Abstract
Purpose
To report a novel finding in a case of idiopathic recurrent branch retinal arterial occlusions.
Observations
We report our findings in a 31-year-old woman with an idiopathic recurrent branch retinal arterial occlusions (BRAOs) who was followed in our clinic for 16 years. Repeated fluorescein angiographies were performed to evaluate the idiopathic recurrent BRAOs. The findings showed multiple segmental arteriolar staining in the fundus. These staining were found at locations with and without branch retinal arterial occlusions. Repeated fluorescein angiography showed that these staining migrated toward the periphery. The speed of the migration of the staining was about 0.64 ± 0.22 mm/day with a range of 0.43–0.85 mm/day in the posterior pole of the eye. In each of the BRAO, the staining did not cause branch retinal arterial occlusions in the peripheral retina again.
Conclusions and importance
Segmental arteriolar staining that migrates towards the periphery may be a clue to the etiology of this disease process.
Keywords: Idiopathic recurrent branch retinal arterial occlusion, Segmental arteriolar fluorescein staining, Migration of segmental arteriolar fluorescein staining
1. Introduction
A recurrent idiopathic branch retinal arterial occlusions (BRAOs) are rare and are characterized by recurrent multiple BRAOs of unknown etiology. It can develop uni- or bilaterally in otherwise healthy patients who also have vestibuloauditory and transient sensorimotor symptoms.1, 2, 3, 4, 5 We have followed a patient with this disease for 16 years and found several new findings that might contribute to the etiology of the disease.
2. Case report
A 15-year-old young woman presented with an acute-onset scotoma in the left eye accompanied with tinnitus and hearing loss in both ears in 1998. She was healthy and not taking any medications. Her visual acuity was 20/20 in both eyes. Fundus examination showed ischemic retinal whitening, and fluorescein angiography (FA) showed BRAOs with multiple segmental arteriolar staining in the left eye. Two of these staining sites appeared to be the sites of BRAOs (Fig. 1 A–C). The fundus of the right eye was completely normal.
Fig. 1.
Color fundus photographs and fluorescein angiograms (FA) of a patient with recurrent idiopathic branch retinal arterial occlusions.
First episode. A: Color fundus photograph on the day of onset, B: Early phase of FA, C: Late phase FA.
Second episode. Color fundus photograph on the day of onset (D), on day 3 (F), and on day 11 (H) after the onset. Fluorescein angiograms on the day of onset (E), on day 3 (G), and on day 11 (I) after the onset. Note that the segmental arteriolar staining movse peripherally and then disappears. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Extensive systemic evaluations including hematologic, cardiovascular, and neurologic examinations revealed no abnormalities. The patient was treated with urokinase, prostaglandin E1, and hyperbaric oxygen therapy but the visual field defects remained.
Five years after the first episode, she presented again with a sudden development of a central scotoma in the right eye. Her visual acuity was counting finger at 30 cm OD and 20/20 OS. Fundus examination of the right eye revealed ischemic retinal whitening, and FA showed macular BRAOs with multiple segmental arteriolar staining around the optic disc. Three days later, a second FA was performed, and it showed that the arteriolar staining had moved peripherally and was weaker. Eleven days later, a third FA revealed that the perfusion was normal with no arteriolar staining (Fig. 1D–I). The visual acuity recovered to 20/100 OD.
Thereafter, BRAOs continued to recur even after she started taking aspirin, warfarin, and oral prednisone. FA were performed each time she complained of new visual field abnormalities or vision disorders to determine whether a BRAO was occurring. If a BRAO or arteriolar staining was found, FA were performed once every few days until the staining disappeared to check whether fluorescein staining caused further BRAOs. No complication from the repeated fluorescein angiography was observed. The total number of BRAOs was 10; 3 in the right eye and 7 in the left eye during the follow-up period of 16 years. Her visual field became smaller, and her latest visual acuity was 32/200 OD and 20/20 OS.
