Abstract
Purpose
Spasm of the near reflex (SNR) is a triad of miosis, excess accommodation and excess convergence. Primary SNR is most often functional in origin We aim to highlight the clinical features which distinguish primary convergence from other conditions with a similar presentation but more sinister underlying aetiology, for example bilateral abducens nerve palsy.
Observations
There is a paucity of published data on SNR, in particular diagnostic criteria and treatment. We report a case of SNR of functional origin in an otherwise healthy young female and discuss the clinical features that differentiate this condition from similar conditions with underlying neurological origin.
Conclusions and importance
SNR is predominantly a clinical diagnosis, and often leads to patients undergoing unnecessary investigations and sometimes treatment. Recognising the salient features that differentiate it could potentially avoid this.
Keywords: Spasm of the near reflex, Pseudo-abducens nerve palsy, Miosis, Excess accommodation, Pseudomyopia
1. Introduction
The near reflex is the action of the eye for adjustment to fixate on a near object. The reflex is a triad which consists of accommodation, convergence and miosis. Spasm of the near reflex (SNR) is when this triad persists when the patient is not fixating on a near object. Patients present with blurred vision, diplopia and asthenopia and on examination with often have an alternating convergent strabismus, abduction deficit and pseudomyopia. The underlying aetiology is functional in the majority of cases a and accurate and prompt diagnosis can sometimes avoid unnecessary investigations and treatment.
2. Case report
We report the case of a 28-year-old woman who presented to the Neurology Department of Beaumont Hospital on the 7th July 2015 complaining of a one day history of sudden onset horizontal binocular diplopia, which was worse for distance with associated headache. Background ocular history, she was a low myope (−1.75 OD, −1.25 OS). Otherwise, her ocular and medical history was unremarkable and she was not taking any regular medications and had no history of recent trauma. Of note, she was currently in the process of moving home.
On examination, visual acuity was 6/6 OU with the above correction. Cover testing revealed a moderate left convergent strabismus and constant limited abduction of her left eye, autrorefraction showed −1.75/−0.25 OD, −1.25/−0.75 OS which was unchanged on cycloplegic refraction. Ophthalmological and neurological exam were otherwise normal. Working diagnosis was isolated left abducens nerve palsy and she was admitted under the Neurology team for further investigation. CT brain and MRI brain followed by MRI pituitary were all normal. All laboratory investigations were normal which included anti Acetylcholine receptor antibodies. Lumbar puncture opening pressure was normal, 10.5 cm water (H2O) with normal CSF analysis.
She was fitted with plano glasses with unilateral occlusion of right eye which controlled diplopia initially. On the 12th July her symptoms worsened. She developed blurred vision in left eye and intermittent but worsening diplopia and bilateral abduction deficits on examination (Fig. 1), representing likely progression to bilateral abducens nerve palsy. She underwent further MRI Brain and MRI C-Spine which were both normal. A Tensilon Test to out rule myasthenia gravis was also considered however was not carried out and she was commenced on IV Methylprednisolone by the Neurology team, 1 g per day for five consecutive days however no improvement in symptoms was noted following treatment.
Fig. 1.

Extraocular movements showing right eye (A) and left eye (B) abduction deficit.
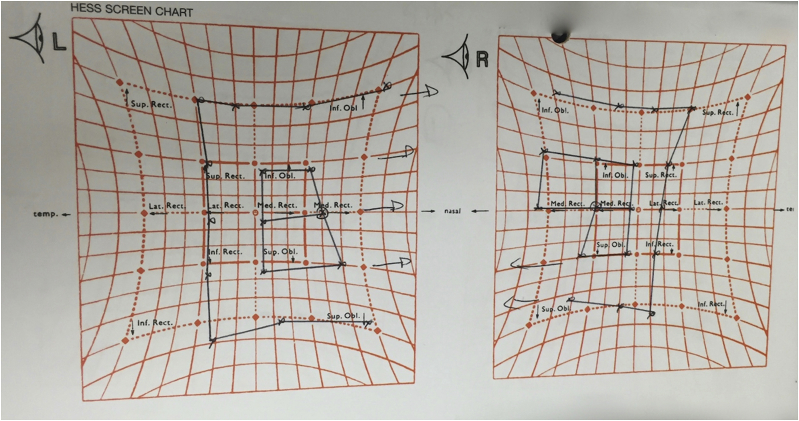
She was again seen in Ophthalmology clinic. Cover testing showed alternating convergent strabismus and abduction deficit in right and left eyes. Hess chart showed under action of the left and right lateral recti and over action of the left and right medial which is consistent with a bilateral abducens nerve palsy (Fig. 2).
