Abstract
Background and Objectives:
Due to the high costs of conventional mental health care, there has been a rise in the application of web-based technologies in recent years, i.e., telemental health care. We conducted this systematic review in 2017, using high quality research articles on the applications, technologies, advantages and challenges associated with telemental health care published since year 2000.
Methods:
We used a combination of relevant key words to search four major databases, such as “Web of Sciences, Embase, PubMed and Science Direct”. From among 156 articles, which had been published since 2000, twenty five articles met all of the inclusion criteria and were selected for the final review. The information extracted from these articles were used to construct Tables 1 and 2. Also, the materials derived from 55 credible articles were used as further support and complementary facts to substantiate the information presented in the Discussion section.
Results:
The findings revealed that telemental health care is an extended domain supportive of conventional mental health services. Currently, telemental health care has multiple capabilities and technologies for providing effective interventions to patients with various mental illnesses. It provides clinicians with a wide variety of innovative choices and strategies for mental interventions, in addition to significant future potentials.
Conclusions:
Telemental health care can provide effective and adaptable solutions to the care of mental illnesses universally. While being comparable to in-person services, telemental health care is particularly advantageous and inexpensive through the use of current technologies and adaptable designs, especially in isolated communities.
Keywords: telemental health, applications, mental disorders, telemedicine, tele-psychiatry
1. INTRODUCTION
In recent decades mental and behavioral disorders have been the fifth costly group of diseases in the U.S. (1). The provision of healthcare services to mental patients has been challenging due to limited access to the costly services (2). Distant areas with insufficient healthcare providers have difficulties providing basic services to the mental patients. Using information technologies, such as telemedicine in the management of mental patients provides them with easy access to modern and efficient healthcare services and reliable diagnosis while being cost-effective (3).
Telemedicine is a popular information and communication system to provide and support distant healthcare services, of which mental care is a major domain (3). Using telephone, video-conferencing and Internet, telemedicine provides a variety of health services to deprived areas. Studies have demonstrated that telemedicine is a cost-effective solution to health care, where access to such services and the costs are prohibitive (4-8). Likewise, telemedicine can effectively facilitate mental care through computer-based interaction of patients with psychiatrists.
The healthcare industry is moving towards monitoring systems, patient’s self-supervision, computer-mediated therapy and instructional videos (9). Results from the surveys of residents in many states have indicated that 80% of Americans use Internet to obtain mental health information. Moreover, patients increasingly take advantage of Internet for meeting their emotional and psychological needs (10). Telemental health care is a new multidisciplinary approach, based on information technologies and computer sciences, enabling psychiatric services rendered to patients. It also seeks to facilitate mental health services at remote clinical sites. Major advantages of telemental health care are tele-psychotherapy, online psychology and networking (1).
We identified a large number of studies, reporting popular applications of telemental health care in various settings (1-8,11-28). However, we did not find a systematic review on all applications of telemental health care. Therefore, we conducted this systematic review of research published since 2000, identifying all of the existing applications of telemental health care. This review can significantly benefit mental healthcare clinicians, particularly those practicing in under-developed communities. It raises the awareness of the efficacy of telemental health care, and can serve as a useful guide for institutions that intend to upgrade their conventional mental health services.
2. METHODS
We searched four major health care literature databases, such as PubMed, Embase, ISI Web Sciences, and Science Direct (29). The key terms used to search these databases included: telemedicine, telemental health care, health informatics, and mental health consulting. We identified 156 relevant articles, 25 of which contained all of the following selection criteria:
Studied various applications of telemental health care, particularly in under-developed communities.
Were published between years 2000 and 2017 in reputable English journals and were available in full-text.
Were indexed by one or more of the selected databases.
The selected articles were primarily reviewed by an experienced psychiatrist-academician, who approved the final 25 articles for further review process. Each article was further reviewed by two members of the team independently. The reviewers also compiled the major findings of the selected articles and grouped them in specific categories and subcategories (Tables 1 and 2). The findings were deliberated collectively by the authors, with a focus on the significant merits of telemental health care, and were assigned for inclusion in the final manuscript.
Table 1.
Applications and potential uses of telemental health care. XML: Extensible markup language; AU: Action units; ADHD: Attention deficit and hyperactivity disorder. a Review article. b Applied research article. c Case study article. d A 5-medical center research document.ve Expert panel statement.
