Abstract
Background
While medication adherence is essential for the secondary prevention of stroke, it is often sub-optimal, and can be compromised by cognitive impairment. This study aimed to systematically review and meta-analyse the association between cognitive impairment and medication non-adherence in stroke.
Methods
A systematic literature search of longitudinal and cross-sectional studies of adults with any stroke type, which reported on the association between any measure of non-adherence and cognitive impairment, was carried out according to PRISMA guidelines. Odds ratios and 95% confidence intervals were the primary measure of effect. Risk of bias was assessed using the Cochrane Bias Methods Group's Tool to Assess Risk of Bias in Cohort Studies, with evidence quality assessed according to the GRADE approach. We conducted sensitivity analyses according to measure of cognitive impairment, measure of medication adherence, population, risk of bias and adjustment for covariates. The protocol was registered with PROSPERO.
Results
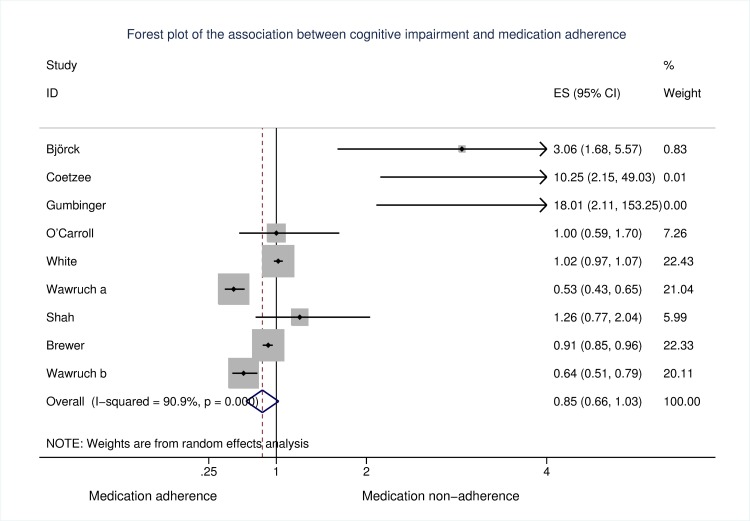
From 1,760 titles and abstracts, we identified 9 studies for inclusion. Measures of cognitive impairment varied from dementia diagnosis to standardised cognitive assessments. Medication adherence was assessed through self-report or administrative databases. The majority of studies were of medium risk of bias (n = 6); two studies had low risk of bias. Findings were mixed; when all studies were pooled, there was no evidence of an association between cognitive impairment and medication non-adherence post-stroke [OR (95% CI): 0.85 (0.66, 1.03)]. However, heterogeneity was substantial [I2 = 90.9%, p < .001], and the overall evidence quality was low.
Conclusions
Few studies have explored associations between cognitive impairment and medication adherence post-stroke, with substantial heterogeneity in study populations, and definitions and assessments of non-adherence and cognitive impairment. Further research using clear, standardised and objective assessments is needed to clarify the association between cognitive impairment and medication non-adherence in stroke.
Introduction
Secondary prevention is essential to maximising health and wellbeing post-stroke. Recurrent strokes account for up to a third of all strokes [1], and are associated with significantly increased risks of mortality [2], long-term disability [3], and dementia [4]. Controlling vascular risk factors through secondary prevention medications, including lipid-lowering medications, antihypertensive and antithrombotic treatment, is vital to decreasing the risk of stroke recurrence [5–8]. Effective secondary stroke prevention is contingent on consistent adherence to prescribed secondary preventive medications [9]. However, medication adherence is frequently poor, with a non-adherence estimate of 30.9% (95% CI: 26.8, 35.3) reported for patients following stroke or transient ischaemic attack (TIA) [10]. Non-adherence is associated with adverse outcomes, including rehospitalisation, recurring vascular events, and death, as well as increased costs of care [8, 11, 12]. Medication adherence has been proposed to consist of three phases: patient initiation, implementation, and discontinuation (non-persistence) [13]. Non-adherence can thus be defined as a patient’s failure to initiate prescribed therapy, sub-optimal implementation of a medication regimen, or early, non-physician initiated discontinuation or non-persistence [13]. We applied this broad definition in order to capture the full breadth of the non-adherence literature.
Cognitive impairment and medication non-adherence
Stroke is associated with a close to 2-fold increased risk of cognitive decline [14], while existing cognitive impairment may predispose to stroke [15, 16]. Cognitive impairment can further increase disability and levels of dependency in patients with stroke, leading to greater burden on carers and the healthcare system [15]. Medication taking involves several cognitive functions, including accessing and scheduling medications, and understanding, remembering and following instructions, all of which may be affected by cognitive impairment [17]. Cardiovascular risk factors, such as hyperlipidaemia, hypertension, and diabetes increase the risk of cognitive decline and dementia [18–20]. The use of anticoagulant, antiplatelet and antihypertensive medications has been reported to be associated with a reduced risk of cognitive impairment post-stroke [7], suggesting that optimum control of risk factors through the regular use of cardiovascular medications could reduce the risk of cognitive decline, as well as reducing the risks of recurrent stroke and cardiovascular events [17, 21].
Considering the prevalence of poor adherence, it is important to consider whether or not patients actually take their medications when evaluating the impact of medications on outcomes [22]. Cognitive impairment has been reported to be associated with poorer adherence to medications in asymptomatic carotid stenosis [21], heart failure [23, 24], and general older adult samples [25, 26], while a recent systematic review explored medication non-adherence in community-dwelling persons with dementia and cognitive impairment [27]. However, only a small number of studies have explored associations between cognitive impairment and adherence post-stroke, with discordant results. Two recent systematic reviews examining a variety of factors associated with medication adherence in stroke featured only a small number of studies of cognitive or memory impairments, and did not meta-analyse the results [10, 28]. The aim of this study, therefore, was to systematically review and meta-analyse the association between cognitive impairment and medication non-adherence in patients with stroke.
Materials and methods
Study design
We performed a systematic review and meta-analysis according to PRISMA guidelines [29]. The review protocol was registered with PROSPERO (available from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015027316).
