Abstract
Objectives:
Each surgical patient is preoperatively, intraoperatively and postoperatively exposed to stress. The aim of this study was to determine the existence of preoperative anxiety, and to determine its impact on hemodynamic parameters (blood pressure, heart rate) in patients and dose of anesthetics during induction of anesthesia.
Methods:
A prospective clinical study conducted at the Department of Anesthesiology and Reanimation and Surgery Clinic of University Clinical Center Tuzla (UCC) in the period May 2012. to January 2015. The 80 patients were analyzed which were planned for and done an elective cholecystectomy surgery or herniectomy surgical intervention. Preoperative anxiety was measured with the help of Spielberg test and evaluation of depth of anesthesia was performed with BIS monitoring.
Results:
The results showed that all patients had some degree of preoperative manifest anxiety. Average values of mean arterial pressure, preoperatively and after the induction of general anesthesia, differed for 15,4 mm/Hg, but were not observed significant association between Spielberg score and differences in blood pressure. Preoperative anxiety is a significant predictor of administered dose of anesthetic. Each additional score on Spielberg scale reduces the dose of anesthetic for 0,304 mg/kgTT.
Conclusion:
Adequate assessment of preoperative anxiety and undertaking of certain steps to reduce it can assist in accurately determining the required dosage of anesthetic for the introduction of general anesthesia.
Keywords: Anxiety, general anesthesia, hemodynamic changes, the dose of anesthetic
1. INTRODUCTION
Every part of human life is characterized by a more or less balanced relationship between the human himself, environment, health and disease. This relationship is not static, it is dynamic. Violation of this relationship has a result in damage of health, disease, and sometimes the need for surgery. Many experts believe that some of us are by nature prone to fear or discomfort more than others, but it is possible that something in the past served as a trigger for a particular expressed anxiety (1). Oppression or anxiety is an “alarm” reaction of the human body to a perceived physical or psychological threat. Anxiety is a special mode of manifestation of fear. A person experiences anxiety of some impending danger. Anxiety usually consists of a series of somatic transient events such as: tachycardia, hypertension, sweating, a feeling of restlessness, nervousness.
Anxiety can manifest itself through the daily care of life, and may be related to a specific event, such as surgery. Patients who are preparing for surgery should not suffer needless anxiety. For some, even the thought of surgery and anesthesia increases the feeling of anxiety (2). Boker et al. in their study reported that 60% of patients who have been ordered for elective surgery experienced preoperative anxiety (3). In a state of acute anxiety we can be before a big event or experience (1). For someone, one of these events may be an upcoming surgery. What follows shortly before the surgery is adequate preoperative preparation of the patient (4).
Good preparation of the patient reduces the possible complications during anesthesia and possible postoperative complications. The extent of the examination and diagnostic tests before surgery is determined according to the type of surgery, the patient’s medical condition and the urgency of the surgery. Preparing for surgery can be performed in a hospital or outside the hospital (5).
The aim of this study was to determine the influence of preoperative anxiety on hemodynamic changes in patients who were planned for elective surgery (laparoscopic cholecystectomy, herniectomy). The increase in mean arterial pressure and heart rate in patients with increased preoperative anxiety was narrower topic of this study. Also, the aim of the study was to determine the total consumption of anesthetic required to achieve optimal depth of anesthesia (BIS 50) depending on the degree of anxiety.
2. PATIENTS AND METHODS
A prospective clinical study conducted at the Department of Anesthesiology and Reanimation and Surgery Clinic of University Clinical Center Tuzla (UCC) in the period May 2013. to January 2015. The study included 80 patients with physical status of ASA1 and ASA2 which were planned for and done elective surgery cholecystectomy or herniectomy. Local ethics committee approval was obtained. Exclusion criteria of the study were: psychiatric diseases, cardiovascular diseases (hypertension), pregnancy, treatment with antidepressants and anxiolytics. According to the degree of anxiety patients were, after the test, divided into two groups: patients with mild (Group I) and patients with moderate to high levels of preoperative anxiety (Group II). Monitoring parameters in this study were: preoperative anxiety (test–STAi) hemodynamic parameters–blood pressure, heart rate and depth of anesthesia and anesthetics consumption–bispectral index (BiS).
