Abstract
Background
Family caregiving is an increasingly important component of care for patients and the elderly.
Objective
The aim of this study is to characterize the burden of family caregiving among employed adults.
Methods
Employed adults (≥18 years) from the 2013 US National Health and Wellness Survey (NHWS) were classified as family caregivers if they reported currently caring for at least one adult relative. Chi-square tests and one-way analyses of variance assessed whether employed caregivers, weighted to the US population, differed from employed non-caregivers on behavioral characteristics, workplace productivity, and health care resource utilization.
Results
Eight million workers were family caregivers in the United States, more often female than male (51% vs. 49%, P < 0.05), and 53% were between 40 and 64 years of age. Eighteen percent of caregivers were Hispanic compared with 15% of non-caregivers (P < 0.05). Similar behavioral characteristics between caregivers and non-caregivers included daily alcohol consumption (6% vs. 5%) and lack of vigorous exercise (25% vs. 29%), but caregivers had a higher prevalence of smoking (26% vs. 19%, P < 0.05). Caregivers reported a higher mean percentage of work time missed (8% vs. 4%, P < 0.05) and greater productivity impairment (24% vs. 14%, P < 0.05). Some form of depression was reported by 53% of caregivers compared with 32% of non-caregivers (P < 0.05), and more caregivers had self-reported insomnia than non-caregivers (46% vs. 37%, P < 0.05). The number of self-reported diagnosed comorbidities was higher among caregivers compared with that of non-caregivers (5.0 vs. 3.1, P < 0.05), as was the mean number of outpatient visits in the previous 6 months (4.1 vs. 2.7, P < 0.05).
Conclusion
Family caregiving is associated with a multidimensional burden that impacts caregivers and has implications for employers and the health care system. Clinicians and employers need to recognize and understand this burden. Characterization of caregivers as reported in this study can inform development of targeted programs to help mitigate the burden.
Keywords: caregiver burden, productivity, mental health, health care resource use, workforce, employed, family caregivers
Background
Family caregiving, or “informal caregiving” to use the older terminology, is defined as unpaid assistance to family members who are unable to function independently. Such caregiving is an important component of care for individuals with chronic conditions and the elderly. Estimates from caregiver interviews in 2014 suggest that 16.6% of the US adult population can be identified as family caregivers for a chronically ill, disabled, or older adult in the last 12 months.1 The need for family caregiving is likely to increase as a result of the aging population, an increase in population longevity, and a higher number of individuals living with chronic diseases.2,3
The opportunity costs of family caregiving, defined as the economic value of activities relinquished as a result of providing care, may be as high as $522 billion annually.4 In addition, family caregiving often requires diverse responsibilities that can be both physically and psychologically demanding, which affects not only the physical and/or mental health of the caregiver but also may reciprocally affect the care recipient.5 With the increasing need for caregiving, there has been a concomitant increase in the recognition of the caregiver burden, and caregiver support has become a national public health priority.6 Consequently, it is also important that clinicians and employers be made cognizant to aware of the caregiver burden and help to mitigate this burden that is manifested as reduced quality of life, physical and mental health issues, and reduced productivity.1 Such mitigation may be of benefit to caregivers and care recipients, resulting in overall improvements in population-level health.
It is recognized that some individual caregivers may derive positive effects from caregiving, such as self-confidence, gratification, and greater appreciation of life, and often these positive benefits occur concurrently with a burden related to the caregiving.7–9 Identifying and managing the caregiver burden require a greater understanding of the caregiver population and their needs. While the medical literature is replete with studies that have characterized the caregiver burden among discrete care recipient populations, i.e., specific diseases or conditions,10–13 less has been published on the population level, especially among an employed population. Therefore, the aims of this study are to identify family caregivers in the US workforce and characterize their burden with regard to work productivity, comorbidities, health care resource utilization, and mental health.
Methods
Data source and population
This cross-sectional study used deidentified data from the US National Health and Wellness Survey (NHWS) for 2013 to describe demographic characteristics and health care resource utilization among employed adults aged 18 years or older, comparing those who reported being family caregivers with those who did not report being a caregiver.