Eligibility criteria
Study designs
Both longitudinal (cohort and (non)randomised controlled trials) and cross-sectional studies were eligible for inclusion. Published abstracts were included if missing information was available from the authors. We excluded qualitative studies, reviews, letters, editorials, and discussion papers.
Participants
Studies of adults aged ≥18 years with any stroke type (ischaemic or haemorrhagic, first or recurrent) were eligible. Patients with TIA were included. Studies were excluded if the study population was <18 years. Studies that included general patient populations were eligible for inclusion if sub-group analyses were available for patients with stroke. Studies that assessed cognitive impairment and adherence as either exposure or outcome at any time point (baseline or follow-up) were included.
Cognitive impairment
Cognitive impairment can range from mild dysfunction to dementia; therefore, studies reporting any measure of cognitive impairment, including a diagnosis of dementia or standardised cognitive assessment, were included [17].
Adherence
Studies reporting any measure of medication (non)adherence or (non)persistence by patients, such as self-report, pill counts, or pharmacy prescription refill data, were included [13, 17]. Studies that did not specify how adherence was assessed were excluded.
Search methods and information sources
The following electronic databases were searched without language restrictions from database start to 31st December 2016: PubMed, EMBASE, PsycINFO, Web of Science, Scopus, Cochrane Library. Search strategies were developed in consultation with a subject librarian. Search terms included variations and synonyms of stroke, cognitive impairment, adherence, and medication. Search strategies for all databases are presented in the Supporting Information (S1 Table). We augmented searches with reference and Google Scholar citation searches of included studies.
Data collection and analysis
Screening and extraction
Retrieved records were imported to Covidence. Two reviewers (DR and NAM/AH) independently screened titles and abstracts to identify studies potentially meeting the inclusion criteria. Disagreements were resolved through discussion. Full texts of potentially eligible studies were retrieved and assessed for eligibility by the first author. Study authors were contacted for missing data or further information as necessary.
Data were extracted by the first author using a standardised form, including: authors, study design, sample size, sample description, length of follow-up, measure of medication adherence, measure of cognitive impairment, results, and conclusions.
Risk of bias
As all included studies were either cohort studies (n = 8) or based on secondary analysis of RCTs (n = 1), we assessed risk of bias using the Cochrane Bias Methods Group's Tool to Assess Risk of Bias in Cohort Studies [30]. This checklist assesses risk of bias, from low to high, for sample selection, assessment of exposure and outcome, presence/absence of outcome at the beginning of the study, adjustment for prognostic variables, and follow-up. Two reviewers (DR and NAM) independently assessed risk of bias, with disagreements resolved through discussion. Due to the small number of studies identified, we did not exclude any studies based on risk of bias, but instead conducted a sensitivity analysis based on risk of bias.
Evidence quality
The overall quality of the evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, which evaluates study design, study quality, consistency, and directness [31]. Using this approach, observational studies are initially assigned a low grade of evidence, but can be upgraded if there is evidence of a strong and consistent association with no plausible confounders or threats to validity, evidence of a dose response gradient, or when all plausible confounders would have reduced the observed effect [31]. Studies are downgraded for risk of bias, inconsistency of results, indirectness of evidence, imprecision, or publication bias [32]. Potential publication bias was explored by means of a funnel plot.
Data analysis
We conducted a narrative synthesis and meta-analysis. The majority of included studies reported odds ratios (ORs) or hazard ratios (HRs) as measure of effect of the association between cognitive impairment and medication non-adherence. In order to facilitate quantitative pooling of all studies, extracted results for the remaining studies were converted to ORs and 95% confidence intervals (CIs), using 2x2 tables or effect size conversion calculators [33–35]. We conducted a random-effects meta-analysis using the metan command in Stata® 13.0, with heterogeneity assessed using I2. For studies that reported associations between cognitive impairment and adherence at numerous time points, we included results pertaining to the longest follow-up period. Where available, we used adjusted results. Given the significant heterogeneity between studies, sensitivity analyses were conducted according to measure of cognitive impairment (dementia diagnosis vs. standardised cognitive assessment), measure of adherence (objective assessments vs. self-report), adjustment for covariates (adjusted vs. unadjusted), risk of bias, and population (participants with atrial fibrillation (AF) vs. all others, due to preponderance of focus on anticoagulant adherence in included studies).
Results
Study selection
The searches returned 3,083 records, including 1,323 duplicates, resulting in 1,760 titles and abstracts screened for inclusion. 1,722 records were excluded following title and abstract screening; reasons for exclusion are detailed in Fig 1. This left 36 papers for full text screening, and one published abstract with missing information provided by the authors. Following full text screen, 24 papers were excluded. Three repeat papers from two datasets were also excluded, resulting in 9 included studies [36–44].
Fig 1. Flow chart of included studies.
Study characteristics
Design
The majority of included studies were retrospective (n = 4) [36, 41–43] or prospective cohort studies (n = 4) [37–40]. One study was based on secondary analysis from the Secondary Prevention of Small Subcortical Strokes trial [44]. Length of follow-up ranged from 5–6 weeks to 3 years, with results of one study based on cross-sectional analysis (Table 1). All studies reported a measure of medication (non)adherence or persistence as the outcome, with a measure of cognitive impairment as exposure.
Table 1. Characteristics of included studies.