Research description
In all patients preoperatively were recorded: body weight (BW), sex, age, previous experience with the operation, if they had them. Patients were not administered sedatives on the eve of surgery. Protocol of anesthesia induction was identical for all patients:Midazolam (Flormidal) 0.01-0.1mg/kg, Atropine 0.5mg, Fentanyl 0,05-0,1mg, Nesdonal (Thiopental) to achieve value of bispectral index (BIS) 50, Tracrium 0.3-0.6mg/kg of body weight. Upon entering the operating room, patients were asked to complete a test for the evaluation of preoperative anxiety (Spielberg test). Blood pressure and heart rate were measured on two occasions. The first measurement after placing the patient on the operating table-preoperatively (T1) and second in value of bispectral index (BIS) 50 on the induction of anesthesia (T2).
Statistics
Statistical tests were done using the software package SPSS 19.0. All variables were tested on affiliation for normal distribution using Kolmogorof-Smirnov test. All variables are presented descriptively using appropriate measures of central tendency (arithmetic mean and median) and dispersion (standard deviation and interquartile range). Quantitative variables were compared using Student’s t-test adjusted for unequal variances where necessary, with the use of variants of the test for related samples where the conditions required to. The frequencies of qualitative variables were compared using the chi-square test with continuity correction for tables 2x2. Comparisons of quantitative variables for the two groups of patients were made using ANOVA analysis with the application of the post-hoc Tukey test. Relationships between variables were tested using the Pearson and Spearman correlation. It is also applied stepped linear regression analysis to quantify the real connection between the variables using the method of elimination of “confounder” variables. All tests were done with a confidence level of 95% (p <0.05).
3. RESULTS
The study included 80 patients, of whom 57 (71.3%) underwent cholecystectomy, while the remaining 23 (28.7%) underwent surgery of hernioplastics. The gender representation in the pattern was in favor of females with a share of 47 (58.8%) of the total pattern, while the remaining 33 (41.3%) of the patients were male, which matched the ratio F:M of 1,42:1. The mean age (SD) in the pattern was 47 years with a minimum of 23 and maximum of 76 years. Age distribution according to gender was 47 (59%) men and 33 (41%) for women. There was no statistically significant difference (t=1.54; df=78; p=0.13) in the average age of men (49±14) and women (45±12) of the patients. Previous experience of surgery had 27 (33.8%) of patients, while the remaining 53 (66.3%) underwent surgery for the first time in their life. Descriptive values of doses of anesthetics, and systolic, diastolic and mean arterial pressure and heart rate in the above measurements are shown in Table 1.
Table 1.
Distribution of pressure value and heart rate depending on the time of measurement
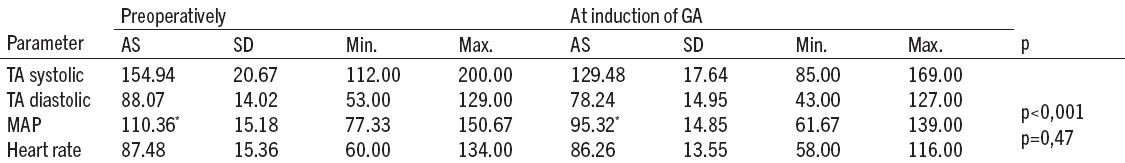
Average values of preoperative MAP and MAP values on the induction of anesthesia differed by an average of 15.04 mmHg (%95CI=11.91-18.18), which was statistically significant (t=9,55; df=79; p<0,001). However, when it comes to heart rate we detected an average difference of 1.22 (%95CI=-2,12-4,54), which was not statistically significant (t=0,72; df=79; p=0,47).
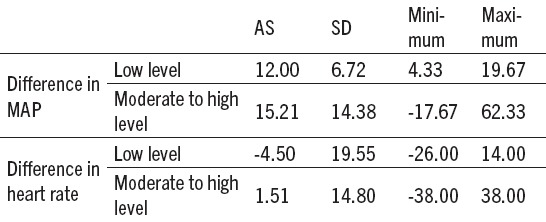
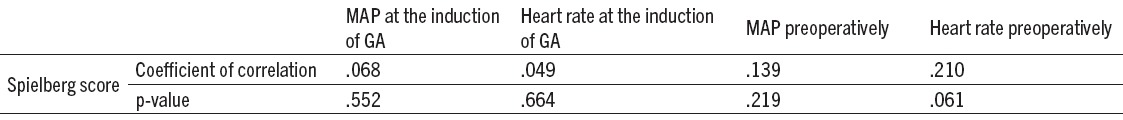
Average values of Spielberg score in the complete pattern were 53 (9) with a range from 35 to 75 scores. According to categories of Spielberg score low level of manifest anxiety had 4 or 5% of patients, moderate level of manifest anxiety 60 or 75% of the patients and the high level of manifest anxiety 16 or 20% of the patients. We performed correlation between Spielberg score, on the one hand and the difference in the values of MAP and heart frequency between measurements before operation and after the induction of general anesthesia (GA). We did not detect significant correlations between Spielberg score and differences in MAP (ρ=0,04; p=0,73), and between Spielberg score and the differences in the heart frequency (p=0,13; p=0,27) (Table 2).