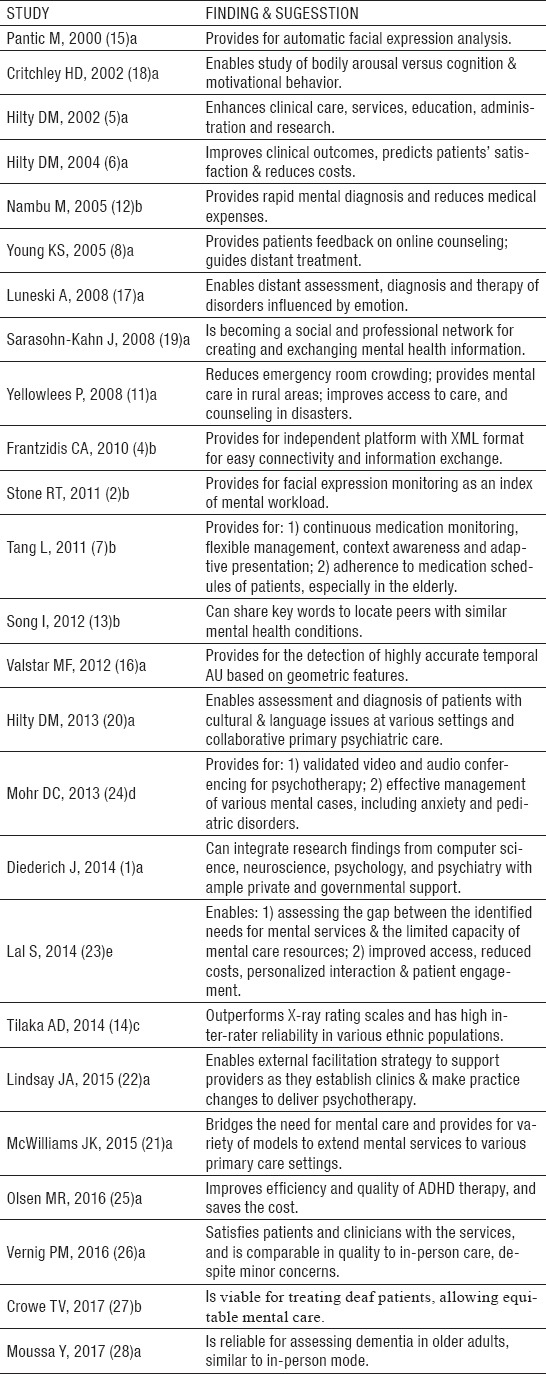
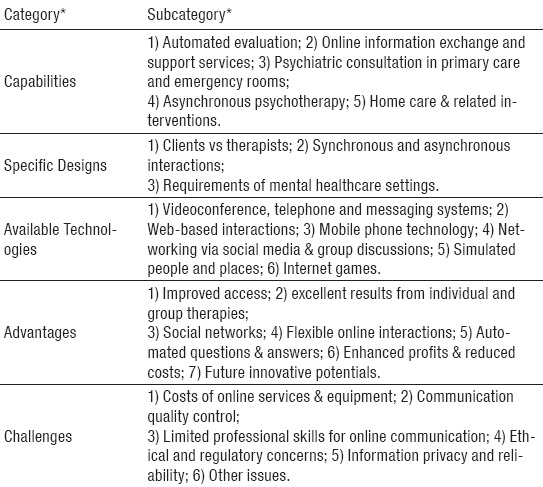
Table 2.
Categories and Subcategories of Findings Concluded from the Reviewed Articles. * Categories and subcategories are discussed in detail under “Discussion” section.
3. RESULTS
For brevity and conciseness, the current applications of telemental health care, as extracted from the 25 reviewed articles, have been presented in Table 1. We found five categories and 25 subcategories of major findings about the various applications of telemental health care upon the completion of the review process. As presented in Table 2, the five categories relevant to telemental health care consisted of: a) Capabilities; b) Specific designs; c) Available technologies; d) Advantages, and e) Challenges. Of the 25 approved articles, there were 16 reviews, six case studies, an original research article, a 5-medical center research document, and an expert panel statement. The above topics and the associated subheadings are elaborated in the “Discussion” section.
4. DISCUSSION
This review strongly suggests that using telemental health care for psychotherapy and other mental services improves patient satisfaction and reduces the costs of care. Almost all of the associated technologies can be effectively used to evaluate and analyze mental disorders while monitoring the quality of service. Currently, telemental health care offers capabilities for imaging, synchronous and asynchronous psychotherapy, and consultation to clinicians in a variety of settings. This review presents its discussion under the following headings and subheadings.