The NHWS is a self-reported general population survey conducted annually through the Internet on adults aged 18 years or older in the United States. It is fielded through an opt-in panel and uses a stratified random sampling framework (sex, age, and race/ethnicity) to ensure that it is representative of the demographic composition of the US adult population. NHWS data have been suggested to compare favorably with estimates of US demographic composition according to the census and with estimates from the National Health Interview Survey.14,15 The NHWS has received approval from Essex Institutional Review Board (IRB) (Lebanon, NJ, USA).
A total of 1,176,292 individuals were contacted for the 2013 NHWS, 109,388 responded (9.3% response rate), of whom 75,000 gave their written informed and/or electronic consent, met the inclusion criteria (age ≥18 years), and completed the survey instrument. For the current analysis, only employed adults were included (N = 40,167), and two cohorts were identified based on their status as family caregivers; subjects were classified as a family caregiver (n = 2,558) if they reported currently caring for at least one adult relative and as a non-caregiver (n = 37,609) if they were not caring for any adult relatives.
Outcomes
In addition to capturing demographics, the NHWS includes questions on lifestyle behaviors such as alcohol consumption, smoking, and exercise; the number of diagnosed comorbid conditions and specific conditions of insomnia, depression, and anxiety; health care resource utilization over the previous 6 months for categories of emergency room (ER) visits, inpatient hospitalizations, outpatient visits, and prescription medications; and general health. The NHWS also includes the Work Productivity and Activity Impairment (WPAI) questionnaire16 to evaluate the impact of health problems on work and overall activity. The WPAI is a validated instrument that measures the loss of work productivity and impairment in daily activities over the past 7 days. The questionnaire includes four items: absenteeism (percentage of work time missed due to health problems), presenteeism (percentage of impairment while at work due to health problems), overall work impairment (total percentage of work time missed due to either absenteeism or presenteeism, since they are mutually exclusive), and activity impairment (percentage activity impairment excluding work). WPAI scores are expressed as mean impairment percentages ranging from 0% to 100%, with higher scores indicating more productivity loss and greater impairment.
The presence and severity of depression was determined using the Patient Health Questionnaire-9 (PHQ-9).17 The PHQ-9 is a validated measure that incorporates Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) depression diagnostic criteria with other major depressive symptoms into a nine-item module that can be used to determine depression severity over the previous 2 weeks.
The general health of the population was evaluated using the Physical Component Summary (PCS) and Mental Component Summary (MCS) scores from the SF-36 v2 Health Survey,18 a generic instrument consisting of 36 questions that encompass physical and mental domains that contribute to health status. Scores for the PCS and MCS are normed to the US population (mean = 50, SD = 10) and vary from 0 to 100, with higher scores indicating better health.
Statistical analyses
Sampling weights were calculated from the 2012 Current Population Survey of the United States Census so that demographic characteristics of the sample reflected those of the total adult population. Summary statistics were used to describe demographic characteristics and characterize outcomes between the two cohorts. Chi-square tests and one-way analyses of variance were used for categorical variables and continuous variables, respectively, incorporating sampling weights to assess whether employed caregivers differed from employed non-caregivers; P < 0.05 indicates statistical significance. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Based on weighted results, of ~124 million US adults aged 18 years or older who employed at least part time, 8,054,000 individuals (6.5%) were self-identified as family caregivers and 115,527,000 as non-caregivers. Among the caregivers, 17.7% were caring for ≥2 family members. Demographic characteristics show significant differences between the populations in sex and age (Table 1), with caregivers more likely to be female (51.4% vs. 46.7%; P < 0.05) and middle aged (40–64 years) than non-caregivers (P < 0.05). Caregivers were also more likely (P < 0.05) to be racial/ethnic minorities than non-caregivers (36.3% vs. 33.7%), and 18.5% of caregivers were Hispanic compared with only 15.1% of non-caregivers (Table 1). There were no differences in education or household income between caregivers and non-caregivers; however, nearly 30% of caregivers reported that caring for a patient has put them under financial strain. In addition, the level of employment was significantly different (P < 0.05), with fewer caregivers employed full time (75.4% vs. 79.1%).