Table 2.
The correlation of MAP heart rate preoperatively with the level of anxiety
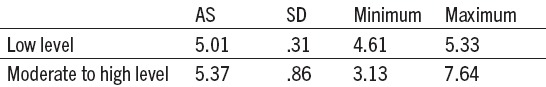
Then we evaluated the link between anesthetic doses per kg/BW and Spielberg score. There was a statistically significant, medium strong and negative correlation between these two variables (r=-0,322; p=0,004)(Table 3).
Table 3.
Dose of anesthetic
And finally we performed the linear regression analysis with the use of stepped techniques, in order to exclude the impact of previous operating experience on the level of anxiety, and thus the dose of administered anesthetic. After controlling for the influence of the previous operational experience, it was found that the level of anxiety according to Spielberg’s test is a significant predictor of administered doses of anesthetics on kgBW, (β=-0,304; p=0,006). This means that by controlling the impact of previous operating experience, for each additional score on the Spielberg scale, the dose of anesthetic per kg/BW falls to 0.304 mg/kg BW. There was no statistically significant correlation between the value of Spielberg score and the value of MAP and heart rate in both measurements (Table 4).
Table 4.
Correlation between the value of Spielberg score and MAP value and heart rate
4. DISCUSSION
The study included 80 patients, of whom 71.3% underwent cholecystectomy, and 28.7% underwent surgery of hernioplastics. Average values of Spielberg score (STAI) in the complete pattern were 53 with a range from 35 to 75 scores. Frequency by categories was 76.95% of moderate to high level of anxiety, and 5% of low if we take the limit value of 40 scores between groups. Thus, we can conclude that all patients had a level of preoperative anxiety. Prior operational experience had 27 (33.8%), while the remaining 53 (66.3%) had no experience. In this research, we compared the values of Spielberg score between patients who did and those who did not have prior operational experience. The difference between them was not statistically significant (p=0,16).
In studies in the UK 82% of patients who were operated have expressed a desire to know more about the surgical procedure prior to surgery. The research results (6,7) shows that patients who have more information about a surgical procedure that will go through and the way of anesthesia, have lower levels of anxiety, and that anxiety correlates night before and immediately before surgery, it is higher in females and those with no previous operational experience. The practice of giving preoperative notice may reduce anxiety level (8).
In this study, by analysis of medium arterial pressure (MAP), the average values of MAP preoperatively (T1) and MAP values on the induction of anesthesia (T2) differed by an average of 15,04 mmHg (%95CI=11,91-18,18), which was statistically significant (t=9,55; df=79; p<0,001). However, when it comes to heart rate, we detected a difference from the average of 1,22 (%95CI=-2,12-4,54), which was not statistically significant (t=0,72; df=79; p=0,47). We performed correlation between Spielberg score, on the one hand and the difference in the values of MAP and heart frequency between measurements before surgery and after the induction of the GA We did not detect significant correlations between Spielberg score and differences in MAP (ρ=0,04; p=0,73), and between Spielberg score and heart rate differences (ρ=0,13; p=0,27). The difference between the values of the MAP preoperatively and on the induction of anesthesia can be explained in the framework of action of sedatives and anesthetics that are used for pre-medication and induction of general anesthesia.
In a study conducted by Memnune et al (2005) they evaluated the effect of pre-medication on the anxiety level, the amount of cortisol, volume and pH of gastric contents. The study was conducted on 100 patients with ASA physical statuses of I-II, which were randomly divided into two groups. One group was treated with placebo, while the other had pre-medication with Diazepam 10mg in the evening and 1.5 mg of Midazolam fifteen minutes before surgery. The level of anxiety was assessed by Spielberg test. In the placebo group, the values of the measured parameters were increased, compared to patients who received pre-medication (9).
The study San et al (2008) determined the preoperative anxiety in various elective surgeries in ophthalmology, gynecology, and urology. Preoperative anxiety was measured in those who were pre-medicated with Diazepam, and those who are not pre-medicated. The authors found that the preoperative anxiety and blood pressure is significantly lower in those patients who received pre-medication (10).