Capabilities
1. Automated Evaluation: The majority of methods used in the evaluation of mental health conditions are time-consuming and costly. Several automated methods have been developed according to the type of data and the required analysis.
a) Imaging and Behavior Analysis: Image analysis methods have been developed to examine an individual’s face, behavior, mood, and the associated symptoms. Little research has been conducted to analyze people’s images, leading to or supporting mental diagnoses. This is largely due to complex image processing issues. Alternative studies have been undertaken to evaluate people’s mental conditions by monitoring their behaviors, which are simpler than analyzing facial and body images. Mental health status can be evaluated in the elderly, using monitors and sensors attached to them while they are engaged in activities, such as watching movies (1,2, 16).
b) Evaluating Biosignals: People’s physical and mental conditions may be evaluated by examining their biological signals, such as electrocardiograms and electroencephalograms (EKG & EEG). Findings from other studies suggest that biological signals can be used to examine mental health disorders (6, 17). Travainen et al. (30) examined the galvanic current of skin to study people’s emotional reactions. In another study (18), there was a significant relationship between the electrodermal activity (EDA) of the subjects and their mental and physiological state. Frantizidis et al (4) have suggested that EEG and EDA signals could be used to diagnose mood, emotional and mental disorders.
c) Language Use in Mental Disorders: Speech and language disorders (SLD) and incoherent speech occur in many mental disorders, and are evaluated to diagnose mental conditions. However, SLD methods are generally time-consuming and costly, therefore, automatic SLD methods are used instead (31). Also, among the common automated methods, there are statistical and latent semantic analysis, and machine-learning methods (13,14, 31).
d) Acoustic Analysis: New technologies have reduced limitations of mental health evaluation and improved its precision. Audio analysis of speech provides useful information about people’s emotional and psychological state, and can lead to mental state diagnosis. The acoustic features, such as speed and shorter-than-usual pauses are the key indicators of emotional symptoms (4, 32).
e) Knowledge-based Methods: Using patients’ data and analysis algorithms can improve the evaluation and diagnostic methods in mental health care (33).
2. Online Information Exchange & Support Services: New advances have been made in mental health informatics, such as online healthcare, social media and networking (34). The latter facilitates data sharing and interactions among patients and clinicians (2,13, 19). There is online support that offers public programs to meet the emotional and psychological needs of patients. These are mainly websites that provide counseling and distant learning to students with mental disorders (8).
3. Psychiatric Consultation in Primary Care & Emergency Rooms: Telemental health technology facilitates psychiatric consultation and therapy at primary care centers, resulting in promising outcomes comparable to in-person services (20). However, it is important that the efficacy of tele-psychotherapy in emergency consultation be evaluated and the detailed clinical guidelines established (11, 35).
4. Asynchronous Psychotherapy: A synchronous tele-psychiatry can provide consultation and primary care interventions to mental patients, e.g., transmitting patient’s record to the psychiatrist via video and text files from the primary care centers. Likewise, the psychiatrist can provide recommendations after evaluating the patient’s medical reports. Nowadays, asynchronous psychotherapy has been designed so that the mental patients receive appropriate primary care locally (36). These programs resolve the access issues and enhance the quality of mental care programs at remote locations (36, 37).
5. Home Care and Related Interventions: Provision of mental care at home can reduce costs. This is particularly warranted when primary care provision at local clinics is limited or accessing the services is impractical. Such services have significantly improved the quality of care and the access. Online video conferencing via personal computers or mobile phones has enhanced the management or follow-up of many mental patients. Using the technology advances the application of tele-psychotherapy and may make the office visits for these patients obsolete soon. However, patient information privacy remains a concern according to HIPAA guidelines (38).
Specific Designs
1. Clients vs. Therapists: Successful client-centered services require the awareness of clients’ mental health needs and their environmental constraints (39). Telemental health programs must be easy to use for clients, although those designed for therapists may be comprehensive and more complex. Most therapists are familiar and agreeable with the use of technology. However, they are still concerned about privacy, data security, work overload and the need for technological upgrades and providing support services (40).
a) Client Engagement: Appropriate communication between clients and therapists is essential for optimizing the process and the quality of care. The information technology must be designed to improve the interactions and eliminates obstacles between clients and therapists. Appropriate interactions lead to a successful patient management and enhance the client-therapist satisfaction (41).
b) Client’s Cultural and Social Background: Past and present medical history, cultural and social factors are regarded as factors influencing the development of mental health disorders. Some of the important social and cultural issues are: sex, social class, education, religious and non-religious beliefs, race and ethnicity. These factors may influence the therapy outcomes, hence the need for matching the system design and contents with the social and cultural background of clients (41).
c) Client’s Learning & perception Issues: System designers should consider that mental health clients may have low learning and perception levels. It is, therefore, essential that appropriate caution be exercised with instrumentation when managing these patients (42).
d) Therapist’s Skills, Perception and Working Style: Mental health therapists are generally concerned about introducing technologies into their practice, worrying that clinical programs might get disrupted, adversely altered, or face difficulty adapting to new protocols. The new changes may also affect the therapist’s perception of the overall efficacy of the care.
e) Extra Demands and Responsibilities of Therapists: The new technologies are not supposed to impose added workload and time demand on the medical staff. In fact, they are expected to reduce work stress, save time and lead to efficient interventions. Therapists may also be concerned about introducing modern technologies into their practice, thereby raising their responsibilities for additional contact time with clients.
