Abstract
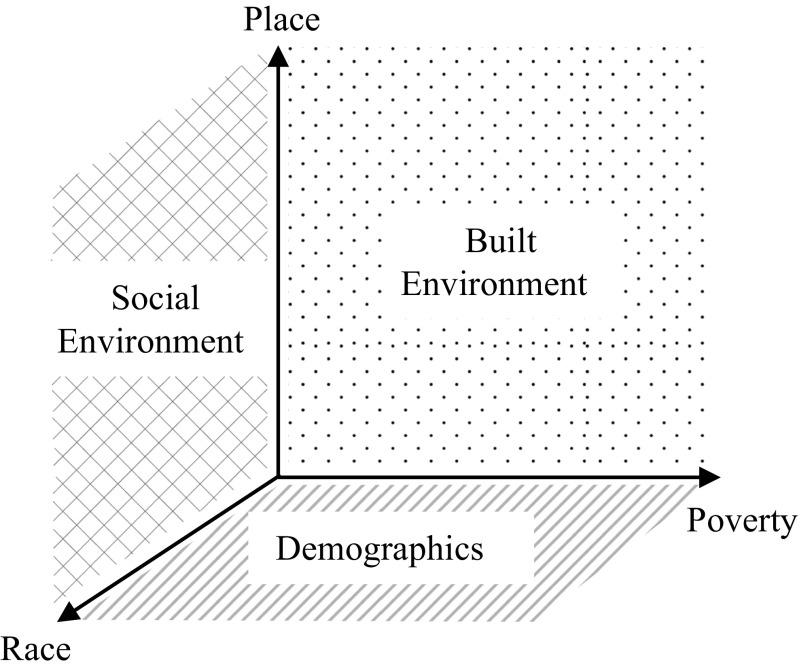
Intimate connections among race, place, and poverty are increasingly featured in the health disparities literature. However, few models exist that can guide our understanding of these interconnections. We build on the Chicago School of Sociology’s contributions in urban research and one of its contemporary elaborations, often described as the “neighborhood effects approach,” to propose a three-axis model of health inequity. This model, in alignment with Chicago School theory, postulates a dynamic and adaptive relationship between spatial context and health inequity. Compositional axes of race and poverty form the foundation of the model. These compositional axes then intersect with a third axis of place to compose the built and social environment planes. We develop this model to provide conceptual guidance for clinical, policy, and public health researchers who aim to examine how these three features, taken together, have important implications for urban health.
Keywords: Health inequity, Health disparities, Racial and ethnic disparities, Chronic disease, Place, Neighborhood effects, Urban sociology
Introduction
Public health crises, such as the Chicago heat wave (1995) and the Flint water crisis (2014), powerfully illustrate the confluence of race, place, and poverty in determining health outcomes. The 1995 Chicago heat wave was responsible for 739 deaths in 5 days [1] and has been immortalized by Eric Klinenberg as the perfect storm of concentrated poverty, deteriorating housing conditions, and the social and residential isolation of aging racial minorities [1]. Similarly, the Flint water crisis has been estimated to have exposed over 100,000 residents to high levels of lead, resulting from decades of economic decline, infrastructure decay, and organizational failure in a city that is predominantly black and poor [2].
These events are notable case studies, but they are singularly placed—that is, they occurred in a fixed spatial context under delimited historical circumstances. However, many contemporary public health crises, such as the obesity and diabetes epidemics, can be more difficult to conceptualize because of their diffuse spatial contexts and innumerable potential determinants. In Baltimore, Maryland, a black man is 50% more likely to die from diabetes than his white counterpart; just 40 miles away in Washington D.C., that same black man is nearly 300% more likely to die from diabetes [3]. This stark disparity challenges assumptions about shared experiences of disease across diverse spatial contexts and settings—what does it mean to be a black man with diabetes in America? In the world? It is in this latter category of ubiquitous global epidemics that definitions of place and its uses in the literature become increasingly haphazard and vague, thus limiting opportunities for comparative work.
