Abstract
Background
Type 2 myocardial infarction (MI) is defined by a rise and fall of cardiac biomarkers and evidence of ischemia without unstable coronary artery disease (CAD), due to a mismatch in myocardial oxygen supply and demand. Myocardial injury is similar but does not meet clinical criteria for MI. There is uncertainty regarding clinical characteristics, management and outcomes of type 2 MI and myocardial injury in comparison to type 1 MI.
Methods
Patients admitted to a Veterans Affairs tertiary-care hospital with a rise and fall in cardiac troponin (cTnI) were identified. MI and injury subtypes, presentation, management, and outcomes were determined.
Results
Type 1 MI, type 2 MI, and myocardial injury occurred in 137, 146, and 175 patients, respectively. Patients with type 2 MI were older (p=0.02), had lower peak cTnI (p<0.001), and were less likely to receive aspirin and statin at discharge (p<0.001) than type 1 MI survivors. All-cause mortality (median follow-up 1.8 years) was not different between patient groups (type 1 MI mortality: 29.9%, type 2 MI: 30.8%, myocardial injury: 29.7%; log-rank p=0.94). A significant proportion of deaths were attributed to cardiovascular causes in all subgroups (type 1 MI: 34.1%, type 2 MI: 17.8%, myocardial injury: 30.8%).
Conclusion
Patients with type 2 MI and myocardial injury were less likely to receive medical therapy for CAD than those with type 1 MI. No differences in all-cause mortality among MI subtypes were observed. Additional studies to determine optimal medical therapy and risk stratification strategies for these high-risk populations are warranted.
Keywords: Acute Coronary Syndrome, Biomarkers, Demand Ischemia, Ischemic Heart Disease, Mortality
Background
According to the Universal Definition of Myocardial Infarction (MI), the diagnosis of MI requires the rise and/or fall of cardiac biomarkers with clinical evidence of ischemia, defined by symptoms, electrocardiographic (ECG) changes, or new regional wall motion abnormalities. Since 2007, this definition has classified MI into 5 distinct subtypes.1 In contrast to MI due to an acute coronary syndrome (type 1 MI), type 2 MI is defined as a mismatch in myocardial oxygen supply and demand that is not attributed to unstable coronary artery disease (CAD). Type 2 MI has been reported in 2% to 25% of cases of MI, depending on the population studied and the sensitivity of the cardiac biomarker assay.2–11 Although type 2 MI has been formally described for a decade, there remains considerable uncertainty regarding its pathogenesis, provoking factors, optimal medical management, and long-term outcomes.2,12 Myocardial injury without definite MI, defined by a rise and/or fall in cardiac biomarkers that does not fulfill the Universal Definition criteria for MI, has also been increasingly recognized as a significant entity. Myocardial injury is well characterized in the post-operative period following non-cardiac surgery and is strongly associated with short-term mortality.3,13,14 The aim of the present study was to evaluate clinical characteristics, medical treatment, and intermediate-term cardiovascular outcomes of all patients admitted to a large urban Veterans Affairs (VA) hospital with abnormal cardiac biomarkers by myocardial injury and MI subtype.
Methods
All patients admitted to the United States Department of Veterans Affairs New York Harbor Healthcare System (a tertiary care hospital and regional referral center for cardiac surgery and percutaneous coronary intervention) from October 1, 2012 to October 31, 2013 with ≥1 abnormal serum cardiac troponin I (cTnI) laboratory values were identified by an automated electronic alert sent to the chief of cardiology. Plasma cTnI was measured using the Troponin-Ultra assay (Siemens Healthcare Diagnostics, Erlangen, Germany), with a normal reference range from 0.006 to 0.06 ng/mL. Per clinical protocol, all patients with ≥1 abnormal cTnI value were required to have a cardiology consultation within 24 hours of hospital admission. The study was approved by the VA New York Harbor Healthcare System Institutional Review Board with a waiver of informed consent.
Patients with a ≥20% rise and/or fall of cTnI were stratified by the presence of symptoms or signs of ischemia. Patients with symptoms or signs of ischemia were classified into MI subtypes 1 through 5 as per the Universal Definition of MI.1 Patients with myocardial injury without evidence of ischemia that occurred in a clinical scenario with a mismatch in oxygen supply and demand were classified as myocardial injury without definite MI. All other elevations in cTnI that did not meet criteria for MI and without a clinically evident mismatch in oxygen supply and demand were classified as non-specific elevations in troponin (e.g. chronic cTnI elevation in the setting of renal disease) and were excluded from the primary analysis. An algorithmic approach to classification of MI and myocardial injury is illustrated in the Supplemental Figure. Classification of myocardial injury and infarction was based on review of all clinical documentation, ECGs, cardiovascular imaging, and the impression of the consulting cardiologist.
