Introduction
Liver cirrhosis is a growing problem with a sharp increase in number of deaths due to this from 676,000 in 1980 to over one million in 2013. In the United States alone there were 53,252 deaths attributable to liver cirrhosis in 2013 compared to 37,419 in 1980 [1-4]. Patients with decompensated cirrhosis are routinely admitted to the hospital and impact in-hospital mortality[5, 6]. However, there are limited data on the etiology and outcomes of inpatient cardiac arrest in cirrhotics. This study aims to provide novel data on the causes, underlying rhythms and survival after in-hospital cardiac arrest in patients with cirrhosis compared to those without cirrhosis at a large tertiary care center.
Methods
This is a retrospective-prospective longitudinal study of 954 patients with in-hospital cardiac arrest at a large tertiary care hospital system between July 2005 and April 2016. A multi-disciplinary team reviewed all cardiac arrests, classified the etiologies, confirmed presenting rhythm and adjudicated the outcomes. Patients with diagnoses of cirrhosis in the electronic medical record were then selected out of the general cardiac arrest population for subgroup analysis. Thorough chart review for medical history, clinical presentation, and confirmation of cirrhosis via ultrasound and/or biopsy and underlying disease was completed.
Statistical Analysis
Cardiopulmonary arrest etiology, prevalence of rhythms (shockable v. non-shockable) and patient characteristics were compared using either chi square or Fisher's exact tests for comparisons between categorical variables and independent samples t-test for mean differences between continuous variables. Using logistic regression models, un-adjusted and multivariable-adjusted odds ratio of in-hospital mortality after cardiac arrest was examined. All statistical analyses were performed using SAS 9.4 (Cary, NC, USA).
Results
There were 954 patients (63.7% men, mean age 59.3 years ±16.8) with in-hospital, primary cardiac arrest events that occurred during the 11-year study period including 88 (9.2%) in patients with cirrhosis and 866 (90.8%) in patients without cirrhosis.
Baseline Characteristics
Of patients who experienced an in-hospital cardiac arrest, patients with cirrhosis were younger than patients without cirrhosis (53.9 ± 11.7 vs. 59.9 ± 17.1, p<0.0001). Patients with cirrhosis were more likely to experience a cardiac arrest in a non-intensive care unit (ICU) setting than patients without cirrhosis (78.4% v. 61.2%, p-value 0.0015) (Figure 1A). The distribution of sex, rhythm (shockable v. non-shockable), day of week, time of day and location of cardiac arrest (non-ICU v. ICU) was similar between both groups.
Figure 1.
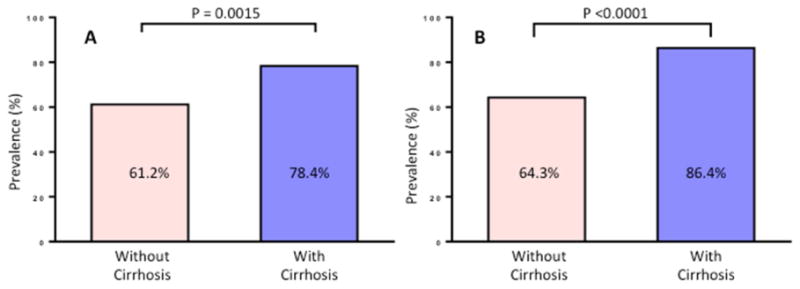
(A) Prevalence of non-ICU cardiac arrest in patients with cirrhosis compared to patients without cirrhosis (B) Prevalence of in-hospital mortality after cardiac arrest in patients with cirrhosis compared to patients without cirrhosis.
Increased In-Hospital Mortality in Cirrhosis
In-hospital mortality after cardiac arrest was higher in patients with cirrhosis than those without cirrhosis (86.4% v. 64.3%, p<0.0001)(Figure 1B). Compared to those without cirrhosis, the odds of in-hospital death after cardiac arrest among those with cirrhosis was 3.51 (95% CI, 1.88-6.56, p<0.0001). These results remained significant even after multivariable adjustment by age, sex, location, time, day and rhythm with an OR of 3.90 (CI 2.06-7.36, p<0.0001).
Causes of Cardiac Arrest in Cirrhosis
In patients with cirrhosis the most common cause of cardiac arrest was circulatory failure including bleeding (25.0%) and sepsis (18.2%). Respiratory failure led to cardiac arrest in 37.5% of patients, followed by dysrhythmias such as primary ventricular fibrillation or vagal events, which led to cardiac arrest in 12.5% of patients. The etiology of cardiac arrest was more likely to be due to circulatory causes in patients with cirrhosis compared to patients without cirrhosis (46.6% v. 34.6%, p = 0.0275).