Place, as most commonly defined in the public health literature, refers to the neighborhood or geography-based attributes that influence a person’s health exposures, attitudes, behaviors, and outcomes [4]. However, prior research in health has implemented a relatively simplistic approach for describing its connections to race and poverty. In many studies, place is conceptualized as a third variable (e.g., urban vs. rural) [5], static in its interactions with race and poverty. For instance, a traditional analysis of race, place, and poverty in the health literature might examine US Census data to determine poverty rates by race and their distribution across urban, suburban, and rural geographies. In this example, place is an inert construct used to organize driving compositional variables (i.e., race and poverty). This perspective has led scholars to question the validity of urban-rural classifications in health-related research [6–8]. In other work, place (i.e., context) and the people who live there (i.e., composition) are perceived as independent and often competing explanations for health inequity, without consideration for the relational and mutually reinforcing dynamic between these factors [9, 10]. Scholars have thus called for more work to reconfigure conventional understandings of place in favor of more adaptive models [9, 10].
We developed a three-axis model to articulate an agile and easily applied theoretical framework for understanding the intricacies of how race, place, and poverty dynamically converge to influence health across manifold spatial contexts and circumstances.
The Chicago School and a Neighborhood Effects Approach
The Chicago School of Sociology and its early focus on urban context put forth a place-based approach to the study of spatial context. These scholars focused their efforts on sociological phenomena such as crime, concentrated poverty, and racial integration. This approach was applied to health and related fields as early as the 1960s [11, 12], an era often described as the “Second Chicago School.” However, application of the Chicago School, specifically to the study of health inequity in urban spatial contexts, is a relatively contemporary development. Robert Sampson, in his contemporary elaboration, describes the neighborhood effects approach and its application to health, arguing that a “durable spatial logic” ultimately organizes and mediates processes by which health is determined [4]. Importantly, this approach investigates “how things hang together,” in direct contrast to a variable-based approach, which investigates “how things split apart.” [4] Thus, the Chicago School fundamentally opposes the reductionism of neighborhood effects into driving compositional variables [13–15]. “Neighborhood difference” (e.g., differences in poverty) is not autonomous from the individuals who experience those differences, and people react and respond to their surroundings by constituting practices, perceptions, relationships, and behaviors that are spatially defined [4]. It is the dynamism of these interactions between race, place, and poverty that perpetuates enduring health inequity.
Place is thus seen as a local phenomenon, predominantly captured in neighborhoods and street-level units, rather than at county, state, or national level units. The Chicago School advocates for analysis at the smallest unit of geographic variation [13–15], sometimes referred to as small area variation in related literature [16, 17]. This theory of analysis emphasizes local neighborhood effects that occur in a spatially-bounded fashion—that is, in opposition to growing speculation about the erasure of physical boundaries due to globalization, residential mobility, and information technology spread (e.g., social media) [4]. People are, after all, physical creatures that must eat, work, play, and sleep in physical spaces. In Great American City, Sampson argues that “social ecological differentiation is everywhere… (and) fascination with globalization has tended to deflect attention from the persistence of local variation, concentration, and the spatial logic of inequality.” [4] Contemporary scholars have also described social disorganization theory and its applications to health, arguing that key features of neighborhood disadvantage influence health through localized, social processes [18, 19]. In general, the notion of the dynamic and animated street and surrounding neighborhood could have pro-social or anti-social implications, affecting social interaction and resulting ties.
A Three-Axis Model
We propose a three-axis model (Fig. 1) to conceptualize race, place, and poverty, building on theory and findings from the neighborhood effects literature. This model uses a constrained-choice approach to understanding health inequity [20], which asserts that human behavior remains highly constrained by social and spatial factors. As such, each behavioral choice can be visualized in our model as a single point in three-dimensional space (Fig. 1), with forces pushing and pulling from every axis and plane. Although rapid modernization and technological advancement in the twenty-first century may portend the illusion of infinite choice, day-to-day decision-making still occurs within physical bodies and local contexts, especially for those who have disproportionately limited resources and opportunities [4, 20].