Repeated FA with the Optos 200Tx ultra-wide field imaging system (Optos, PLC, Dunfermline, Scotland) showed the characteristics of segmental branch retinal arteriolar staining. The segmental arteriolar staining at each episode resembled that of the previous episodes but they were present in different arterioles. They tended to occur at or around the optic disc but occasionally elsewhere in the fundus. Segmental arteriolar staining was found 4 to 8 times/year in either eye but were not cause a BRAO each time, although a BRAO could be present at some of the segmental staining sites.
The arteriolar staining migrated peripherally and usually split into two at the bifurcations of the arterioles (Fig. 2). The staining was not very obvious at the site of the occlusion (Fig. 1B, E, 1G). Examinations of the repeated fluorescein angiograms showed that the speed of the migration of the fluorescein branch arteriolar staining was about 0.64 ± 0.22 mm/day with a range of 0.43–0.85 mm/day in the posterior pole of the eye.
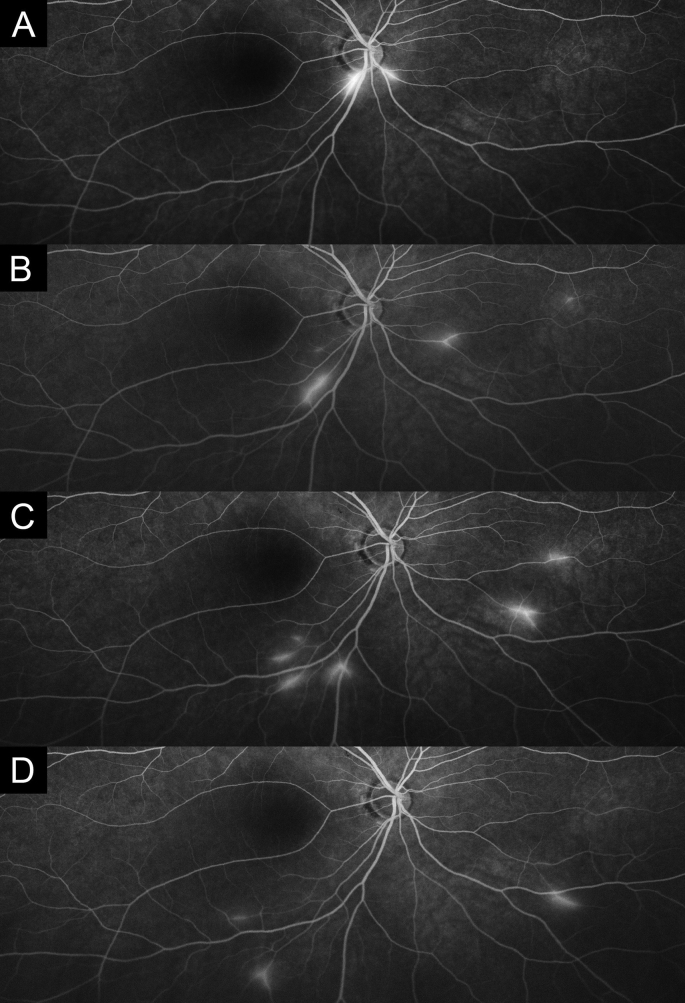
Fig. 2.
Optos fluorescein angiograms of one of repeated episodes. A: First examination. B: Five days from A. C: Ten days from A. D: Fourteen days from A.
Note that the segmental arteriolar staining moves to the periphery with mild leakage. The speed of the migration of the branch arteriolar staining was about 0.64 ± 0.22 mm/day with a range of 0.43–0.85 mm/day in the posterior pole of the eye.
