Abstract
Purpose
Hypopyon in the eye is an alarming sign. A case of tuberculous uveitis which presented with pigmented hypopyon has been described. The aim of this paper is to report pigmented hypopyon, a rare presentation of tuberculous uveitis in a diabetic patient.
Observations
A 42-year-old patient with diabetes with a known history of miliary tuberculosis, on anti-tubercular therapy since two months presented with complaints of pain and redness followed by diminution of vision in the right eye since one month. Visual acuity was counting fingers close to face in right eye. Anterior chamber (AC) showed grade 4 cells and flare with a pigmented hypopyon measuring two mm. Fundus details were not made out. B scan revealed increased choroidal thickness with moderate vitritis. Routine blood counts revealed leucopenia and anemia suggestive of an immunosuppressed state. AC tap analysis was not helpful in diagnosis initially. Patient was lost to follow up and presented one month later with three - fourth of AC having hypopyon. AC wash was done and the AC sample evaluation revealed acid fast bacilli. Polymerase chain reaction results confirmed it to be Mycobacterium tuberculosis.
Conclusions and importance
Tuberculous anterior uveitis thus presenting as pigmented hypopyon is very rare and can cause diagnostic difficulties. High index of suspicion in tuberculosis endemic areas is a must for a prompt diagnosis. A possible association between immunosuppression and pigmented hypopyon may exist and needs to be studied further.
Keywords: Tuberculous anterior uveitis, Pigmented hypopyon, Miliary tuberculosis, Hypopyon uveitis, Immunosuppression
1. Introduction
Hypopyon is the sediment of whie blood cells forming in the dependent part of the anterior chamber (AC). It may be associated with intraocular inflammation, infection, malignancy (as pseudo hypopyon) or keratitis. Tuberculosis (TB) causing pigmented hypopyon is quite rare and has been reported only once by Rathinam et al.1 However as TB could be diagnosed only after culture, there might have been a delay in starting ATT in their case and the eye had to be enucleated. We report a similar case of pigmented tubercular hypopyon which could be diagnosed with polymerase chain reaction (PCR).
2. Case report
A 42-year-old South Indian male presented to a uvea clinic with a history of fever since 2 months, pain and redness in right eye (RE) since 1 month followed by diminution of vision RE since 15 days. He gave history of low grade fever, weight loss and malaise, more in the evenings, which was not accompanied with any chills and rigors since 2 months. He had consulted a local physician and was diagnosed to have miliary tuberculosis and diabetes mellitus. He was being treated with anti-tubercular therapy (ATT) and oral hypoglycemics for the same. There was no history of using oral rifabutin. He had no history of ocular trauma, surgery or injections, joint pains, oral or genital ulcers, skin disorders, hypertension or any high-risk sexual behaviour.
On examination, his best-corrected vision was counting fingers close to face (CFCF) in RE and 20/20 in left eye (LE). His intraocular pressures were normal in both eyes. Anterior segment examination of RE showed circumciliary congestion with corneal haze and medium sized pigmented keratic precipitates. AC showed an immobile hypopyon measuring 2 mm in size. Iris was muddy with multiple diffuse iris nodules. A thin fibrinous membrane was present over the pupil causing a seclusio pupillae with 360° posterior synechiae and a dull fundal glow. Relative afferent pupillary defect (RAPD) could have been assessed through the consentual reflex but was erroneously not checked. Fundus details (RE) could not be made out due to anterior segment findings. LE anterior segment was within normal limits. Fundus (LE) showed microaneurysms at the fovea suggestive of mild non-proliferative diabetic retinopathy (NPDR). B scan (RE) showed few to moderate number of low reflective dot echoes which were more in the anterior vitreous suggestive of moderate vitritis. Retina was attached throughout while choroid was diffusely thickened with a peripapillary choroidal thickness of 1.8 mm. Clinically in RE endogenous (fungal) endophthalmitis or panuveitis was suspected.
Blood investigation showed elevated erythrocyte sedimentation rate (46 mm at first hour), anemia and leucopenia with normal renal profile suggestive of some underlying immunosuppression. Serum ELISA for HIV was negative. HLA B51 and HLA B27 were negative. Mantoux was negative. Patient underwent AC tap for Gram, Potassium hydroxide (KOH), Calcoflour and Ziehl- Neelsen (ZN) staining; culture for bacteria and fungus and PCR for eubacteria, panfungal and Propionibacterium acnes genomes. Gram stain showed few pus cells and plenty of uveal pigments but no bacteria were seen. KOH, calcofluor and ZN staining were all negative. PCR was negative for eubacteria, panfungal and P.acnes genomes. Culture showed no growth of any bacteria and fungus. The patient refused admission due to personal reasons related to his low socioeconomic status. He was advised 1 hourly prednisolone acetate and moxifloxacin eye drops, atropine eye drops three times a day and to review in three days. However, he developed TB meningitis and was lost to follow-up.