Discussion
Utilizing a well-characterized, consecutive cohort of patients with primary in-hospital cardiac arrest, here we report that patients with cirrhosis have significantly higher risk of mortality after in-hospital cardiac arrest than patients without cirrhosis. The main causes of in-hospital cardiac arrest in patients with cirrhosis include bleeding, sepsis, and respiratory failure, all of which are potentially preventable[7]. Furthermore, patients with cirrhosis are more likely to experience a cardiac arrest in a non-ICU setting than non-cirrhotic patients. These data suggest that patients with cirrhosis should have a lower threshold for transfer to the ICU especially in the setting of suspected bleeding, SIRS/sepsis, or respiratory distress. These data are novel and provocative and if validated may help us develop specific care pathways that continue to promote early recognition of deterioration, prompt resuscitation for bleeding, early initiation of antibiotics for sepsis, and early intubation in patients with cirrhosis to reduce in-hospital mortality due to liver disease. To our knowledge, ours is the first systemic study investigating the etiology of arrest and outcomes of in-hospital cardiac arrest in cirrhosis patients[8]. Additional research is needed to further examine the causes of in-hospital cardiac arrest and mortality in patients with cirrhosis and to identify potential areas of intervention.
Acknowledgments
Funding support: The study was conducted at the Clinical and Translational Research Institute, University of California at San Diego. R.L. is supported in part by the American Gastroenterological Association (AGA) Foundation—Sucampo—ASP Designated Williams Scholarship Award; Funding provided by: Atlantic
Philanthropies, Inc, the John A. Hartford Foundation, the Association of Specialty Professors, and the American Gastroenterological Association and grant K23-DK090303 and R01-DK106419-01
Research reported in this publication was supported by the National Institute Of Environmental Health Sciences of the National Institutes of Health under Award Number P42ES010337. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- ICU
intensive care unit
Footnotes
Guarantor(s) of the article: Rohit Loomba, MD, MHSc
Conflict of Interest: The authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author contributions: Megan E Reinders: study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript, approved final submission
Daniel Bouland: critical revision of the manuscript, approved final submission
Ricki Bettencourt: analysis and interpretation of data, organization of tables and figures, critical revision of the manuscript, approved final submission
Jessica Bazick: critical revision of the manuscript, approved final submission
Gabriel Wardi: critical revision of the manuscript, approved final submission
Michael Mendler: critical revision of the manuscript, approved final submission
Irine Vodkin: critical revision of the manuscript, approved final submission
Denise Kalmaz: critical revision of the manuscript, approved final submission
Thomas Savides: critical revision of the manuscript, approved final submission
David A. Brenner: critical revision of the manuscript, approved final submission
Rebecca E Sell: study concept and design, data collection, analysis and interpretation of data, critical revision of the manuscript, study supervision, approved final submission
Rohit Loomba: study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript, obtained funding, study supervision, approved final submission
All authors approved the final version of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mokdad AA. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. doi: 10.1186/s12916-014-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleming KM. All-cause mortality in people with cirrhosis compared with the general population: a population-based cohort study. Liver Int. 2012;32(1):79–84. doi: 10.1111/j.1478-3231.2011.02517.x. [DOI] [PubMed] [Google Scholar]
- 3.Roberts SE, Goldacre MJ, Yeates D. Trends in mortality after hospital admission for liver cirrhosis in an English population from 1968 to 1999. Gut. 2005;54(11):1615–21. doi: 10.1136/gut.2004.058636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jalan R. Acute-on-Chronic Liver Failure: A Distinct Clinical Condition. Semin Liver Dis. 2016;36(2):107–8. doi: 10.1055/s-0036-1583287. [DOI] [PubMed] [Google Scholar]
- 6.Arroyo V. Acute-on-chronic liver failure in cirrhosis. Nat Rev Dis Primers. 2016;2:16041. doi: 10.1038/nrdp.2016.41. [DOI] [PubMed] [Google Scholar]
- 7.Ratib S. Causes of death in people with liver cirrhosis in England compared with the general population: a population-based cohort study. Am J Gastroenterol. 2015;110(8):1149–58. doi: 10.1038/ajg.2015.191. [DOI] [PubMed] [Google Scholar]
- 8.Roedl K. Epidemiology and outcome of cardiac arrest in patients with liver cirrhosis. Intensive Care Med Exp. 2015;3(Suppl 1):687. [Google Scholar]