| Author, Year, Location | Design | N (baseline, follow-up) | Follow-up | Population | Outcome | Adherence measure | Cognitive impairment measure | Statistical results | Effect sizes for meta-analysis (Cognitive impairment and non- adherence) | Adjusted for | RoB |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Björck 2015 Sweden [36] | Retrospective cohort | 4583, 4583 | up to 5 years | Stroke and AF | Warfarin non- persistence (treatment gap >7 days registered in AuriculA) | AuriculA: Swedish national quality register for AF and OAC (OAC use registered and updated daily) |
Dementia diagnosis (Swedish National Patient Register) (n = 45) | Patients with dementia more likely to be non-persistent [HR 2.22 (1.51, 3.27)]. | OR (95% CI): 3.0593 (0.6796, 5.5722) | Low | |
| Gumbinger 2015 Germany [39] | Prospective cohort | 284, 139 | 15 months | IS/TIA and AF | Anticoagulant adherence |
Self-report (ascertained through interview) | Dementia diagnosis (stated by the patient, the primary care physician, or relatives) (n = 17) | Dementia predicted non-adherence [OR 18.01 (2.11, 153.25)]. | OR (95% CI): 18.01 (2.11, 153.25) | Sex, nursing home residence | Medium |
| Shah 2016 Canada [41] | Retrospective cohort | 2877, 2877 | 12 months | IS/TIA and AF | Oral anticoagulant adherence |
Prescription claims (PDC<0.4 = poor adherence) |
Dementia diagnosis (Ontario Stroke Registry, based on hospital chart review) (n = 590) | Dementia not associated with poor adherence (PDC <0.4) [OR 1.26 (0.77, 2.04)]. | OR (95% CI): 1.26 (0.77, 2.04) | Age, sex, income, TIA/stroke, residence, stroke severity, comorbidities, long-term care residence. | Low |
| Wawruch 2016a Slovakia [43] | Retrospective cohort |
4319, 4319 | 3 years | Stroke | Antiplatelet non-persistence |
Prescription records (treatment gap> = 6 months) | Dementia diagnosis (extracted from the database of the largest health insurance provider in the Slovak Republic) (n = 694) | Dementia decreased probability of non-persistence [HR 0.69 (0.57, 0.83)]. | OR (95% CI): 0.526 (0.428, 0.648) |
Age, sex, hypertension, diabetes, high cholesterol, depression, anxiety, Parkinson's, epilepsy, polypharmacy, medication switching. | Medium |
| Wawruch 2016b Slovakia [42] |
Retrospective cohort | 2748, 2748 | 3 years | Ischaemic stroke | Statin non-persistence |
Prescription records (treatment gap> = 6 months) |
Dementia diagnosis (extracted from the database of the largest health insurance provider in the Slovak Republic) (n = 518) | Dementia decreased probability of non-persistence [HR 0.84 (0.73, 0.98)]. | OR (95% CI): 0.6366 (0.5129, 0.7901) | Age, sex, hypertension, diabetes mellitus, hypercholesterolemia, depression, anxiety. | Medium |
| Coetzee 2008 Australia [38] | Prospective cohort | Baseline unclear, 25 | 6 weeks | IS/TIA | Medication adherence |
Pill counts and self-report (Treatment Assessment Schedule) | Cognitive assessment (EFQ) | Memory dysfunction associated with poorer adherence [r = -.54]. Dysfunction in planning/ organisation associated with poorer adherence [r = -.52]. | OR (95% CI): 10.248 (2.154, 49.029) | High | |
| O'Carroll 2011 Scotland [40] | Prospective cohort | 180, 180 | 5–6 weeks | Ischaemic stroke | Medication adherence |
Self-report (MARS) | Cognitive assessment (MMSE) | Cross-sectional—MMSE score associated with adherence score (β = 0.201). | Age, sex, stroke severity, illness perception and belief about medications variables, emotional distress, social deprivation index, perception of risk of further stroke. | Medium | |
| Longitudinal- MMSE score not associated with adherence score (β = 0.005). | OR (95% CI): 1.000 (0.589, 1.698) | ||||||||||
| White 2010 North America, Latin America, Spain [44] | RCT (patients active on both arms included) |
526, 471, 323 | 3 years | Lacunar stroke | Medication adherence |
Pill counts and self-report (self-report method unclear) |
Cognitive assessment (CASI) | No association between cognitive impairment and adherence at year 1 [OR 1.001 (0.981, 1.021)]; year 2 [OR 0.988 (0.960, 1.016)]; year 3 [OR 0.979 (0.933, 1.028)]. | OR (95% CI): 1.021 (0.973, 1.071) | Age, sex, education, ethnicity, employment status, smoking, alcohol consumption, exercise, BMI, marital status, living arrangements, health rating, number of medications, Rankin, Barthel, missed clinic visits, previously inactive on any therapy. | Medium |
| Brewer 2015 Ireland [37] | Prospective cohort | 302, 256 | 6 months | Ischaemic stroke | Medication adherence |
Self-report (MARS) | Cognitive assessment (MoCA) | Cross-sectional analysis: absence of cognitive impairment associated with non-adherence [OR 1.10 (1.04, 1.17)]. | OR (95% CI): 0.91 (0.85, 0.96) | Age, sex. | Medium |
Note: IS ischaemic stroke; PDC proportion of days covered; RoB risk of bias; OAC oral anticoagulant
Population
Three studies included stroke or stroke and TIA patients with AF [36, 39, 41]. Five studies included ischaemic stroke or ischaemic stroke and TIA patients [37, 40, 42–44], one study included mixed stroke types [38]. Sample sizes ranged from 25 to 4,583 participants.
Cognitive impairment measure
Five studies included a diagnosis of dementia as a measure of cognitive impairment [36, 39, 41–43], while one study each used the Montreal Cognitive Assessment (MoCA) [37], Mini Mental State Examination (MMSE) [40], Cognitive Abilities Screening Instrument (CASI) [44], or Everyday Functioning Questionnaire (EFQ) [38]. Diagnosis of dementia was based on data recorded in health insurance or patient registry databases [36, 41–43], or on report by the patient, relative, or primary care physician [39].
Outcome measure
Assessments of (non)adherence included the Medication Adherence Report Scale (MARS) (n = 2) [37, 40], self-report either alone or in combination with pill counts (n = 3) [38, 39, 44], prescription records (n = 3) [41–43], or ongoing treatment registered in a Swedish national quality register for atrial fibrillation and oral anticoagulation (AuriculA) (n = 1) [36]. Three studies considered adherence to anticoagulant medications in stroke patients with AF [36, 39, 41], one study each focused on antiplatelets [43] and statins [42]. Three studies utilising self-report did not distinguish between medications [37, 38, 40], while one study combined pill counts of antiplatelet medications with self-reported antihypertensive medication adherence to create a composite adherence measure [44]. In addition to the MARS, self-report measures of adherence included the non-validated Treatment Assessment Schedule [38]. Two studies did not provide details on the use of self-report instruments [39, 44].
Risk of bias
The majority of studies were rated at medium risk of bias [37, 39, 40, 42–44], with two studies considered at low [36, 41] and one at high risk of bias [38].