Fig. 1.
A three-axis model of health inequity
Compositional variables of race and poverty are depicted as axes and form the foundation of our model (Fig. 1), because people experience their neighborhoods based on sociodemographic differences that are frequently fixed in time and space. Our model can be applied to the experiences of both individuals and groups, as constraints on human behavior can occur at both levels. At the individual level, there are clear and obvious ways in which race and poverty can determine a person’s daily health choices and behaviors. For instance, low socioeconomic status can be associated with food insecurity and rationing, leading individuals to choose low-cost, high-calorie foods with a greater shelf life, thus precipitating poor metabolic control [21]. Alternatively, perceived racial discrimination and distrust of the health care system can lead to avoidance of routine preventive care and delays in clinical diagnosis [22]. At the group level, racially discriminatory policing practices can mean that people of color experience high levels of chronic stress and cumulative allostatic load [23, 24].
These processes, amplified by place, can lead to constraints on health choices and behaviors that are spatially ordered. In urban contexts, where physical sorting often occurs along lines of racial and economic similarity, disadvantage can become concentrated and thereby constrain choice along physical boundaries. For instance, a person of color with low economic status may live in a high-poverty neighborhood with predominantly poor neighbors. However, the Chicago School contends that these processes extend beyond merely neighborhood deprivation [4]. As previously described, people react and respond to their surroundings, generating a host of mechanisms that can further accentuate privilege or disadvantage. For example, perceived discrimination and communication barriers among non-English speaking immigrants may lead to social isolation and further concentration of poverty, additionally cultivating poor health literacy and related health problems [25]. These responses thus interact with place to compose the built environment and social environment planes (Fig. 1) that further constrain or enable health.
The built environment refers to the physical spaces or structures created by people for day-to-day use, including grocery stores, health care facilities, local businesses, and physical infrastructure (e.g., roadways) [26]. This plane, most proximally operationalized from axes of place and poverty, builds on social disorganization theory, which underscores the impact of structural or physical disadvantages (e.g., poor access to resources, physical decay) that constrain choice and lead to deleterious outcomes [19]. Limited access to health-enabling resources, such as grocers, fitness centers, and pharmacies, generates a “friction of distance,” whereby disadvantaged groups pay additional travel costs to make healthy choices [20]. It is important to note that this plane (i.e., the built environment), derived from place-poverty axes, can also interface with race-place axes in meaningful ways. For instance, recent studies have described retail redlining, a discriminatory practice whereby businesses and services forego investing in certain neighborhoods based on their racial or ethnic composition, rather than economic prospects [27]. Such practices, which can severely limit access to health-enabling resources in communities of color, illustrate a pathway by which race can serve as a lever of neighborhood disadvantage and consequent health outcomes.
The social environment refers to the immediate social setting in which people live, including interpersonal behaviors, cultures, and attitudes (e.g., social cohesion, informal social control, distrust of institutions) [4, 28]. This plane builds on aspects of social disorganization theory related to residential segregation by race, social disadvantage, and loss of informal social control [19, 29]. Drawing from this early work, scholars suggest that the ordering of diverse groups via segregation into disadvantaged communities—with already limited health-related knowledge and influence—can lead to a meaningful disconnect from the larger urban experience [20, 30]. Residents thus belong to closed social networks by which information sharing may propagate false narratives about health (e.g., “fruit is not real sugar”), erode trust within the community, and further limit personal control over future health outcomes [20]. Alternatively, unhealthy social norms (e.g., poor dietary practices, tobacco use) can constrain personal choices by way of social context: if an individual wishes to eat healthily, but his mother prepares a traditionally Southern diet of fried pork, roasted potatoes, and sweet tea, he might pay an additional social cost to instead choose healthier options.