Baseline, treatment, and outcome variables were collected by review of the medical record. Provoking conditions associated with a mismatch in myocardial oxygen supply and demand were identified. Conditions associated with decreased myocardial oxygen supply were hypotension, anemia, bradyarrhythmia, and respiratory failure. Tachycardia, tachyarrhythmias, severe hypertension, and sepsis were associated with increased myocardial oxygen demand. Hypotension was defined as a systolic blood pressure (SBP) <90 mm Hg or a mean arterial pressure (MAP) <65 mmHg. Anemia was defined as hemoglobin ≤7 g/dL or recent bleeding or hemorrhage. Respiratory failure was defined by the administration of high flow oxygen, application of non-invasive positive pressure ventilation, or urgent/emergent intubation with mechanical ventilation. Tachycardia and bradycardia were recorded as a provoking condition when the cardiac arrhythmia was suspected as an etiology of myocardial ischemia by the treating physician. Severe hypertension was defined as a SBP >180 mm Hg or a diastolic blood pressure (DBP) >110 mm Hg. Sepsis was defined as infectious illness meeting systemic inflammatory response syndrome criteria. Results of cardiovascular testing, including echocardiography and coronary angiography, were obtained. Obstructive CAD was defined as any lesion with ≥50% angiographic stenosis. Medications prescribed at hospital discharge were identified for surviving patients.
The primary outcomes of interest were defined as all-cause and cardiovascular mortality assessed through May 12, 2015 (median follow-up of 1.8 years). Secondary outcomes of interest included in-hospital mortality and hospital readmission to VA medical centers. Readmissions were further classified as hospitalization for MI and acute decompensated heart failure based on the primary indication for hospital admission as per clinical discharge documentation. All deaths were classified as cardiovascular or non-cardiovascular based on review of VA clinical documentation.
Normally distributed continuous data are displayed as mean ± standard deviation (SD) and compared using independent sample t-test. Skewed continuous data are presented as median [interquartile range] and compared using the Mann-Whitney test. Categorical variables are presented as n (proportion) and compared using Fisher exact or Chi-square tests. Kaplan-Meier curves were generated to depict intermediate-term survival, with between-group comparisons performed using the log rank test. Cox proportional hazard models were used to evaluate predictors of intermediate-term mortality after adjustment for demographic and key clinical variables. Models included age, sex, race, tobacco use, chronic obstructive pulmonary disease, hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease, end stage renal disease, prior myocardial infarction, prior coronary revascularization, heart failure, peripheral artery disease, malignancy, peak troponin during hospitalization, MI or myocardial injury subtype, and aspirin and statin prescription at hospital discharge as covariates. Two-sided P-values <0.05 were considered to be statistically significant for all tests. Statistical analyses were performed using SPSS 20 (IBM SPSS Statistics, Armonk, NY).
Results
Of the 768 patients admitted to the VA New York Harbor Healthcare System with ≥1 cTnI measurement above the 99% upper reference limit of the laboratory assay, 710 patients (92.4%) had a ≥20% rise and fall in cTnI. Within this cohort, 420 (59.2%) patients had myocardial injury and 290 (40.8%) met the Universal Definition criteria for MI. Among MI patients, type 1 MI was identified in 137 patients (47.2%), with 20 (14.6%) ST segment elevation MI (STEMI) and 117 (85.4%) non-ST segment elevation MI (NSTEMI), type 2 MI was identified in 146 patients (50.3%), and type 3, type 4, or type 5 MI was identified in 7 patients (2.4%). Among the 420 patients with myocardial injury without definite MI, myocardial injury was identified in 175 patients (41.7%) and non-specific elevation in troponin was identified in the remaining 245 patients (58.3%) (Supplemental Table 1). The final cohort for analysis consisted of 458 patients with type 1 MI, type 2 MI, or myocardial injury without definite MI.
Baseline demographics, clinical comorbidities, and clinical presentation of patients with type 1 MI, type 2 MI, or myocardial injury without definite MI are shown in Table 1. Overall, the average age was 73.5±12.4 years, 98.6% were male, and 56.8% were white. Cardiovascular risk factors were prevalent in all groups. Peak serum cTnI levels were higher among patients with type 1 MI than type 2 MI and higher among patients with type 2 MI than myocardial injury without MI. Patients with type 2 MI were less likely to have chest pain or ischemic symptoms than patients presenting with type 1 MI, but there was no difference in the proportions with ischemic ECG changes between these two groups. (Table 1)
Table 1.