3. Discussion
One of the characteristics of idiopathic recurrent BRAOs is segmental branch retinal arteriolar staining in the fluorescein angiograms.1, 2, 3, 4, 5 It is not known what causes this staining but vasculitis is the most likely cause. Because the speed of the migration of the fluorescein staining was much slower than the blood flow, Inflammatory cells or deposits of immunocomplexes may contribute to the vasculitis and the formation of thrombi. Eventually, the inflammatory cells or deposits of the immunocomplexes in the arterioles migrate within the arterioles. However, no treatment including steroid and anticoagulant seemed to reduce the frequency of the occlusions and segmental branch retinal arteriolar staining. The inflammatory hematological parameters such as C-reactive protein (CRP) are always within the normal range in these patients. Currently, this is the first study of the migration of the fluorescein staining in any kind of retinal disease, the clinical significance of this migration is unclear. However, a migration of segmental arteriolar fluorescein staining toward the periphery may be a clue to the etiology of the disease process.
In the repeated FAs, a BRAO was not observed in the peripheral retina once staining moved to the peripheral retina. It is not clear why staining that migrated to the periphery did not cause a BRAO. One of the reason may be the differences of the blood stream in the posterior pole and periphery. This may be related to the etiology of this disease. Further study is needed to elucidate this phenomenon.
One of the limitations of this study was that the FA examinations was performed only when the patient noticed changes in her visual condition. Thus, BRAO might have occurred during the period between the examinations, and the frequency of BRAO may have been more often than we found. However, because the visual symptoms were quite frequent, FA was performed at least once every 2 weeks. Therefore, the number of missed BRAOs was probably few. Another limitation is that continuous migration of fluorescein staining was not directly observed because longer continuous observation of fluorescein angiography is not possible. Fluorescein arteriolar staining tends to be found at arteriolar bifurcation, and there is a possibility that the speed of the migration can be different at the bifurcation and the straight segments of the arteries. Further studies are needed to determine how the fluorescein staining moves in the arteries.
4. Conclusions
Segmental arteriolar staining of the fluorescein angiograms is a characteristic findings of recurrent idiopathic branch retinal arterial occlusions. This staining migrated to the periphery after the onset. Because it is not known how this disease develops and what these stainings are, this report may be helpful not only for not only for the diagnosis of this vascular abnormality but also for determining the etiology of this abnormality.
Patient consent
The patient consented to publication of the case in writing.
Funding
This study was supported in part by Grant-in Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (16K11265 (YI)).
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Conflicts of interest
The authors have no financial disclosures.
Acknowledgements
The authors thank Professor Emeritus Duco Hamasaki of the Bascom Palmer Eye Institute for his critical discussion and final manuscript revision.
References
- 1.Gass J.D., Tiedeman J., Thomas M.A. Idiopathic recurrent branch retinal arterial occlusion. Ophthalmology. 1986;93:1148–1157. doi: 10.1016/s0161-6420(86)33600-5. [DOI] [PubMed] [Google Scholar]
- 2.Johnson M.W., Flynn H.W., Jr., Gass J.D. Idiopathic recurrent branch retinal arterial occlusion. Arch Ophthalmol. 1989;107:757. doi: 10.1001/archopht.1989.01070010775044. [DOI] [PubMed] [Google Scholar]
- 3.Johnson M.W., Thomley M.L., Huang S.S., Gass J.D. Idiopathic recurrent branch retinal arterial occlusion. natural history and laboratory evaluation. Ophthalmology. 1994;101:480–489. doi: 10.1016/s0161-6420(94)31309-1. [DOI] [PubMed] [Google Scholar]
- 4.Barak N., Ferencz J.R., Freund M., Mekori Y. Urticaria in idiopathic bilateral recurrent branch retinal arterial occlusion. Acta Ophthalmol Scand. 1997;75:107–108. doi: 10.1111/j.1600-0420.1997.tb00264.x. [DOI] [PubMed] [Google Scholar]
- 5.Trevino R., Pearlman R. Idiopathic recurrent branch retinal arterial occlusion in a young adult. Optom Vis Sci. 1998;75(1):11–16. doi: 10.1097/00006324-199801000-00019. [DOI] [PubMed] [Google Scholar]