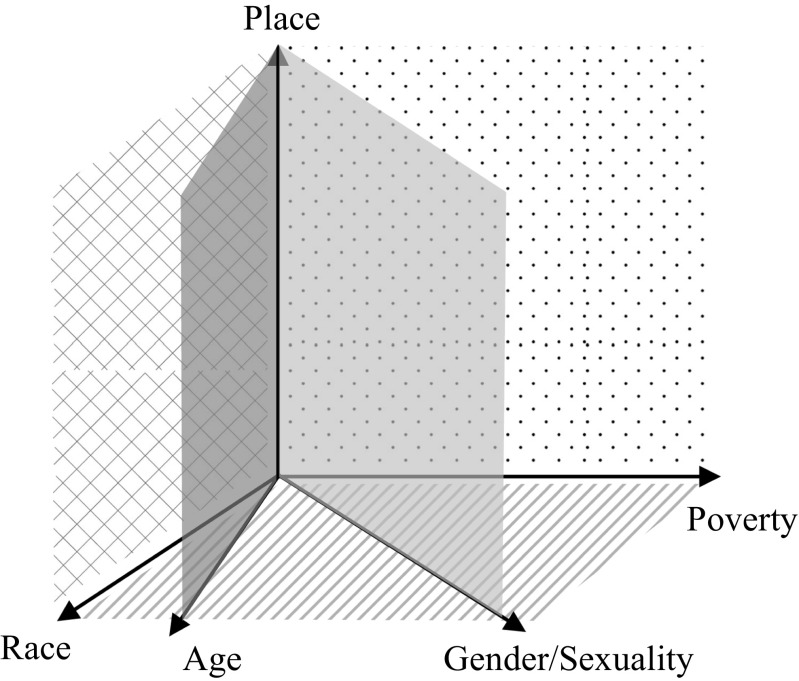
Our model adopts a three-axis approach as meaningfully representative of the most critical, real-world drivers of health inequity. However, it is important to note that additional compositional axes (e.g., education level, gender/sexuality, age) can similarly interact with place, thus constituting multinomial planes of shared experience and “neighborhood effects” (Fig. 2). For instance, studies of HIV transmission in communities of high-risk men who have sex with men (MSM) may adapt our model to include axes of race, place, and gender/sexuality. Alternatively, an examination of what it means to age in poverty may adapt our model to include axes of race, age, place, and poverty.
Fig. 2.
Multinomial planes of neighborhood effects
Finally, we specifically denoted each of our principal constructs—race, place, and poverty—as a directional axis in our model to depict a scalar component. This depiction of scale has implications for both local and globalizing forces in the twenty-first century. As racial and economic inequities grow across enlarging spatial contexts, there is expansion of the three-dimensional matrix (Fig. 1) in which healthy lifestyle choices arise. As Thomas Frieden theorizes, the best public health interventions are those by which healthy decisions become default or automated [31]. Our model suggests that as the magnitude of inequity intensifies along each axis, healthy lifestyle choices become less and less automated due to growing uncertainty in an expanding decision matrix. For example, someone from an affluent community may default to healthier dietary choices due to an abundance of high-quality, organic grocery stores and fewer financial limitations. However, as the gradient of inequality extends along each axis, nutritional decisions are constrained within a matrix of competing forces. As economic inequality increases along the poverty axis, individual financial concerns may lead to a propensity for processed foods with a longer shelf life, making fresh food purchases less common. As space expands along the place axis, healthy food choices become more unstable in the context of enlarging food deserts, increasing travel distances, and widespread retail redlining. Globalizing social forces (e.g., social media) are a relatively new phenomenon and remain poorly understood in the health literature [32]. However, the notion of uncertainty is only fortified by conceptualizing virtual spaces along an infinite directional axis, inviting an expanding deluge of new decision points and unknowns.
Practical Applications
Our three-axis model postulates a dynamic relationship between race, place, and poverty that should be taken together when analyzing spatial contexts and health inequity. Public health efforts to understand poor dietary practices in low-income neighborhoods constitute a prime illustration of how our model can be applied. For instance, studies examining the built environment and health have postulated a relatively straightforward relationship between access to healthy foods and obesity-related disease. However, in the context of numerous studies with mixed or negative findings [33], recent studies have explored more nuanced relationships between personal demographics, neighborhood effects, and choice [34, 35].
