation of neurosyphilis, the entity has not been described using newer ophthalmic imaging modalities. The optic disc appearance of our case is similar to that of prior reported anterior optic nerve gummas. Although initially thought to represent NAION, the patient's optic disc swelling persisted months after the development of his initial symptoms, contrary to what would be expected in ischemic optic neuropathy. Furthermore, the fluorescein pattern demonstrated prominent telangiectatic vessels with elevation of the lesion on OCT. This is similar to the pathologic features of previously described optic nerve gummas and the fluorescein characteristics are consistent with presumed retinochoroidal gummas.6, 12 Most importantly, our patient had a profound and complete response to IV penicillin, further supporting the syphilitic etiology of the lesion.
Ocular syphilis is an elusive entity and has a diverse clinical presentation. It is exceptionally important to consider this entity when evaluating visual dysfunction, particularly in patients with HIV-positivity, even with initially unremarkable orbital and cerebral imaging.13 Given the increasing prevalence of ocular syphilis, and the profound response to appropriate treatment, these lesions should be considered when confronted with an optic neuropathy in an at-risk patient.
Patient consent
Written patient consent to publish the report was obtained.
Funding
No funding or grant support.
Authorship
All authors attest that they met the current ICMJE criteria for authorship.
Conflict of interest
Nailyn Rasool, James Stefater and Dean Cestari have no financial disclosures. Dean Eliott has previously received honoraria from the following: Acucela, Alcon, Alimera, Allergan, Arctic, Avalanche, Biogen, Dutch Ophthalmic, MacuLogix, Neurotech, Ocata Therapeutics, Ophthotech, ReNeuron, Santen, Thrombogenics.
Acknowledgements
None.
References
- 1.(CDC) Center for Disease Control and Prevention . US Department of Health and Human Services; Atlanta: 2014. Sexually Transmitted Disease Surveillance. 2015. [Google Scholar]
- 2.Tamesis R.R., Foster C.S. Ocular syphilis. Ophthalmology. 1990;97:1281–1287. doi: 10.1016/s0161-6420(90)32419-3. [DOI] [PubMed] [Google Scholar]
- 3.Moradi A., Salek S., Daniel E. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334–343. doi: 10.1016/j.ajo.2014.10.030. e331. [DOI] [PubMed] [Google Scholar]
- 4.Smith J.L., Byrne S.F., Cambron C.R. Syphiloma/gumma of the optic nerve and human immunodeficiency virus seropositivity. J Clin Neuroophthalmol. 1990;10:175–184. [PubMed] [Google Scholar]
- 5.Centers for disease control and prevention department of STD prevention. sex Transm Dis Surveill. 2013:2014. [Google Scholar]
- 6.Browning D.J. Posterior segment manifestations of active ocular syphilis, their response to a neurosyphilis regimen of penicillin therapy, and the influence of human immunodeficiency virus status on response. Ophthalmology. 2000;107:2015–2023. doi: 10.1016/s0161-6420(00)00457-7. [DOI] [PubMed] [Google Scholar]
- 7.Prokosch V., Thanos S. Emerging syphilitic optic neuropathy: critical review and recommendations. Restor Neurol Neurosci. 2008;26:279–289. [PubMed] [Google Scholar]
- 8.Chao J.R., Khurana R.N., Fawzi A.A. Syphilis: reemergence of an old adversary. Ophthalmology. 2006;113:2074–2079. doi: 10.1016/j.ophtha.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 9.Darwish B.S., Fowler A., Ong M. Intracranial syphilitic gumma resembling malignant brain tumour. J Clin Neurosci. 2008;15:308–310. doi: 10.1016/j.jocn.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 10.Koff R. Gumma of the optic papilla. Am J Ophthalmol. 1939;22:663–665. [Google Scholar]
- 11.Verhoeff F.H. Ein fall von syphilom des optikus und der papille mit spirochatenbefund. Klin Monatsbl Augenheilkd. 1910;48:315–321. [Google Scholar]
- 12.Sigford D.K., Schaal S. Asymptomatic retinal gumma. JAMA Ophthalmol. 2015;133:355–357. doi: 10.1001/jamaophthalmol.2014.5232. [DOI] [PubMed] [Google Scholar]
- 13.Smith G.T., Goldmeier D., Migdal C. Neurosyphilis with optic neuritis: an update. Postgrad Med J. 2006;82:36–39. doi: 10.1136/pgmj.2004.020875. [DOI] [PMC free article] [PubMed] [Google Scholar]