Evidence quality
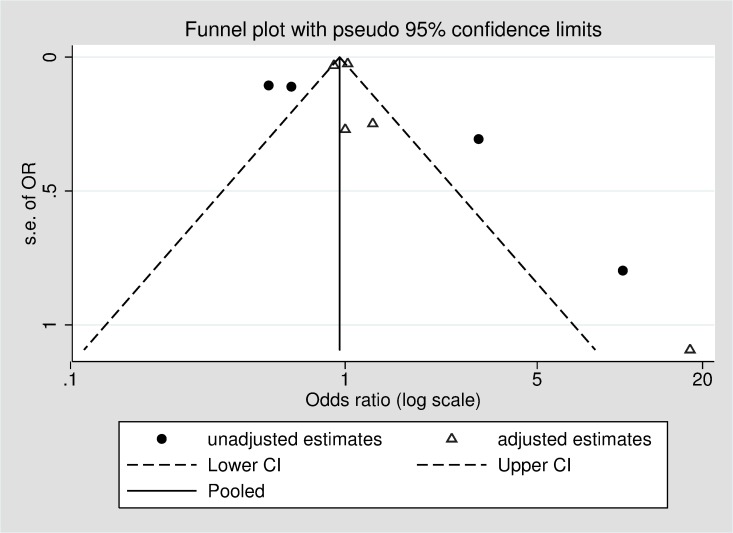
Based on the GRADE approach, the overall quality of the evidence was rated as low, with no studies being upgraded from their initial rating, and two studies downgraded due to inconsistent large and imprecise effect estimates based on unadjusted or minimally adjusted analyses and uncertainty about the directness of the predictor or outcome (Table 2). Fig 2 displays a funnel plot of included studies, showing a potential absence of small and medium-sized studies, and smaller studies reporting that cognitive impairment may reduce the likelihood of medication non-adherence. However, it is important to note that asymmetry in funnel plots can have several causes, including heterogeneity or chance [45]. The pseudo 95% confidence limits indicate the distribution of studies that would be expected in the absence of heterogeneity [46], indicating that the asymmetry seen here could be due to significant heterogeneity between studies, for example as a result of differences between adjusted and unadjusted estimates.
Table 2. GRADE quality of evidence.
| Quality assessment | Summary of findings |
|||||||
|---|---|---|---|---|---|---|---|---|
| Studies | Design | Risk of bias | Consistency | Directness | Other modifying factors | No of participants at follow-up | Effect OR (95% CI) | Quality of evidence (GRADE) |
|
Cognitive assessment as measure of cognitive impairment | ||||||||
| Brewer [37] | Observational | Medium | No major inconsistencies | Direct (but self-report) | Cross-sectional analysis | 256 | 0.91 (0.85, 0.96) | Low ⊕⊕ |
| O’Carroll [40] | Observational | Medium | No major inconsistencies | Direct (but self-report) | 180 | 1.000 (0.589, 1.698) | Low ⊕⊕ | |
| White [44] | RCT (analysis of adherence based both active arms) | Medium | No major inconsistencies | Uncertainty about outcome measure–unclear self report method | 323 | 1.021 (0.973, 1.071) | Low ⊕⊕ | |
| Coetzee [38] | High | Effect estimate is large and imprecise. | Uncertainty about directness of predictor–cognitive impairment based on memory dysfunction or dysfunction in planning/organisation (rather than global cognitive impairment). Uncertainty about outcome measure–non-validated self-report | Estimate is based on unadjusted analyses. | 25 | 10.248 (2.154, 49.029) | Very low ⊕ | |
|
Dementia diagnosis as measure of cognitive impairment$ | ||||||||
| Gumbinger [39] | Observational | Medium | Effect estimate is large and imprecise | Uncertainty about outcome measure–non-validated self-report | Minimal adjustment for confounders. | 139 | 18.01 (2.11, 153.25) | Very low ⊕ |
| Björck [36] | Observational | Low | Effect estimate is quite large. | Estimate included in meta-analysis is unadjusted. | 4583 | 3.059 (0.680, 5.572) | Low ⊕⊕ |
|
| Shah [41] | Observational | Low | No major inconsistencies | PDC<0.4 taken to indicate poor adherence–more usual to use cut-off of <0.8 | 2877 | 1.26 (0.77, 2.04) | Low ⊕⊕ | |
| Wawruch a [43] | Observational | Medium | No major inconsistencies | Estimate included in meta-analysis is unadjusted | 4319 | 0.526 (0.428, 0.648) | Low ⊕⊕ | |
| Wawruch b [42] | Observational | Medium | No major inconsistencies | Estimate included in meta-analysis is unadjusted | 2748 | 0.637 (0.513, 0.790) | Low ⊕⊕ | |
Note: observational studies are assigned a baseline rating of low in the GRADE system. Studies may be upgraded if there is a large magnitude of effect, evidence of a dose response relationship, or when all plausible confounders would have reduced the observed effect
$ Some uncertainty about directness of predictor. Diagnosis of dementia represents the severe end of the cognitive impairment spectrum only. Several studies have reported physician-initiated discontinuation of anticoagulants in patients with dementia, which may confound associations between dementia and adherence to anticoagulants (considered by Gumbinger, Björck and Shah).
Fig 2. Funnel plot of included studies, stratified by adjustment for covariates.
Associations between cognitive impairment and medication non-adherence
Evidence on the association between cognitive impairment and non-adherence was discordant; three studies found no association between medication adherence and cognitive impairment [40, 41, 44], three reported that cognitive impairment was associated with increased non-adherence [36, 38, 39] while three studies reported that cognitive impairment was associated with decreased non-adherence [37, 42, 43]. When all studies were pooled, there was no evidence of an association between cognitive impairment and non-adherence [OR (95% CI): 0.85 (0.66, 1.03)]; however, heterogeneity was substantial [I2 = 90.9%, p < .001] (Fig 3). Excluding one study rated at high risk of bias did not affect this estimate [OR (95% CI): 0.85 (0.66, 1.03); I2 = 92.0%, p < .001]. Due to the significant heterogeneity between studies and differing study populations, assessments of cognitive impairment and adherence, and adjustment for covariates, a number of sensitivity analyses were conducted.
Fig 3. Forest plot of included studies.