Baseline Characteristics, Clinical Presentation, and Provoking Conditions
| Variable | Type 1 MI (n=137) |
Type 2 MI (n=146) |
Myocardial Injury (n=175) |
P1† | P2* |
|---|---|---|---|---|---|
| Baseline Characteristics | |||||
| Age, mean ± SD, y | 70.9 ± 12.7 | 74.3 ± 12.2 | 74.9 ± 12.2 | 0.02 | 0.67 |
| Male, n (%) | 130 (94.9) | 144 (98.6) | 170 (97.1) | 0.07 | 0.36 |
| Race, n (%) | 0.29 | 0.75 | |||
| White | 83 (60.6) | 82 (56.2) | 95 (54.3) | ||
| Black | 40 (29.2) | 54 (37.0) | 64 (36.6) | ||
| Other | 14 (10.2) | 10 (6.8) | 16 (9.1) | ||
| Tobacco Use (Former or Current), n (%) | 89 (65.0) | 96 (65.8) | 100 (57.1) | 0.89 | 0.12 |
| Chronic Obstructive Pulmonary Disease, n (%) | 31 (22.6) | 32 (21.9) | 42 (24.0) | 0.89 | 0.66 |
| Hypertension, n (%) | 118 (86.1) | 128 (87.7) | 149 (85.1) | 0.7 | 0.51 |
| Dyslipidemia, n (%) | 98 (71.5) | 102 (69.9) | 114 (65.1) | 0.75 | 0.37 |
| Diabetes Mellitus, n (%) | 61 (44.5) | 58 (39.7) | 73 (41.7) | 0.41 | 0.72 |
| Chronic Kidney Disease (eGFR<60), n (%) | 41 (29.9) | 41 (28.1) | 37 (21.1) | 0.73 | 0.15 |
| End Stage Renal Disease, n (%) | 7 (5.1) | 7 (4.8) | 12 (6.9) | 0.92 | 0.43 |
| Prior Myocardial Infarction, n (%) | 26 (19.0) | 28 (19.2) | 19 (10.9) | 0.92 | 0.04 |
| Prior Coronary Artery Bypass Surgery, n (%) | 21 (15.3) | 27 (18.5) | 15 (8.6) | 0.48 | 0.009 |
| Prior Percutaneous Coronary Intervention, n (%) | 31 (22.6) | 25 (17.1) | 20 (11.4) | 0.25 | 0.14 |
| Prior Heart Failure, n (%) | 61 (44.5) | 75 (51.4) | 63 (36.0) | 0.25 | 0.006 |
| Peripheral Artery Disease, n (%) | 13 (9.5) | 11 (7.5) | 6 (3.4) | 0.55 | 0.10 |
| History of Malignancy, n (%) | 30 (21.9) | 51 (34.9) | 63 (36.0) | 0.02 | 0.84 |
| Clinical Presentation | |||||
| Peak troponin (ng/mL), median (IQR) | 3.79 (0.54 – 11.60) | 0.34 (0.14 – 1.72) | 0.15 (0.10 – 0.40) | <0.001 | <0.001 |
| Universal Definition of MI Criteria, n (%) | |||||
| Chest pain and/or ischemic symptoms | 128 (93.4%) | 46 (31.5) | 0 (0) | <0.001 | - |
| Ischemic ECG changes^ | 89 (65.0%) | 85 (58.2) | 0 (0) | 0.24 | - |
| Imaging loss of viable myocardium OR new regional wall motion abnormality | 57 (41.6%) | 75 (51.4) | 0 (0) | 0.09 | - |
| Intracoronary thrombus (at angiography or autopsy) | 84 (61.3%) | 0 (0.0) | 0 (0) | <0.001 | - |
| Multiple criteria fulfilled | 91 (66.4%) | 66 (45.2) | 0 (0) | <0.001 | - |
| Provoking Conditions, n (%) | |||||
| Tachyarrhythmia | 0 (0) | 43 (29.5) | 67 (38.3) | - | 0.10 |
| Severe hypertension | 0 (0) | 29 (19.9) | 41 (23.4) | - | 0.44 |
| Sepsis | 0 (0) | 23 (15.8) | 35 (20.0) | - | 0.33 |
| Severe Anemia | 0 (0) | 29 (19.9) | 35 (20.0) | - | 0.92 |
| Hypotension | 0 (0) | 20 (13.7) | 27 (15.4) | - | 0.66 |
| Respiratory Failure | 0 (0) | 25 (17.1) | 23 (13.1) | - | 0.32 |
| Bradyarrhythmia | 0 (0) | 10 (6.8) | 9 (5.1) | - | 0.52 |
| Noncardiac Surgery | 0 (0) | 8 (5.5) | 30 (17.1) | - | 0.001 |
| Multiple provoking conditions | 0 (0) | 62 (42.5) | 70 (40.0) | - | 0.65 |
P1: P-value for the comparison of type 2 MI versus type 1 MI
P2: P-value for the comparison of type 2 MI versus myocardial injury
Includes ST segment changes, T-wave Inversions, new LBBB, Pathologic Q waves
Provoking conditions associated with type 2 MI and myocardial injury are shown in Table 1. Overall, tachyarrhythmia (34.3%), severe hypertension (21.8%), and anemia (19.9%) were the most common provoking conditions associated with a mismatch in myocardial oxygen supply and demand. Non-cardiac surgery was a provoking condition of myocardial injury or type 2 MI in 11.8% of cases. Among patients with any myocardial injury after non-cardiac surgery, only 21% (8/38) met the universal definition for type 2 MI. Multiple provoking conditions were identified in 41% of patients with type 2 MI or myocardial injury without definite MI.
