Abstract
Purpose
To describe the appearance of the superficial and deep retinal capillary plexi in three patients with fovea plana of differing severity using spectral-domain optical coherence tomography angiography (OCTA).
Observations
In the first case of grade 1 fovea plana (a patient with 20/25 vision), OCTA showed an orderly branching pattern of vessels from the superficial and deep retinal plexi extending to the center of the fovea. The second case of grade 3 fovea plana (20/30 vision) showed some disruption of the orderly vascular pattern with small caliber vessels from both superficial and deep layers densely covering the fovea center. Case 3 represented a patient with grade 4 fovea plana associated with PAX6 mutation and poor visual acuity. OCTA revealed a disorganized pattern of large and small caliber vessels from the superficial capillary network extending into the center of the fovea.
Conclusions and importance
Previously available imaging modalities were unable to specifically target different layers of the retinal vasculature. Using OCTA we have been able to show progressive changes in the vascular pattern in the deep and superficial retinal layers of patients with different grades of fovea plana. This novel imaging technique may play a role in the classification and assessment of patients with fovea plana.
Keywords: Fovea plana, Optical coherence tomography, Optical coherence tomography angiography, PAX6 mutation
1. Introduction
Fovea plana is a term first described by Marmor et al., in 2008.1 It describes the anatomic lack of a foveal pit, which can be associated with variable visual acuity.1 Fovea plana occurs secondary to disruption of the development of the fovea and has been reported in cases of ocular albinism and in conjunction with PAX6 gene mutations.2, 3 Thomas et al.4 proposed a structural grading system for fovea plana based on the stages of foveal development, namely displacement of inner retinal cells towards the periphery (extrusion of plexiform layers and deepening of the foveal pit), migration of cone photoreceptors towards the fovea center (represented by outer nuclear layer (ONL) widening) and finally, specialization of cone photoreceptors (represented on optical coherence tomography (OCT) by outer segment lengthening). The grading system was then correlated with visual acuity such that Grade 1 (the mildest form) was associated with better visual acuity and Grade 4 with worse visual prognosis. The characteristic imaging findings associated with this condition include an absent foveal pit on OCT.1 The inner retinal layer remains uniform in thickness through the center of the macula and the ONL can display central widening. Fluorescein angiography (FA) has demonstrated vessels that cross the fovea center.1
It is known that the retinal microcirculation is comprised of multiple vascular layers,5, 6 of which the superficial and deep capillary plexi are most commonly differentiated for characterizing pathology. However, vessels visualized using FA correspond to the superficial plexus only. OCT angiography (OCTA) is a new, non-invasive technique that images retinal vessels based on flow characteristics and has the ability to produce high resolution images of both the deep and superficial retinal capillary networks.7 The superficial capillary plexus as visualized using OCTA includes vasculature from the nerve fiber layer and ganglion cell layer while the deep capillary plexus includes both the intermediate and deep inner retinal vasculature.6 This technique has already been used in the characterization of many retinal diseases.8 This case series reports three cases each with a different structural grading of fovea plana with corresponding OCTA images, clearly showing the deep and superficial capillary networks and their involvement in this condition.