Sensitivity analyses
Measure of cognitive impairment
Five studies included a diagnosis of dementia as the measure of cognitive impairment [36, 39, 41–43]. Two of these reported increased non-adherence in patients with dementia [36, 39], while two reported that dementia was associated with reduced non-adherence [42, 43]. When these five studies were pooled, diagnosis of dementia appeared to be associated with a reduced likelihood of non-adherence [OR (95% CI): 0.70 (0.45, 0.94)]; however, there was significant heterogeneity between studies [I2 = 67.7%, p = .015]. Each of the remaining four studies used a different assessment of cognitive impairment. When these studies were pooled, there was no evidence of an association between cognitive impairment and medication adherence [OR (95% CI): 0.97 (0.87, 1.07); I2 = 67.9%, p = .025] (Table 3).
Table 3. Meta-analysis and sensitivity analyses.
|
Included studies |
Medication non-adherence | ||
|---|---|---|---|
| OR (95% CI) | Heterogeneity (I2) | ||
| All | 0.845 (0.664, 1.026) | 90.9% | |
| Measure of cognitive impairment | Diagnosis of dementia (n = 5) | 0.696 (0.451, 0.942) | 67.7% |
| Assessment of cognitive impairment (n = 4) | 0.968 (0.870, 1.065) | 67.9% | |
| Population | Stroke patients with AF only (n = 3) | 0.827 (0.436, 3.219) | 36.5% |
| All other stroke patients (n = 6) | 0.799 (0.614, 0.983) | 93.9% | |
| Adherence measure |
Objective (n = 4) | 0.703 (0.448, 0.958) | 75.4% |
| Self-report (n = 5) | 0.968 (0.875, 1.060) | 58.0% | |
| Adjustment for covariates | Adjusted (n = 4) | 0.973 (0.881, 1.066) | 58.8% |
| Unadjusted (n = 5) | 0.612 (0.390, 0.834) | 64.4% | |
| Risk of Bias | Medium (n = 6) | 0.798 (0.614, .983) | 93.9% |
| Low (n = 2) | 1.915 (0.218, 3.612) | 66.3% | |
| High (n = 1) | 10.248 (2.154, 49.029) | ||
Study population
Three studies included stroke or stroke/TIA patients with AF, and assessed adherence to anticoagulant medications [36, 39, 41]. All three studies included a diagnosis of dementia, but used a different measure and definition of adherence. Two studies noted that non-adherence was more likely in patients with dementia [36, 39]; however, when all three were pooled, there was no evidence of an association between cognitive impairment and non-adherence [OR (95% CI): 1.83 (0.44, 3.22); I2 = 36.5%, p = 0.207]. The remaining studies did not focus exclusively on patients with stroke and AF. When these studies were subjected to meta-analysis, cognitive impairment appeared to be associated with a reduced likelihood of non-adherence; however, heterogeneity between studies was substantial [OR (95% CI): 0.80 (0.61, 0.98); I2 = 93.9%, p < .001].
Measure of medication adherence
When studies that assessed medication adherence based on administrative databases (prescription claims or national register) were pooled, dementia again appeared to be associated with a reduced likelihood of non-adherence [OR (95% CI): 0.70 (0.45, 0.96); I2 = 75.4%, p = .007]. Conversely, there was no evidence of an association between medication non-adherence based on self-report (either alone or in combination with pill counts), and cognitive impairment OR (95% CI): 0.97 (0.88, 1.06); I2 = 58.0%, p = .049].
Adjustment for covariates
Adjustment for covariates varied widely between studies (Table 1). While we included adjusted measures of effect size in the meta-analysis where possible, in order to facilitate pooling of estimates from all studies, some unadjusted results were included [36, 38, 42, 43]. When studies with adjusted and unadjusted estimates were considered separately, there was no evidence of an association between cognitive impairment and medication non-adherence in studies with adjusted results [OR (95% CI): 0.97 (0.88, 1.07); I2 = 58.8%, p = .046]. However, for studies with unadjusted estimates, cognitive impairment was associated with reduced non-adherence [OR (95% CI): 0.61 (0.39, 0.83); I2 = 64.4%, p = .038]. The funnel plot suggests that these differences between studies reporting adjusted and unadjusted results may partially account for the heterogeneity between studies (Fig 2).
Adjustment for long-term care residence, living arrangements or social support
The majority of studies did not include information on living arrangements, long-term care residence or social support, all of which may plausibly influence adherence. Two studies controlled for long-term care residence in their analyses of the association between cognitive impairment and non-adherence. Gumbinger et al. reported that nursing home residence was a risk factor for non-adherence to oral anticoagulants [39], while Shah et al. found no association between long-term care residence and non-adherence in adjusted analyses [41]. White et al. adjusted for living arrangements (alone vs. with others), and found no evidence of an association between living arrangements and adherence [44]. Coetzee et al. reported that social support was associated with better adherence in unadjusted analyses [38].
Discussion
When all studies were pooled, we found no evidence of an association between cognitive impairment and medication non-adherence. The substantial heterogeneity in study populations and various definitions and assessments of adherence and cognitive impairment, combined with the overall low quality of the evidence, make it difficult to draw definitive conclusions. Significant heterogeneity was also noted in two recent systematic reviews on adherence to secondary preventive medications post-stroke [10, 28]. It may be that no association exists between cognitive impairment and medication adherence, with associations reported by observational studies due to inadequate adjustment for confounding. Indeed, while cognitive impairment was associated with reduced medication non-adherence in studies reporting unadjusted results, we found no association between cognitive impairment and adherence in our sensitivity analysis of studies reporting adjusted results. A recent study of a general adult population similarly found no association between cognitive impairment and adherence to cardiovascular medications after adjustment for a range of potential confounders [22].