The results of in-hospital cardiovascular diagnostics are shown in Table 2. Coronary angiography was more common among patients with type 1 MI versus type 2 MI (83.2% vs. 13.0%, p<0.0001), but not significantly different between type 2 MI and myocardial injury.
Table 2.
Cardiovascular diagnostic imaging and coronary revascularization
| Type 1 MI | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| All Type 1 MI (n=137) |
NSTEMI (n=117) |
STEMI (n=20) |
Type 2 MI (n=146) |
Myocardial Injury (n=175) |
P1† | P2* | |
| Transthoracic Echocardiography (in-hospital) | 114 (83.2) | 97 (82.9) | 17 (85.0) | 127 (87.0) | 115 (65.7) | 0.37 | 0.0001 |
| New Wall Motion Abnormalities | 60 (52.6) | 43 (44.3) | 17 (100.0) | 75 (59.1) | 0 (0) | 0.32 | 0.0001 |
| Coronary Angiography (within 90 days) | 114 (83.2) | 96 (82.1) | 18 (90.0) | 19 (13.0) | 19 (10.9) | 0.0001 | 0.55 |
| Multi-vessel CAD (stenosis >50%) | 24 (21.1) | 19 (19.8) | 5 (27.8) | 1 (5.3) | 1 (5.3) | 0.10 | 0.47 |
| Single vessel CAD (stenosis >50%) | 87 (76.3) | 74 (77.1) | 13 (72.2) | 14 (73.7) | 13 (68.4) | 0.81 | 0.72 |
| Non-Obstructive CAD | 3 (2.6) | 3 (3.1) | 0 (0.0) | 4 (21.1) | 5 (26.3) | 0.006 | 0.70 |
| Coronary Revascularization (within 90 days of admission) | |||||||
| Percutaneous Coronary Intervention | 53 (46.5) | 36 (37.5) | 17 (94.4) | 8 (42.1) | 8 (42.1) | 0.72 | 0.74 |
P1: P-value for the comparison of type 2 MI versus type 1 MI
P2: P-value for the comparison of type 2 MI versus myocardial injury
CAD: Coronary artery disease
At hospital discharge, survivors of type 1 MI were more likely to receive aspirin, statin, and dual antiplatelet therapy at discharge in comparison to type 2 MI patients. There was no significant difference in the proportion of survivors of type 2 MI that were prescribed aspirin, statin, and dual antiplatelet therapy compared to survivors of myocardial injury. (Table 3)
Table 3.
Discharge Therapy*
| Type 1 MI | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| All Type 1 MI (n=119) |
NSTEMI (n=104) |
STEMI (n=15) |
Type 2 MI (n=129) |
Myocardial Injury (n=159) |
P1† | P2* | |
| Aspirin | 101 (84.9) | 87 (83.7) | 14 (93.3) | 86 (66.7) | 107 (67.3) | 0.001 | 0.91 |
| Statin | 100 (84.0) | 86 (82.7) | 14 (93.3) | 83 (64.3) | 103 (64.8) | <0.001 | 0.94 |
| Aspirin + Statin | 92 (77.3) | 79 (76) | 13 (86.7) | 68 (52.7) | 83 (52.2) | <0.001 | 0.93 |