One recent study compared potential access to healthy foods (proximity to nearby grocers) with realized access to healthy foods (proximity to utilized grocers) and found that many residents in high-poverty neighborhoods chose to bypass nearby grocers to use grocers that were farther away [36]. Moreover, bypassing nearby grocers was associated with a higher body mass index [36]. Residents chose to pay a “travel cost,” despite the availability of more proximal food resources, suggesting that choice was not strictly a function of geographic access. Thus, a model examining the built environment and geographic access alone would be insufficient to capture the full range of explanatory mechanisms that meaningfully affect dietary patterns and obesity status. Indeed, the built environment constitutes a single plane in our three-axis model (Fig. 1), with additional levers informing choice from numerous directions. In this particular study, investigators elicited open-ended responses from participants to capture their reasons for bypassing nearby grocers. Preference (“I don't like the brands there”), safety (“There are bad folks who hang in the parking lot”), and cost (“I can buy in bulk for cheaper”) were among participant responses that signified additional reasons and sociocultural influences in driving choice [36].
Another study, analyzing nationally representative data, found that community racial and ethnic composition was associated with obesity status, but only under certain individual-level conditions [37]. For instance, people living in a predominantly Hispanic community were more likely to be obese—but only if they themselves were Hispanic or white, and not if they were non-Hispanic black. Researchers concluded that in addition to the built environment characteristics that influence obesity status in a given neighborhood, personal identification with or acculturation to a community’s sociocultural environment may also play a role in influencing obesity status [37]. These studies illustrate the importance of conceptualizing race, place, and poverty as a dynamic, three-dimensional model of socioecological influences, rather than a flat, static model of causative influences.
Implementation of the model will require more flexible study designs that allow for innovative statistical analyses. For example, Gaskin and colleagues developed a race-place-poverty gradient to examine its relationship with diabetes prevalence [38]. In addition to examining binary relationships within the individual and neighborhood levels (e.g., neighborhood racial composition and neighborhood poverty concentration), they built models to examine race-place, poverty-place, and race-place-poverty combinations to account for interactions between and among levels (e.g., individual race/neighborhood racial composition, individual race/individual poverty/neighborhood poverty concentration). They found that adults living in poor neighborhoods had higher rates of diabetes than adults in non-poor neighborhoods. However, after implementing a gradient approach, they unveiled an important nuance: black adults living in a poor neighborhood had similar rates of diabetes regardless of individual poverty status, but non-poor whites were able to mollify the harmful health effects of living in a poor neighborhood [38]. Although Gaskin and colleagues did not explicitly propose a conceptual model in this work, their analytical approach implicitly underscores a relational and non-binary dynamic between composition (i.e., race and poverty) and context (i.e., place) [10]. Other techniques such as spatial regression, use of spatial lags, and agent-based modeling will also be important applications to this field [39]. These types of novel methodologies are emerging and will be critical for elucidating the granular relationships expressed in our model.
The three-axis model of health inequity portrays intersecting influences of race, place, and poverty on environmental exposures (i.e., the built and social environment), health choices, and, ultimately, health status. As depicted by our model, an analysis of spatial context and health inequity capitulates a complicated narrative—one that necessitates a clear and adaptive framework to guide meaningful inquiry.
Conclusions
Research examining the impact of race, place, and poverty is increasingly salient in the public health literature, making it imperative that a robust theoretical framework exists to center the conversation on shared meanings and definitions. We build on the Chicago School’s framework for the central role of neighborhood context and propose a three-axis model as a way to depict key concepts in the extant literature and guide future research. In a political discourse that is increasingly fraught with false dichotomies positing race against poverty, we also hope to shift the conversation to contend with the nuance of race and poverty in dynamic spatial contexts. Disparities in health continue to widen—predictably—in some of the most segregated and disadvantaged communities in the USA. As public health crises center on preventable chronic conditions in the twenty-first century, a clear understanding of place, and its relationship to race and poverty, will be the cornerstone for eradicating health inequity.
