Abstract
Purpose
To present an example of how close clinical monitoring of a patient with acute Horner syndrome from carotid artery dissection may be critical in reversing neurologic dysfunction.
Observations
A patient whose initial neuro-ophthalmic manifestation was Horner syndrome, but who evolved over 14 days to display transient monocular vision loss, ipsilateral ocular ischemic syndrome, and episodic contralateral hemiparesis. Digital subtraction angiography demonstrated progressive ipsilateral carotid occlusion with lack of collateral flow. The patient underwent stenting with rapid reversal of transient monocular visual loss and hemiparesis. Follow-up examination several months later confirmed complete resolution of all clinical abnormalities.
Conclusions and importance
This case displayed protracted evolution of ischemic manifestations following carotid artery dissection and their prompt reversal with stenting. This case emphasizes the value of close clinical attention to a patient with acute Horner syndrome because manifestations may appear more than 10 days after event onset that impel intervention for the dissection.
Keywords: Horner syndrome, Carotid artery dissection, Ischemic ocular syndrome, Hemiparesis, Carotid artery stenting
1. Introduction
Internal carotid artery dissection is a common cause of ischemic stroke in young patients and can be spontaneous or traumatic.1 Among the ophthalmic manifestations reported in the setting of internal carotid artery dissections are Horner syndrome, transient monocular vision loss, ischemic optic neuropathy, and central retinal artery occlusion.2 There has been one report of ocular ischemic syndrome (OIS), reflecting extreme compromise of the blood supply to the eye.3 We report a patient who developed a traumatic internal carotid artery dissection that evolved from causing a Horner syndrome to causing OIS and ipsilateral cerebral hypoperfusion, signaled by transient orthostatic monocular visual loss and contralateral hemiparesis. Stenting of the dissection promptly resolved all clinical manifestations.
2. Case report
A 50-year-old man fell 20 feet from a tree and sustained fractures of the left frontal sinus, T6, left iliac crest and left 12th rib. CT angiography disclosed a high cervical right internal carotid artery dissection with preservation of antegrade flow (Fig. 1 AB). Accordingly, he was treated conservatively with aspirin 325 mg/day.
Fig. 1.
Initial computed tomography angiogram (CTA) in axial projection (A) demonstrates a narrowed column of contrast in the high cervical right internal carotid artery (arrow) consistent with dissection. Corresponding maximum intensity projection (MIP) (B) demonstrates the narrowed arterial portion (arrows). Repeat CTA performed 12 days after the initial CTA in the axial projection (C) demonstrates interval worsening of the internal carotid artery dissection (arrow). Corresponding MIP (D) demonstrates apparent occlusion at the cervical-petrous junction (arrows).
Seven days later he noted that during physical therapy sessions he would have 1 h episodes of seeing colors and patterns with his right eye, followed by complete loss vision in that eye. Five days after onset of these provoked episodes, they began to occur at rest. Ophthalmological examination at that time (12 days after admission) revealed a pinhole near visual acuity of 20/20-3 in the right eye and 20/20 in the left eye. The right pupil measured 2 mm and the left pupil measured 4 mm in dim illumination, and both constricted briskly to direct light, but there was a relative afferent pupillary defect (RAPD) in the right eye, suggesting a right optic neuropathy. There was 2 mm of ptosis of the right upper eyelid. Intraocular pressures were 5 mmHg in the right eye and 9 mmHg in the left eye. Portable slit lamp examination disclosed no abnormalities of the anterior ocular segment. Fundus examination through dilated pupils revealed arteriolar narrowing and mid-peripheral intra-retinal hemorrhages in the right eye and no abnormalities in the left eye, consistent with a diagnosis of OIS. Instillation of apraclonidine 0.5% in both eyes showed reversal of anisocoria and a reduction in the right upper lid ptosis, confirming the presence of a right Horner syndrome.
Owing to new ocular ischemic manifestations, he underwent repeat CT angiography, performed 5 days after onset of the visual symptoms, which showed extension of the previously documented right internal carotid artery dissection into the intracranial compartment with progressive luminal narrowing and apparent occlusion at the skull base (Fig. 1C and D). Digital subtraction angiography confirmed severe stenosis (string sign) at the cervical-petrous junction. There was prolonged transit time and persistent antegrade flow which was slower than the flow in the ipsilateral external carotid artery (Fig. 2 A,C). Selective injection of the left internal carotid artery failed to demonstrate filling of the right middle cerebral artery (MCA) (Fig. 2D). However, the right MCA filled through a patent right posterior communicating artery during selective injection of the left vertebral artery. This pattern of slow antegrade flow and lack of sufficient collateral vessels was considered sufficient to explain the ocular ischemia.