| P2Y12 inhibitor | 59 (49.6) | 46 (44.2) | 13 (86.7) | 33 (25.6) | 39 (24.5) | <0.001 | 0.84 |
| Aspirin + P2Y12 inhibitor^ | 58 (48.7) | 45 (43.3) | 13 (86.7) | 31 (24) | 36 (22.6) | <0.001 | 0.78 |
| Anticoagulant‖ | 11 (9.2) | 8 (7.7) | 3 (20.0) | 11 (8.5) | 10 (6.3) | 0.84 | 0.47 |
| Aspirin + P2Y12+ Anticoagulant | 8 (6.7) | 5 (4.8) | 3 (20.0) | 2 (1.6) | 2 (1.3) | 0.05 | 0.99 |
| ACEi / ARB | 63 (52.9) | 53 (51) | 10 (66.7) | 62 (48.1) | 76 (47.8) | 0.44 | 0.97 |
| Beta-Blocker | 78 (65.5) | 70 (67.3) | 8 (53.3) | 88 (68.2) | 94 (59.1) | 0.66 | 0.11 |
| Calcium Channel Blocker | 25 (21) | 22 (21.2) | 3 (20) | 32 (24.8) | 41 (25.8) | 0.48 | 0.85 |
Patients who expired in-hospital were excluded
Clopidogrel, Prasugrel, Ticagrelor
Warfarin. Enoxaparin, Apixaban, Rivaroxaban, Dabigatran
P1: P-value for the comparison of type 2 MI versus type 1 MI
P2: P-value for the comparison of type 2 MI versus myocardial injury
ACEi: Angiotensin-converting-enzyme inhibitor, ARB: Angiotensin receptor blocker
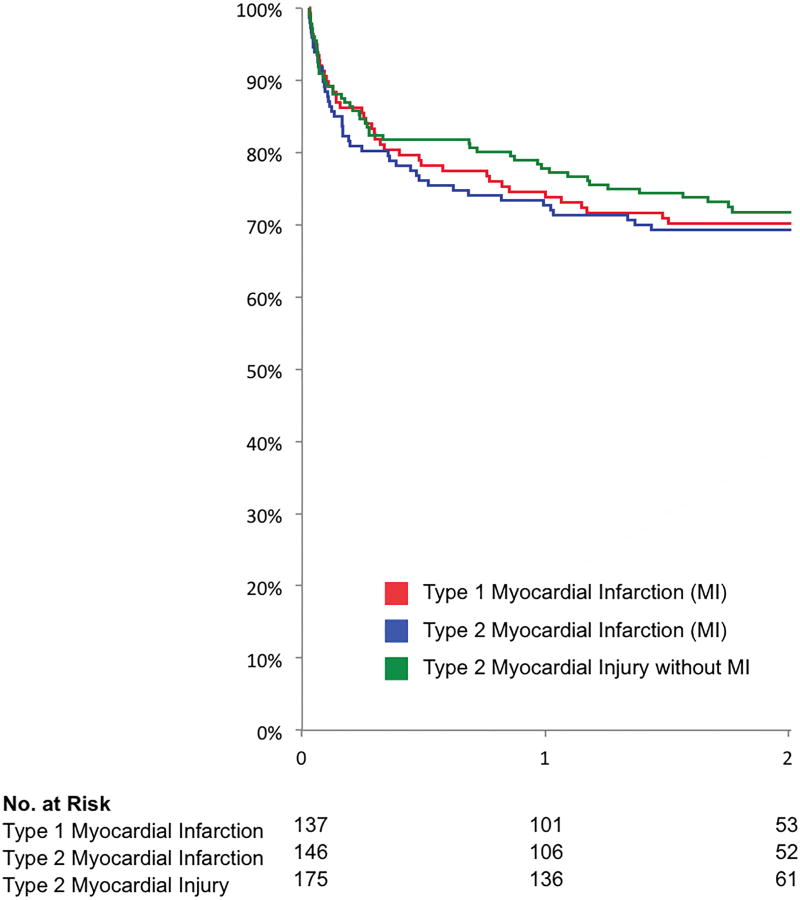
Clinical outcomes for the study cohort are shown in Table 4. Among patients with type 1 MI, type 2 MI, or myocardial injury, 138 deaths (30.1%) occurred over 705 patient-years of follow-up (median 1.82 years [IQR 0.97–2.14]). No difference in all-cause mortality was observed for patients with type 1 MI versus type 2 MI, or for type 2 MI versus myocardial injury (overall log-rank p=0.94) (Table 4; Figure 1). A significant proportion of deaths were attributed to cardiovascular causes in each subgroup (type 1 MI: 34.1%, type 2 MI: 17.8%, myocardial injury: 30.8%. (Table 4). In Cox proportional hazards models adjusted for demographics and cardiovascular risk factors, type 1 MI, type 2 MI, and myocardial injury without definite MI were each associated with a similar hazard for all-cause mortality and cardiovascular mortality at intermediate-term follow-up. Characteristics of patients with type 2 MI and myocardial injury who did and did not survive intermediate term follow-up are shown in Supplemental Tables 2 & 3. In a pooled analysis of patients with type 2 MI and myocardial injury who survived the index hospitalization, prescriptions of statin and angiotensin-converting-enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB) were less frequent among patients who died during intermediate-term follow up (Supplemental Table 4).
Table 4.