Fig. 2.
Hess chart. Hess chart showed under action of the left and right lateral recti and over action of the left and right medial, which is consistent with a bilateral abducens nerve palsy.
However, she could abduct to beyond the midline with each eye tested separately (Fig. 3). She also had marked pupillary constriction on attempted abduction of either eye. There may also be nystagmus in the each eye when adducting on attempted lateral gaze. Salient examination findings are demonstrated (Video 1). She was diagnosed with likely convergence spasm, reassured and continued with occlusion of right eye. She was discharged from clinic, at four week follow up she showed a marked improvement in abduction and by three-month follow-up the deficit had resolved completely and she had full range of extraocular movements.
Fig. 3.

Abduction beyond midline: separate eye testing. Extraocular movements showing abduction beyond the midline with the right (A) and left (B) eye tested separately.
Supplementary video related to this chapter can be found at http://dx.doi.org/10.1016/j.ajoc.2017.01.006.
The following is the supplementary data related to this chapter:
1
3. Discussion
3.1. Background and clinical presentation
Spasm of the near reflex is a collection of findings which appears as a clinical spectrum. The typical presentation of SNR is a history of intermittent diplopia and asthenopia. Cover testing often reveals an alternating esotropia with miosis on attempted abduction. Abduction may appear restricted but a full range of extraocular movements can be demonstrated with each eye tested separately. Pseudo myopia may be seen which is eliminated on cycloplegic refraction. One of the earliest published reports of SNR was by Fitzgerald1 in 1884 describes a patient with sudden onset of myopia with acute spasm of accommodation.
3.2. Aetiology
SNR may be primary or acquired. Primary generally affects young women who are otherwise well, is associated with uncorrected hypermetropia and is often psychogenic in origin. These patients may have a background of psychiatric diagnosis or careful history may uncover trigger factors.
Acquired convergence spasm is based on the neuroanatomic location of the three areas involved in the near reflex, the cerebral cortex, the pretectum of the midbrain and the oculomotor nuclear complex and is seen in neurological diseases such as dorsal midbrain syndrome, disease at the diencephalic-mesencephalic junction also called thalamic esotropia, Wernicke-Korsakoff Syndrome, and posterior fossa lesions, such as cerebellar disease and Arnold-Chiari malformation.2
3.3. Diagnosis
The diagnosis of SNR is largely clinical and key learning points from this case are how to differentiate primary SNR from other neurological signs. A history of episodic diplopia with normal conjugate eye movements and intermittent blurred vision is suggestive. SNR may mimic bilateral abducens nerve palsy; however, pupil size will be normal, no new refractive error and consistent restriction of abduction with abducens nerve palsy.
The vestibule-ocular reflex (VOR) and absence of optokinetic nystagmus can help differentiate from acquired brainstem causes of SNR. In comatose patients the VOR can be used to test if brainstem eye movement pathways are intact. The oculocephalic reflex, a form of the VOR can be tested, once the cervical spine has been cleared, by holding the eyes open and rotating the head from side to side or up and down. The reflex is present if the eyes move in the opposite direction of the head. Voluntary eye movements may mask the reflex in conscious patients. To test the VOR reflex in a conscious patient you ask the patient to maintain fixation on a central target such as the examiner's nose. With a nuclear or infranuclear lesion such as a restrictive myopathy the eyes will move with the head. With normal function or in a supranuclear lesion they eyes will move in the opposite direction to the head to maintain fixation on the target, demonstrating a positive VOR.