2. Synchronous vs. Asynchronous Interactions: Appropriate interventions, mental health condition of the client, and the need for distant versus in-person therapy sessions must be thoroughly evaluated before making a decision to offer synchronous or asynchronous interactions. Thoughtful therapy plans can significantly improve the outcomes.
3. Requirements of Mental Healthcare Settings: In designing new systems, the clinical guidelines and protocols of the mental health settings should be followed so that the system performance continues smoothly (43). These include:
Abiding by the national and international regulations.
Basing system development on acceptable theoretical models of mental health care.
Creating a safe environment for storing patients’ data.
Respecting client’s privacy.
a) Creation of an Adaptable and Stable System: System adaptability to new technologies is the key requirement for designing new programs. New technologies are used for diverse clients from different socio-cultural backgrounds and for different mental disorders. Also, they are used by diverse population of therapists and patients. Therefore, such systems must be adaptable and stable enough to meet varying clinical circumstances (41).
b) Flexibility in Providing Support Services: The system design and access should be adaptable to divergent customer needs and applications. Therefore, each system should provide its support services through multiple user-friendly means.
Available Technologies
1. Videoconference, Telephone & Messaging Systems: Due to limited transportation and access to distant geographic locations, and the cost involved, video-conferencing and telephone messaging can facilitate patient access to mental health services (44). Video-conferencing omits the full-scale physical presence and some of the behavioral cues. Telephone excludes visual cues, and text messaging omits both sound and visual cues. E-mailing eliminates synchronous communication (45). Although communication technologies can widen the scope of healthcare services, certain concerns still remain.
The provision of mental services through multimedia reduces the need for physical presence of patients and therapists. However, it may not lead to the same therapeutic effect. Also, they may risk patient privacy or disrupt the management of critical cases. Research on the use of technologies in psychotherapy suggests that video-conferencing can provide effective services and has been received well by patients. Similarly, telephone and messaging systems have been effective, especially for clients residing in distant locations (46).
2. Web-based Interventions: Web-based services have a structure similar to face-to-face sessions, and can offer live opportunity for therapists to have successful interaction with patients. The service may include instructional components, evidence-based psychotherapy and opportunity for the clinicians to improve their clinical skills (47). Web-based interventions can be offered as textual, audiovisual or animated programs. They have interactive tools for feedback and supervision of the therapy sessions, and for enhancing patient learning experience (48).
3. Mobile Phone Technology: Mobile phones provide patients and therapists with an excellent communication means. They can send and receive text, voice and video messages, facilitating many forms of clinical interactions between therapists and patients (49).
4. Networking via Social Media & Group Discussions: Networking refers to the use of digital, web-based technologies and mobile phones to promote information transfer and communication among patients and therapists.
5. Simulated People and Places: Simulated methods refer to the use of three-dimensional, animated video presentations for mental health care purposes. One drawback in using simulators is the production cost; however, online virtual world is an excellent environment for providing mental health services. This environment was used for the first time to provide interactive and instructional programs via social media and chat rooms to promote healthy lifestyle among people with HIV infection (50). Using such technologies also help to extend sympathy and promote unity among social groups with similar conditions (51).
6. Internet Games: Fascinating games can motivate patients, promote therapies for mental disorders and can potentially lead to changes in abnormal behaviors. Using internet games in some cases can even serve as a remedy for some mental disorders, such as hyperactivity, autism and aggressive personality (52).
Advantages
Studies have suggested that telemental health care has promising potentials to fill the existing gaps between the current needs and innovations for future within the expected constraints. The future innovations may fall under four major headings: data provision; screening and evaluation; interventions; and social support (53). Many of these services may be simultaneously offered at mental health centers.
Regarding data provision, it is essential that they are analyzed and the quality is assured before making them available to mental health care clinicians. Currently, screening and evaluation tools are Internet-based, facilitating information access and utilization by practitioners serving mental health centers in many nations. Findings from literature reviews suggest that web-based capabilities lead to excellent coherence and reliable results for mental health services. They provide comprehensive and up-to-date information for use by patients, either individually or in groups (54, 55).
Social support networks offered through telemental health care are available in different web-based formats, such as group discussions, commercial bulletins, weblogs, chat rooms and other networks. In general, telemental health care consists of three types: a) Based on disease phases (i.e., prevention, preterm intervention, active treatment, maintenance or preventing recurrences); b) Based on the type of relations (between clinician and client or among clinicians, or clients);
c) Based on the therapy (i.e., behavioral or psychotherapy). Unlike conventional therapies, telemental health care is available for both individuals and groups. Recent studies suggest that the cost, efficacy, usefulness and profits on the investment, warrant establishing telemental health care services in many institutions (20, 46, 56, 57).