In this study, we also analyzed a relationship between dose of anesthetic per kgBW and Spielberg score. There was a statistically significant, medium strong and negative correlation between these two variables (r=-0,322; p=0,004). By linear regression analysis with the use of stepped techniques, we tested the effects of previous operating experience on the level of anxiety, and thus the dose of administered anesthetic. After controlling for the influence of the previous operational experience, it was found that the level of anxiety according to Spielberg’s test is a significant predictor of administered dose of anesthetics on kgBW, with β=-0,304; p=0,006. This means that by controlling the impact of previous operating experience, for each additional score on the Spielberg scale, the dose of anesthetic per kg/BW falls to 0.304 mg/kg BW.
In a study by Maranets et al (1999) authors were checking whether higher doses of anesthetics are needed in anxious patients. The study was conducted on 57 female patients who underwent gynecological surgery. General-TRAI and current-STAI (related to the upcoming surgery) anxiety were evaluated immediately before surgery, and recorded the dose of propofol for induction and maintenance of anesthesia. They proved that female patients with high general anxiety need more propofol for induction and maintenance of anesthesia, while in the current anxiety the influence on the dose of anesthetic was not found. So they concluded that the dose of anesthetic administered by the anesthesiologist should be changed based on the level of anxiety for each patient (11).
5. CONCLUSIONS
This research revealed that all tested patients had some level of preoperative manifest anxiety. According to Spielberg score categories 4,5% patients had low, 16,2 % mild, and 60,75 % high level of preoperative anxiety. Average values of mean arterial pressure (MAP) preoperatively and values of MAP at the induction of anesthesia differed for 15,4 mmHg. Detected differences in the values of heart rate in both measurements were not statistically significant. There is a slight tendency to those without prior operational experience to have a higher level of preoperative anxiety, but this difference still was not statistically significant. There was no significant association between Spielberg score and differences in the values of the MAP and the heart rate in both measurements. There is a correlation between the level of preoperative anxiety and doses of anesthetic. The level of preoperative anxiety according to Spielberg test is a significant predictor of administered dose of anesthetic in kg/BW. After controlling for prior operational experience, each additional score on the Spielberg scale reduces the dose of anesthetic to 0,304 mg/kgBW.
Footnotes
• Conflict of interest: none declared.
• Authors contributions: All authors participated in every step of research and gave final approval of the version to be submitted.
REFERENCES
- 1.Ayyadhah Alanazi A. Reducing Anxiety in Preoperative Patients: A Systematic Review. British Journal of Nursing. 2014;23:387–93. doi: 10.12968/bjon.2014.23.7.387. [DOI] [PubMed] [Google Scholar]
- 2.White PF. Pharmacologic and clinical aspects of pre-operative medication. Anesthesia and Analgesia. 1986;65:963–74. [PubMed] [Google Scholar]
- 3.Boker A, Brownell Donen N. The Amsterdam preoperative anxiety and information scale provides a simple and reliable measure of preoperative anxiety. Can J Anaesth. 2002;49:792–8. doi: 10.1007/BF03017410. [DOI] [PubMed] [Google Scholar]
- 4.Vesel J. Medical psychology with psychopathology. Belgrade. 1978:86–91. [Google Scholar]
- 5.Jaime Ortiz, Suwei Wang, MacArthur A, Elayda, Daniel A. Tolpin Preoperative patient education: can we improve satisfaction and reduce anxiety? Brazilian Journal of Anesthesiology (English Edition) 2015;65(1):7–13. doi: 10.1016/j.bjan.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Hashimoto Y, Baba S, Koh H, Takagi H, Ishihara H, Matsuki A. Anxiolytic effect of preoperative showing of anesthesia video for surgical patients. Anesth Analg. 1993;42:611–6. [PubMed] [Google Scholar]
- 7.Moerman N, van Dam FS, Muller MJ, Oosting H. The Amsterdam preoperative anxiety and information scale (APAIS) Anesth Analg. 1996;82:445–51. doi: 10.1097/00000539-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Johnston M. Impending surgery. In: Fisher S, Reason J, editors. Handbook of life stress. New York: John Wiley & Sons; 1988. pp. 79–100. [Google Scholar]
- 9.Memnune P, Bilge C. The Effect of pre-medication on preoperative anxiety. Middle East Journal of Anesthesiology. 2005;18:421–33. [PubMed] [Google Scholar]
- 10.Sun GC, Hsu MC, Chia YY, Chen PY, Shaw FZ. Effect of age and gender on intravenous midazolam pre-medication: a randomized double - blind study. Br J Anaestesya. 2008;101:632–9. doi: 10.1093/bja/aen251. [DOI] [PubMed] [Google Scholar]
- 11.Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg. 1999;89:134. doi: 10.1097/00000539-199912000-00003. [DOI] [PubMed] [Google Scholar]