It may, however, be important to distinguish between degrees of cognitive impairment, as individuals with more severe impairments and dementia may rely on caregivers to administer medications, leading to increased adherence [17, 47], while those with mild cognitive impairment managing their own medications may be most at risk of sub-optimal adherence. The association between cognitive impairment and adherence, if it exists, may in fact be U-shaped, with poorer adherence in patients with milder cognitive impairments who self-administer their medications, and better adherence in patients with more severe impairments who receive support with medication taking. Increased support from family and higher levels of care at home have been reported to be associated with better adherence [27, 28]. The majority of included studies did not report living arrangements, long-term care residence or social support, with no clear pattern emerging regarding the potential impact of these factors on adherence in studies that did include them. Indeed, there is limited information on factors associated with non-adherence in individuals who rely on family members or carers for medication management, and further research in this area is required [48, 49]. While we found that a diagnosis of dementia may be associated with better medication adherence, there was no evidence of an association for cognitive impairment based on cognitive assessments. However, we were unable to distinguish between degrees of cognitive impairment in these studies. A diagnosis of dementia has also been associated with physician-initiated discontinuation of oral anticoagulation in stroke patients (for example, due to a perceived increased risk of falls) [39, 41, 50], further complicating the association between medication adherence and cognitive function post-stroke.
A substantial number of studies screened for this review did not include or report measures of cognitive impairment. A smaller number assessed both cognitive impairment and medication non-adherence, but did not report the association between these two measures; or included general adult/patient populations and did not report sub-group analyses for stroke survivors (Supporting Information S2 Table). The authors of these studies were contacted for further information; however, data were either unavailable (n = 4) or no response was received (n = 4), a problem noted in other systematic reviews [28]. Few studies to date have explored or reported associations between cognitive impairment and adherence post-stroke, with six of the nine studies included in this review published since 2015.
A variety of factors can influence stroke patients’ medication adherence, including concerns about treatment, knowledge about medications and beliefs about benefits and consequences [28, 40], increased disability, more severe stroke, polypharmacy [10], living in a nursing home and initiation of medications during in-hospital stay [39], self-rated health [44], age [40, 41], sex [43, 51], education [51], and presence of other comorbidities [36]. Considering the number of different measures and definitions of adherence and cognitive impairment, it is not surprising that predictors of medication (non)adherence have varied widely between studies. The use of a similarly wide variety of definitions and measures of medication non(adherence) has been noted by other systematic reviews [27, 52]. This lack of conceptual clarity in the definition and measurement of adherence leads to difficulties in comparing methods and results across studies [52]. While sensitivity analyses suggested a potential association between cognitive impairment and adherence based on objective measures, there was no association between self-reported adherence and cognitive impairment. Self-report instruments are subject to social desirability and recall bias, which may be particularly problematic in patients with cognitive impairments [12]. Where possible, future studies should focus on objective measures, such as prescription records, to assess adherence. Future studies could also explore how adherence to secondary preventive medications might affect post-stroke cognitive impairment or decline [49], and investigate associations between medication adherence and individual cognitive domains [27].
Limitations
Only published, peer-reviewed articles or published abstracts of conference proceedings were considered for this review. Due to time and resource constraints, grey literature was excluded, which may lead to a publication or time lag bias. While two reviewers independently screened titles and abstracts, full text screening and data extraction were conducted by one reviewer only, which could have resulted in some studies being missed. However, any doubts over inclusion/exclusion were discussed with a second reviewer before the final decision was made. In studies that included a diagnosis of dementia as a measure of cognitive impairment, this was based on data recorded in health insurance or patient registry databases, or patient, relative, or physician report. This may have led to an underestimation of the number of participants with dementia, an underestimation of those with at least some level of cognitive impairment, and subsequent underestimation of the association between dementia and (non)adherence. Further, there was substantial heterogeneity between studies, and only two of the included studies were considered as low risk of bias. Given the significant heterogeneity between studies in terms of assessments of medication adherence and cognitive impairment, and differential adjustment for confounders, the meta-analysis and sensitivity analyses should be interpreted with caution. Indeed, based on the GRADE assessment, the overall quality of the evidence was low, suggesting that the true association between cognitive impairment and non-adherence may be substantially different, with further research likely to have an impact on the estimates [31, 32]. In spite of these limitations however, the pooled estimates provide an important quantification of the substantial heterogeneity between the limited number of studies that have been published in this area, and highlight the need for further research, using clear, standardised and where possible objective assessments of both cognitive impairment and medication non-adherence.
Conclusion
Few studies have explored associations between cognitive impairment and medication non-adherence in stroke patients. The substantial heterogeneity in study populations and definitions and assessments of adherence and cognitive impairment, coupled with the overall low quality of evidence, make it difficult to draw definitive conclusions. Given the importance of secondary prevention post-stroke and the association between medication adherence and outcomes, further research, with objective measures of adherence, is required to help identify those patients at greatest risk of non-adherence. Once suboptimal adherence has been recognised, care providers and patients can work together to address barriers to adherence and improve outcomes [11].