In summary, the major advantages of telemental health care include improved access, reduced costs, flexibility under most circumstances, and interactive sessions between clients and clinicians (54, 58). Telemental health care is particularly warranted for under-developed communities and nations where these services are not available locally.
Challenges
Key concerns about telemental health care are: a) necessary skills to use the technologies by both the clinicians and patients; b) necessary investment for establishing the equipment and periodic upgrades; c) subscribing to Internet services; and, d) regular evaluation of the service and its efficacy (59). Another concern is whether the service is covered by insurance coverage, which directly impacts the physicians’ revenue and may lead to bias against some patients (60). Unclear quality control and standards, clinician’s reluctance, anxiety and technophobia constitute other challenges to providing telemental health care (59, 60). Concerns also exist about marginalizing clients with physical and cognitive disabilities who are unable to use the equipment properly, making in-person services as the only feasible choice. Another concern is the lack of stable signals or access to Internet, that may make telemental health services unpopular (61). Lastly, ethical and regulatory concerns exist about the use of web-based services, since the patients’ privacy might be at risk, and the physicians may not be sure who else may be hearing the conversation between the clinicians and patients (58, 59, 62-69). National and international authorities are in the process of developing standards for web-based professional and medical services (60, 61).
5. CONCLUSIONS
Our findings indicate that telemental health care is cost effective and can lead to efficient and adaptable solutions to the care of patients with mental illnesses, with promising outcomes. The institutions currently providing or planning to provide this service are strongly advised to benefit from the feedback collected from both clients and clinicians, if successful outcomes are expected. Since a large majority of studies have attested to the efficiency, low costs and usefulness, telemental health care is the next logical step to delivering a state-of-the-art care to mental patients alongside the conventional care, especially in under-developed communities and nations. Considering the potentials of telemental health care, further research is required to evaluate its current applications and to explore its future promises.
Acknowledgement
The authors are grateful to the medical library and staff of School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran, for their valuable assistance with this study. Funding for this project was provided by Iran University of Medical Sciences, Tehran, Iran.
Footnotes
• Conflict of Interests: None declared.
• Authors’ Contributions: All authors participated in each step of this research.
REFERENCES
- 1.Diederich J, Song I. Mental health informatics: current approaches. Springer: Mental Health Informatics; 2014. pp. 1–16. [Google Scholar]
- 2.Stone RT, Wei CS, editors. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. SAGE Publications; 2011. Exploring the linkage between facial expression and mental workload for arithmetic tasks. [Google Scholar]
- 3.Angaran DM. Telemedicine and telepharmacy: current status and future implications. American Journal of Health-System Pharmacy. 1999;56(14):1405–26. doi: 10.1093/ajhp/56.14.1405. [DOI] [PubMed] [Google Scholar]
- 4.Frantzidis C, Bratsas C, Klados M, Konstantinidis E, Lithari CD, Vivas AB, et al. On the classification of emotional biosignals evoked while viewing affective pictures: an integrated data-mining-based approach for healthcare applications. Information Technology in Biomedicine, IEEE Transactions on. 2010;14(2):309–18. doi: 10.1109/TITB.2009.2038481. [DOI] [PubMed] [Google Scholar]
- 5.Hilty DM, Luo JS, Morache C, Marcelo DA, Nesbitt TS. Telepsychiatry. CNS drugs. 2002;16(8):527–48. doi: 10.2165/00023210-200216080-00003. [DOI] [PubMed] [Google Scholar]
- 6.Hilty DM, Marks SL, Urness D, Yellowlees PM, Nesbitt TS. In Review. Canadian Journal of Psychiatry. 2004;49:12–23. doi: 10.1177/070674370404900103. [DOI] [PubMed] [Google Scholar]
- 7.Tang L, Zhou X, Yu Z, Liang Y, Zhang D, Ni H. MHS: a multimedia system for improving medication adherence in elderly care. Systems Journal, IEEE. 2011;5(4):506–17. [Google Scholar]