Adduction nystagmus on lateral gaze, as demonstrated here can be seen in internuclear ophthalmoplegia (INO) of abduction, or reverse INO so this would be included in your differential diagnosis. INO of abduction is a rare horizontal gaze palsy that can be unilateral or bilateral where the patient exhibits abduction restriction and contralateral adduction nystagmus, the reverse of a typical INO.3 INO of abduction is can be caused by a lesion along the horizontal gaze pathway but lesion localization is highly debated. The most likely causes are stroke, demyelinating disease, neoplasm and myasthenia gravis.
3.4. Management
Management of primary convergence spasm with underlying neurologic disorder outruled is largely conservative and is based on symptom control. Reassurance should not be underestimated. Convergence exercises can be used with the aim to ‘break the cycle’ of spasm and uniocular occlusion for relief of diplopia. Cycloplegic eye drops such as cyclopentolate 1% have been used with limited success. One drawback is that they blur vision. This can be overcome somewhat by the use of bifocal glasses. Cogan and Freese3 reported that while Atropine provided and immediate effect it did not produce a long-term cure. Hyun et al.4, reported early resolution of convergence spasm over a two-month period with the use of S Sertraline 25mg PO, and Diazepam 2mg PO. These were being used to treat childhood emotional disorder. Logically, treating the underlying psychological disorder is likely to alleviate the spasm attacks. One study by Merino et al.5 used botulinum toxin to the medial rectus. It produced an improvement in symptoms but the patient did develop a consecutive exotropia and the spasm relapsed after eight months requiring further injection. A consensus on the most appropriate treatment has not been reached. Our case report shows a complete resolution with conservative management and reassurance for good prognosis on resolution.
4. Conclusion
Griffin et al.6 reported patients with primary NRS who underwent intracranial surgery and another patient who underwent several strabismus surgeries. Baseline neuroimaging is often appropriate in these cases. However once acquired causes are outruled, symptomatic relief and management of underlying psychogenic causes are the mainstay of treatment. Probing patients in the history for psychological triggers or stressors is important. The patient in our case was in the process of quite a stressful house move which may have been a contributing factor.
4.1. Patient consent
Written consent was obtained from this patient to publish her case details including images and video recording.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Conflict of interest
The following authors have no financial disclosures: MR, CB, PL.
Acknowledgements
None.
References
- 1.Fitzgerald C.E. Acute spasm of accommodation. Trans Ophthalmol Soc U K. 1884;4:311–315. [Google Scholar]
- 2.Kaski D., Bronstein A.M., Edwards M.J. Stone J. Cranial functional (psychogenic) movement disorders. Lancet Neurol. 2015;14:1196–1205. doi: 10.1016/S1474-4422(15)00226-4. [DOI] [PubMed] [Google Scholar]
- 3.Cogan D.G., Freese C.G. Spasm of the near reflex. Arch Opthalmol. 1955;54:752–759. doi: 10.1001/archopht.1955.00930020758020. [DOI] [PubMed] [Google Scholar]
- 4.Hyun H.J., Chung U.S., Chun B.Y. Early resolution of convergence spasm following the addition of antipsychotic medication. Korean J Ophthalmol. 2011;25:66–68. doi: 10.3341/kjo.2011.25.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merino P., Rojas P., Gomez de Liano P., Iglesia G. Spasm of the near reflex. Treatment with botulinum toxin. Arch Soc espanola Oftalmol. 2015;90:244–246. doi: 10.1016/j.oftal.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Griffin J.F., Wray S.H., Anderson D.P. Misdiagnosis of spasm of the near reflex. Neurology. 1976;26:1018–1020. doi: 10.1212/wnl.26.11.1018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1