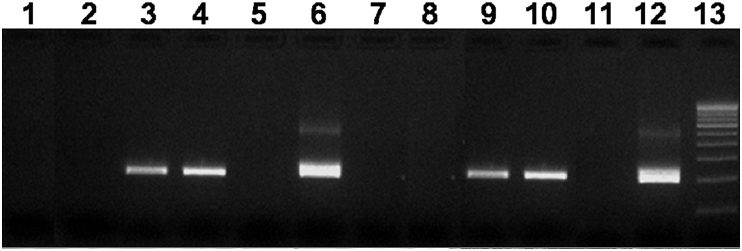
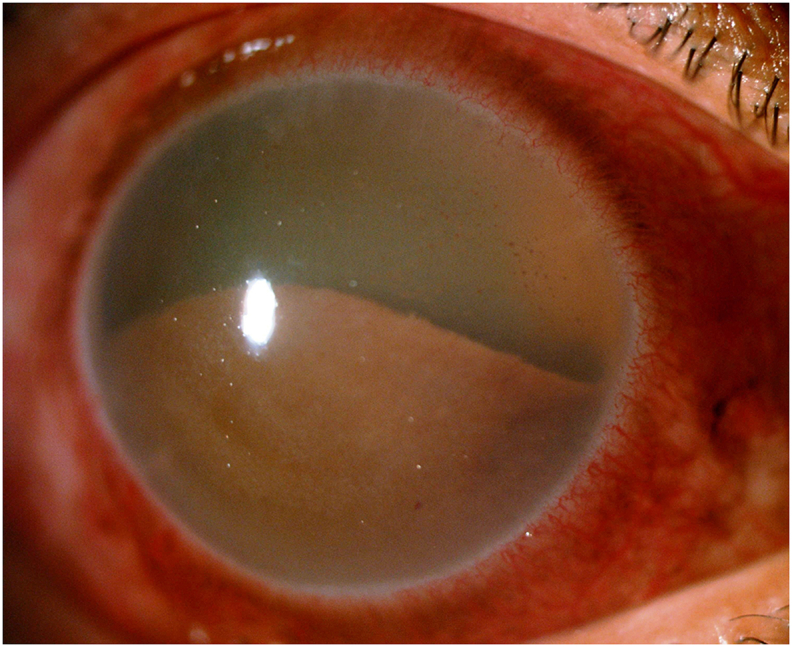
He presented after one month with a further drop in vision to hand movements in RE. RE showed an organized brownish hypopyon filling three - fourths of the AC with grade 4 cells and flare (Fig. 1). Other anterior segment and fundus details were not clear. Red glow was absent. B scan findings were similar to the previous scan with no evidence of any intraocular mass lesion. Patient underwent AC wash with intracameral 0.1 ml moxifloxacin (Vigamox®-Alcon Laboratories, Inc., Fort Worth, TX, USA). AC tap was sent for Gram, KOH and acid fast staining, cytological examination, PCR for MPB64 and IS6110 region of M tuberculosis genome and routine culture. Gram stain showed plenty of pus cells and uveal pigments with no bacteria. KOH and calcoflour stains did not reveal fungus. ZN staining was positive suggestive of acid fast bacilli. The presence of M tuberculosis was confirmed by positive PCR for MPB64 and IS6110 region of M tuberculosis genome (Fig. 2). Culture showed no growth of any bacteria and fungi. Cytology showed numerous neutrophils, necrotic cells and uveal pigments. Diagnosis of tuberculous panuveitis was made. As the patient was not responding to standard ATT, multi-drug resistant tuberculosis was suspected and the patient was referred to pulmonologist. Clearance for starting oral steroids was also sought. Topical treatment was continued as previously and he was advised review in 2 days. However, the patient has been lost to follow up again.
Fig. 1.
Right eye slit lamp photograph – A brownish pigmented hypopyon was seen filling 1/2–3/4th the anterior chamber with circum ciliary congestion and muddy iris. Rest of the details were not clear.
Fig. 2.