- 8.Young KS. An empirical examination of client attitudes towards online counseling. CyberPsychology and Behavior. 2005;8(2):172–7. doi: 10.1089/cpb.2005.8.172. [DOI] [PubMed] [Google Scholar]
- 9.Coyle D, Doherty G, Matthews M, Sharry J. Computers in talk-based mental health interventions. Interacting with computers. 2007;19(4):545–62. [Google Scholar]
- 10.Elkin N. How America searches: Health and wellness. Opinion Research Corporation: iCrossing; 2008. pp. 1–17. [Google Scholar]
- 11.Yellowlees P, Burke MM, Marks SL, Hilty DM, Shore JH. Emergency telepsychiatry. Journal of telemedicine and telecare. 2008;14(6):277–81. doi: 10.1258/jtt.2008.080419. [DOI] [PubMed] [Google Scholar]
- 12.Nambu M, Nakajima K, Noshiro M, Tamura T. An algorithm for the automatic detection of health conditions. Engineering in Medicine and Biology Magazine, IEEE. 2005;24(4):38–42. doi: 10.1109/memb.2005.1463394. [DOI] [PubMed] [Google Scholar]
- 13.Song I, Marsh NV. Anonymous indexing of health conditions for a similarity measure. Information Technology in Biomedicine, IEEE Transactions on. 2012;16(4):737–44. doi: 10.1109/TITB.2012.2194717. [DOI] [PubMed] [Google Scholar]
- 14.Tilaka AD, Diederich J, Song I, Teoh AN. Automated method for diagnosing speech and language dysfunction in schizophrenia. Mental Health Informatics: Springer. 2014:201–15. [Google Scholar]
- 15.Pantic M, Rothkrantz LJ. Automatic analysis of facial expressions: The state of the art. Pattern Analysis and Machine Intelligence, IEEE Transactions on. 2000;22(12):1424–45. [Google Scholar]
- 16.Valstar MF, Pantic M. Fully automatic recognition of the temporal phases of facial actions. Systems, Man, and Cybernetics, Part B: Cybernetics, IEEE Transactions on. 2012;42(1):28–43. doi: 10.1109/TSMCB.2011.2163710. [DOI] [PubMed] [Google Scholar]
- 17.Luneski A, Bamidis PD, Hitoglou-Antoniadou M. Affective computing and medical informatics: state of the art in emotion-aware medical applications. Studies in health technology and informatics. 2008;136:517. [PubMed] [Google Scholar]
- 18.Critchley HD. Book review: electrodermal responses: what happens in the brain. The Neuroscientist. 2002;8(2):132–42. doi: 10.1177/107385840200800209. [DOI] [PubMed] [Google Scholar]
- 19.Sarasohn-Kahn J. The wisdom of patients: Health care meets online social media. Oakland, CA: California HealthCare Foundation; 2008. [Google Scholar]
- 20.Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemedicine and e-Health. 2013;19(6):444–54. doi: 10.1089/tmj.2013.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McWilliams JK. Integrating Telemental Healthcare with the Patient-Centered Medical Home Model. Journal of child and adolescent psychopharmacology. 2015 doi: 10.1089/cap.2015.0044. [DOI] [PubMed] [Google Scholar]
- 22.Lindsay JA, Kauth MR, Hudson S, Martin LA, Ramsey DJ, Daily L, et al. Implementation of video telehealth to improve access to evidence-based psychotherapy for posttraumatic stress disorder. Telemedicine and e-Health. 2015;21(6):467–72. doi: 10.1089/tmj.2014.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lal S, Adair CE. E-mental health: a rapid review of the literature. Psychiatric Services. 2014;65(1):24–32. doi: 10.1176/appi.ps.201300009. [DOI] [PubMed] [Google Scholar]
- 24.Mohr DC, Burns MN, Schueller SM, Clarke G, Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. General hospital psychiatry. 2013;35(4):332–8. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olsen MR, Casado-Lumbreras C, Colomo-Palacios R. ADHD in eHealth - A Systematic Literature Review. Procedia Computer Science. 2016;100:207–14. [Google Scholar]
- 26.Vernig PM. Telemental Health: Digital disruption and the opportunity to expand care. Journal of the American Psychiatric Nurses Association. 2016;22(1):73–5. doi: 10.1177/1078390315623947. [DOI] [PubMed] [Google Scholar]
- 27.Crowe TV. Is Telemental Health Services a Viable Alternative to Traditional Psychotherapy for Deaf Individuals? Community Mental Health Journal. 2017;53(2):154–62. doi: 10.1007/s10597-016-0025-3. [DOI] [PubMed] [Google Scholar]