Supporting information
(DOCX)
(DOCX)
(DOC)
(PDF)
(XLS)
Acknowledgments
The authors would like to thank Ms. Grainne McCabe for her help in designing the systematic database search strategies.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Irish Health Research Board (grant nos. SPHeRE 2013/1 and RL-15-1579; http://www.hrb.ie). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hankey GJ. Secondary stroke prevention. Lancet Neurol. 2014;13(2):178–94. doi: 10.1016/S1474-4422(13)70255-2 [DOI] [PubMed] [Google Scholar]
- 2.Aarnio K, Haapaniemi E, Melkas S, Kaste M, Tatlisumak T, Putaala J. Long-Term Mortality After First-Ever and Recurrent Stroke in Young Adults. Stroke. 2014;45(9):2670 doi: 10.1161/STROKEAHA.114.005648 [DOI] [PubMed] [Google Scholar]
- 3.Dhamoon MS, McClure LA, White CL, Lakshminarayan K, Benavente OR, Elkind MS. Long-term disability after lacunar stroke: secondary prevention of small subcortical strokes. (1526-632X (Electronic)).D—NLM: PMC4352098 EDAT- 2015/02/11 06:00 MHDA- 2015/05/15 06:00 CRDT- 2015/02/10 06:00 AID—WNL.0000000000001331 [pii] AID—10.1212/WNL.0000000000001331 [doi] PST—ppublish. [DOI] [PMC free article] [PubMed]
- 4.Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8(11):1006–18. doi: 10.1016/S1474-4422(09)70236-4 [DOI] [PubMed] [Google Scholar]
- 5.O'Carroll RE, Chambers JA, Dennis M, Sudlow C, Johnston M. Improving adherence to medication in stroke survivors: a pilot randomised controlled trial. Ann Behav Med. 2013;46(3):358–68. doi: 10.1007/s12160-013-9515-5 [DOI] [PubMed] [Google Scholar]
- 6.Sjölander M, Eriksson M, Glader EL. The association between patients' beliefs about medicines and adherence to drug treatment after stroke: a cross-sectional questionnaire survey. BMJ Open. 2013;3(9):e003551 doi: 10.1136/bmjopen-2013-003551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Douiri A, McKevitt C, Emmett ES, Rudd AG, Wolfe CD. Long-term effects of secondary prevention on cognitive function in stroke patients. Circulation. 2013;128(12):1341–8. doi: 10.1161/CIRCULATIONAHA.113.002236 [DOI] [PubMed] [Google Scholar]
- 8.Bergström L, Irewall AL, Söderström L, Ögren J, Laurell K, Mooe T. One-Year Incidence, Time Trends, and Predictors of Recurrent Ischemic Stroke in Sweden From 1998 to 2010: An Observational Study. Stroke. 2017;48(8):2046–51. doi: 10.1161/STROKEAHA.117.016815 [DOI] [PubMed] [Google Scholar]
- 9.Murphy SJ, Coughlan CA, Tobin O, Kinsella J, Lonergan R, Gutkin M, et al. Continuation and adherence rates on initially-prescribed intensive secondary prevention therapy after Rapid Access Stroke Prevention (RASP) service assessment. J Neurol Sci. 2016;361:13–8. doi: 10.1016/j.jns.2015.12.009 [DOI] [PubMed] [Google Scholar]
- 10.Al AlShaikh S, Quinn T, Dunn W, Walters M, Dawson J. Predictive factors of non-adherence to secondary preventative medication after stroke or transient ischaemic attack: A systematic review and meta-analyses. European Stroke Journal. 2016. doi: 10.1177/2396987316647187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–35. doi: 10.1161/CIRCULATIONAHA.108.768986 [DOI] [PubMed] [Google Scholar]
- 12.Kronish IM, Ye S. Adherence to cardiovascular medications: lessons learned and future directions. Prog Cardiovasc Dis. 2013;55(6):590–600. doi: 10.1016/j.pcad.2013.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. doi: 10.1111/j.1365-2125.2012.04167.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajan KB, Aggarwal NT, Wilson RS, Everson-Rose SA, Evans DA. Association of cognitive functioning, incident stroke, and mortality in older adults. Stroke. 2014;45(9):2563–7. doi: 10.1161/STROKEAHA.114.005143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brainin M, Tuomilehto J, Heiss WD, Bornstein NM, Bath PM, Teuschl Y, et al. Post-stroke cognitive decline: an update and perspectives for clinical research. European Journal of Neurology. 2015;22(2):229–38, e13-6. doi: 10.1111/ene.12626 [DOI] [PubMed] [Google Scholar]
- 16.Pendlebury ST. Dementia in patients hospitalized with stroke: rates, time course, and clinico-pathologic factors. Int J Stroke. 2012;7(7):570–81. doi: 10.1111/j.1747-4949.2012.00837.x [DOI] [PubMed] [Google Scholar]
- 17.Campbell NL, Boustani MA, Skopelja EN, Gao S, Unverzagt FW, Murray MD. Medication adherence in older adults with cognitive impairment: a systematic evidence-based review. Am J Geriatr Pharmacother. 2012;10(3):165–77. doi: 10.1016/j.amjopharm.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 18.Jefferson AL, Hohman TJ, Liu D, Haj-Hassan S, Gifford KA, Benson EM, et al. Adverse vascular risk is related to cognitive decline in older adults. J Alzheimers Dis. 2015;44(4):1361–73. doi: 10.3233/JAD-141812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Unverzagt FW, McClure LA, Wadley VG, Jenny NS, Go RC, Cushman M, et al. Vascular risk factors and cognitive impairment in a stroke-free cohort. Neurol. 2011;77(19):1729–36. doi: 10.1212/WNL.0b013e318236ef23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Allan LM, Rowan EN, Firbank MJ, Thomas AJ, Parry SW, Polvikoski TM, et al. Long term incidence of dementia, predictors of mortality and pathological diagnosis in older stroke survivors. Brain. 2011;134(Pt 12):3716–27. doi: 10.1093/brain/awr273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirkpatrick AC, Vincent AS, Guthery L, Prodan CI. Cognitive impairment is associated with medication nonadherence in asymptomatic carotid stenosis. Am J Med. 2014;127(12):1243–6. doi: 10.1016/j.amjmed.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 22.Rohde D, Hickey A, Williams D, Bennett K. Cognitive impairment and cardiovascular medication use: Results from Wave 1 of The Irish Longitudinal Study on Ageing. Cardiovascular Therapeutics [Internet]. 2017; e12300:[e12300 p.]. [DOI] [PubMed] [Google Scholar]
- 23.Alosco ML, Spitznagel MB, van Dulmen M, Raz N, Cohen R, Sweet LH, et al. Cognitive Function and Treatment Adherence in Older Adults With Heart Failure. Psychosomatic Medicine. 2012;74(9):965–73. doi: 10.1097/PSY.0b013e318272ef2a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawkins LA, Kilian S, Firek A, Kashner TM, Firek CJ, Silvet H. Cognitive impairment and medication adherence in outpatients with heart failure. Heart Lung. 2012;41(6):572–82. doi: 10.1016/j.hrtlng.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 25.Vinyoles E, De la Figuera M, Gonzalez-Segura D. Cognitive function and blood pressure control in hypertensive patients over 60 years of age: COGNIPRES study. Curr Med Res Opin. 2008;24(12):3331–9. doi: 10.1185/03007990802538724 [DOI] [PubMed] [Google Scholar]
- 26.Leung DYP, Bai X, Leung AY, Liu BC, Chi I. Prevalence of medication adherence and its associated factors among community-dwelling Chinese older adults in Hong Kong. Geriatrics and Gerontology International. 2015;15(6):789–96 doi: 10.1111/ggi.12342 [DOI] [PubMed] [Google Scholar]
- 27.Smith D, Lovell J, Weller C, Kennedy B, Winbolt M, Young C, et al. A systematic review of medication non-adherence in persons with dementia or cognitive impairment. PLoS One. 2017;12(2):e0170651 doi: 10.1371/journal.pone.0170651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crayton E, Fahey M, Ashworth M, Besser SJ, Weinman J, Wright AJ. Psychological Determinants of Medication Adherence in Stroke Survivors: a Systematic Review of Observational Studies. Ann Behav Med. 2017. doi: 10.1007/s12160-017-9906-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535 doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cochrane Bias Methods Group. Tool to Assess Risk of Bias in Cohort Studies. 2013 [cited 16 April 2015]. [cited 16 April 2015]. Available from: http://bmg.cochrane.org/sites/bmg.cochrane.org/files/uploads/Tool to Assess Risk of Bias in Cohort Studies.pdf to Assess Risk of Bias in Cohort Studies.pdf.