Table 1.
Demographic characteristics among caregivers and non-caregivers in the 2013 wave of the National Health and Wellness Survey
| Variable | Caregiver (n = 8,054)a | Non-caregiver (n = 115,527)a | P-value |
|---|---|---|---|
| Sex, n (%) | <0.05 | ||
| Male | 3,914 (48.6) | 61,639 (53.4) | |
| Female | 4,140 (51.4) | 53,889 (46.7) | |
| Age (years), n (%) | <0.05 | ||
| 18–39 | 3,380 (42.0) | 50,977 (44.1) | |
| 40–64 | 4,277 (53.1) | 58,785 (50.9) | |
| ≥65 | 397 (4.9) | 5,765 (5.0) | |
| Race/ethnicity, n (%) | <0.05 | ||
| White | 5,128 (63.7) | 76,643 (66.3) | |
| African American | 784 (9.7) | 12,616 (10.9) | |
| Hispanic | 1,486 (18.5) | 17,467 (15.1) | |
| Others | 655 (8.1) | 8,802 (7.6) | |
| Education, n (%) | NS | ||
| High school | 1,588 (19.7) | 22,525 (19.5) | |
| Some college, no degree | 2,328 (28.9) | 34,002 (29.4) | |
| Associates degree or higher | 4,139 (51.4) | 59,000 (51.1) | |
| Employment, n (%) | <0.05 | ||
| Part time | 1,985 (24.6) | 24,108 (20.9) | |
| Full time | 6,069 (75.4) | 91,420 (79.1) | |
| Household income, n (%)b | NS | ||
| <$75,000 | 5,281 (68.4) | 74,504 (68.0) | |
| ≥$75,000 | 2,442 (31.6) | 35,042 (32.0) |
Notes:
Number of participants for all characteristics are represented in thousands to reflect weighted population.
Among subjects who provided income data (caregiver = 7,723; non-caregiver = 109,546).
Abbreviation: NS, not significant.
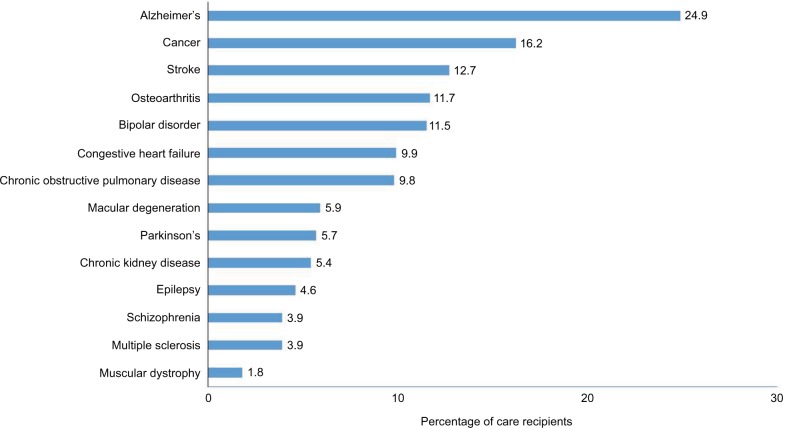
Alzheimer’s disease was the primary condition for which family care was provided (24.9%) followed by cancer (16.2%; Figure 1). While most of the conditions were related to aging, neurologic and psychiatric conditions also reflected the need for family care. In addition to these specific diseases, other conditions were present in 16.5% of recipients, but the prevalence of these individual conditions was <1%. Caregiving included a range of responsibilities, and approximately one-quarter of caregivers (25.8%) reported that they were the ones mainly responsible for transportation, meal preparation, grocery shopping, housework, medication management, or arranging outside services. While a similar proportion (26.5%) were mainly responsible for managing the finances of the care recipient, only 10.4% were mainly responsible for bathing or grooming, toileting, feeding, transferring from bed to chair, or dealing with incontinence.
Figure 1.
Conditions of patients for whom caregivers are providing care in the 2013 wave of the National Health and Wellness Survey.
Note: Percentages exceed 100% since some recipients may have multiple conditions and/or are caring for multiple family members.