Clinical Outcomes
| Type 1 MI | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| All Type 1 MI (n=137) |
NSTEMI (n=117) |
STEMI (n=20) |
Type 2 MI (n=146) |
Myocardial Injury (n=175) |
P1† | P2* | |
| In-Hospital Mortality | 18 (13.1) | 13 (11.1) | 5 (25.0) | 17 (11.6) | 16 (9.1) | 0.70 | 0.46 |
| Cardiovascular Death | 8 (44.4) | 4 (30.8) | 4 (80.0) | 3 (17.6) | 4 (25.0) | 0.18 | 0.69 |
| Non-cardiovascular Death | 10 (55.6) | 9 (69.2) | 1 (20.0) | 14 (82.4) | 12 (75.0) | - | - |
| In-hospital or 30-Day Mortality | 21 (15.3) | 15 (12.8) | 6 (30.0) | 22 (15.1) | 23 (13.1) | 0.92 | 0.62 |
| Cardiovascular Death | 9 (42.9) | 4 (26.7) | 5 (83.3) | 6 (27.3) | 7 (30.4) | 0.45 | 0.92 |
| Non-cardiovascular Death | 11 (52.4) | 10 (66.7) | 1 (16.7) | 15 (68.2) | 15 (65.2) | - | - |
| Unknown Cause of Death | 1 (4.8) | 1 (6.7) | 0 (0.0) | 1 (4.5) | 1 (4.3) | - | - |
| All-Cause Mortality on intermediate-term follow-up | 41 (29.9) | 33 (28.2) | 8 (40.0) | 45 (30.8) | 52 (29.7) | 0.86 | 0.82 |
| Cardiovascular Death | 14 (34.1) | 8 (24.2) | 6 (75.0) | 8 (17.8) | 16 (30.8) | 0.08 | 0.14 |
| Non-cardiovascular Death | 22 (53.7) | 21 (63.6) | 1 (12.5) | 29 (64.4) | 30 (57.7) | 0.31 | 0.50 |
| Unknown Cause of Death | 5 (12.2) | 4 (12.1) | 1 (12.5) | 8 (17.8) | 6 (11.5) | 0.47 | 0.38 |
| All Cause Readmission | 57 (41.6) | 49 (41.9) | 8 (40.0) | 62 (42.5) | 80 (45.7) | 0.89 | 0.56 |
| Readmission for Myocardial Infarction | 19 (33.3) | 17 (34.7) | 2 (25.0) | 13 (21.0) | 8 (10.0) | 0.19 | 0.11 |
| Readmission for Heart Failure | 12 (21.1) | 10 (20.4) | 2 (25.0) | 15 (24.2) | 19 (23.8) | 0.84 | 0.89 |
| Death or Myocardial Infarction | 54 (39.4) | 44 (37.6) | 10 (50.0) | 52 (35.6) | 57 (32.6) | 0.59 | 0.65 |
P1: P-value for the comparison of type 1 MI versus type 2 MI
P2: P-value for the comparison of type 2 MI versus myocardial injury
Figure 1. Survival of patients with type 1 MI, type 2 MI and myocardial injury without definite MI.
Overall log-rank P-value = 0.94 for 3-way comparison. Log-rank p-value = 0.81 for type 1 MI vs. type 2 MI; log-rank p-value = 0.74 for type 2 MI vs. myocardial injury.
Among patients who survived to hospital discharge, a total of 199 patients (62.1%) were re-hospitalized at a VA healthcare facility over the course of follow-up. Rates of all-cause rehospitalization, rehospitalization for heart failure, and re-hospitalization for MI were high in patients with type 1 MI, type 2 MI and myocardial injury during intermediate-term follow-up (Table 4).
Discussion
In this study of patients who presented to a large VA tertiary care hospital in New York City, a greater proportion of patients with type 1 MI underwent coronary angiography and received guideline-directed medical therapy (GDMT) for CAD at discharge as compared to those with type 2 MI or myocardial injury without MI. After 1.8 years of follow-up, no significant differences in intermediate-term all-cause mortality were identified among patients with type 2 MI and myocardial injury in comparison to type 1 MI, even after multivariable adjustment for demographics, clinical presentation, and discharge medications.
Clinical features were similar among patients with type 2 MI and myocardial injury without definite MI, suggesting a considerable overlap between these diagnoses. Since distinctions between type 2 MI and myocardial injury are particularly challenging when clinical symptoms of ischemia cannot be reliably detected, such as after surgery, proposals for a revised Universal Definition of type 2 MI have garnered increased attention.3,13,15
Among patients who survived the index hospitalization, patients with type 2 MI and myocardial injury were less likely to receive GDMT for CAD, including aspirin or statin, than patients with type 1 MI. These data suggest that clinical providers remain uncertain regarding the benefits of conventional GDMT in the treatment of myocardial injury or infarction precipitated by mismatch in myocardial oxygen supply and demand. Similarly, few patients with type 2 MI (13.0%) and myocardial injury (10.9%) underwent coronary angiography, and both groups were less likely to undergo coronary angiography than type 1 MI (83%). This may reflect advanced age, a higher burden of concomitant non-cardiac illness, or lower cTnI values in patients with type 2 MI or myocardial injury in comparison to patients presenting with type 1 MI. However, rates of percutaneous coronary interventions were similar among patients with type 1 MI, type 2 MI, and myocardial injury who were referred for angiography. This suggests that type 2 MI and myocardial injury patients may be under-referred for invasive evaluation of CAD, and there may be a large burden of under-diagnosed CAD in these subgroups. Still, it remains uncertain whether differences in diagnostic cardiovascular testing and GDMT negatively impact patients with type 2 MI and myocardial injury.