- 31.GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490 doi: 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schünemann H, Brożek J, Guyatt GH, Oxman AD. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach 2013. Available from: http://gdt.guidelinedevelopment.org/app/handbook/handbook.html - h.svwngs6pm0f2.
- 33.Lipsey MW, Wilson DB. Practical meta-analysis. London: Sage; 2001. [Google Scholar]
- 34.Wilson DB. Practical meta-analysis effect size calculator 2010 [cited 2017 25 April]. Available from: https://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-Home.php.
- 35.DeCoster J. Effect size converter 2012 [cited 2017 25 April]. Available from: http://stat-help.com/spreadsheets.html.
- 36.Björck F, Renlund H, Svensson PJ, Själander A. Warfarin persistence among stroke patients with atrial fibrillation. Thrombosis Research. 2015;136(4):744–8 doi: 10.1016/j.thromres.2015.07.028 [DOI] [PubMed] [Google Scholar]
- 37.Brewer L, Mellon L, Hall P, Dolan E, Horgan F, Shelley E, et al. Secondary prevention after ischaemic stroke: the ASPIRE-S study. BMC Neurol. 2015;15:216 doi: 10.1186/s12883-015-0466-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coetzee N, Andrewes D, Khan F, Hale T, Jenkins L, Lincoln N, et al. Predicting compliance with treatment following stroke: A new model of adherence following rehabilitation. Brain Impairment. 2008;9(2):122–39. doi: 10.1375/brim.9.2.122 [Google Scholar]
- 39.Gumbinger C, Holstein T, Stock C, Rizos T, Horstmann S, Veltkamp R. Reasons underlying non-adherence to and discontinuation of anticoagulation in secondary stroke prevention among patients with atrial fibrillation. Eur Neurol. 2015;73(3–4):184–91. doi: 10.1159/000371574 [DOI] [PubMed] [Google Scholar]
- 40.O'Carroll R, Whittaker J, Hamilton B, Johnston M, Sudlow C, Dennis M. Predictors of adherence to secondary preventive medication in stroke patients. Ann Behav Med. 2011;41(3):383–90. doi: 10.1007/s12160-010-9257-6 [DOI] [PubMed] [Google Scholar]
- 41.Shah R, Li S, Stamplecoski M, Kapral MK. Low use of oral anticoagulant prescribing for secondary stroke prevention results from the Ontario stroke registry. Medical Care. 2016;54(10):907–12 doi: 10.1097/MLR.0000000000000589 [DOI] [PubMed] [Google Scholar]
- 42.Wawruch M, Zatko D, Wimmer G Jr., Luha J, Hricak V Jr., Murin J, et al. Patient-related characteristics associated with non-persistence with statin therapy in elderly patients following an ischemic stroke. Pharmacoepidemiol Drug Saf. 2016. doi: 10.1002/pds.4148 [DOI] [PubMed] [Google Scholar]
- 43.Wawruch M, Zatko D, Wimmer G Jr., Luha J, Kuzelova L, Kukumberg P, et al. Factors Influencing Non-Persistence with Antiplatelet Medications in Elderly Patients After Ischaemic Stroke. Drugs Aging. 2016;33(5):365–73. doi: 10.1007/s40266-016-0365-2 [DOI] [PubMed] [Google Scholar]
- 44.White CL, Szychowski JM, Talbert RL, Holzemer E, Lau H, McClure LA. Self-rating of health and adherence to secondary stroke prevention medications in the secondary prevention of small subcortical strokes trial. Stroke. 2010;41(4):e290 [Abstract] [Google Scholar]
- 45.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002 doi: 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 46.Sterne JA, Harbord RM. Funnel plots in meta-analysis. The stata journal. 2004;4(2):127–41 [Google Scholar]
- 47.Polymeris AA, Traenka C, Hert L, Seiffge DJ, Peters N, De Marchis GM, et al. Frequency and Determinants of Adherence to Oral Anticoagulants in Stroke Patients with Atrial Fibrillation in Clinical Practice. Eur Neurol. 2016;76(3–4):187–93. doi: 10.1159/000450750 [DOI] [PubMed] [Google Scholar]
- 48.De Simoni A, Mant J, Sutton S. Adherence to medication in stroke survivors dependent on caregivers. Br J Gen Pract. 2015;65(640):e789–e91 doi: 10.3399/bjgp15X687589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rohde D, Williams D, Gaynor E, Bennett K, Dolan E, Callaly E, et al. Secondary prevention and cognitive function after stroke: a study protocol for a 5-year follow-up of the ASPIRE-S cohort. BMJ Open. 2017;7(3):e014819 doi: 10.1136/bmjopen-2016-014819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilke T, Groth A, Pfannkuche M, Harks O, Fuchs A, Maywald U, et al. Real life anticoagulation treatment of patients with atrial fibrillation in Germany: extent and causes of anticoagulant under-use. J Thromb Thrombolysis. 2015;40(1):97–107. doi: 10.1007/s11239-014-1136-8 [DOI] [PubMed] [Google Scholar]
- 51.Sjölander M, Eriksson M, Glader E-L. Inequalities in medication adherence to statin treatment after stroke: A nationwide observational study. European Stroke Journal. 2016;1(2):101–7. doi: 10.1177/2396987316646026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wessol JL, Russell CL, Cheng AL. A Systematic Review of Randomized Controlled Trials of Medication Adherence Interventions in Adult Stroke Survivors. J Neurosci Nurs. 2017;49(2):120–33. doi: 10.1097/JNN.0000000000000266 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOC)
(PDF)
(XLS)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.