Positive polymerase chain reaction for Mycobacterium tuberculosis. Lane 1: Negative Control 2 for Mycobacterium Protein B 64 (MPB 64) gene, Lane 2: Negative Control 1 for MPB 64, Lane 3: Aqueous Aspirate – Vision Research Foundation (VRF) 2961/14 Positive for MPB 64, Lane 4: Aqueous Wash – VRF 2960/14 Positive for MPB 64, Lane 5: Aqueous Aspirate – Negative for MPB 64, Lane 6: Positive Control for MPB 64, Lane 7: Negative Control 2 for Insertion Sequence 6110 (IS 6110), Lane 8: Negative Control 1 for IS 6110, Lane 9: Aqueous Aspirate – VRF 2961/14 positive for IS 6110, Lane 10: Aqueous Wash – VRF 2960/14 Positive for MPB 64, Lane 11: Aqueous Aspirate – Negative for IS 6110, Lane 12: Positive Control for IS 6110, Lane 13: Molecular Weight – 100 base pair (bp) ladder.
3. Discussion
Blood-streaked or dark pigmented hypopyon is found in melanoma.2 Pigmented hypopyon is not common and has been rarely reported with Listeria monocytogenes 3or Serratia 4endogenous endophthalmitis. Serratia marcescens has been reported to cause both pink and dark hypopyon.5 Tuberculosis (TB) can have a varied presentation.6 Hypopyon is not common in tuberculous uveitis7 and pigmented hypopyon is very rare.1 Only one case of pigmented tuberculous hypopyon has been reported earlier by Rathinam et al.1 In our case, as the patient was a diabetic, we clinically suspected him to have endogenous endophthalmitis. As hypopyon is not a usual presentation for ocular TB7 and the patient was already on ATT, we erroneously overlooked the possibility of TB. Hence PCR for TB was unfortunately not ordered during the initial AC tap, due to inability of the patient to cover the cost of this test, and a chance for early diagnosis was probably missed. However, in the case of Rathinam et al., where the diagnosis could be confirmed only post enucleation, in our case, PCR of the AC wash sample helped in an in vivo diagnosis.
The cause of dark hypopyon is supposed to be dispersion of melanin from necrotic iris.3 In both our case and the case by Rathinam et al.,1 necrotic iris and melanin pigments were present in the AC sample, suggesting a common pathogenesis for pigmented hypopyon. A common feature in all these reported cases was immuosuppression.1, 3, 4, 5 It may be speculated that a deficient immune status predisposes to uveal tissue necrosis and pigment dispersion, resulting in a pigmented hypopyon.
4. Conclusion
Our case highlights that apart from Listeria, Serratia endophthalmitis and intraocular tumors, TB must also be considered in the differential diagnosis in a case of hypopyon, pigmented or not, especially in endemic areas. PCR for TB, at an early stage will be helpful to salvage such eyes. Noting a dark hypopyon in an immunosuppressed patient, may thus aid in diagnostic and therapeutic decisions.
Patient consent
Consent to publish the case report could not be obtained as the patient was lost to follow-up. This report does not contain any personal information that could identify the patient.
Funding
No funding or grant support.
Conflict of interest
The authors have no financial disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Rathinam S.R., Rao N.A. Tuberculous intraocular infection presenting with pigmented hypopyon: a clinicopathological case report. Br J Ophthalmol. 2004;88:721–722. doi: 10.1136/bjo.2003.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albert D.M., Lahav M., Troczynski E., Bahr R. Black hypopyon: report of two cases. Albr Von Graefes Arch Klin Exp Ophthalmol. 1975;193:81–94. doi: 10.1007/BF00410528. [DOI] [PubMed] [Google Scholar]
- 3.Eliott D., O'Brien T.P., Green W.R. Elevated intraocular pressure, pigment dispersion and dark hypopyon in endogenous endophthalmitis from Listeria monocytogenes. Surv Ophthalmol. 1992;37:117–124. doi: 10.1016/0039-6257(92)90074-4. [DOI] [PubMed] [Google Scholar]
- 4.Al Hazzaa S.A., Tabbara K.F., Gammon J.A. Pink hypopyon: a sign of Serratia marcescens endophthalmitis. Br J Ophthalmol. 1992;76:764–765. doi: 10.1136/bjo.76.12.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Equi R.A., Green W.R. Endogenous Serratia marcescens endophthalmitis with dark hypopyon: case report and review. Surv Ophthalmol. 2001;46:259–268. doi: 10.1016/s0039-6257(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 6.Gupta V., Gupta A., Rao N.A. Intraocular tuberculosis—an update. Surv Ophthalmol. 2007;52:561–587. doi: 10.1016/j.survophthal.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Chatziralli I.P., Keryttopoulos P., Papazisis L., Moschos M.M. Hypopyon in the context of tuberculous uveitis. Clin Exp Optom. 2012;95:241–243. doi: 10.1111/j.1444-0938.2011.00680.x. [DOI] [PubMed] [Google Scholar]