Outcomes for patients with type 2 MI and myocardial injury in this analysis were poor, with approximately 10% in-hospital mortality, and 30% all-cause mortality at a median of 1.8-years follow-up. These data are comparable to prior reports of long-term outcomes after type 2 MI.5,7 Importantly, all-cause mortality did not differ between MI subtypes in the present analysis, and rates of cardiovascular morbidity and mortality were high in all groups. Although a few prior studies have also reported no significant differences in outcomes among MI subtypes,16,17 others report significantly higher long-term mortality in patients with type 2 MI than those with type 1 MI.5,7,18–20 Many of these studies were conducted outside the US with relatively small cohorts.5,19,20 A larger study comparing outcomes of MI subtypes at a single center in the United Kingdom reported a higher risk of death in the type 2 versus type 1 MI cohorts at 1 year. However, patients with type 1 MI outnumbered those with type 2 MI by nearly 3:1, suggesting the practice patterns of cTnI measurement in type 2 MI settings at international centers may differ substantially from those at the VA New York Harbor Healthcare System.7
Explanations for poor intermediate-term outcomes observed in patients with type 2 MI and myocardial injury without definite MI remain speculative. Troponin elevation in the absence of unstable coronary artery disease may reflect the presence of significant stable coronary artery disease (i.e. left main or triple-vessel CAD), which may be under-diagnosed and under-treated. Alternatively, troponin elevations may simply reflect the burden of non-cardiovascular illness, which may be a primary driver of adverse outcomes and mortality in the long term. Additional studies are necessary to determine the underlying mechanisms of troponin elevation in these syndromes and their strong associations with survival.
There are a few notable limitations to the present study. Although clinical data and ECGs were available for in-depth medical record review, misclassification bias is possible, especially regarding the subtle distinctions between type 2 MI, myocardial injury without definite MI, and non-specific elevations in troponin. Indeed, lower use of echocardiography in myocardial injury may represent a missed opportunity to identify new wall motion abnormalities consistent with type 2 MI. However, as an ongoing institutional quality initiative, all patients with ≥1 abnormal cTnI were prospectively evaluated by a consultant in cardiovascular disease to determine the mechanism of myocardial injury. Still, variability in clinical presentations and perceived severity of illness may bias approaches to treatment, particularly among patients with type 2 MI and myocardial injury. Second, although the VA New York Harbor Health Care System serves a large and diverse urban area, the sample size of patients with an abnormal cTnI was relatively small, and few patients with STEMI were included. However, given the high-risk nature of the population, the number of adverse events, including death, was high. Third, due to the demographics of the overall population of military veterans, few women were included in this analysis. Fourth, despite the availability of intermediate-term mortality, data from non-VA facilities on re-hospitalization or subsequent cardiovascular testing was not available for analysis, and as a consequence, rehospitalization rates may be underreported.
Conclusion
In conclusion, among patients admitted to an urban VA hospital network, an abnormal rise and fall of cTnI was attributed to type 2 MI or myocardial injury without definite MI in 45% of cases. Patients with type 2 MI and myocardial injury without definite MI were less likely to receive guideline-directed medical therapy for CAD than patients with type 1 MI. No significant differences in intermediate-term all-cause mortality between patients with type 1 MI, type 2 MI and myocardial injury were observed, even after multivariable adjustment for demographics, clinical covariates, and medical therapy. Rates of cardiovascular morbidity and mortality were high in all subgroups. Ultimately, additional studies to determine long-term benefits of intensive GDMT and coronary revascularization for atherosclerotic cardiovascular disease in the high-risk population of patients with type 2 MI and myocardial injury are warranted.
Supplementary Material
Acknowledgments
Sponsor: None / Investigator-initiated.
Funding: None / Investigator-initiated
Binita Shah, MD is supported in part by the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development (I01BX007080).
Footnotes
Disclosures: The authors report no relationships that could be construed as a conflict of interest.