Of the evaluated lifestyle behaviors (Table 2), caregivers had a higher prevalence of smoking (26.0% vs. 18.8%; P < 0.05) and daily alcohol consumption (6.0% vs. 4.8%; P < 0.05) than non-caregivers, and the proportion of individuals reporting no vigorous exercise in the past month was lower in caregivers than in non-caregivers (25.1% vs. 28.6%).
Table 2.
Lifestyle characteristics among caregivers and non-caregivers in the 2013 wave of the National Health and Wellness Survey
| Variable | Caregiver (n = 8,054)a | Non-caregiver (n = 115,527)a | P-value |
|---|---|---|---|
| Currently smoker, n (%) | <0.05 | ||
| Yes | 2,096 (26.0) | 21,715 (18.8) | |
| No | 5,958 (74.0) | 93,812 (81.2) | |
| Number of days vigorously exercised, n (%) | <0.05 | ||
| 1–4 | 1,418 (17.6) | 17,936 (15.5) | |
| 5–9 | 1,183 (14.7) | 15,454 (13.4) | |
| 10–14 | 1,032 (12.8) | 13,991 (12.1) | |
| 15–19 | 837 (10.4) | 10,930 (9.5) | |
| 20–24 | 863 (10.7) | 13,539 (11.7) | |
| 25–29 | 415 (5.2) | 6,188 (5.4) | |
| 30–31 | 285 (3.5) | 4,406 (3.8) | |
| Never | 2,022 (25.1) | 33,085 (28.6) | |
| Alcohol consumption, n (%) | <0.05 | ||
| Daily | 483 (6.0) | 5,574 (4.8) | |
| Once a week or more | 2,807 (34.9) | 36,735 (31.8) | |
| Monthly | 2,676 (33.2) | 40,368 (34.9) | |
| Do not drink | 2,088 (25.9) | 32,851 (28.4) |
Note:
Number of participants for all characteristics are represented in thousands to reflect weighted population.
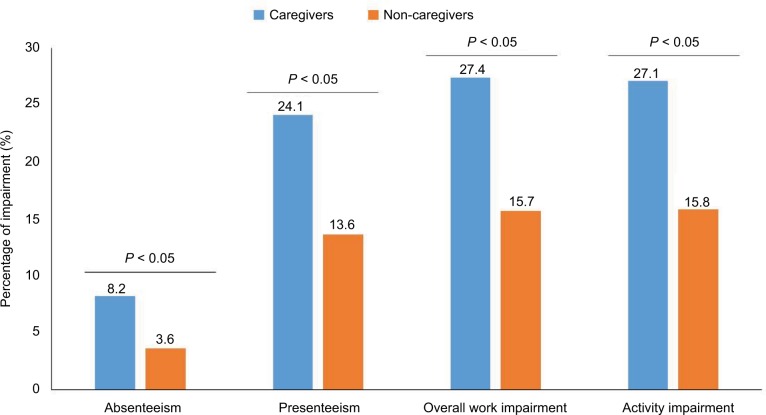
Work and activity impairment were more likely to be reported among caregivers than among non-caregivers (Figure 2). Both absenteeism and presenteeism were significantly higher among caregivers, with overall work productivity impairment of 27.4% among caregivers compared with 15.7% among non-caregivers (P < 0.05). Similarly, caregivers reported total activity impairment of 27.1% vs. 15.8% for non-caregivers (P < 0.05).
Figure 2.
Work productivity and activity impairment, assessed using the Work Productivity and Impairment questionnaire, among caregivers and non-caregivers in the 2013 wave of the National Health and Wellness Survey.
Summary scores on the SF-36 showed significantly lower mental and physical health status among caregivers compared to that of non-caregivers, with greater effects on mental health; MCS scores were 45.5 and 48.7 for caregivers and non-caregivers, respectively (P < 0.05), and PCS scores were 49.3 and 52.6, respectively (P < 0.05).