Acknowledgements
This manuscript was supported by the Chicago Center for Diabetes Translation Research (CCDTR), NIDDK grant P30DK092949. E. Tung was also supported by the AHRQ Patient-Centered Outcomes Research (PCOR) Institutional Mentored Career Development Program (K12), AHRQ grant 5K12HS023007. E. Tung takes full responsibility for the integrity of this manuscript.
Authors’ Contributions
Respective author contributions are as follows: Manuscript concept and design: E. Tung and M. Chin. Drafting of the manuscript: E. Tung and M. Chin. Critical revision of the manuscript for important intellectual content: All authors. Administrative, technical, or material support: M. Chin. Supervision: M. Chin and M. Peek. Final approval of the version to be published: All authors.
References
- 1.Klinenberg E. Heat wave: a social autopsy of disaster in Chicago. Chicago, IL: University of Chicago Press; 2002. [DOI] [PubMed] [Google Scholar]
- 2.Hanna-Attisha M, LaChance J, Sadler RC, Champney Schnepp A. Elevated blood lead levels in children associated with the Flint drinking water crisis: a spatial analysis of risk and public health response. Am J Public Health. 2016;106(2):283–290. doi: 10.2105/AJPH.2015.303003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenstock S, Whitman S, West JF, Balkin M. Racial disparities in diabetes mortality in the 50 most populous US cities. J Urban. 2014;91(5):873–885. doi: 10.1007/s11524-013-9861-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sampson RJ. Great American City: Chicago and the enduring neighborhood effect. Chicago, IL: University of Chicago Press; 2012. [Google Scholar]
- 5.Davoudi S, Stead D. Urban-rural relationships: an introduction and a brief history. Built Environment. 2002;28(4):269–277. [Google Scholar]
- 6.Gillanders WR, Buss TF, Hofstetter CR. Urban/rural elderly health status differences: the dichotomy reexamined. J Aging Soc Policy. 1996;8(4):7–24. doi: 10.1300/J031v08n04_02. [DOI] [PubMed] [Google Scholar]
- 7.Dahly DL, Adair LS. Quantifying the urban environment: a scale measure of urbanicity outperforms the urban-rural dichotomy. Soc Sci Med. 2007;64(7):1407–1419. doi: 10.1016/j.socscimed.2006.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lerner AM, Eakin H. An obsolete dichotomy? Rethinking the rural-urban interface in terms of food security and production in the Global South. Geogr J. 2011;177(4):311–320. doi: 10.1111/j.1475-4959.2010.00394.x. [DOI] [PubMed] [Google Scholar]
- 9.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55(1):125–139. doi: 10.1016/S0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 10.Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’ in health research: a relational approach. Soc Sci Med. 2007;65(9):1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 11.Goffman E. Asylums: essays on the social situation of mental patients and other inmates. Garden City, NY: Anchor Books; 1961. [Google Scholar]
- 12.Glaser BG, Strauss AL. Awareness of dying. New York, NY: Transaction Publishers; 1965. [Google Scholar]
- 13.Park RE, Burgess EW. The city: suggestions for investigation of human behavior in the urban environment. Chicago, IL: University of Chicago Press; 1967. [Google Scholar]
- 14.Shaw CR, McKay HD. Juvenile delinquency and urban areas. Chicago, IL: University of Chicago Press; 1969. [Google Scholar]
- 15.Vasishth A, Sloane DC. Returning to ecology: an ecosystem approach to understanding the city. In: Dear M, editor. From Chicago to LA: making sense of urban theory. Thousand Oaks, CA: Sage Publications; 2002. pp. 347–360. [Google Scholar]
- 16.Wennberg J, Gittelsohn. Small area variations in health care delivery. Science (New York, NY) 1973;182(4117):1102–1108. [DOI] [PubMed]
- 17.Wennberg JE. Future directions for small area variations. Medical care. 1993;31(5 Suppl):Ys75–Ys80. doi: 10.1097/00005650-199305001-00012. [DOI] [PubMed] [Google Scholar]