2. Findings
2.1. Case 1
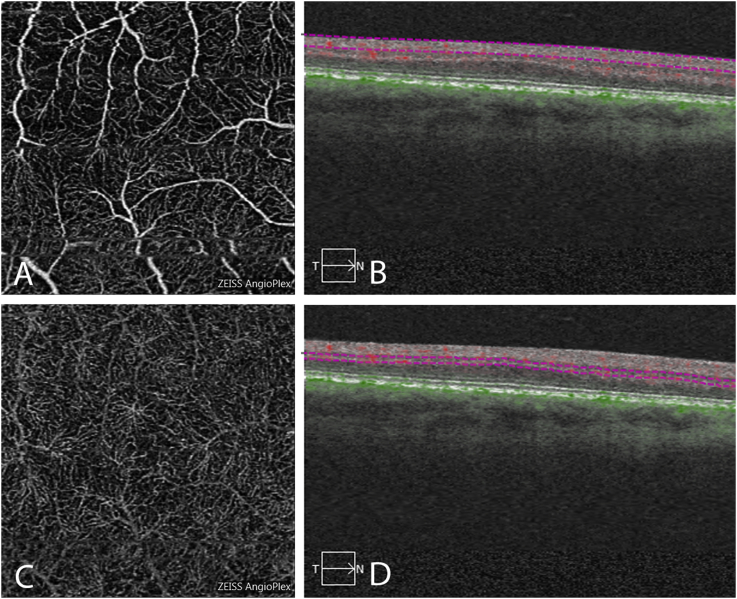
A 26-year-old female presented for retinal examination. She had a history of right amblyopia diagnosed during childhood, that had failed patching therapy. She reported no other past medical history. Her best-corrected visual acuity (BCVA) was 20/40 in her right eye and 20/25 in her left eye. Intraocular pressure was within normal limits. Examination of the external eye and orbit, and anterior segment were unremarkable. Dilated fundus examination revealed a blunted foveal reflex bilaterally with no clinical evidence of edema. Spectral-domain OCT (SD-OCT Carl Zeiss Meditec, Dublin, CA) showed a blunted foveal contour bilaterally and characteristic widening of the ONL centrally. Slight lengthening of the outer segment could also be visualized. These features can be appreciated on b-scan images from the left eye shown in Fig. 1. There was no evidence of intra-retinal edema. OCTA was performed using an investigational OCTA prototype (Carl Zeiss Meditec, Dublin, CA) under Stanford University Institutional Review Board approval. Written, informed consent was obtained from all patients. Manual segmentation was performed such that the inner plexiform layer (IPL)/inner nuclear layer (INL) border made up the outer boundary of the superficial layer and the IPL/INL and INL/outer plexiform layer (OPL) borders encompassed the deep layer. OCTA showed small capillaries from the superficial and deep retinal plexus crossing the midline, resulting in an absent foveal avascular zone (FAZ) (Fig. 1). This case is consistent with Grade 1 disease according to the grading system proposed by Thomas et al.4 as the three key features of normal development have been achieved at least partially (centrifugal displacement of inner retinal layers with foveal pit formation remains minimal, though present). The visual acuity of the patient described in this case (20/25) was also consistent with Grade 1 disease.
Fig. 1.
OCTA fields of view showing superficial and deep retinal capillaries (Case 1). Images from the left eye are shown. The right eye showed similar findings and is not presented. A: 3 × 3 mm optical coherence tomography angiography (OCTA) of the superficial capillary plexus. The small caliber superficial retinal capillaries are seen crossing the foveal center, with increased intercapillary spacing centrally. B: Corresponding b-scan highlighting the level of the superficial retinal OCTA (purple dashed line). A blunted foveal contour and widening of the outer nuclear layer centrally are seen. C: 3 × 3 mm OCTA of the deep capillary plexus. The deep retinal vessels extend into the fovea center with reduced density centrally. D: Corresponding b-scan highlighting the level of the deep retinal OCTA (purple dashed line). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.2. Case 2
A 55-year-old male with a history of type 2 diabetes mellitus presented for retinal review. He reported never having 20/20 vision. At the time of review, BCVA was 20/30 bilaterally. IOP was within normal limits and anterior segment exam was unremarkable. Dilated fundus exam revealed an absent foveal reflex. There was no diabetic retinopathy present. SD-OCT was absent for a foveal depression bilaterally and the ONL was widened centrally (Fig. 2). There was no evidence of macular edema. OCTA (with manual segmentation as described previously) showed a haphazard arrangement of retinal vessels from both superficial and deep capillary plexi extending into the central macula (Fig. 2). The larger caliber superficial vessels did not cross the foveal center. There is some motion artifact noted. This case represents grade 3 disease with widening of the cone outer segment represented by ONL widening at the fovea.4
Fig. 2.