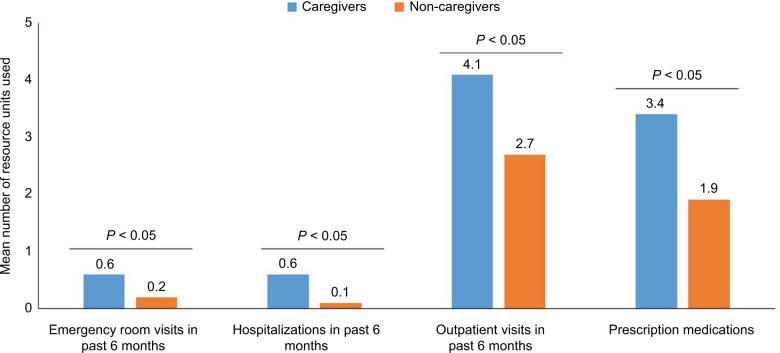
Health care resource utilization was significantly higher among caregivers across all resource categories (Figure 3). For the previous 6 months and compared to non-caregivers, caregivers reported a greater mean number of ER visits (0.6 vs. 0.2; P < 0.05), hospitalizations (0.6 vs. 0.1; P < 0.05), and outpatient visits (4.1 vs. 2.7; P < 0.05), as well as a greater number of prescription medications (3.4 vs. 1.9; P < 0.05).
Figure 3.
Health care resource utilization among caregivers and non-caregivers in the 2013 wave of the National Health and Wellness Survey.
Caregivers had significantly more diagnosed comorbid conditions than non-caregivers (5.0 vs. 3.1; P < 0.05). For example, insomnia was present in a significantly higher proportion of caregivers than non-caregivers (17.9% vs. 9.9%; P < 0.05), as were shift work sleep disorder (1.8% vs. 0.5%; P < 0.05) and generalized anxiety disorder (4.0% vs. 1.8%; P < 0.05). When measured using the PHQ-9, depression was also significantly more prevalent among caregivers (53.0% vs. 31.7%; P < 0.05), with the proportion of caregivers higher than non-caregivers for depression severity levels of mild (23.2% vs. 18.1%), moderate (15.5% vs. 7.7%), moderately severe (9.8% vs. 4.0%), and severe (4.5% vs. 1.9%; all P < 0.05).
Discussion
This analysis provides a population-level approach to characterize the family caregiver burden in the US workforce, especially as it relates to activity participation and health. The results suggest that there is a substantial burden associated with family caregiving, which affects physical, mental, and economic components of the caregiver’s daily life. In addition, the caregiver burden may also potentially impact the quality of care provided to the recipient, resulting in a broader societal burden. Notably, this analysis relied on a larger and more heterogeneous population than previous studies10–13 that have evaluated caregiver burden associated with caring for patients with particular health conditions, and also included comparison with non-caregivers. These factors enable more complete demographic characterization of caregivers and highlight the magnitude and impact of the multidimensional burden from the caregiver perspective. In addition, the specific use of an employed population and the capture of health care resource utilization have applicability to the societal perspective especially related to employers and the health care system.
Comparison of demographic characteristics shows that education and income were similar between caregivers and non-caregivers, but caregivers were more likely to be female, middle aged, and non-white. These findings are similar to those reported in a non-comparative study of a caregiver population.1 Consistent with the time required for caregiving, caregivers were also more likely to be employed part time. As a result, overall work impairment, as well as non-work activity impairment, was significantly greater among caregivers than non-caregivers, by almost twofold. Interestingly, presenteeism rather than absenteeism appeared to be the primary driver of work impairment among caregivers. While work productivity impairment cannot be definitively linked to the caregiving, it may be proposed that the higher presenteeism may, at least in part, result from the higher rates of depression and insomnia among caregivers.
Alzheimer’s disease was the most frequently reported condition for which family caregivers provided care. This condition has also been reported to be the most challenging, since it is not only associated with a high need for performing activities of daily living for the recipient but also results in greater vulnerability of the caregiver to emotional stress and negative health.1 Furthermore, ~18% of caregivers reported caring for multiple family members, suggesting that such situations are common, although the effect of multiple recipients on the caregiver burden was not determined.