- 18.Browning CR, Cagney KA. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. J Health Soc Behav. 2002;43(4):383–399. doi: 10.2307/3090233. [DOI] [PubMed] [Google Scholar]
- 19.Browning CR, Cagney KA. Moving beyond poverty: neighborhood structure, social processes, and health. J Health Soc Behav. 2003;44(4):552–571. doi: 10.2307/1519799. [DOI] [PubMed] [Google Scholar]
- 20.Fitzpatrick K, LaGory M. Unhealthy cities: poverty, race, and place in America. New York: PB-Routledge. Int J Urban Reg Res. 2014;38(5):1923–1925. doi: 10.1111/1468-2427.12191_3. [DOI] [Google Scholar]
- 21.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093–3099. doi: 10.2337/dc13-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peek ME, Wagner J, Tang H, Baker DC, Chin MH. Self-reported racial discrimination in health care and diabetes outcomes. Med Care. 2011;49(7):618–625. doi: 10.1097/MLR.0b013e318215d925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McEwen BS. Stress, adaptation, and disease: allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 24.Gaber N, Wright A. Protecting urban health and safety: balancing care and harm in the era of mass incarceration. J Urban Health. 2015; [DOI] [PMC free article] [PubMed]
- 25.Park RE. Human migration and the marginal man. Am J Sociol. 1928;33(6):881–893. doi: 10.1086/214592. [DOI] [Google Scholar]
- 26.Lee V, Mikkelsen L, Srikantharajah J, Cohen L. Strategies for enhancing the built environment to support healthy eating and active living. Oakland, CA: Prevention Institute, PolicyLink; 2008. [Google Scholar]
- 27.Kwate NO, Loh JM, White K, Saldana N. Retail redlining in New York City: racialized access to day-to-day retail resources. J Urban Health. 2013;90(4):632–652. doi: 10.1007/s11524-012-9725-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnett E, Casper MA. Definition of “social environment”. Am J Public Health. 2001;91(3):465. doi: 10.2105/ajph.91.3.465a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sampson RJ, Raudenbush SW. Systematic social observation of public spaces: a new look at disorder in urban neighborhoods. Am J Sociol. 1999;105(3):603–651. doi: 10.1086/210356. [DOI] [Google Scholar]
- 30.Wilson WJ. The truly disadvantaged: the inner city, the underclass, and public policy. 2. Chicago, IL: University of Chicago Press; 1987. [Google Scholar]
- 31.Frieden TRA. Framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):e85. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 34.Drewnowski A, Aggarwal A, Hurvitz PM, Monsivais P, Moudon AV. Obesity and supermarket access: proximity or price? Am J Public Health. 2012;102(8):e74–e80. doi: 10.2105/AJPH.2012.300660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cannuscio CC, Tappe K, Hillier A, Buttenheim A, Karpyn A, Glanz K. Urban food environments and residents’ shopping behaviors. Am J Prev Med. 2013;45(5):606–614. doi: 10.1016/j.amepre.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 36.Tung EL, Peek ME, Makelarski JA, Escamilla V, Lindau ST Adult BMI and access to built environment resources in a high-poverty, urban geography. Am J Prev Med. 2016. [DOI] [PMC free article] [PubMed]
- 37.Kirby JB, Liang L, Chen HJ, Wang Y. Race, place, and obesity: the complex relationships among community racial/ethnic composition, individual race/ethnicity, and obesity in the United States. Am J Public Health. 2012;102(8):1572–1578. doi: 10.2105/AJPH.2011.300452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gaskin DJ, Thorpe RJ, Jr, McGinty EE, et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health. 2014;104(11):2147–2155. doi: 10.2105/AJPH.2013.301420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Richardson DB, Volkow ND, Kwan MP, Kaplan RM, Goodchild MF, Croyle RT. Medicine. Spatial turn in health research. Science (New York, NY). 2013;339(6126):1390–1392. [DOI] [PMC free article] [PubMed]