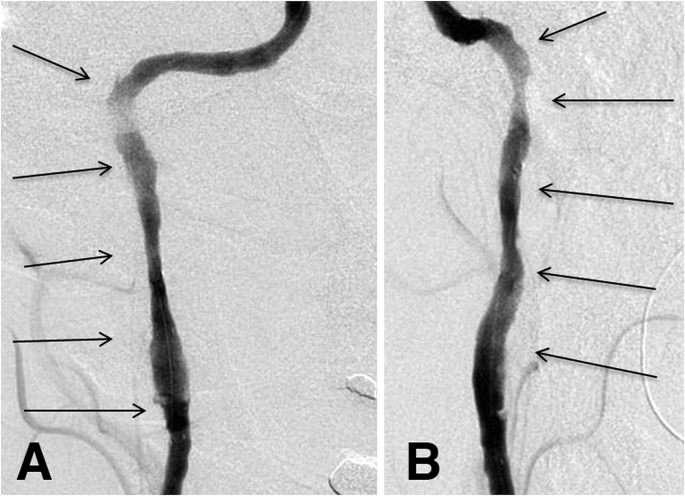
Fig. 2.
Catheter angiogram (early arterial phase) in the anteroposterior (A) and lateral (B) projections, performed on the same day as the repeat computed tomography angiogram (Fig. 1CD), demonstrates an irregular, narrowed column of contrast in the right internal carotid artery (solid arrows) consistent with dissection. There is normal opacification of right external carotid branches (dashed arrow). Anteroposterior projection in the late arterial phase (C) demonstrates washout of the contrast within the right external carotid artery (dashed arrow) but persistence of contrast within the right internal carotid artery (arrow head), indicating prolonged transit time compared to the right external carotid artery (dashed arrow). Left internal carotid artery angiogram in the anteroposterior projection (D) demonstrates normal left cerebral vascular opacification (solid arrow) but absence of cross filling of the right anterior and middle cerebral arteries. The lack of collateral flow partly explains why a critical stenosis of the right internal carotid artery might have led to enough cerebral ischemia to cause transient contralateral hemiparesis.
Two days after the digital angiogram, the patient reported left arm and leg weakness provoked by standing. These additional symptoms prompted a diagnosis of critically impaired right cerebro-ocular perfusion. Therefore, he underwent Neuroform (Stryker, Kalamazoo, Michigan) stenting of the right internal carotid artery (Fig. 3A and B). All symptoms resolved over the next 2 days.
Fig. 3.
Right internal carotid angiogram in anteroposterior (A) and lateral (B) projections performed after placement of three Neuroform stents within the right internal carotid artery demonstrates substantial improvement in caliber and flow within the carotid artery (arrows).
Ophthalmologic examination performed 4 months after stenting disclosed normal visual acuity in both eyes, a mild right afferent pupil defect, and a persistent right Horner syndrome. The retinal vasculature was of normal caliber in both eyes and the retinal hemorrhages had resolved. The persistent optic neuropathy was attributed to blunt forehead trauma. The patient reported no further episodes of extremity weakness and neurologic examination was normal.(see Fig. 4)
Fig. 4.
Time line of the patient’s clinical and radiologic events.
3. Discussion
Our patient experienced a traumatic carotid dissection that evolved over a 14-day period from causing Horner syndrome to causing ipsilateral transient monocular vision loss, retinal hemorrhages, low intraocular pressure, and to episodic contralateral hemiparesis. OIS in the setting of internal carotid artery dissection has been previously reported in a single case of spontaneous internal carotid artery dissection but the patient in that report had neovascularization of the iris, indicating a longer duration of ischemia than in our patient.4 The interval from the time of the dissection to the development and discovery of ocular manifestations, which included transient monocular vision loss, could not be determined. Thus, our case is unusual in displaying prolonged evolution of ischemic manifestations. Although 60% of patients with internal carotid artery dissection present with such manifestations, they rarely experience evolution after receiving antiplatelet therapy or anticoagulation.5 A report of 80 dissection cases, of which 64 were spontaneous and 16 were traumatic, found that nearly 90% of completed strokes occurred within 7 days of the clinical manifestations signaling the dissection.6 Our report is also notable for including a digital angiogram that accounted for the episodic cerebral hemispheric dysfunction by showing progressive ipsilateral carotid artery occlusion and limited collateralization to the right anterior and middle cerebral arteries. Finally, our case is novel in demonstrating rapid reversal of manifestations following stenting of the dissection and follow-up examination months later that confirmed resolution of ischemia.