OCTA fields of view showing superficial and deep retinal capillaries (Case 2). Images from the right eye are shown. The left eye showed similar findings and is not presented. A: 3 × 3 mm optical coherence tomography angiography (OCTA) of the superficial capillary plexus. The normal orderly branching pattern is disrupted. The superficial retinal vessels are seen crossing the fovea center. B: Corresponding b-scan highlighting the level of the superficial retinal OCTA (purple dashed line). There is no foveal depression present. Widening of the outer nuclear layer centrally is seen. C: 3 × 3 mm OCTA of the deep capillary plexus. The deep retinal vessels are seen crossing the fovea center. D: Corresponding b-scan highlighting the level of the deep retinal OCTA image (purple dashed line). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.3. Case 3
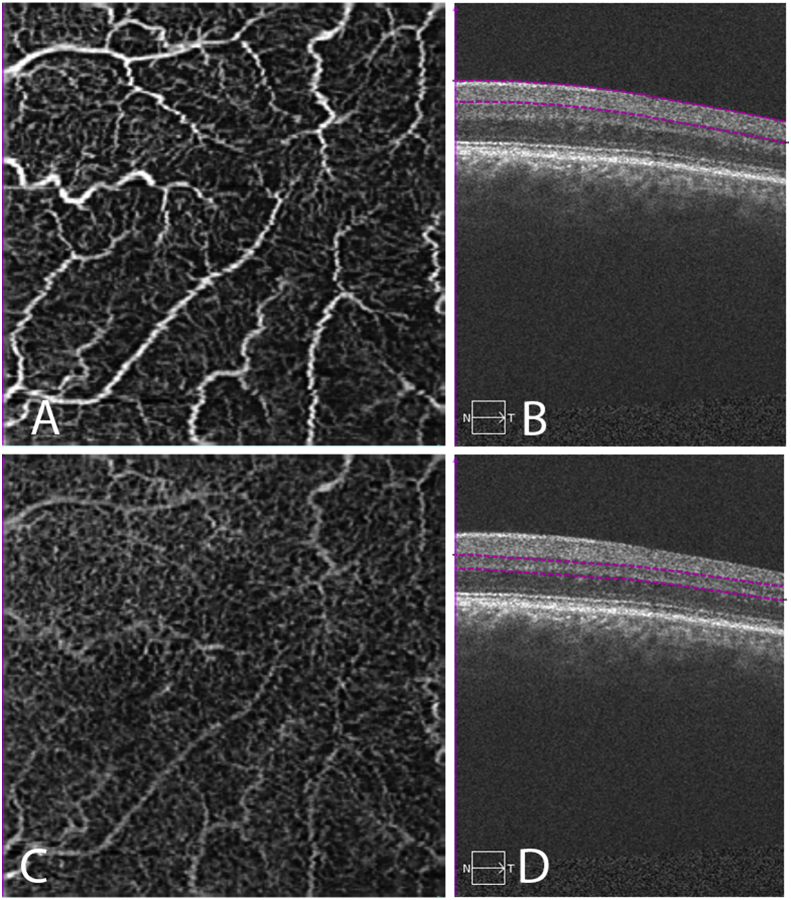
A 46-year-old male presented with longstanding decreased vision. He had a known history of nystagmus since birth and fovea plana associated with a PAX6 mutation. His past medical history included hyperlipidaemia and hypertension for which he was pharmacologically managed with amlodipine and pravastatin. BCVA at presentation was 20/150 in the right eye and 20/100 in the left eye. There was full extraocular motility, with pendular nystagmus bilaterally. Anterior segment exam showed bilateral trans-illumination defects. Dilated fundus examination showed blunted foveal reflexes, with no associated edema present in either eye. Cross-sectional SD-OCT showed no evidence of a foveal contour and the ONL was uniformly thickened across the fovea (Fig. 3). OCTA (with manual segmentation as described previously) revealed large vessels from the superficial layer and densely arranged finer vessels from the deep capillary network extending into the center of the fovea (Fig. 3). There is motion and projection artifact noted, particularly affecting the deep vascular plexus. Multifocal electroretinogram demonstrated decreased amplitudes in the central fovea consistent with mild to moderate central macular dysfunction. This case correlated with Grade 4 disease where none of the developmental processes of the fovea have occurred and the retina resembles that of the parafovea. Visual acuity was poor in this case as predicted by the grading system.4
Fig. 3.
OCTA fields of view showing superficial and deep retinal capillaries (Case 3). Images from the left eye are shown. The right eye showed similar findings and is not presented. A: 3 × 3 mm optical coherence tomography angiography (OCTA) of the superficial capillary plexus. The vasculature is distributed in a haphazard arrangement. Both large and small caliber superficial retinal vessels are seen crossing the foveal center. B: Corresponding b-scan highlighting the level of the superficial retinal OCTA (purple dashed line). The foveal contour is absent and widening of the outer nuclear layer centrally is not seen. C: 3 × 3 mm OCTA of the deep capillary plexus. The deep retinal vessels are seen crossing the foveal center with uniform density. D: Corresponding b-scan highlighting the level of the deep retinal OCTA (purple dashed line). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
This report has identified three patients with fovea plana who present with differing arrangements of vasculature in the superficial and deep capillary plexi. Dolz-Marco et al.9 recently published a case series of 3 cases of fovea plana with normal visual function, showing the absence of or markedly reduced FAZ in both deep and superficial vascular plexi in these idiopathic cases. To our knowledge the current report is the first time that cases of foveal plana with associated visual impairment have been reported in the literature.