The SF-36 summary scores among caregivers approximated normative values, which may not be surprising considering the age distribution, education, and socioeconomic status of these individuals. In particular, age may be related to perceptions of health status among caregivers, with older caregivers (i.e., ≥65 years) more frequently reporting fair or poor health than younger caregivers, but younger caregivers more frequently reporting greater mental distress and dissatisfaction.19 Nevertheless, these scores were significantly lower than those among non-caregivers, suggesting a poorer general health state. The greater impact on MCS compared to PCS is in concordance with the higher presence of depression and anxiety among caregivers. These results are consistent with another nationally representative survey that suggested caregivers report general health status similar to non-caregivers, but that caregivers were more likely to report poor mental health and inadequate sleep, which may have downstream effects on health.20 Notably, in the current study, inadequate sleep was suggested by the higher rate of insomnia in caregivers compared to that in non-caregivers, which may also be associated with the higher rate of, and more severe, depression symptoms, since there is a relationship between insomnia and depression.21,22
With regard to physical health, it is generally considered that there is little evidence, at least from well-controlled comparative population-based studies, indicating that objective physical health status is poorer among caregivers than the general population.9 However, the higher rates of resource use observed among caregivers in the present study, which was significant across all resource categories (i.e., inpatient hospitalizations, ER, outpatient visits, and medications), suggest poorer physical health even though resource use cannot be directly attributed to caregiving. The higher rates of insomnia, depression, and anxiety as mentioned earlier are also likely to contribute to the higher use of health care resources. Of note, adverse health behaviors were more frequent among caregivers, and these results support previous studies suggesting that caregivers more frequently engage in negative health behaviors than non-caregivers.23,24
Strengths and limitations
The strengths of this study include the use of a weighted population-level analysis that enhances generalizability of the results to the US population and inclusion of employed subjects, which provides evaluation of productivity that is of potential relevance from the economic and employer perspectives. However, a key limitation is that this is a cross-sectional study. Consequently, no inferences of causality can be made regarding caregiving as the direct source of the reported outcomes, and these relationships should be only considered associative. Another limitation is that while this study presents a broad, population-level perspective, the burden is likely to vary within subpopulations and may be related to a variety of factors. These factors include condition of the care recipient, number of hours required for caregiving, and demographic characteristics of the caregiver such as age and race or ethnicity,1 since cultural factors are likely to play a role in the caregiving process and how the burden is perceived.25,26 In addition, a proportion of caregivers (~18%) were caring for multiple recipients and potentially biased the results toward a higher burden. Finally, since the NHWS is a self-reported Internet survey, mode of recruitment and survey administration may represent a form of selection bias; comorbidities could not be clinically confirmed; and responses may be subject to recall bias and potential misinterpretation of the questions.
Despite these limitations, this study suggests that at the population level and compared to non-caregivers, there is a substantial and multidimensional burden associated with family caregiving. On the individual level, the burden is manifested by the potential for mental health issues, a daily impact on participatory activities including reductions in work productivity and impairment of general health. It should also be considered that these issues may potentially impact the quality of care provided to the recipient. Furthermore, there are economic implications that suggest a large societal burden resulting from reduced work productivity and increased use of health care resources by caregivers. This latter variable adds to the overall costs of health care. These findings suggest a need among clinicians and employers for identifying family caregivers and implementing programs for effective management strategies that can help reduce the burden. The factors that are likely to affect specific outcomes especially warrant further evaluation for determining and developing appropriate interventions that will be of benefit to the caregivers and their care recipients.
Acknowledgments
The authors would like to acknowledge the contributions of Kantar Health employees who provided the analysis on the NHWS data. Editorial assistance was provided by E Jay Bienen, PhD, who was funded by Pfizer. This study was funded by Pfizer, Inc.
Footnotes
Disclosure
The authors are employees of Pfizer Inc. The authors report no other conflicts of interest in this work.
References
- 1.National Alliance for Caregiving and the AARP Public Policy Institute Caeregiving in the U.S. 2015 Report. 2015. [Accessed October 20, 2016]. Available from: http://www.caregiving.org/wp-content/uploads/2015/05/2015_Caregivingin-theUS_Final-Report-June-4_WEB.pdf.