- 28.Moussa Y, Mahdanian AA, Yu C, Segal M, Looper KJ, Vahia IV, et al. Mobile Health Technology in Late-Life Mental Illness: a Focused Literature Review. The American Journal of Geriatric Psychiatry. 2017 doi: 10.1016/j.jagp.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Haghdoost AA, Sadeghirad B. Systematic Review & Meta Analysis concepts, Applications & Statistical Practices. Tehran Gap Publications; 2015. [Google Scholar]
- 30.Tarvainen MP, Koistinen AS, Valkonen-Korhonen M, Partanen J, Karjalainen PA. Analysis of galvanic skin responses with principal components and clustering techniques. Biomedical Engineering, IEEE Transactions on. 2001;48(10):1071–9. doi: 10.1109/10.951509. [DOI] [PubMed] [Google Scholar]
- 31.Elvevåg B, Foltz PW, Rosenstein M, DeLisi LE. An automated method to analyze language use in patients with schizophrenia and their first-degree relatives. Journal of neurolinguistics. 2010;23(3):270–84. doi: 10.1016/j.jneuroling.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goh TJ, Diederich J, Song I, Sung M. Mental Health Informatics. Springer; 2014. Using diagnostic information to develop a machine learning application for the effective screening of autism spectrum disorders; pp. 229–45. [Google Scholar]
- 33.Panagiotakopoulos TC, Lyras DP, Livaditis M, Sgarbas KN, Anastassopoulos GC, Lymberopoulos DK. A contextual data mining approach toward assisting the treatment of anxiety disorders. Information Technology in Biomedicine, IEEE Transactions on. 2010;14(3):567–81. doi: 10.1109/TITB.2009.2038905. [DOI] [PubMed] [Google Scholar]
- 34.McKay E, Martin J. Mental health and wellbeing: Converging HCI with human informatics in higher education. Issues Inf Sci Inf Technol. 2010;7(3):339–51. [Google Scholar]
- 35.Williams M, Pfeffer MM, Hilty DM. Telepsychiatry in the emergency department. California HealthCare Foundation; 2009. [Google Scholar]
- 36.Yellowlees PM, Odor A, Michelle Burke Parish B, Iosif A-M, Haught K, Hilty D. A feasibility study of the use of asynchronous telepsychiatry for psychiatric consultations. Psychiatric Services. 2010 doi: 10.1176/ps.2010.61.8.838. [DOI] [PubMed] [Google Scholar]
- 37.Butler TN, Yellowlees P. Cost analysis of store-and-forward telepsychiatry as a consultation model for primary care. Telemedicine and e-Health. 2012;18(1):74–77. doi: 10.1089/tmj.2011.0086. [DOI] [PubMed] [Google Scholar]
- 38.Hollingsworth JM, Saint S, Hayward RA, Rogers MA, Zhang L, Miller DC. Specialty care and the patient-centered medical home. Medical care. 2011;49(1):4–9. doi: 10.1097/MLR.0b013e3181f537b0. [DOI] [PubMed] [Google Scholar]
- 39.Coyle D, Doherty G. Towards Ontologies for Technology in Mental Health Interventions. Ontologies in Interactive Systems, 2008 ONTORACT' 08 First International Workshop on. IEEE. 2008 [Google Scholar]
- 40.Doherty G, Coyle D, Matthews M. Design and evaluation guidelines for mental health technologies. Interacting with computers. 2010;22(4):243–52. [Google Scholar]
- 41.Coyle D, Doherty G. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. ACM; 2009. Clinical evaluations and collaborative design: developing new technologies for mental healthcare interventions. [Google Scholar]
- 42.Coyle D, Doherty G, Sharry J. An evaluation of a solution focused computer game in adolescent interventions. Clinical Child Psychology and Psychiatry. 2009;14(3):345–60. doi: 10.1177/1359104508100884. [DOI] [PubMed] [Google Scholar]
- 43.Roberts LW, Dyer AR. Concise guide to ethics in mental health care. American Psychiatric Pub. 2007 [Google Scholar]
- 44.Kazdin AE. Evidence-based treatment research: Advances, limitations, and next steps. American Psychologist. 2011;66(8):685. doi: 10.1037/a0024975. [DOI] [PubMed] [Google Scholar]
- 45.Mohr D, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. Journal of medical Internet research. 2011;13(1):e30. doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richardson LK, Christopher Frueh B, Grubaugh AL, Egede L, Elhai JD. Current directions in videoconferencing tele-mental health research. Clinical Psychology: Science and Practice. 2009;16(3):323–38. doi: 10.1111/j.1468-2850.2009.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ritterband LM, Tate DF. The science of internet interventions. Annals of Behavioral Medicine. 2009;38(1):1–3. doi: 10.1007/s12160-009-9132-5. [DOI] [PubMed] [Google Scholar]