Looking at the three cases presented here, Case 1 had the most complete foveal development. The microvasculature was seen to be uniformly laid out with larger vessels radiating towards, but not crossing the fovea center. Small caliber vessels of both superficial and deep retinal vascular layers did cross the fovea center. Of all three cases, this pattern is most consistent with the vascular arrangement surrounding the normally formed fovea.10 However, in the normal macula the superficial capillaries approach the FAZ more closely than the deep capillaries, with vessels from neither layer crossing the fovea center.10 The second case of Grade 3 severity, showed a haphazardly arranged radial pattern of the large retinal vessels. The smaller capillaries in the deep layer appeared to be distributed with uniform density across the macula. The final case demonstrating the most severe form of the disease showed both small and large caliber vessels crossing the center of the macula, and the branching pattern of the superficial plexus appeared severely disrupted. From these findings, we propose that there is progressive vessel disorganization at the fovea with more severe grades of foveal plana. Furthermore, subjective evaluation of the images suggests that there may be increased vascular density at the would-be fovea with increased disease severity and worse visual acuity. The software used for OCTA imaging did not have the capability of measuring vascular density in these cases, however this would be interesting to determine in future.
Marmor et al.1 determined that cone specialization at the fovea can be preserved in patients with fovea plana, allowing for intact vision despite the lack of foveal pit and a FAZ. Given the limited number of patients in this case series, the functional implications of our findings could not be investigated in detail. However, the trends seen from imaging these three cases with OCTA suggests that the architecture of central macular vessels may play a role in the functional capacity of the foveal cones. Further exploration is warranted to determine whether the vascular density at the central macula in the superficial and deep capillary plexi has any affect on cone function and visual outcomes.
4. Conclusions
This report presents OCTA images of patients with fovea plana of differing severity. Using OCTA we identified variations in the vascular architecture with increasing disorganization of the branching pattern of these vessels at the center of the macula in the superficial capillary layer. This novel imaging technique may play a role in the classification and assessment of patients with fovea plana.
5. Patient consent
The OCTA device was a prototype and the Stanford University Institutional Review Board approved the use of the device for this study. The patients provided written consent for imaging and publication of personal identifying information including medical record details and OCT imaging.
Conflicts of interest
None.
References
- 1.Marmor M.F., Choi S.S., Zawadzki R.J., Werner J.S. Visual insignificance of the foveal pit: reassessment of foveal hypoplasia as fovea plana. Arch Ophthalmol. 2008;126(7):907–913. doi: 10.1001/archopht.126.7.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meyer C.H., Lapolice D.J., Freedman S.F. Foveal hypoplasia in oculocutaneous albinism demonstrated by optical coherence tomography. Am J Ophthalmol. 2002;133(3):409–410. doi: 10.1016/s0002-9394(01)01326-5. [DOI] [PubMed] [Google Scholar]
- 3.Thomas S., Thomas M.G., Andrews C. Autosomal-dominant nystagmus, foveal hypoplasia and presenile cataract associated with a novel PAX6 mutation. Eur J Hum Genet. 2014;22(3):344–349. doi: 10.1038/ejhg.2013.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas M.G., Kumar A., Mohammad S. Structural grading of foveal hypoplasia using spectral-domain optical coherence tomography : a predictor of visual acuity? Ophthalmology. 2011;118(8):1653–1660. doi: 10.1016/j.ophtha.2011.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snodderly D.M., Weinhaus R.S., Choi J.C. Neural-vascular relationships in central retina of macaque monkeys (Macaca fascicularis) J Neurosci. 1992;12(4):1169–1193. doi: 10.1523/JNEUROSCI.12-04-01169.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dansingani K.K., Inoue M., Engelbert M., Freund K.B. Optical coherence tomographic angiography shows reduced deep capillary flow in paracentral acute middle maculopathy. Eye. 2015;29(12):1620–1624. doi: 10.1038/eye.2015.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spaide R.F., Klancnik J.M., Cooney M.J. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133(1):45–50. doi: 10.1001/jamaophthalmol.2014.3616. [DOI] [PubMed] [Google Scholar]
- 8.de Carlo T.E., Romano A., Waheed N.K., Duker J.S. A review of optical coherence tomography angiography (OCTA) Int J Retina Vitreous. 2015;1(1) doi: 10.1186/s40942-015-0005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolz-Marco R., Phasukkijwatana N., Sarraf D., Freund K.B. Optical coherence tomography angiography in fovea plana. Ophthalmic Surg Lasers Imaging Retina. 2016;47(7) doi: 10.3928/23258160-20160707-10. [DOI] [PubMed] [Google Scholar]
- 10.Foreman D.M., Bagley S., Moore J., Ireland G.W., McLeod D., Boulton M.E. Three dimensional analysis of the retinal vasculature using immunofluorescent staining and confocal laser scanning miscroscopy. Br J Ophthalmol. 1996;80(3):246–251. doi: 10.1136/bjo.80.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]