- 2.National Institute on Aging [webpage on the Internet] Global Health and Aging. 2011. [Accessed May 16, 2017]. (NIH Publication 11–7737). Available from: https://www.nia.nih.gov/research/publication/global-health-and-aging/preface.
- 3.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chari AV, Engberg J, Ray KN, Mehrotra A. The opportunity costs of informal elder-care in the United States: new estimates from the American Time Use Survey. Health Serv Res. 2015;50(3):871–882. doi: 10.1111/1475-6773.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1060. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services [webpage on the Internet] Healthy People 2020. Disability and Health. [Accessed October 21, 2016]. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/disability-and-health/objectives.
- 7.Beach SR, Schulz R, Yee JL, Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15(2):259–271. doi: 10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- 8.Haley WE, Allen JY, Grant JS, Clay OJ, Perkins M, Roth DL. Problems and benefits reported by stroke family caregivers: results from a prospective epidemiological study. Stroke. 2009;40(6):2129–2133. doi: 10.1161/STROKEAHA.108.545269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roth DL, Fredman L, Haley WE. Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist. 2015;55(2):309–319. doi: 10.1093/geront/gnu177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hillman L. Caregiving in multiple sclerosis. Phys Med Rehabil Clin N Am. 2013;24(4):619–627. doi: 10.1016/j.pmr.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Goren A, Gilloteau I, Lees M, DaCosta Dibonaventura M. Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer. 2014;22(6):1637–1646. doi: 10.1007/s00520-014-2122-6. [DOI] [PubMed] [Google Scholar]
- 12.Goren A, Montgomery W, Kahle-Wrobleski K, Nakamura T, Ueda K. Impact of caring for persons with Alzheimer’s disease or dementia on caregivers’ health outcomes: findings from a community based survey in Japan. BMC Geriatr. 2016;16:122. doi: 10.1186/s12877-016-0298-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ullrich A, Ascherfeld L, Marx G, Bokemeyer C, Bergelt C, Oechsle K. Quality of life, psychological burden, needs, and satisfaction during specialized inpatient palliative care in family caregivers of advanced cancer patients. BMC Palliat Care. 2017;16(1):31. doi: 10.1186/s12904-017-0206-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DiBonaventura MD, Wagner JS, Yuan Y, L’Italien G, Langley P, Ray Kim W. Humanistic and economic impacts of hepatitis C infection in the United States. J Med Econ. 2010;13(4):709–718. doi: 10.3111/13696998.2010.535576. [DOI] [PubMed] [Google Scholar]
- 15.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat 10. 2012;(252):1–207. [PubMed] [Google Scholar]
- 16.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ware JE, Jr, Kosinski M, Dewey M, Gandek B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8TM Health Survey. Lincoln, RI: QualityMetric Inc and Health Assessment Lab; 2001. [Google Scholar]
- 19.Anderson LA, Edwards VJ, Pearson WS, Talley RC, McGuire LC, Andresen EM. Adult caregivers in the United States: characteristics and differences in well-being, by caregiver age and caregiving status. Prev Chronic Dis. 2013;10:E135. doi: 10.5888/pcd10.130090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trivedi R, Beaver K, Bouldin ED, et al. Characteristics and well-being of informal caregivers: results from a nationally-representative US survey. Chronic Illn. 2014;10(3):167–179. doi: 10.1177/1742395313506947. [DOI] [PubMed] [Google Scholar]
- 21.Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–449. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28(11):1457–1464. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 23.Acton GJ. Health-promoting self-care in family caregivers. West J Nurs Res. 2002;24(1):73–86. doi: 10.1177/01939450222045716. [DOI] [PubMed] [Google Scholar]
- 24.Hoffman GJ, Lee J, Mendez-Luck CA. Health behaviors among Baby Boomer informal caregivers. Gerontologist. 2012;52(2):219–230. doi: 10.1093/geront/gns003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: a 20-year review (1980–2000) Gerontologist. 2002;42(2):237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- 26.Pinquart M, Sorensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist. 2005;45(1):90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]