References
- 1.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012 Oct 16;60(16):1581–1598. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Smilowitz NR, Naoulou B, Sedlis SP. Diagnosis and management of type II myocardial infarction: increased demand for a limited supply of evidence. Current atherosclerosis reports. 2015 Feb;17(2):478. doi: 10.1007/s11883-014-0478-1. [DOI] [PubMed] [Google Scholar]
- 3.Smilowitz NR, Weiss MC, Mauricio R, et al. Provoking conditions, management and outcomes of type 2 myocardial infarction and myocardial necrosis. International journal of cardiology. 2016 Sep 1;218:196–201. doi: 10.1016/j.ijcard.2016.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melberg T, Burman R, Dickstein K. The impact of the 2007 ESC-ACC-AHA-WHF Universal definition on the incidence and classification of acute myocardial infarction: a retrospective cohort study. International journal of cardiology. 2010 Mar 18;139(3):228–233. doi: 10.1016/j.ijcard.2008.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Saaby L, Poulsen TS, Diederichsen AC, et al. Mortality rate in type 2 myocardial infarction: observations from an unselected hospital cohort. Am J Med. 2014 Apr;127(4):295–302. doi: 10.1016/j.amjmed.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 6.Saaby L, Poulsen TS, Hosbond S, et al. Classification of myocardial infarction: frequency and features of type 2 myocardial infarction. Am J Med. 2013 Sep;126(9):789–797. doi: 10.1016/j.amjmed.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 7.Shah AS, McAllister DA, Mills R, et al. Sensitive troponin assay and the classification of myocardial infarction. Am J Med. 2015 May;128(5):493–501. e493. doi: 10.1016/j.amjmed.2014.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stein GY, Herscovici G, Korenfeld R, et al. Type-II myocardial infarction--patient characteristics, management and outcomes. PloS one. 2014;9(1):e84285. doi: 10.1371/journal.pone.0084285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonaca MP, Wiviott SD, Braunwald E, et al. American College of Cardiology/American Heart Association/European Society of Cardiology/World Heart Federation universal definition of myocardial infarction classification system and the risk of cardiovascular death: observations from the TRITON-TIMI 38 trial (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis in Myocardial Infarction 38) Circulation. 2012 Jan 31;125(4):577–583. doi: 10.1161/CIRCULATIONAHA.111.041160. [DOI] [PubMed] [Google Scholar]
- 10.White HD, Reynolds HR, Carvalho AC, et al. Reinfarction after percutaneous coronary intervention or medical management using the universal definition in patients with total occlusion after myocardial infarction: results from long-term follow-up of the Occluded Artery Trial (OAT) cohort. Am Heart J. 2012 Apr;163(4):563–571. doi: 10.1016/j.ahj.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baron T, Hambraeus K, Sundstrom J, et al. Type 2 myocardial infarction in clinical practice. Heart. 2015 Jan;101(2):101–106. doi: 10.1136/heartjnl-2014-306093. [DOI] [PubMed] [Google Scholar]
- 12.Alpert JS, Thygesen KA, White HD, Jaffe AS. Diagnostic and therapeutic implications of type 2 myocardial infarction: review and commentary. Am J Med. 2014 Feb;127(2):105–108. doi: 10.1016/j.amjmed.2013.09.031. [DOI] [PubMed] [Google Scholar]
- 13.Alpert JS, Thygesen KA. The Case for a Revised Definition of Myocardial Infarction-The Ongoing Conundrum of Type 2 Myocardial Infarction vs Myocardial Injury. JAMA Cardiol. 2016 Jun 01;1(3):249–250. doi: 10.1001/jamacardio.2016.0543. [DOI] [PubMed] [Google Scholar]
- 14.Writing Committee for the VSI. Devereaux PJ, Biccard BM, et al. Association of Postoperative High-Sensitivity Troponin Levels With Myocardial Injury and 30-Day Mortality Among Patients Undergoing Noncardiac Surgery. JAMA. 2017 Apr 25;317(16):1642–1651. doi: 10.1001/jama.2017.4360. [DOI] [PubMed] [Google Scholar]
- 15.Sandoval Y, Apple FS, Smith SW. Type 2 myocardial infarction. Potential hazards of nomenclature systems: user discretion advised. International journal of cardiology. 2015 Jan 20;179:373–374. doi: 10.1016/j.ijcard.2014.11.056. [DOI] [PubMed] [Google Scholar]
- 16.Gaggin HK, Liu Y, Lyass A, et al. Incident Type 2 Myocardial Infarction in a Cohort of Patients Undergoing Coronary or Peripheral Arterial Angiography. Circulation. 2016 Nov 21;135(2):116–127. doi: 10.1161/CIRCULATIONAHA.116.023052. [DOI] [PubMed] [Google Scholar]
- 17.Etaher A, Chew D, Redfern J, et al. Suspected ACS Patients Presenting With Myocardial Damage or a Type 2 Myocardial Infarction Have a Similar Late Mortality to Patients With a Type 1 Myocardial Infarction: A Report from the Australian and New Zealand 2012 SNAPSHOT ACS Study. Heart, lung & circulation. 2016 Dec 31; doi: 10.1016/j.hlc.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Winchester DE, Burke L, Agarwal N, Schmalfuss C, Pepine CJ. Predictors of short- and long-term mortality in hospitalized veterans with elevated troponin. Journal of hospital medicine. 2016 Nov;11(11):773–777. doi: 10.1002/jhm.2619. [DOI] [PubMed] [Google Scholar]
- 19.Cediel G, Gonzalez-Del-Hoyo M, Carrasquer A, Sanchez R, Boque C, Bardaji A. Outcomes with type 2 myocardial infarction compared with non-ischaemic myocardial injury. Heart. 2016 Oct 14; doi: 10.1136/heartjnl-2016-310243. [DOI] [PubMed] [Google Scholar]
- 20.Landes U, Bental T, Orvin K, et al. Type 2 myocardial infarction: A descriptive analysis and comparison with type 1 myocardial infarction. Journal of cardiology. 2016 Jan;67(1):51–56. doi: 10.1016/j.jjcc.2015.04.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.