- 48.Vernon ML. A review of computer-based alcohol problem services designed for the general public. Journal of substance abuse treatment. 2010;38(3):203–11. doi: 10.1016/j.jsat.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Høybye MT, Dalton SO, Deltour I, Bidstrup P, Frederiksen K, Johansen C. Effect of Internet peer-support groups on psychosocial adjustment to cancer: a randomised study. British journal of cancer. 2010;102(9):1348–54. doi: 10.1038/sj.bjc.6605646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beard L, Wilson K, Morra D, Keelan J. A survey of health-related activities on second life. Journal of Medical Internet Research. 2009;11(2):e17. doi: 10.2196/jmir.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bickmore T, Gruber A, Picard R. Establishing the computer–patient working alliance in automated health behavior change interventions. Patient education and counseling. 2005;59(1):21–30. doi: 10.1016/j.pec.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 52.Wilkinson N, Ang RP, Goh DH. Online video game therapy for mental health concerns: a review. International journal of social psychiatry. 2008;54(4):370–82. doi: 10.1177/0020764008091659. [DOI] [PubMed] [Google Scholar]
- 53.Diamond G, Levy S, Bevans KB, Fein JA, Wintersteen MB, Tien A, et al. Development, validation, and utility of internet-based, behavioral health screen for adolescents. Pediatrics. 2010;126(1):e163–e170. doi: 10.1542/peds.2009-3272. [DOI] [PubMed] [Google Scholar]
- 54.Farrell SP, Mahone IH, Zerull LM, Guerlain S, Akan D, Hauenstein E, et al. Electronic screening for mental health in rural primary care: implementation. Issues in mental health nursing. 2009;30(3):165–73. doi: 10.1080/01612840802694411. [DOI] [PubMed] [Google Scholar]
- 55.Masic I, Mihalas G, et al. Contributions to the History of Medical Informatics. Sarajevo: Avicena; 2014. ISBN 978-9958-720-56-7. [Google Scholar]
- 56.Morland LA, Greene CJ, Rosen C, Mauldin PD, Frueh BC. Issues in the design of a randomized noninferiority clinical trial of telemental health psychotherapy for rural combat veterans with PTSD. Contemporary clinical trials. 2009;30(6):513–22. doi: 10.1016/j.cct.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 57.Hilty DM, Yellowlees PM, Cobb HC, Bourgeois JA, Neufeld JD, Nesbitt TS. Models of telepsychiatric consultation - liaison service to rural primary care. Psychosomatics. 2006;47(2):152–7. doi: 10.1176/appi.psy.47.2.152. [DOI] [PubMed] [Google Scholar]
- 58.Tillfors M, Carlbring P, Furmark T, Lewenhaupt S, Spak M, Eriksson A, et al. Treating university students with social phobia and public speaking fears: internet delivered self-help with or without live group exposure sessions. Depression and Anxiety. 2008;25(8):708–17. doi: 10.1002/da.20416. [DOI] [PubMed] [Google Scholar]
- 59.Christensen H, Hickie IB. Using e-health applications to deliver new mental health services. Medical Journal of Australia. 2010;192(11):S53. doi: 10.5694/j.1326-5377.2010.tb03695.x. [DOI] [PubMed] [Google Scholar]
- 60.Emmelkamp PM. Technological innovations in clinical assessment and psychotherapy. Psychotherapy and psychosomatics. 2005;74(6):336–43. doi: 10.1159/000087780. [DOI] [PubMed] [Google Scholar]
- 61.Ybarra ML, Eaton WW. Internet-based mental health interventions. Mental health services research. 2005;7(2):75–87. doi: 10.1007/s11020-005-3779-8. [DOI] [PubMed] [Google Scholar]
- 62.Masic I. E-learning as new method of medical education. Acta Inform Med. 2008;16(2):102–17. doi: 10.5455/aim.2008.16.102-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Perecherla S. Web matters. Evidence Based Mental Health. 2009;12(1):4–6. doi: 10.1136/ebmh.12.1.4. [DOI] [PubMed] [Google Scholar]
- 64.Masic I, Pandza H, Kulasin I, Masic Z, Valjevac S. Tele-education as a method of medical education. Med Arh. 2009;63(6):350–8. doi: 10.5455/medarh.2009.63.350-353. [DOI] [PubMed] [Google Scholar]
- 65.Masic I. Telematika u medicini - perspektive razvoja u BiH. Med Arh. 1995;49(3-4):69–70. [PubMed] [Google Scholar]
- 66.Masic I, Sivic S. Social networks in medical education in Bosnia and Herzegovina. Mater Sociomed. 2012;24(3):162–4. doi: 10.5455/msm.2012.24.162-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Masic I, Novo A, Kudumovic M, Masic Z. E-learning at Medical faculty of Sarajevo University. Acta Inform Med. 2005;13(3):132–5. [Google Scholar]
- 68.Masic Z, Novo A, Masic I, Kudumovic M, Toromanovic S, Rama A, et al. Distance Laerning at Biomedical Faculties in Bosnia and Herzegovina. Stud Health Technol Inform. 2005;116:267–72. [PubMed] [Google Scholar]