We acknowledge that most patients with cervicocranial dissections are adequately managed for stroke prevention with antiplatelet therapy or anticoagulation and do not require stenting.7, 8 However, carotid stenting is becoming an accepted treatment for those rare patients with carotid artery dissection who have failed medical management, as evidenced by the development of ischemic manifestations after having been adequately anticoagulated.9, 10 In a series of 26 patients, Kadkhodayan et al.9 found stenting to be safe and effective in reducing vessel stenosis. Risks associated with the procedure include bleeding, hematoma, myocardial infraction, stroke, stent malfunction or occlusion and even death. In that study,9 eventual stent occlusion and death occurred in 6.9% of patients. Smaller series have reported similarly promising results.10
We have described a patient with a traumatic internal carotid artery dissection who progressed from Horner syndrome to OIS to reversible cerebral ischemia despite medical management with antiplatelet therapy and subsequently underwent stenting with rapid resolution of all ischemic manifestations. This case highlights the importance of close monitoring of patients with known carotid dissection for symptoms which may indicate progression of the dissection and potential need for endovascular intervention.
Patient consent
Consent to publish this case was obtained orally from the patient. This report does not contain any personal identifying information.
Funding
No funding or grant support.
Disclosures
The authors (DLA, BP, AS, JDT) have no financial disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Conflict of interest
None. The authors (DLA, BP, AS, JDT) have no conflict of interest.
Acknowledgments
None.
References
- 1.Patel R.R., Adam R., Maldjian C., Lincoln C.M., Yuen A., Arneja A. Cervical carotid artery dissection: current review of diagnosis and treatment. Cardiol Rev. 2012;20:145–152. doi: 10.1097/CRD.0b013e318247cd15. [DOI] [PubMed] [Google Scholar]
- 2.Biousse V., Touboul P.J., D'Anglejan-Chatillon J., Lévy C., Schaison M., Bousser M.G. Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol. 1998;126:565–577. doi: 10.1016/s0002-9394(98)00136-6. [DOI] [PubMed] [Google Scholar]
- 3.Mendrinos E., Machinis T.G., Pournaras C.J. Ocular ischemic syndrome. Surv Ophthalmol. 2010;55:2–34. doi: 10.1016/j.survophthal.2009.02.024. [DOI] [PubMed] [Google Scholar]
- 4.Duker J.S., Belmont J.B. Ocular ischemic syndrome secondary to carotid artery dissection. Am J Ophthalmol. 1988;106:750–752. doi: 10.1016/0002-9394(88)90721-0. [DOI] [PubMed] [Google Scholar]
- 5.Lee V.H., Brown R.D., Jr., Mandrekar J.N., Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809. doi: 10.1212/01.wnl.0000244486.30455.71. [DOI] [PubMed] [Google Scholar]
- 6.Biousse V., D'Anglejean-Chatillon J., Touboul P.J., Amarenco P., Bousser M.G. Time course of symptoms in extracranial carotid artery dissections. Stroke. 1995;26:235–239. doi: 10.1161/01.str.26.2.235. [DOI] [PubMed] [Google Scholar]
- 7.Schievink W.I. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344:898–906. doi: 10.1056/NEJM200103223441206. [DOI] [PubMed] [Google Scholar]
- 8.CADISS trial investigators. Markus H.S., Hayter E., Levi C., Feldman A., Venables G., Norris J. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015;44:361–367. doi: 10.1016/S1474-4422(15)70018-9. [DOI] [PubMed] [Google Scholar]
- 9.Kadkhodayan Y., Jeck D.T., Moran C.J., Derdeyn C.P., Cross D.T. Angioplasty and stenting in carotid dissection with or without associated pseudoaneurysm. AJNR Am J Neuroradiol. 2005;99:2328–2335. [PMC free article] [PubMed] [Google Scholar]
- 10.Ansari S.A., Thompson B.G., Gemmete J.J., Gandhi D. Endovascular treatment of distal cervical and intracranial dissections with the neuroform stent. Neurosurgery. 2008;62:636. doi: 10.1227/01.NEU.0000311350.25281.6B. [DOI] [PubMed] [Google Scholar]